Abstract
Objective
The southern United States is highly affected by HIV, and community health centers play a key role in addressing the health-care needs of residents of southern cities. In 2012, Southside Medical Care Services (“Southside”) in Atlanta, Georgia, and Central Care Community Health Center (“Central Care”) in Houston, Texas, began comprehensive programs for routine HIV screening and linkage to HIV care.
Methods
We examined patient-level testing outcomes using medical record-derived data. We also compared the total number of HIV tests and HIV-positive tests in the most recent 12 months of the program with the number of HIV tests and HIV-positive tests during the 12 months prior to the program start.
Results
Southside saw 52,437 eligible patients from June 2012 through April 2014; 41,720 (80%) were offered an HIV test, 11,092 (27% of those offered a test) were tested, 75 (0.7% of those tested) had a positive result, and 74 (99% of those with a positive result) were linked to HIV care. Compared with the 12 months prior to the start of routine HIV screening implementation, Southside's routine HIV screening program conducted 5,955 more HIV tests (733% increase) and had 31 more patients who tested positive (238% increase).
Central Care saw 22,658 eligible patients from July 2012 to April 2014; 10,904 (48%) were offered an HIV test, 9,909 (91% of those offered a test) were tested, 52 (0.5% of those tested) had a positive result, and 41 (79% of those with a positive result) were linked to HIV care. Compared with the 12 months before routine HIV screening was implemented, Central Care's routine HIV screening program conducted 4,559 more HIV tests (618% increase) and had 36 more patients who tested positive (600% increase).
Conclusion
Southside and Central Care effectively implemented routine HIV screening programs that dramatically increased their testing volume while also linking the majority of HIV-positive patients to care. Other community health centers should consider similar programs.
The southern region of the United States is overrepresented in the national human immunodeficiency virus (HIV) epidemic.1,2 In 2010, southern states represented 37% of the U.S. population but more than 50% of those living with HIV infection. In 2011, nine of the 15 states with the largest numbers of new HIV diagnoses were in the South. Atlanta, Georgia, and Houston, Texas, ranked 8th and 12th in the nation, respectively, for the highest rates of new HIV diagnoses in 2011. It is estimated that more than 20,000 people are living with diagnosed HIV infection in Atlanta and Houston.2
The substantial geographic disparities in HIV infection are also intertwined with HIV infection disparities for African Americans and those of lower socioeconomic status.1 According to national estimates, only four out of five people who are infected with HIV have been diagnosed, and that number may be even lower among African Americans than for others.3 Even when diagnosed, African Americans may be less likely to receive life-saving HIV medical care than people of other races.4 Independent of these racial/ethnic disparities, people with low socioeconomic status in urban areas may also have a substantially higher prevalence of HIV infection than those with higher socioeconomic status.5
To address the national HIV epidemic and, particularly, these disparities, the Obama Administration issued the first-ever National HIV/AIDS Strategy in 2010.6 This strategy calls for reducing HIV incidence through increased access to medical care for people living with HIV and for reducing HIV-related health disparities. One means to achieving this goal is broader implementation of routine HIV screening in clinical settings. In 2006, the Centers for Disease Control and Prevention (CDC) recommended that all people aged 13–64 years should be offered routine, opt-out HIV screening during clinical visits.7 In 2013, the U.S. Preventive Services Task Force affirmed this recommendation with its Category A recommendation for routine HIV screening, thus paving the way for reimbursement of this screening by public health systems.8 Shortly thereafter, the U.S. Bureau of Primary Health Care released a new recommendation on the delivery of routine HIV screening at all federally qualified health centers (FQHCs) and added performance measures to evaluate implementation.9,10
Identifying the best approaches to conducting routine, opt-out HIV screening will ensure that the FQHC recommendation and national strategy goals are being met. Best approaches may be particularly important for FQHCs in southern U.S. cities, where HIV prevalence and poverty is high.2,11 In summer 2012, two southern FQHCs implemented new programs for routine HIV screening: Southside Medical Care Services (“Southside”) in Atlanta and Central Care Community Health Center (“Central Care”) in Houston. This article describes the Southside and Central Care programs and initial outcomes during a one-year period. These FQHCs were part of a larger collaborative, HIV on the Frontlines of Communities in the United States,12 which explores improved models to make HIV screening a routine part of health care.
METHODS
Southside Medical Center
Southside is a private, nonprofit FQHC in southeast Atlanta. Founded in 1967 by a coalition of civic leaders, federal health officials, and community representatives, Southside serves the medical needs of the medically underserved and impoverished communities in metropolitan Atlanta.
Of the total population in the geographic area near Southside, 24% live below 200% of the federal poverty level, and 16% are uninsured. Even within this area, Southside clients are overrepresented by those with fewer resources, with 56% earning incomes below the federal poverty level and 56% lacking health insurance. Southside serves 30,000 patients each year, the majority of whom are black (89%), female (68%), living below 200% of the federal poverty level (56%), and uninsured (56%).13 Southside employs some of Georgia's acquired immunodeficiency syndrome (AIDS) pioneers as thought leaders and actively engages in the local HIV planning processes that are part of the Ryan White Comprehensive AIDS Resources Emergency (CARE) Act.14 These relationships facilitate referrals, ensuring that Southside patients with HIV get speedy access to specialty care and support services. Before implementing routine, opt-out HIV screening for all patients in June 2012, Southside conducted routine HIV screening in the women's health clinic and conducted HIV risk assessments, testing, and counseling in the behavioral health clinic.
Central Care
Central Care is Houston's oldest FQHC, serving the southeast area of Houston since 1994. Central Care has approximately 20,000 patient encounters and more than 10,000 patients per year. The majority of those patients are black (85%), female (69%), living below 200% of the federal poverty level (54%), and uninsured (74%).15 Before implementing routine HIV screening in July 2012, Central Care provided risk-based HIV testing or testing on patient request.
Routine HIV screening processes
Southside.
During check-in, patients received an information sheet explaining routine, opt-out HIV screening. In the examination room, an alert in the electronic medical record (EMR) reminded the medical assistants and health-care provider to let the patient know about Southside's policy to conduct HIV screening with all patients unless they declined the test. The provider conducted the clinical assessment, confirmed contact information, explained the laboratory procedures, and reminded the patient to return for results. If the patient did not decline the test, a laboratory order was entered in the EMR and phlebotomists performed a blood draw. HIV testing using standard enzyme immunoassays (not rapid tests) was conducted in Southside's laboratory; results were entered into the EMR and returned to the patient within a week at a follow-up visit. When an abnormal result was detected, a Western blot confirmation was conducted. In addition to a prescheduled follow-up visit, all patients with abnormal test results, regardless of the type of test (e.g., cholesterol or HIV), were mailed a letter requesting them to come in for results. Results were not given by telephone. If the patient did not come in to receive the result within a week, the nursing staff then sent a certified letter, and clients were referred to the local health department.
Central Care.
Central Care designed an all-inclusive, general consent form for all treatment, including HIV testing. At initial check-in, the patient was orally informed about routine HIV screening. If the patient signed the general consent form, the EMR box for test acceptance was checked. The checked box triggered an EMR alert for the clinical team that this patient had consented. During the normal intake process, the triage nurse conducted a point-of-care, rapid HIV test. If the patient declined the original test offer, the EMR box for test decline was checked. The triage nurse would then offer the test again during the intake process in a more private setting and, if the patient accepted, would conduct the test. For the very few patients who declined this second offer, the provider conducting the examination would offer the test one final time. The provider relayed all rapid test results to patients before the end of the visit, and the results were documented in the EMR. For patients with a reactive rapid test, blood specimens were collected for confirmatory HIV testing at a commercial laboratory, one-week follow-up appointments were made to return confirmatory test results, and a case manager was assigned.
Systems changes to implement routine HIV screening
To fully implement routine HIV screening, Southside and Central Care had to make multiple key system changes. These changes were categorized as follows: change policy and involve leadership, modify EMRs, educate staff, and conduct continuous quality improvement.
Change policy and involve leadership.
At Southside, an organizational policy was created that made routine, opt-out HIV screening a standing order for all patients. Senior managers were critical to organizational acceptance of the policy change. They implemented the policy change by engaging providers, providing feedback on initial outcomes, and emphasizing the need to reach HIV testing goals to achieve Southside's overall mission. At Central Care, a policy was developed to offer HIV screening to all patients annually. This policy change required meetings with board members and providers to get their views on bringing a program of this magnitude into the organization and fundamentally changing the scope of service. Central Care's chief medical officer led these meetings.
Modify EMRs.
At Southside, an EMR upgrade allowed the creation of an HIV testing template that reminded providers to talk with the patient about HIV screening. The testing template default was set to automatically order an HIV test unless the provider documented that the patient declined. At Central Care, the existing EMR was modified to generate alerts in the EMR system for patients who were eligible for an HIV test offer. Staff members would get alerts every time the patient's chart was viewed, if the eligible patient was not tested. If the patient declined offers at previous visits, the alert was not deactivated, so as not to miss an opportunity to test if a patient changed his or her mind.
Educate staff.
Southside collaborated with the Southeast AIDS Training and Education Center to provide five staff trainings on HIV care and prevention. To educate staff members about the policy change to routine HIV screening, Southside leadership presented the policy and standing order at monthly staff meetings. When the “Order the Test” campaign was launched, staff members were given shirts, stickers, and instructions on routine HIV screening. The campaign's purpose was to educate and encourage staff members to implement the policy. To highlight the achievements in routine HIV screening, Southside identified a champion provider at each monthly staff meeting and gave that person a certificate and a free lunch. Central Care staff received training on EMR documentation, cultural sensitivity, HIV infection basics, conducting a rapid HIV test, and diagnosing and treating HIV infection. The type and depth of training depended on the staff member's role. Central Care also implemented the “Know Your Status” campaign to reinforce testing among patients and providers. As part of the campaign, staff members wore logo T-shirts that acted as reminders for clinicians to order HIV testing on all clients unless they decided to opt out.
Conduct continuous quality improvement.
At Southside, the number and proportion of eligible patients who had been tested were monitored at the provider level. These data were shared with providers during monthly staff meetings to encourage providers to test all eligible patients. At Central Care, monthly reports were generated to examine test offers among eligible patients seen by each provider. These reports were returned to providers during weekly webinars and monthly meetings with other staff members and those in leadership. When the number of test offers decreased, additional one-on-one education with staff members was implemented. This education frequently involved role-playing to help staff members better address patient confusion, questions, and fear of being tested.
Preparing to coordinate HIV care
Southside created a care team that included an HIV clinical coordinator, a patient navigator, and a care coordinator to help clients smoothly transition into care. Insured patients were treated in-house by their primary care provider, and uninsured patients were linked by the care team to a facility that provided Ryan White CARE Act services. The care team actively followed all patients (treated in-house or referred elsewhere) to monitor their care outcomes.
Central Care established in-house HIV care services for all clients. The only clients who were regularly referred to outside providers were those who were determined to be at high risk for not complying with treatment, had advanced into stage 3 HIV, or were pregnant. Central Care provided services to both insured and uninsured patients. During this study, Central Care was not receiving Ryan White CARE Act funding. Uninsured patients received help with applying for medication assistance through drug companies' patient-assistance programs and/or were referred to additional services through the county health department. To prepare for an increase in new HIV-infected patients after implementation of routine HIV screening, Central Care hired additional specialized staff, including patient care technicians, a case manager, and other providers. The primary medical care provider delivered most HIV care services at Central Care. Primary medical care providers and specialized HIV care providers at Central Care used the central EMR to coordinate patients' care.
Evaluation methods
Monitoring of routine HIV screening in FQHCs required continual review of, and action based upon, key outcome measures, such as the number/proportion of patients tested, the number/proportion of positive tests, and the number/proportion of positive patients linked to HIV care. Southside and Central Care tracked the number of patients who should have been offered an HIV test (i.e., those eligible), who were offered an HIV test, who were tested, and who tested positive. Patients aged 13–64 years who had not previously been diagnosed with HIV and did not have an HIV test documented in the EMR within the past year were eligible for an HIV test. Patients were considered to have been offered an HIV test if there was positive documentation in the EMR of the offer being made by at least one clinic staff member during the visit. Patients who visited the health centers multiple times during the year were eligible for and offered a test multiple times (e.g., if they declined a test at a previous visit), but they were not counted twice in the monitoring data.
HIV test results and linkage to care were also documented in the EMR. Linkage to care was defined as patients having kept their first HIV medical care appointment within 90 days of their HIV diagnosis, either by documentation of the actual visit (for patients receiving their HIV care at the FQHC) or in patient notes regarding referral appointments outside of the FQHC.
We also compared the number of HIV tests and HIV-positive test results in the most recent 12 months of the program (May 2013 through April 2014) with the 12-month period prior to the start of the program. We present numbers of HIV tests and HIV-positive tests by patient demographics. For demographic categories with 1–4 patients, we display data as <5 to prevent indirect identification of an individual.
RESULTS
Southside
Routine HIV screening for all patients at Southside began in June 2012. A total of 52,437 eligible patients were seen, 41,720 (80%) were offered an HIV test, and 11,092 (27% of those offered a test) were screened through April 2014 (Figure). As such, HIV screening was conducted among 21% of eligible patients. Among those screened, 75 (0.7%) were diagnosed with HIV infection, and 74 (99%) were linked to HIV care within 90 days of diagnosis.
Figure.
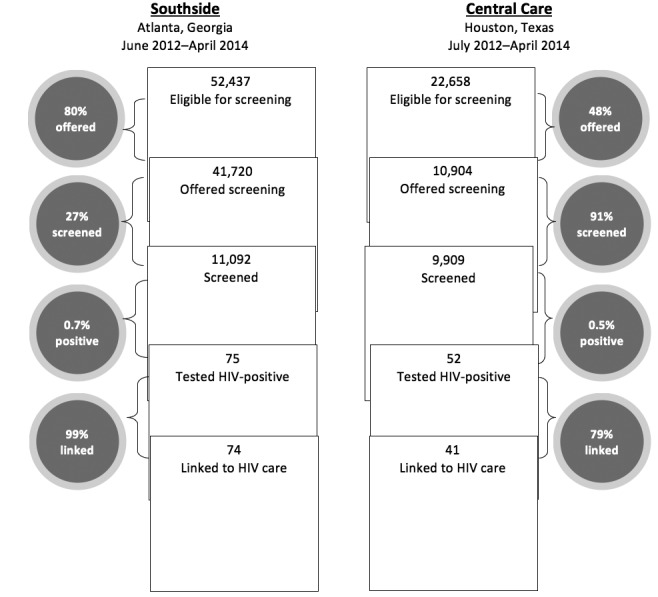
Outcomes of a routine HIV screening program at two southern federally qualified health centers, 2012–2014
The majority of patients who received an HIV test at Southside were female, aged 23–40 years, non-Hispanic, and black (Table 1). The majority of patients who tested positive for HIV at Southside were male, aged 31–50 years, non-Hispanic, and black. The highest proportions of positive tests were among patients who were male, aged 41–50 years, non-Hispanic, and black. In the 12-month period before implementation of routine HIV screening, Southside conducted 812 HIV tests, 13 (1.6%) of which were positive. In the most recent 12 months of the routine screening program, Southside conducted 6,767 HIV tests, 44 (0.7%) of which were positive (Table 2).
Table 1.
Demographic characteristics of patients tested for HIV in a routine HIV screening program in two southern federally qualified health centers, 2012–2014
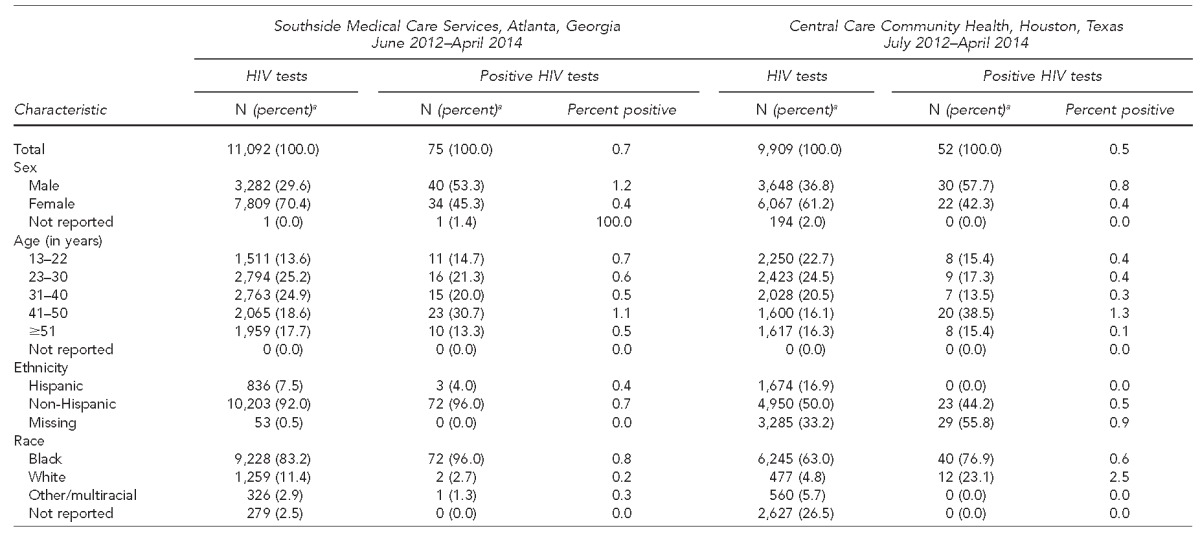
aPrecentages may not total to 100 due to rounding.
HIV = human immunodeficiency virus
Table 2.
Outcomes of previous HIV testing programs compared with routine HIV screening programs at two southern federally qualified health centers, 2012–2014
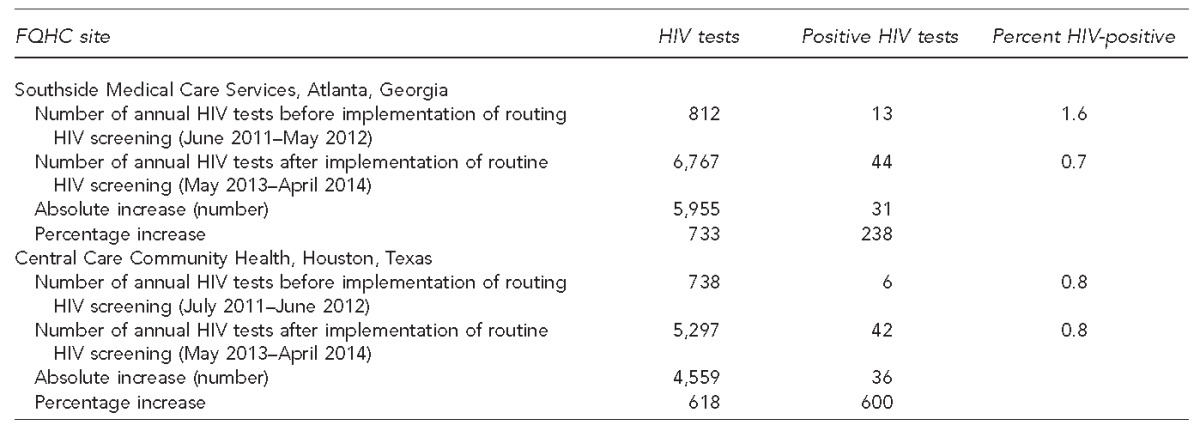
HIV = human immunodeficiency virus
FQHC = federally qualified health center
Central Care
Routine HIV screening for all patients at Central Care began in July 2012. A total of 22,658 eligible patients were seen, of which 10,904 (48%) were offered an HIV test and 9,909 (91% of those offered a test) were screened through April 2014 (Figure). Therefore, HIV screening was conducted among 44% of eligible patients. Among those screened, 52 (0.5%) were diagnosed with HIV infection, and 41 (79% of those diagnosed with HIV) were linked to HIV care within 90 days of diagnosis.
The majority of patients who received an HIV test at Central Care were female and aged 13–30 years (Table 1). The majority of those tested self-identified as non-Hispanic and black. The majority of patients who tested positive for HIV at Central Care were male, aged 41–50 years, and black. The highest proportions of positive tests were among patients who were male, aged 41–50 years, non-Hispanic, and white.
Central Care conducted 738 HIV tests, six (0.8%) of which were positive, in the 12-month period before implementation of routine HIV screening (Table 2). In the most recent 12 months of the routine HIV screening program, Central Care conducted 5,297 HIV tests, 42 (0.8%) of which were positive.
LESSONS LEARNED
These two southern FQHCs were able to effectively implement a routine HIV screening program using a comprehensive approach to policy change, leadership engagement, systems improvements, and ongoing training and promotion. The FQHCs were able to increase annual testing volume more than six-fold and diagnosed dozens more patients with HIV infection. Both FQHCs were also able to link the vast majority of these patients to HIV medical care within 90 days of diagnosis.
Several differences in the testing program outcomes between the two FQHCs are worth noting. Southside had a substantially larger eligible patient population and was able to offer testing to 78% of eligible patients, while Central Care offered HIV testing to 48% of eligible patients. This disparity in offers could have been due to variations in staff member/provider willingness to make or document the offer, or it could have been due to differences in the EMR process. Southside employed an EMR prompt that required staff members to enter either an “accept” or a “decline” for a test offer for each patient, whereas Central Care used EMR prompts as reminders, but did not require a response. Required responses in EMR templates, also known as “hardstops,” have been shown to increase staff compliance with institutions' care protocols,16,17 including for offers of HIV screening.16 The difference may also be reflected in the proportion of patients screened (Central Care screened 91% of patients offered vs. Southside's 27%), where a declined test would have been documented by Southside's EMR prompt after the offer but not entered at Central Care. It is also possible that the different testing approaches (Central Care used point-of-care, rapid HIV tests, and Southside used laboratory-based testing) may have resulted in different rates of testing among those who were offered a test.
Few previously published evaluations of routine HIV screening programs in FQHCs have been conducted.18,19 One of the more comprehensive evaluations was conducted with six southern FQHCs that had implemented routine HIV screening using rapid HIV tests shortly after the revised CDC screening recommendations.7,19 In that study, the clinics saw a similar increase in the volume of HIV screening and positive tests compared with our study, but substantially lower proportions of patients were offered testing (28%) compared with Southside and Central Care (80% and 48%, respectively). The changing health-care environment potentially makes it easier to get provider and patient buy-in on routine HIV screening.8,9 The improved outcomes may also reflect success in implementing a comprehensive approach to policy changes and developing new systems (e.g., EMRs with staff prompts and patient tracking) that better support routine HIV screening.
In the aforementioned study, the proportion of patients who were offered a test and then screened (67%) was higher than at Southside (27%) but lower than at Central Care (91%). Again, this variation in proportion of patients screened could be due to -variations in how offers were tracked in the two studies, but it could also be due to variations in test acceptance if rapid HIV tests were deemed more acceptable to patients. Although little research has compared patient acceptance of different types of HIV tests, one meta-analysis of adolescents' HIV testing preferences favored rapid tests over conventional tests.18 Patient test acceptance should be examined further in FQHCs.
The core mission of FQHCs is predicated on coordination of care services for their clients, but direct provision of HIV medical care may not be part of the services that FQHCs have historically provided in house. Optimizing HIV medical care is critical for many FQHC clients who may have reduced economic resources and other barriers to accessing care.19,20 To ensure the best outcomes for their patients, Southside and Central Care established improved mechanisms to get patients into HIV care. These mechanisms included adding care coordination staff and case managers, and managing HIV care in the context of primary medical care delivery. The success of these improvements was reflected in the near-complete linkage to care at Southside and 79% linkage to care at Central Care. Additional analyses are underway to examine the initial care outcomes (e.g., initiation of antiretroviral therapy and HIV viral suppression) of these patients.
Limitations
Several limitations to this evaluation should be noted. The patients who tested positive in this program may not have been newly diagnosed with HIV infection. Although Southside and Central Care determined screening eligibility based on not having had a previous HIV diagnosis noted within their own EMR system, a patient may have been diagnosed elsewhere and may not have disclosed this diagnosis when being screened. We were unable to consistently determine whether those who were offered a test but did not get one were not tested because they declined the test or because the test could not be administered (e.g., specimen could not be obtained, or the patient left before the test could be performed).
Additionally, a substantial number of Central Care patients were missing information on race/ethnicity. Because of the way monitoring data for this program were collected, we could not construct mutually exclusive racial/ethnic categories (e.g., non-Hispanic black), which could have helped to more clearly describe this issue. Central Care also conducted routine HIV screening at satellite sites in fall 2013. Although these sites followed all other Central Care routine screening procedures, they were not mandated to complete the race/ethnicity information normally required for FQHC client services.
Finally, although Southside and Central Care implemented very similar program components and collected standardized monitoring data, substantive differences in their approaches were not easily quantifiable, which may have limited our ability to draw definitive conclusions about the relative success of a program's approach. Such interpretations should be made with caution.
CONCLUSION
Southside and Central Care successfully implemented routine HIV screening programs. As FQHCs located in the center of the U.S. HIV epidemic, they are well positioned to continue to seek new ways to improve HIV screening, linkage to care, and, ultimately, care outcomes for patients. Other FQHCs should consider these experiences and develop their own improvements to fully integrate HIV screening into their programs.
Footnotes
This publication was supported by funding from Gilead Sciences, Inc. The programs described herein were also supported by funding from Gilead Sciences, Inc. The information used in this study was derived from data collected as part of the routine monitoring of the delivery of clinical services and does not constitute human subjects research.
REFERENCES
- 1.Sullivan PS. United States map of persons living with an HIV or AIDS diagnosis, 2012 [cited 2015 Aug 30] Available from: http://aidsvu.org/map.
- 2.Centers for Disease Control and Prevention (US) HIV Surveillance Report. Vol. 23. Atlanta: CDC; 2013. Diagnoses of HIV infection in the United States and dependent areas, 2011. Also available from: http://www.cdc.gov/hiv/pdf/statistics_2011_hiv_surveillance_report_vol_23.pdf [cited 2015 Jun 10] [Google Scholar]
- 3.Chen M, Rhodes PH, Hall HI, Kilmarx PH, Branson BM, Valleroy LA, et al. Prevalence of undiagnosed HIV infection among persons aged ≥13 years—National HIV Surveillance System, United States, 2005–2008. MMWR Morb Mortal Wkly Rep. 2012;61(2):57–64. [PubMed] [Google Scholar]
- 4.Hall HI, Frazier EL, Rhodes P, Holtgrave DR, Furlow-Parmley C, Tang T, et al. Differences in human immunodeficiency virus care and treatment among subpopulations in the United States. JAMA Intern Med. 2013;173:1337–44. doi: 10.1001/jamainternmed.2013.6841. [DOI] [PubMed] [Google Scholar]
- 5.Denning PH, DiNenno EA, Wiegand RE Division of HIV/AIDS Prevention; National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Characteristics associated with HIV infection among heterosexuals in urban areas with high AIDS prevalence—24 cities, United States, 2006–2007. MMWR Morb Mortal Wkly Rep. 2011;60(31):1045–9. [PubMed] [Google Scholar]
- 6.The White House (US), Office of National AIDS Policy. National HIV/AIDS strategy for the United States. 2010 [cited 2015 Jun 10] Available from: https://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf.
- 7.Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. [PubMed] [Google Scholar]
- 8.Moyer VA U.S. Preventive Services Task Force. Screening for HIV: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:51–60. doi: 10.7326/0003-4819-159-1-201307020-00645. [DOI] [PubMed] [Google Scholar]
- 9.Department of Health and Human Services (US), Health Resources and Services Administration. HIV testing in health centers: new recommendations [cited 2015 Jun 10] Available from: http://bphc.hrsa.gov/policiesregulations/policies/pdfs/pal201309.pdf.
- 10.Health Resources and Services Administration (US), Bureau of Primary Health Care. What is a health center? [cited 2015 Jun 10] Available from: http://bphc.hrsa.gov/about/what-is-a-health-center/index.html.
- 11.Bishaw A. American Community Survey Reports. Washington: Census Bureau (US); 2014. Changes in areas with concentrated poverty: 2000 to 2010. Also available from: https://www.census.gov/content/dam/census/library/publications/2014/acs/acs-27.pdf [cited 2015 Jun 10] [Google Scholar]
- 12.Sanchez TH, Sullivan PS, Rothman RE, Brown EH, Fitzpatrick LK, Wood AF, et al. A novel approach to realizing routine HIV screening and enhancing linkage to care in the United States: protocol of the FOCUS program and early results. JMIR Res Protoc. 2014;3:e39. doi: 10.2196/resprot.3378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Health Resources and Services Administration (US), Bureau of Primary Health Care. 2013 health center profile: Southside Medical Center, Inc. [cited 2015 Jun 10] Available from: http://bphc.hrsa.gov/uds/datacenter.aspx?q=d&bid=040400&state=GA&year=2013.
- 14. Pub. L. No. 111-87, 123 Stat. 2885 (Oct. 30, 2009)
- 15.Health Resources and Services Administration (US), Bureau of Primary Health Care. 2013 health center profile: South Central Houston Action Council, Inc. [cited 2015 Jun 10] Available from: http://bphc.hrsa.gov/uds/datacenter.aspx?q=d&bid=065800&state=TX&year=2013.
- 16.Schedlbauer A, Prasad V, Mulvaney C, Phansalkar S, Stanton W, Bates DW, et al. What evidence supports the use of computerized alerts and prompts to improve clinicians' prescribing behavior? J Am Med Inform Assoc. 2009;16:531–8. doi: 10.1197/jamia.M2910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vawdrey DK, Chang N, Compton A, Tiase V, Hripcsak G. Impact of electronic medication reconciliation at hospital admission on clinician workflow. AMIA Annu Symp Proc. 2010;2010:822–6. [PMC free article] [PubMed] [Google Scholar]
- 18.Weis KE, Liese AD, Hussey J, Coleman J, Powell P, Gibson JJ, et al. A routine HIV screening program in a South Carolina community health center in an area of low HIV prevalence. AIDS Patient Care STDS. 2009;23:251–8. doi: 10.1089/apc.2008.0167. [DOI] [PubMed] [Google Scholar]
- 19.Myers JJ, Modica C, Dufour MS, Bernstein C, McNamara K. Routine rapid HIV screening in six community health centers serving populations at risk [published erratum appears in J Gen Intern Med 2010;25:277] J Gen Intern Med. 2009;24:1269–74. doi: 10.1007/s11606-009-1070-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turner SD, Anderson K, Slater M, Quigley L, Dyck M, Guiang CB. Rapid point-of-care HIV testing in youth: a systematic review. J Adolesc Health. 2013;53:683–91. doi: 10.1016/j.jadohealth.2013.07.029. [DOI] [PubMed] [Google Scholar]


