Abstract
Introduction:
The best treatment for intertrochanteric fractures remains controversial. Many methods have been recommended.
Aim:
We aimed to assess the results of osteosynthesis using the Proximal Femoral Nail Antirotation (PFNA) system.
Patients and Methods:
We retrospectively analyzed 113 consecutive patients with intertrochanteric fractures treated with PFNA. Fractures were classified in accordance with the AO/OTA classification system into the groups A1, A2 and A3. The postoperative quality of fracture reduction was described as good, acceptable or poor. The location of the blade within the head was recorded as per the Cleveland method. Tip-apex distance (TAD) was used as a method for evaluating screw position. Pre-fracture and postoperative functional level were evaluated by the new mobility score (NMS).
Results:
The average age at the time of surgery was 75.9 years. The majority, 75 (66.3 %), were unstable fracture types. The reduction was good in 67 (61.4 %) cases. Of the 24 deaths, 19 patients had comorbidities (p < 0.001). The number of deaths in the first 6 months was significantly higher than in the next 6 months (p = 0.001). The mean TAD was 25.6 mm. The Cleveland zone centre-centre was the most common placement of the blade, accounting for 33 (29 %) of the cases. Reoperation was required in four patients. There were four patients with cut-out. The pre-facture mean value NMS was 8.6 (SD 1.1) and the postoperative mean value was 4.3 (SD 3.6).
Conclusion:
We concluded that PFNA offers biomechanical advantages, but the best position of the blade is still unknown.
Keywords: intertrochanteric fractures, PFNA, cut-out, mobility
1. INTRODUCTION
Intertrochanteric fractures occur mostly in elderly patients, and the outcome may be extremely poor if there is prolonged bed-rest. The best treatment for trochanteric fracture remains controversial (1, 2, 3). Many methods have been recommended (4, 5, 6). Stable fixation that allows early mobilization is the treatment of choice. Cephalomedullary devices are favored as the treatment for unstable A2 and A3 fractures, especially in the absence of medial buttressing (2, 3, 6, 7). While there are numerous operative devices for treatment of trochanteric fractures, none of them are totally free of complications. There is no advantage to an intramedullary nail versus a sliding compression hip screw for low-energy pertrochanteric fractures classified by Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) 31-A1 and A2, specifically given its increased cost and the lack of evidence to show decreased complications or improved patient outcome (4). The treatment of unstable trochanteric femoral fractures is still challenging.
Unstable proximal femoral fractures were treated successfully with Proximal Femoral Nail Antirotation (PFNA; Synthes, Oberdorf, Switzerland). Insertion of the blade compacts the cancellous bone. These characteristics provide optimal anchoring and stability when the implant is inserted into osteoporotic bone and have been bio-mechanically proven to retard rotation and varus collapse. The inserted PFNA blade achieves an excellent fit through bone compaction and requires less bone removal compared to a screw (6, 7). In this study, we aimed to assess the results of osteosynthesis using the PFNA system, in the treatment of intertrochanteric fractures including operative and postoperative complications, general complications and final outcome measurements.
2. PATIENTS AND METHODS
We retrospective analyzed all the patients with intertrochanteric fractures treated with PFNA at our institution from 1st June 2011 to 31st May 2013. The study included 113 consecutive patients. Closed nails were placed in all of the patients with the exception of three patients. All nails were statically locked. The desired position of the implant was in the anterior-posterior (AP) view, in the inferior half of the femoral neck. In the lateral view, it should be positioned in the center of the femoral neck and the tip within 5–10 mm of the subchondral bone (7). The location of the blade within the head was recorded as per the Cleveland method, on a lateral X-ray of the femoral head, divided into nine sections (8). Radiographs were examined to assess the fracture type, quality of fracture reduction, position of the screw, tip-apex distance (TAD) and union with use of preoperative and postoperative A-P and lateral radiographs. All specifications were measured in the picture archiving and communication system (PACS).
Fractures were classified according to the AO/OTA classification system into the groups A1, A2 and A3 and into subgroups (9). The postoperative quality of fracture reduction was described as good, acceptable or poor, according to the definitions of the three-grade classification system proposed by Baumgaertner et al. (10). The TAD was used as a method of evaluating screw position. The TAD is the sum in millimeters of the distance from the tip of the screw to the apex of the femoral head on AP and lateral views. The first postoperative radiographs were used to measure the TAD. Non-union was defined by routine clinical and radiological criteria, and the need for a further surgical procedure. The blood transfusions performed during or after the operation were recorded in the milliliters. Traffic accident and fall from height as fracture cause was defined as high-energy trauma.
In the present study, all patients received prophylactic antibiotic therapy as follows: 2 grams of cephalosporine were given before and 24 hours after treatments. In addition, low-molecular-weight heparin was administered once every day for 6 weeks. After treatment, active contraction exercises were carried out on the muscles, such as ankle active dorsiflexion and plantar flexion, and isometric contraction activities of the quadriceps. The patients also started to walk with full weight-bearing with a walking aid as soon as possible.
On admission, the medical condition was assessed and classified according to the American Society of Anaesthesiologists (ASA) grade (11). Health status was classified as poor (ASA 3–4) or good (ASA 1–2) (12). Pre-fracture and postoperative functional level were evaluated by the new mobility score (NMS), with a scale of 0 (immobile) to 9 (independently mobile) (13). During the work on the study, we contacted 98 patients (excluding six who died in the hospital and nine who had no contact) or their family members by phone, which gave us information about the functional level evaluated by the NMS. All tests were performed with 95 percent confidence level (p < 0.05). All statistical analysis procedures were performed by using SPSS 20.0 (SPSS, Chicago, IL, USA).
3. RESULTS
The average age at the time of surgery was 75.9 years (range 24–95 years); 80 patients were women and 33 were men. The average length of the follow-up period was 22 months (range 8-25 months). Associated injuries were noted in 16 patients (14.2 %), and in 13 (11.1 %) with fractures. There were 61 (54 %) left and 52 (46 %) right hip fractures. Low-energy trauma was the cause of fractures in 99 patients (87.6 %), fall from height in nine, traffic accidents in four and one suicide attempt. All fractures were closed. The average waiting time for hospitalization was 1.9 days (range 0-32 days). Time from fracture to surgery was on average 3.7 days (range 0-33 days). Nine (7.9 %) patients were treated within 6 hours after suffering the injury. The average length of hospital stay was 12.5 days (range 6-43 days). The longest hospitalization was 43 days (patient with deep infection and subsequent non-union) and another one was 41 days (with refixation, deep infection with Escherichia coli and Actinobacter species, and lethal outcome). There were 63 patients (56 %) with a good health status, while the remaining 50 patients (44 %) had poor health status. There were no significant differences in the total number of deaths when compared between patients stratified according to ASA score (X2 = 0.084; df = 1; p = 0.77). During the first 3 months of follow-up after the surgical treatment, lethal outcome was observed in eight patients with ASA scores of 3 and 4. There were no significant differences in deaths within the first 3 months after surgery when compared between groups stratified according to ASA score (p = 0.72).
The average age of patients who died was 81.1 (SD 6.4) while the average age of the living patient was a significantly lower 74.2 (SD 13.3) years (t = 2.44; df = 80.85; p = 0.001). Of the 24 deaths (23 %) during the first year, 18 were women. The incidence of deaths in the first 3 months was 16 of which 12 were women. Comparing the incidence of death by gender does not indicate a statistically significant difference (X2 = 0.311; df = 1; p = 0.58). The number of deaths in the first 6 months was significantly higher than in the next 6 months (p < 0.001). The average survival time was 10.1 months (95 % CI = 9.37-10.88) (Figure 1). Six patients died in the early postoperative period in the hospital and one from complications (infection) 9 months after surgery. There was no statistically significant difference in time from injury to surgery in patients who died and survived (Mann-Whitney; Z = -1.15; p = 0.25) (Figure 2). The ratio between patients with or without co-existent disease was 7:1. Of the 24 deaths, 19 patients (79.2 %) had comorbidities (p < 0.001).
Figure 1.
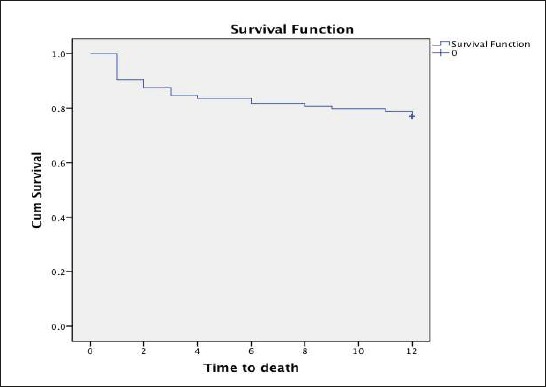
Kaplan-Meier curve depicting survival of patients in the postoperative period
Figure 2.
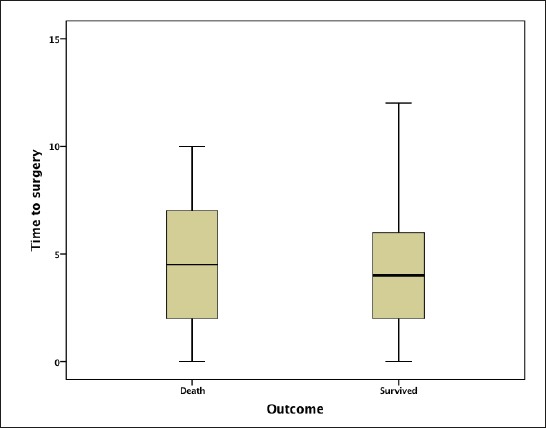
Comparison of the mean time from injury to surgery according to the survival of patients
The majority, 75 (66 %), were unstable fracture types; of these, 51 were A2 (46 %) and 24 were A3 (21 %). Dominant subgroups were A1.2 (26.5 %) and A2.3 (25.6 %). The reduction was good in 67 (61.4 %) of cases, acceptable in 24 (21.4 %) and poor in 19 (17.2 %) cases (three patients died postoperatively in the intensive care unit without control radiographs). Of the total number of deaths during the year, there were eight deaths associated with poor reduction and three with acceptable reductions. There was no statistically significant difference in the comparison of the incidence of death according to the postoperative quality of fracture reduction (X2 = 1.69; df = 1; p = 0.43). Two lateral greater trochanter fractures caused by insertion of the nail were observed intraoperatively. The proximal end of the nail penetrated the top of the trochanter in five patients. On average, each patient received 423.6 ml (range 0-2530 ml) of blood or blood products. The most blood, 2530 ml, was received by a patient with infection, revision surgery and non-union. The number of intraoperative radiation exposures was 63 (range 13-148). The average duration of surgery was 71.2 minutes (range 25-175 minutes).
The Cleveland zone 5 (centre-centre) was the most common placement of the tip of the blade on postoperative radiographs, accounting for 33 (29 %) of the cases. The second-most common location was zone 8, (central-inferior) with 24 (21 %) cases (Figure 3). Reoperation for the treatment of implant or fracture-related complications was required in four patients (infection, reimplantation and two extractions). There were two non-unions. Delayed healing was observed in six patients with poor reduction. Union with backing out blade were in three patients. Blade migration within the femoral head and telescoping of the blade along its axis was in one patient. Deep vein thrombosis developed in three patients diagnosed by phlebography, and were treated by the high dose of low-molecular-weight heparin. There were two deep and one superficial infection. Patients with deep infection died during the first year after surgery.
Figure 3.
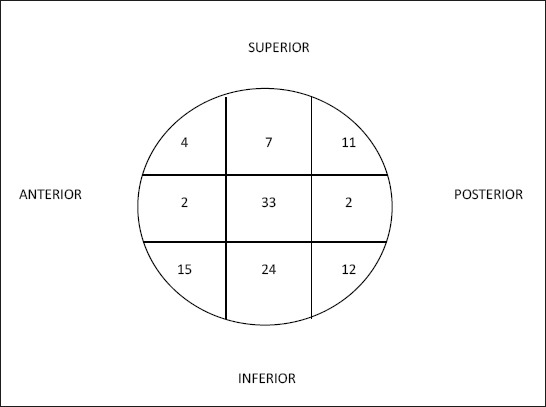
Cleveland index distribution
The mean TAD was 25.6 (SD 10.3) mm. TAD smaller than 25 mm was seen in 60 (53 %) patients. TAD larger than 20 mm was seen in 77 (69.2 %) patients (p < 0.001). There were four patients with cut-out. Cephalad cut-out occurred in three and axial cut-out (medial perforation) in one out of 110 cases. Three cut-out cases were in A3 unstable fracture types and one in type A1. The good reduction was seen in two of the cases and poor and acceptable in one case each. Two of the cephalad cut-outs had a TAD greater than 30 mm. The one axial cut-out occurred where the TAD was less than 15 mm (Figure 4).
Figure 4.
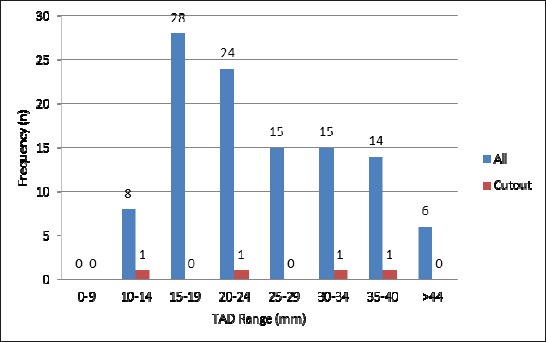
Distribution of TAD in cut-out and all cases
The pre-facture mean value NMS was 8.6 (SD 1.1) and the postoperative 4.3 (SD 3.6), which was significantly different (t = 13.005; df = 103; p < 0.001). A total of 26 patients (25 %) regained pre-fracture mobility status. Of the patients 28 (27 %) were unable to walk after surgery.
4. DISCUSSION
The general consensus in the literature is that the primary goal of treatment should be to obtain a stable fixation of the fracture that will allow early mobilization, restoring the function of the limb. Early operation was crucial for the good functional outcome and for the avoidance of serious postoperative complications for the implant or the patient (14, 16).
Moran et al. concluded that a delay in surgery of up to four days in patients without an acute medical comorbidity does not increase postoperative mortality, morbidity, or duration of the rehabilitation following (15). In our study, the time from fracture to surgery was on average 3.7 days. Siegmeth et al. (17) shows a significant increase in length of stay that was found in patients operated on after 48 hours when compared with those in the earlier group (21.6 vs. 32.5 days). In our study, the average length of hospital stay was 12.5 days. In the study by Takigami et al. (2), the length of the surgical procedure averaged 20.3 minutes (range 9-83 minutes). Intraoperative blood loss averaged 22.8 ml (range 5-100 ml). It would be wrong to conclude that, given the length of the surgical procedure, it is a simple procedure. In our study, the average duration of surgery was 73.1 minutes. On average, each patient received 423.6 ml of blood or blood products. Repeated reduction and manipulation will increase operative and fluoroscopy time and intraoperative blood loss, especially in more unstable fracture types (18). In our study, the reduction was good in 67 (60.9 %), acceptable in 24 (21.4 %) and poor in 19 (17.2 %) cases. In a study by Mereddy et al., fracture reduction was good in 41 (66.1 %) (6).
The rotation of the head might lead to a cutting out. The centre-centre position in the head of femur of any kind of lag screw or blade is to be achieved in order to minimize rotation of the femoral head and to prevent further mechanical complications (19). The first biomechanical study of a PFNA device suggests that the inferior position of the helical blade in the frontal plane and center position in the sagittal plane is superior to the centre-centre position and provides better biomechanical stability (20). Central-inferior and anterior-inferior positions, after adjustment for tip apex distance and screw position, were significantly protective against cut-out (24). Perfect placement of implants cannot always be achieved (17). Failed osteosynthesis has a major impact on mortality and morbidity among the elderly (21). The TAD was shown to be the most important predictive factor for cut-out, followed by screw position, fracture pattern, reduction and patient age. A significantly higher incidence of lag screw cut-out was associated with unstable fracture and older-age factors that cannot be controlled by the surgeon (22).
Palm et al. (23) study shows the influence of the performing surgeon’s experience and degree of supervision on the reoperation rate in technically demanding proximal femoral fractures. The 19.9 mm threshold thus proves to be a better predictor (although not significantly) than the 25 mm threshold. Poor fracture reduction also contributes to higher risks (up to five times higher) of screw cut-out (24). In our study, three cut-out cases were in unstable fracture types. Good reduction was recorded in two of the cases and poor and acceptable reduction in one case each. The technique guide for the Synthes PFNA suggests inserting the guide wire to 5–10 mm from subchondral bone on the AP and lateral views, which would yield a TAD of 10–20 mm (7). In the study by Nikoloski et al., there were six (6.2 %) cases of cut-out (25). They believe that the TAD rule of < 25 mm should not apply for the PFNA. They suggest avoiding a TAD < 20 mm due to possible axial cut-out and avoiding a TAD > 30 mm to avoid cephalad cut-out. In our study, 36 (32.7 %) patients had a TAD < 20 mm with one cut-out and 35 (31.8 %) ≥ 30 mm with two cut-out. Centre-centre or central-inferior position blade was not used in 53 (48.1 %) patients. A high percentage discrepancy from the desired position of the blade supports the good cut-out resistance of PFNA.
Subtle migration (2 mm) of the tip of the blade within the femoral head occurred in all fractures, but this did not preclude maintenance of reduction and fracture healing, and was not predicted by fracture type, reduction quality, age or gender. More telescoping occurred in unstable compared to stable fractures (26). In our study, union with backing out blade were in three patients. Blade migration within the femoral head and telescoping of the blade along its axis was in one patient. In a study from Strasbourg of 3066 patients, 1.5 % infection and 1.85 % cut-out was recorded (27). In our study, there were two deep and one superficial infection (2.6 %). Patients with deep infection died during the first year after surgery.
In our study the number of deaths in the first 6 months was significantly higher than in the next 6 months (p < 0.001). Of the 24 (23 %) deaths, 19 patients had comorbidities (p < 0.001). In van Balen et al. study (21), cumulative mortality was 20 % at 4 months after fracture. In our study, the pre-facture mean value NMS was 8.6 (SD 1.1) and postoperative 4.3 (SD 3.6). In a study by Kristensen et al. (28), 223 patients (80 %) achieved independence in basic mobility during their hospital stay, with 208 (93 %) regaining this independence within 2 weeks of surgery. Despite improvements in implant technology, operative technique, anesthesia and rehabilitation, the outcome for many patients with a hip fracture remains poor (29).
5. CONCLUSION
Even though this study shows the high level of mortality and morbidity associated with intertrochanteric fractures, we have suggested that PFNA offers advantages, as it can be easily inserted and provides stable fixation, which allows early mobilization of the patient. Therefore, early operation, good reposition, strict respect of technical steps and stable fixation will result in good functional recovery. The best position of the blade within the head is still unknown.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Norris R, Bhattacharjee D, Parker JM. Occurrence of secondary fracture around intramedullary nails used for trochanteric hip fractures: A systematic review of 13,568 patients. Injury. 2012;43(6):706–711. doi: 10.1016/j.injury.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 2.Anglen JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008;90(4):700–707. doi: 10.2106/JBJS.G.00517. [DOI] [PubMed] [Google Scholar]
- 3.Takigami I, Matsumoto K, Ohara A, Yamanaka K, Naganawa T, Ohashi M, et al. Treatment of trochanteric fractures with the PFNA (proximal femoral nail antirotation) nail system. Bull NYU Hosp Jt Dis. 2008;66(4):276–279. [PubMed] [Google Scholar]
- 4.Saudan M, Lübbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer P. Pertrochanteric fractures: is there an advantage to an intramedullary nail?: a randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma. 2002;16(6):386–393. doi: 10.1097/00005131-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Palm H, Krasheninnikoff M, Holck K, Lemser T, Foss NB, Jacobsen S, et al. A new algorithm for hip fracture surgery. Reoperation rate reduced from 18 % to 12 % in 2,000 consecutive patients followed for 1 year. Acta Orthop. 2012;83(1):26–30. doi: 10.3109/17453674.2011.652887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mereddy P, Kamath S, Ramakrishnan M, Malik H, Donnachi N. The AO/ASIF proximal femoral nail antirotation (PFNA): A new design for thetreatment of unstable proximal femoral fractures. Injury. 2009;40(4):428–432. doi: 10.1016/j.injury.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 7.Stratec Med. PFNA: Leading the way to optimal stability: Synthes. Original instruments andimplants of the Association for the Study of Internal Fixation. AO/ASIF. Technique guide. Stratec Medical. 2004:1–44. [Google Scholar]
- 8.Cleveland M, Thompson F, Wilson H, Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959;41:1399–1408. [PubMed] [Google Scholar]
- 9.Muller ME, Nazarian S, Koch P, Schatzker J. Berlin: Springer-Verlag; 1990. The Comprehensive Classification of Fractures of the Long Bones; pp. 116–121. [Google Scholar]
- 10.Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 11.American Society of Anesthesiologists. New classification of physical status. Anesthesiology. 1963;24:111–114. [Google Scholar]
- 12.Parker MJ, Palmer CR. Prediction of rehabilitation after hip fracture. Age Ageing. 1995;24:96–98. doi: 10.1093/ageing/24.2.96. [DOI] [PubMed] [Google Scholar]
- 13.Parker MJ, Palmer CR. A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br. 1993;75:797–798. doi: 10.1302/0301-620X.75B5.8376443. [DOI] [PubMed] [Google Scholar]
- 14.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States 2005-2025. J Bone Miner Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 15.Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87(3):483–489. doi: 10.2106/JBJS.D.01796. [DOI] [PubMed] [Google Scholar]
- 16.Efstathopoulos NE, Nikolaou VS, Lazarettos JT. Intramedullary fixation of intertrochanteric hip fractures: A comparison of two implant designs. Int Orthop. 2007;31(1):71–76. doi: 10.1007/s00264-006-0128-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87:1123–1126. doi: 10.1302/0301-620X.87B8.16357. [DOI] [PubMed] [Google Scholar]
- 18.Zhang S, Zhang K, Jia Y, Yu B, Feng W. InterTan Nail Versus Proximal Femoral Nail Antirotation-Asia in the Treatment of Unstable Trochanteric Fractures. Orthopedics. 2013;36(3):182–183. doi: 10.3928/01477447-20130222-16. [DOI] [PubMed] [Google Scholar]
- 19.Lenich A, Bachmeier S, Prantl L, Nerlich M, Hammer J, Mayr E, et al. Is the rotation of the femural head a potential initiation for cutting out? A theoretical and experimental approach. BMC Musculoskelet Disord. 2011;12:79. doi: 10.1186/1471-2474-12-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hwang HJ, Garg KA, Oh KJ, Oh WC, Lee JS, Rae MC, et al. A biomechanical evaluation of proximal femoral nail antirotation with respect to helical blade position in femoral head: A cadaveric study. Indian J Orthop. 2012;46(6):627–632. doi: 10.4103/0019-5413.104186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Balen R, Steyerberg EW, Polder JJ, Ribbers TL, Habbema JD, Cools HJ. Hip fracture in elderly patients: outcomes for function, quality of life, and type of residence. Clin Orthop Relat Res. 2001;390:232–243. [PubMed] [Google Scholar]
- 22.Hsueh KK, Fang KC, Chen MC, Su PY, Wu FH, Chiu YF. Risk factors in cutout of sliding hip screw in intertrochanteric fractures: an evaluation of 937 patients. Int Orthop. 2010;34(8):1273–1276. doi: 10.1007/s00264-009-0866-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Palm H, Jacobsen S, Krasheninnikoff M, Foss BN, Kehlet H, Gebuhr P. Influence of surgeon’s experience and supervision on re-operation rate after hip fracture surgery. Injury. 2007;38(7):775–779. doi: 10.1016/j.injury.2006.07.043. [DOI] [PubMed] [Google Scholar]
- 24.De Bruijn K, den Hartog D, Tuinebreijer W, Roukema G. Reliability of Predictors for Screw Cutout in Intertrochanteric Hip Fractures. J Bone Joint Surg Am. 2012;94(14):1266–1272. doi: 10.2106/JBJS.K.00357. [DOI] [PubMed] [Google Scholar]
- 25.Nikoloski NA, Osbrough LA, Yates JP. Should the tip-apex distance (TAD) rule be modified for the proximal femoral nail antirotation (PFNA)? A retrospective study. J Orthop Surg Res. 2013;8:35. doi: 10.1186/1749-799X-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gardner MJ, Briggs SM, Kopjar B, Helfet DL, Lorich DG. Radiographic outcomes of intertrochanteric hip fractures treated with the trochanteric fixation nail. Injury. 2007;38(10):1189–1196. doi: 10.1016/j.injury.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 27.Bojan JA, Biemel C, Speitling A, Taglang G, Ekholm C, Jönsson A. 3066 consecutive Gamma Nails 12 years experience at a single center. BMC Musculoskelet Disord. 2010;11:133. doi: 10.1186/1471-2474-11-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kristensen MT, Foss NB, Ekdahl C, Kehlet H. Prefracture functional level evaluated by the New Mobility Score predicts in-hospital outcome after hip fracture surgery. Acta Orthop. 2010;81:296–302. doi: 10.3109/17453674.2010.487240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Egol KA, Koval KJ, Zuckerman JD. Functional recovery following hip fracture in the elderly. J Orthop Trauma. 1997;11:594–599. doi: 10.1097/00005131-199711000-00009. [DOI] [PubMed] [Google Scholar]


