Abstract
Background:
Fatigue is a common symptom referred by many patients undergoing hemodialysis. Fatigue is associated with poor health-related quality of life (HRQoL) and is an important predictor for survival of hemodialysis patients.
Aim:
To assess the levels of fatigue and demographic factors affecting it among patients with End Stage Renal Disease undergoing hemodialysis.
Methods:
This quantitative study was carried out in two Dialysis Units of Hospitals in Athens Region. Between January 2015 and June 2015, 129 hemodialysis patients completed the Greek Version of the Fatigue Assessment Scale (FAS). Demographic data of patients was recorded. For the statistical analysis IBM SPSS Statistics version 20 was used.
Results:
The mean FAS score was 24.99. 49 patients (38.0%) were non fatigued, 61 patients (47.3%) were fatigued, and 19 patients (13.7%) were extremely fatigued. Higher levels of fatigue were reported among hemodialysis patients residing in urban areas, in those with low educational level and unemployed.
Conclusion:
The findings of this study can be used in the assessment of fatigue and early identification of high-risk patients (especially of the unemployed, those who occupy with domestic works, those with low educational level and of urban citizens). Use of this knowledge by hemodialysis nurses may lead to a better understanding of the factors of fatigue in ESRD, which in turn may lead to a more effective treatment.
Keywords: Fatigue, End Stage Renal Disease, Hemodialysis, Fatigue Assessment Scale
1. INTRODUCTION
Fatigue experienced by patients with End Stage Renal Disease (ESRD) undergoing hemodialysis (HD) is one of the daily problems in their life. Although dialysis is a procedure that saves lives, it cannot replace the function of healthy kidneys. Fatigue associated with HD significantly affects the quality of life of these patients (1-4). HD patients suffer from low levels of physical activity and decreased functional capacity while suffering from general muscle weakness resulting in a general feeling of fatigue (5). The significance of fatigue in ESRD is underlined by the fact that 94% of patients would prefer to undergo more dialysis sessions if there was the possibility to increase their energy level (6).
The incidence of fatigue in HD patients ranges from 60%–97% (7) while the level of fatigue of HD patients is one of the highest among chronic patients including cancer patients receiving chemotherapy (8), depressive patients (9) and patients with Systemic Lupus Erythematosus (10). HD patients have also many similarities to those suffering from chronic fatigue syndrome, since they present generalized weakness (11), decreased exercise tolerance (12) and sleep disorders (13).
The concept of fatigue in ESRD is difficult to be described. HD patients may express fatigue in different ways (weakness, lack of energy, and tiredness). Hardy & Studenski (14) refer two types of fatigue: mental (including emotional and cognitive) and physical (including insomnia, lack of energy and weakness).
The causes of fatigue in ESRD cannot be understood (15) but it seems that the correction of anemia (3) and physical activity (12, 16) actually improve the clinical situation of these patients. Despite improvements, it has been observed that the functional capacity of HD patients is not similar to that of the healthy population. A cause of reduced levels of physical activity are likely the HD procedure itself and, in particular, the duration of the session (4). Thirty three percent (33%) of HD patients reported that they feel bad the first few hours immediately after HD session while one in four indicate severe to very severe intensity of fatigue after the HD session (2). Identification of fatigue by HD nurses may be difficult since the recovery from this situation highly varies among patients (17). Moreover, the majority of HD patients complain of “nonspecific symptoms” which are assessed by health professionals as “irrelevant” to fatigue (18). Therefore, the diagnosis of fatigue is important in order to achieve early detection and treatment (17).
The aim of this study was to investigate the levels of fatigue as well as the demographic factors affecting fatigue among patients with End Stage Renal Disease undergoing hemodialysis.
2. MATERIALS AND METHODS
The study adopts an analytic study design. All 135 HD patients from 2 Hospital Units located in the broader area of Athens were asked to take part in this study. The inclusion criteria were: (a) age> 18 years, (b) undergoing hemodialysis for at least 6 months, (c) ability to write and read the Greek language fluently. The exclusion criteria were: (a) patients with history of mental illness (b) patients with serious mobility or eye problems. Finally, 129 patients met the above mentioned criteria. The study was conducted from January 2015 to June 2015.
Data were collected using anonymous questionnaires. Participants were given two questionnaires. The first questionnaire was related to the demographic characteristics of patients (gender, age, marital and employment status, educational level). The second questionnaire was the Greek version of the «Fatigue Assessment Scale (FAS)» (19). Specifically, FAS is a tool which collects information related to the perceived fatigue. The original form of FAS was constructed in 2003 by Michielsen et al (20) and consists of 10 questions. Furthermore, it has been used in Dutch (21) patients with sarcoidosis. It takes only two minutes to complete. The patients’ responses on 10 questions are summed in order to construct the score. The coding of responses is as follows. 1 = never, 2 = sometimes, 3 = regularly, 4 = often, 5 = always. Therefore, the score ranges between 10-50. Five questions are related to the physical fatigue and the other five to mental fatigue. Patients are categorized as “non-fatigued” if the FAS score is below 22, “fatigued” if the FAS score is higher or equal to 22 and “extremely fatigued” if the FAS score is higher or equal to 35. Psychometrics properties of Greek version have been tested and the internal consistency of the scale was found to be equal to 0.761 (19).
Firstly, the Hospitals Ethics Committees approved the study protocol. Patients, after informed about the purpose of the research, gave their written consent. Moreover, they were informed that their participation is voluntary. The anonymity of the participants was protected and the results obtained were used solely for the purposes of this research. Quantitative variables are presented as mean (± standard deviation) while qualitative variables are presented as frequencies and percentages. The internal consistency of the FAS scale was evaluated through Cronbach’s a coefficient. The effect of demographics on the indices was evaluated, where appropriate, through the parametric t test for two independent samples, the parametric ANOVA and the non-parametric methods of Mann-Whitney and Kruskal-Wallis. Results with p-value lower than 0.05 were considered as statistically significant. For the statistical analysis IBM SPSS Statistics version 20 (SPSS Inc., 2003, Chicago, USA) was used.
3. RESULTS
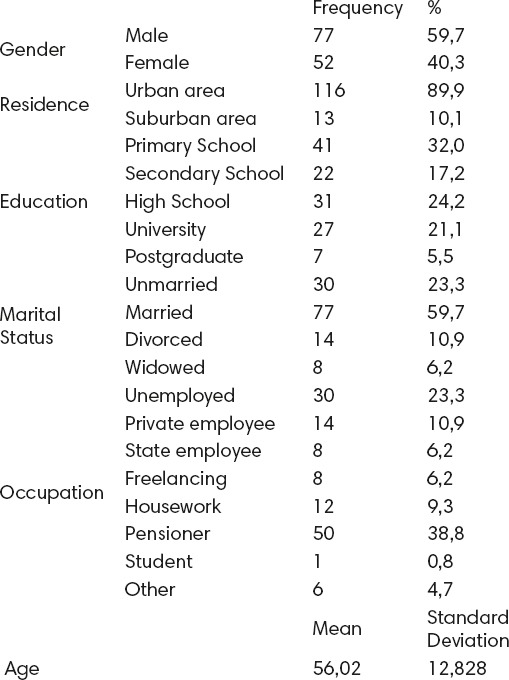
In this study, 129 hemodialysis patients participated. Of these patients 59.7% were males and 40.3% females. The mean of age was 56.02 (± 12,828) years. Descriptive characteristics of the sample are presented in Table 1.
Table 1.
Descriptive characteristics
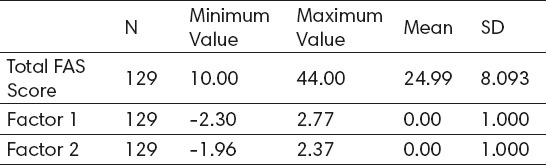
The responses of patients in questions are presented in Table 2. The Cronbach’s a coefficient, after the reversal of questions 4 and 10, was equal to 0.825, a value considered very satisfactory. Three fatigue indices were used: total FAS score (calculated as the sum of the 10 items after reversing questions 4 and 10), and the two factors (physical and mental fatigue). The descriptive data of the three indices are given in Table 3. The mean FAS score was 24.99. Forty nine (49) patients (38.0%) were non fatigue, 61 patients (47.3%) were fatigue, and 19 patients (13.7%) were extremely fatigue.
Table 2.
The Fatigue Assessment Scale
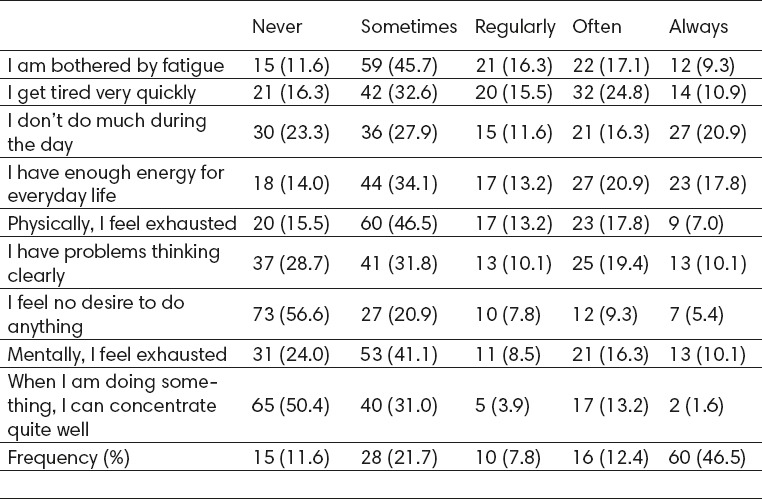
Table 3.
Descriptive characteristics of fatigue indicators
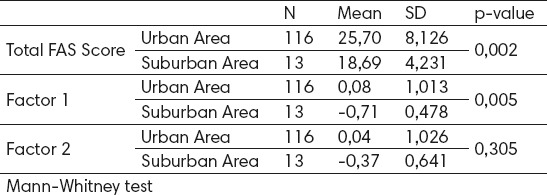
Statistical analysis revealed that none of the fatigue indices were statistically significantly correlated with the patient’s age. The gender did not affect significantly any of the three indices. Conversely, according to Table 4, we observe that the place of residence affected significantly both total FAS score (Mann-Whitney U = 354.0; p = 0.002) and factor 1 (Mann-Whitney U = 394.0; p = 0.005). HD patients residing in urban areas, showed higher values of total FAS score (mean: 25.70) compared to residents of suburban areas (mean: 18.69).
Table 4.
Influence of residence in fatigue indicators
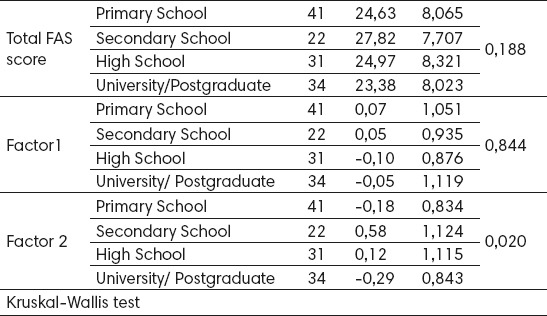
The educational level of patient affected only factor 2 (Kruskal-Wallis x2(3) = 9.863; p = 0.020). Specifically, high school graduates differed from University graduates or postgraduates (p = 0.017) (Table 5).
Table 5.
Influence of educational level in fatigue indicators
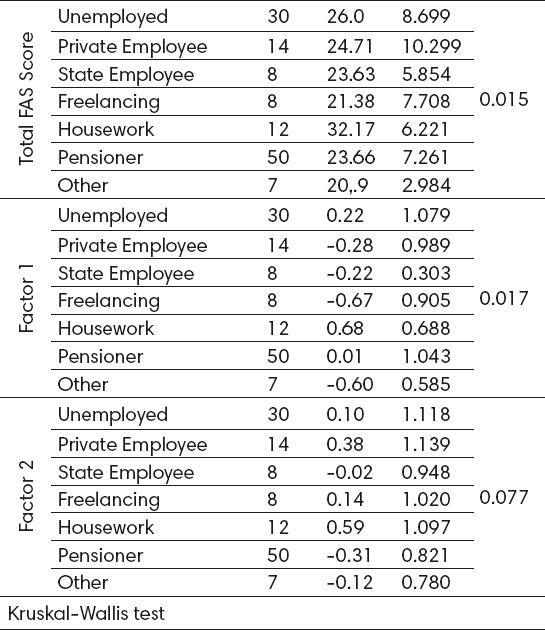
Regarding the profession, Table 6 shows that there was a statistically significant difference in total FAS score (x2(6) = 15.724; p = 0.015). Specifically, individuals who dealt with domestic tasks differed significantly from retired (p = 0.049) and those who did other profession (p = 0.038). Patients dealing with domestic tasks experienced higher total fatigue (mean: 32.17) than freelancers (mean: 21.38). Furthermore, a significant difference in factor 1 revealed according to the profession (x2(6) = 15.488; p = 0.017). Freelancers differed significantly from those who dealt with domestic tasks (p = 0.027). In contrast, the profession did not affect significantly factor 2 (x2(6) = 11.382; p = 0.077). Marital status did not affect significantly any of the three fatigue indices.
Table 6.
Influence of professional situation in fatigue indicators
4. DISCUSSION
This study was carried out in Athens region and aimed to assess the perceived fatigue among 129 hemodialysis patients. In this study, the Fatigue Assessment Scale was used for first time in Greek patients while it has been used among Croatian (22) patients with sarcoidosis and Dutch chronic heart failure patients (23).
The reliability and validity of the Greek Version’s scale has been tested (19). Although studies of De Vries et al (21) and Michielsen et al (22) demonstrated that FAS is a unidimensional scale, the factor analysis of the Greek version revealed two factors of fatigue–physical and mental. Although there is not an “ideal” tool for the assessment of fatigue–since fatigue is a subjective concept and difficult to be defined–there are reliable scales to measure it. Most of them are focused on patients with rheumatic diseases. The scale Brief Fatigue Inventory consists of 6 questions and studies the effect of patients’ fatigue on daily activities (24). The Fatigue Severity Scale was constructed to assess fatigue in patients with multiple sclerosis (25). The Multidimensional Assessment of Fatigue (MAF) Scale is a 10 point scale consisted of 16 multi-choice questions and has been used in patients with chronic diseases (26).
In conclusion, the above scales are merely a sampling of scales for measuring fatigue. The decision to use a particular one depends on the clinical specificity and disease as there is no suitable tool for a specific disease entity (16).
According to our study results, fatigue is an important feature in dialysis patients. The total score of fatigue in our sample was 24.99 (SD± 8.093). This value is higher than the value presented in the study of Croatian patients with sarcoidosis (mean fatigue: 24.2)(22) and in the study with Dutch workers (mean fatigue: 19.26) (20). In contrast, fatigue levels of Dutch and U.S.A. patients with sarcoidosis were higher (mean: 30.3 ± 8.1 and 27.1 ± 7.4 respectively) (27). The possible explanation of this difference is the symptom’s subjectivity.
Statistical analysis in our study revealed that the levels of fatigue in hemodialysis patients vary according to educational level, employment status and place of residence.
As far as the educational level is concerned, it seems that this has affected statistically significant factor 2 (mental fatigue) similar to many studies which have shown that people with low levels of education have a higher score on fatigue (22, 27, 28). In the study of Lerdal et al (29), 60.1% of patients felt tired while the lower the level of education, the higher was the level of fatigue. Therefore, patients with low educational level seem to face fatigue inadequately and experience fatigue to a greater extent. In addition, patients with a high level of education may face fatigue effectively (30).
The relationship between occupational status and fatigue level is clear in our study. Specifically, the unemployed and patients dealing with household recorded a higher overall fatigue index in relation to self-employed and civil servants. Staying at home may reduce the level of physical activity and social support from colleagues (31, 32, 33).
Searching the literature, there were no studies that correlate the level of fatigue with the place of residence in hemodialysis patients. In our study we found that the place of residence influences the level of fatigue since patients living in suburban areas noted lower indicator of overall fatigue and physical fatigue than those who live in the city center. This may be due to the extra time to dispose patients of heavy populated cities in order to be in time at the hemodialysis unit.
In this study, age did not seem to be significantly associated with fatigue. This finding is in agreement with other studies that have used FAS to assess fatigue, both in the general population and in patients (20, 21, 34, 35). In contrast, other studies (31, 36, 37) have shown that there is a positive correlation between age and fatigue level. This may be due to physiological changes that occur in elderly people and the psychosocial impact of a chronic disease on the individual (30).
Regarding the relationship of fatigue with gender, our study found that there was no statistically significant difference between the sexes. Another study found similar results (37) while in other searches (30, 38, 39) seems that women are more “tired” than men.
Limitations
The fact that the questionnaires were completed during the HD session, with the presence of physicians, nurses and other health professionals might have affected the objectivity of responses.
5. CONCLUSIONS
Based on the above, we conclude that the need for early identification and assessment of fatigue is vital for patients undergoing hemodialysis. The administration of erythropoietin and L-carnitine, physical and spiritual practice have been used successfully to relieve fatigue in patients undergoing hemodialysis (35). However, the complexity of fatigue’s pathogenesis and the lack of measurement tools, makes the effective intervention by dialysis nurses difficult (7). Therefore, health care professionals working in hemodialysis units and renal clinics should be vigilant in the detection of fatigue factors in order to help patients to develop coping and prevention strategies. Of particular importance is the identification of high-risk patients (especially of the unemployed, those who remain at home, those with low educational level and of urban citizens). Therefore, future studies should focus on identifying these factors as predictors of poor prognosis in ESRD. Since some studies (40-42) have already identified the importance of fatigue in terms of ESRD prognosis, it is also vital to identify possible mechanisms through which fatigue have toxic impact. It is not well known which interventions should focus on either physical fatigue, mental fatigue, or both. The therapeutic relationship between patient and health professionals and the involvement of patients in clinical decision making might help patients to develop coping strategies and self-management techniques (43). Hence, use of this knowledge by hemodialysis nurses may lead to a better understanding of the factors of fatigue in ESRD, which in turn may lead to a more effective treatment.
ACKNOWLEDGMENTS:
We kindly thank the Hospital Ethics Committees, patients and nursing personnel of Iatriko Therapeftirio Iliou and G.N.A. G. Gennimatas Hospital of Athens.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.ΜcCann K, Boore J R. Fatigue in persons with renal failure who require maintenance haemodialysis. J Adv Nurs. 2000;32:1132–1142. doi: 10.1046/j.1365-2648.2000.01584.x. [DOI] [PubMed] [Google Scholar]
- 2.Gordon P, Doyle J, Johansen K. Postdialysis fatigue is associated with sedentary behavior. Clin Nephrol. 2011;75:426–433. [PubMed] [Google Scholar]
- 3.Jhamb M, Pike F, Ramer S, Argyropoulos C, Steel J, Dew MA, et al. Impact of fatigue on outcomes in the hemodialysis (HEMO) study. Am J Nephrol. 2011;33:515–523. doi: 10.1159/000328004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caplin B, Kumar S, Davenport A. Patients’perspective of haemodialysis-associated symptoms. Nephrol Dial Transplant. 2011;26:2656–2663. doi: 10.1093/ndt/gfq763. [DOI] [PubMed] [Google Scholar]
- 5.Johansen KL, Painter P. Exercise in individuals with CKD. Am J Kidney Dis. 2012;59:126–134. doi: 10.1053/j.ajkd.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramkumar N, Beddhu S, Eggers P, Pappas LM, Cheung AK. Patient preferences for in-center intense hemodialysis. Hemodial Int. 2005;9:281–295. doi: 10.1111/j.1492-7535.2005.01143.x. [DOI] [PubMed] [Google Scholar]
- 7.Jhamb M, Argyropoulos C, Steel JL, Plantinga L, Wu AW, Fink N, et al. Correlates and Outcomes of Fatigue among Incident Dialysis Patients. Clin J Am SocNephrol. 2009;4:1779–1786. doi: 10.2215/CJN.00190109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adamsen L, Quist M, Andersen C, Møller T, Herrstedt J, Kronborg D, et al. Effect of a multimodal high intensity exercise intervention in cancer patients undergoing chemotherapy: A randomised controlled trial. BMJ. 2009;339:b3410. doi: 10.1136/bmj.b3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yatham LN, Lecrubier Y, Fieve RR, Davis KH, Harris SD, Krishnan AA. Quality of life in patients with bipolar I depression: data from 920 patients. Bipolar Disord. 2004;6:379–385. doi: 10.1111/j.1399-5618.2004.00134.x. [DOI] [PubMed] [Google Scholar]
- 10.Jolly M. How does quality of life of patients with systemic lupus erythematosus compare with that of other common chronic illnesses? J Rheumatol. 2005;32:1706–1708. [PubMed] [Google Scholar]
- 11.Johansen KL, Shubert T, Doyle J, Soher B, Sakkas G K, Kent-Braun JA. Muscle atrophy in patients receiving hemodialysis: effects on muscle strength, muscle quality, and physical function. Kidney Int. 2003;63:291–297. doi: 10.1046/j.1523-1755.2003.00704.x. [DOI] [PubMed] [Google Scholar]
- 12.Koufaki P, Mercer TH, Naish PF. Effects of exercise training on aerobic and functional capacity of end-stage renal disease patients. Clin Physiol Funct Imaging. 2002;22:115–124. doi: 10.1046/j.1365-2281.2002.00405.x. [DOI] [PubMed] [Google Scholar]
- 13.Sakkas GK, Gourgoulianis KI, Karatzaferi C, Liakopoulos V, Maridaki MD, Pastaka C. Haemodialysis patients with sleep apnoea syndrome experience increased central adiposity and altered muscular composition and functionality. Nephrol Dial Transplant. 2008;23:336–344. doi: 10.1093/ndt/gfm559. [DOI] [PubMed] [Google Scholar]
- 14.Hardy SE, Studenski SA. Qualities of fatigue and associated chronic conditions among older adults. J Pain Symptom Manage. 2010;39:1033–1042. doi: 10.1016/j.jpainsymman.2009.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johansen KL, Doyle J, Sakkas GK, Kent-Braun JA. Neural and metabolic mechanisms of excessive muscle fatigue in maintenance hemodialysis patients. Am J Physiol Regul Integr Comp Physiol. 2005;289:R805–R813. doi: 10.1152/ajpregu.00187.2005. [DOI] [PubMed] [Google Scholar]
- 16.Sakkas GK, Sargeant AJ, Mercer TH, Ball D, Koufaki P, Karatzaferi C, et al. Changes in muscle morphology in dialysis patients after 6 months of aerobic exercise training. Nephrol Dial Transplant. 2003;18:1854–1861. doi: 10.1093/ndt/gfg237. [DOI] [PubMed] [Google Scholar]
- 17.Lindsay RM, Heidenheim PA, Nesrallah G, Garg AX, Suri R. Minutes to recovery after a hemodialysis session: a simple health-related quality of life question that is reliable, valid, and sensitive to change. Clin J Am SocNephrol. 2006;1:952–959. doi: 10.2215/CJN.00040106. [DOI] [PubMed] [Google Scholar]
- 18.Sakkas G, Karatzaferi C. Hemodialysis fatigue: just “simple” fatigue or a syndrome on its own right? Front Physiol. 2012;31:306. doi: 10.3389/fphys.2012.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alikari V, Fradelos E, Sachlas A, Panoutsopoulos G, Lavdaniti M, Palla P, et al. Reliability and validity of the Greek version of «the Fatigue Assessment Scale». Archives of Hellenic Medicine. Article in press. [Google Scholar]
- 20.Michielsen HJ, De Vries J, Van Heck GL. Psychometric qualities of a brief self-rated fatigue measure: The Fatigue Assessment Scale. J Psychosom Res. 2003;54:345–352. doi: 10.1016/s0022-3999(02)00392-6. [DOI] [PubMed] [Google Scholar]
- 21.De Vries J, Michielsen H, Van Heck GL, Drent M. Measuring fatigue in sarcoidosis: the Fatigue Assessment Scale (FAS) Br J Health Psychol. 2004;9:279–291. doi: 10.1348/1359107041557048. [DOI] [PubMed] [Google Scholar]
- 22.Michielsen HJ, De Vries J, Drent M, Peros-Golubicic T. Psychometric qualities of the Fatigue Assessment Scale in Croatian sarcoidosis patients. Sarcoidosis Vasc Diffuse Lung Dis. 2005;22:133–138. [PubMed] [Google Scholar]
- 23.Smith OR, Michielsen HJ, Pelle AJ, Schiffer AA, Winter JB, Denollet J. Symptoms of fatigue in chronic heart failure patients: clinical and psychological predictors. Eur J Heart Fail. 2007;9:922–927. doi: 10.1016/j.ejheart.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 24.Mendoza TR, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, et al. The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer. 1999;85:1186–1196. doi: 10.1002/(sici)1097-0142(19990301)85:5<1186::aid-cncr24>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 25.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–1123. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 26.Belza BL. Comparison of self-reported fatigue in rheumatoid arthritis and controls. J Rheumatol. 1995;22:639–643. [PubMed] [Google Scholar]
- 27.De Kleijn WP, Elfferich MD, De Vries J, Jonker GJ, Lower EE, Baughman RP, et al. Fatigue in sarcoidosis: American versus Dutch patients. Sarcoidosis Vasc Diffuse Lung Dis. 2009;26:92–97. [PubMed] [Google Scholar]
- 28.Van Mens-Verhulst J, Bensing J. Distinguishing between chronic and nonchronic fatigue, the role of gender and age. Soc Sci Med. 1998;47:621–634. doi: 10.1016/s0277-9536(98)00116-6. [DOI] [PubMed] [Google Scholar]
- 29.Lerdal A, Celius EG, Moum T. Fatigue and its association with sociodemographic variables among multiple sclerosis patients. Mult Scler. 2003;9:509–514. doi: 10.1191/1352458503ms943oa. [DOI] [PubMed] [Google Scholar]
- 30.Mollaoglou M. Fatigue in people undergoing hemodialysis. Dialysis & Transplantation. 2009;29:216–220. [Google Scholar]
- 31.Liu HE. Fatigue and associated factors in hemodialysis patients in Taiwan. Res Nurs Health. 2006;29:40–50. doi: 10.1002/nur.20109. [DOI] [PubMed] [Google Scholar]
- 32.O’Sullivan D, McCarthy G. An exploration of the relationship between fatigue and physical functioning in patients with end stage renal disease receiving haemodialysis, Journal of Clinical Nursing. 2007;16:276–284. doi: 10.1111/j.1365-2702.2007.01965.x. [DOI] [PubMed] [Google Scholar]
- 33.Zyga S. Maintaining the identity and self-worth in patients with severe illness or injury. International Journal of Caring Sciences. 2012;5:1–2. [Google Scholar]
- 34.De Vries J, Van Der Sreeg A, Roukema J. Psychometric properties of the Fatigue Assessment Scale (FAS) in women with breast problems. Int J Clin Health Psychol. 2010;10:125–139. [Google Scholar]
- 35.De Vries J, Michielsen H, Van Heck Gl. Assessment of fatigue among working people: a comparison of six questionnaires. Occup Environ Med. 2003;60(Suppl 1):i10–i15. doi: 10.1136/oem.60.suppl_1.i10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Akin S, Mendi B, Ozturk B, Cinper C, Durna Z. Assessment of relationship between self-care and fatigue and loneliness in haemodialysis patients. J Clin Nurs. 2014;23:856–864. doi: 10.1111/jocn.12248. [DOI] [PubMed] [Google Scholar]
- 37.Letchmi S, Das S, Halim H, Zakariah FA, Hassan H, Mat S, Packiavathy R. Fatigue experienced by patients receiving maintenance dialysis in hemodialysis units. Nurs Health Sci. 2011;13:60–64. doi: 10.1111/j.1442-2018.2011.00579.x. [DOI] [PubMed] [Google Scholar]
- 38.Morsch CM, Gonclaves LF, Barros E. Health-related quality of life among haemodialysis patients - relationship with clinical indicators, morbidity and mortality. J Clin Nurs. 2006;15:498–504. doi: 10.1111/j.1365-2702.2006.01349.x. [DOI] [PubMed] [Google Scholar]
- 39.Bonner A, Caltabiano M, Berlund L. Quality of life, fatigue, and activity in Australians with chronic kidney disease: a longitudinal study. Nurs Health Sci. 2013;15:360–367. doi: 10.1111/nhs.12038. [DOI] [PubMed] [Google Scholar]
- 40.Horigan A, Rocchiccioli J, Trimm D. Dialysis and fatigue: implications for nurses-a case study analysis. Medsurg Nurs. 2012;21:158–163. [PMC free article] [PubMed] [Google Scholar]
- 41.Koyama H, Fukuda S, Shoji T, Inaba M, Tsujimoto Y, Tabata T, et al. Fatigue is a predictor for cardiovascular outcomes in patients undergoing hemodialysis. Clin J Am Soc Nephrol. 2010;5:659–666. doi: 10.2215/CJN.08151109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fukuda S, Koyama H, Kondo K, Fujii H, Hirayama Y, Tabata T, et al. Effects of nutritional supplementation on fatigue, and autonomic and immune dysfunction in patients with end-stage renal disease: a randomized, double-blind, placebo-controlled, multicenter trial. PLoS One. 2015;6(10(3)):e0119578. doi: 10.1371/journal.pone.0119578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fradelos EC, Tzavella F, Koukia E, Papathanasiou IV, Aikari V, Stathoulis, et al. Integrating chronic kidney disease patient’s spirituality in their care: health benefits and research perspectives. Mater Sociomed. 2015;27:354–358. doi: 10.5455/msm.2015.27.354-358. [DOI] [PMC free article] [PubMed] [Google Scholar]


