Abstract
BACKGROUND
Diagnostic imaging is not recommended in the evaluation and management of non-specific acute low back pain.
OBJECTIVE
To estimate the variation among primary care providers (PCPs) in the use of diagnostic imaging for older patients with non-specific acute low back pain.
DESIGN AND PARTICIPANTS
Retrospective cohort study using 100 % Texas Medicare claims data. We identified 145,320 patients aged 66 years and older with non-specific acute low back pain during the period January 1, 2007, through November 30, 2011, cared for by 3297 PCPs.
MAIN MEASURES
We tracked whether each patient received lumbar imaging (radiography, computed tomography [CT], or magnetic resonance imaging [MRI]) within 4 weeks of the initial visit. Multilevel logistic regression models were used to estimate physician-level variation in imaging use.
KEY RESULTS
Among patients, 27.2 % received radiography and 11.1 % received CT or MRI within 4 weeks of the initial visit for low back pain. PCPs varied substantially in the use of imaging. The average rate of radiography within 4 weeks was 53.9 % for PCPs in the highest decile, compared to 6.1 % for PCPs in the lowest decile. The average rates of CT/MRI within 4 weeks were 18.5 % vs. 3.2 % for PCPs in the highest and lowest deciles, respectively. The specific physician seen by a patient accounted for 25 % of the variability in whether imaging was performed, while only 0.44 % of the variance was due to measured patient characteristics and 1.4 % to known physician characteristics. Use of imaging by individual physicians was stable over time.
CONCLUSIONS
PCPs vary substantially in the use of imaging for non-specific acute low back pain. Provider-level measures can be employed to provide feedback to physicians in an effort to modify imaging use.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-015-3475-3) contains supplementary material, which is available to authorized users.
KEY WORDS: back pain, care management, practice variation, primary care, quality assessment
INTRODUCTION
Acute low back pain is the second most common symptomatic reason for primary care visits in the United States, with an estimated annual prevalence of 15–20 % among adults.1 Only a small proportion of these patients have an identifiable underlying cause; for example, less than 2 % have disc herniation.2 Most patients improve within a month with conservative management and do not require immediate diagnostic testing.3,4 Randomized controlled trials have found no significant differences in clinical outcomes (pain, function, and quality of life) in patients with non-specific acute low back pain between those receiving immediate lumbar imaging (radiography, computed tomography [CT] or magnetic resonance imaging [MRI]) and those who receive usual clinical care without imaging.5–7
The lack of benefits is accompanied by potential harms. Imaging may detect abnormalities unrelated to the pain, leading to additional tests, interventions, and referrals that do not improve outcomes.8,9 Cumulative low-level radiation exposure is associated with an increased risk of cancer, with about 1,200 additional future cases of cancer anticipated for the 2.2 million lumbar CT scans performed annually in the US.10–12
Medical societies recommend against imaging for acute low back pain.13–20 Table 1 summarizes the current guidelines and recommendations. Imaging for low back pain is a target in the “Choosing Wisely” campaign to eliminate unnecessary tests and procedures.13 Physicians, however, continue to use imaging in this manner, despite guidelines and recommendations.21 One third of patients with acute low back pain receive imaging without a clinical indication, with 85 % of the imaging occurring within 28 days of the initial visit.22
Table 1.
Current Guidelines on the Use of Imaging for Patients with Acute Low Back Pain
| Organization | Guideline/Recommendation |
|---|---|
| American College of Physicians16,17 | Clinicians should not routinely obtain imaging or other diagnostic tests in patients with non-specific acute low back pain*† |
| American Pain Society17 | |
| American College of Radiology15 | Acute low back pain without red flags‡ is a benign, self-limiting condition that does not require imaging evaluation |
| American Academy of Family Physicians18 | Without clinical signs of serious pathology, diagnostic imaging is not indicated in patients with acute low back pain |
| American Chronic Pain Association20 | Do not routinely obtain imaging or other diagnostic tests in patients with non-specific low back pain |
| American Physical Therapy Association, the Orthopaedic Section19 | Routine ordering of imaging for low back pain should be discouraged. In particular, imaging in acute low back pain has not been shown to yield significant new findings or alter outcomes. |
* Acute low back pain is defined as low back pain present for fewer than 4 weeks
† Non-specific low back pain is defined as pain occurring primarily in the back, with no signs of a serious underlying condition (such as cancer, infection, or cauda equina syndrome), spinal stenosis or radiculopathy, or another specific spinal cause (such as vertebral compression fracture or ankylosing spondylitis). Degenerative changes on lumbar imaging are usually considered non-specific, as they correlate poorly with symptoms
‡ Red flags are defined as one of the following: 1) recent significant trauma or milder trauma at age > 50 years; 2) unexplained weight loss; 3) unexplained fever; 4) immunosuppression; 5) history of cancer or prior surgery; 6) intravenous drug use; 7) prolonged use of corticosteroids or osteoporosis; 8) age > 70 years; 9) focal neurologic deficit with progressive or disabling symptoms; and 10) duration longer than 6 weeks
A number of studies have shown that individual physician variation is a major determinant of whether a patient receives a test, independent of patient characteristics.23,24 This is especially the case when the test is not generally recommended in a given clinical presentation.25 Studies report that imaging use for low back pain varies by physician characteristics.22,26 To our knowledge, no data exist on variation among individual primary care physicians (PCPs) in obtaining imaging for patients with acute low back pain.
In the present study, we examined the use of imaging for acute low back pain and variability in use at the level of individual PCPs using Medicare claims data.
METHODS
The study was approved by the Institutional Review Board of the University of Texas Medical Branch.
Data Sources
We used 100 % Medicare claims data from Texas for January 1, 2006, through December 31, 2011. These include the Medicare Denominator File for demographic and enrollment information, the Carrier File for physician claims, the Outpatient Statistical Analysis File (OUTSAF) for outpatient claims, and the Medicare Provider Analysis and Review (MEDPAR) File for inpatient claims. Physician characteristics were extracted from the American Medical Association (AMA) Physician Masterfile, which were linked with Medicare claims data via the National Provider Identification (NPI) number.
Study Subjects
The overall approach was to identify older patients with non-specific acute low back pain during the period January 1, 2007, through November 30, 2011, and the PCPs who initially saw those patients. We employed an algorithm developed by the National Committee for Quality Assurance to identify non-specific acute low back pain.14 Medicare claims from January 1, 2006, through December 31, 2011, were included to ensure a 12-month look-back period and a 4-week follow-up period.
Specifically, we identified patients aged 66 years and older who had an outpatient claim for evaluation and management with a diagnosis of low back pain. We excluded cases with initial evaluation made in an emergency room. To ensure that we had complete patient claims from which to extract comorbidity and outcome variables, we included only patients with full coverage of Medicare Parts A and B and with no HMO coverage from 1 year before to 4 weeks after the diagnosis of low back pain (n = 1,118,453 episodes). Patients with claims with a diagnosis code for low back pain within the previous year were excluded. We also excluded those with “red flags” as indicators for imaging. These included any claims at the initial visit or in the previous year for trauma, cancer, intravenous drug use, or neurologic impairment14 (n = 388,511 episodes). Appendix 1 shows the algorithm used to identify episodes of non-specific acute low back pain. For patients with multiple episodes, we included the first episode only, leaving 293,333 patients.
Physicians who initially saw these patients were identified from the NPI number, and their specialties were identified from the Health Care Financing Administration (HCFA) specialty field. We included only PCPs in the present study (170,880 patients cared for by 7707 PCPs). To ensure reliable physician-level measures, we restricted analyses to PCPs with at least 20 patients with non-specific acute low back pain during the period 2007–2011, resulting in 145,320 patients (85 % of eligible patients), who saw 3297 PCPs (43 % of eligible PCPs).
Patient Characteristics
The Medicare Denominator File was used to extract information on patient age, sex, and race/ethnicity. Medicaid eligibility was measured using the state buy-in information in the Medicare Denominator File. The percentage of high school graduates in the patient’s ZIP Code area was obtained from US Census data. We categorized the patient’s county of residence as metro, non-metro, or rural, using US Department of Agriculture definitions.27 Comorbidity was assessed using the Charlson comorbidity index based on outpatient, inpatient, and carrier claims 1 year prior to the diagnosis of low back pain.28,29 For each patient, we also extracted the number of visits within the previous year to the physician who provided care for low back pain.
Physician Characteristics
Physician age, gender, board certification, years in practice, and medical school training in or outside the US were obtained from the AMA Physician Masterfile. PCPs’ specialties were obtained from the HCFA specialty field in the carrier files. Due to the small number of general practitioners (n = 59) and geriatricians (n = 16), we classified PCPs as either family medicine (combining family medicine and general practice) or internal medicine (combining general internal medicine and geriatrics).
Use of Diagnostic Imaging
We tracked each patient’s physician and outpatient claims to identify any lumbar or sacral spine imaging, including radiography, CT, or MRI, within 4 weeks of an initial visit for low back pain (Appendix 1). We then identified whether the physician who ordered the imaging was the same PCP who saw the patient at the initial visit.
Statistical Analysis
We summarized, in percentage statistics, (i) the overall percentage of patients who received imaging by any physician and (ii) the percentage of patients who received imaging by the same PCP as they saw at the initial visit. To focus on examining PCP-level imaging use, we restricted the outcome variable in the subsequent analyses to imaging ordered by the same PCP as seen at the initial visit. Descriptive analysis was used to summarize patient and physician characteristics and rates of imaging use. Our data have a two-level structure, with patients clustered within PCPs. Multilevel logistic regression modeling30 was used to generate PCP-level estimates on rates of imaging use, adjusting for patient characteristics and the clustering of patients within physicians. The average adjusted imaging rate derived from the multilevel model was used to identify physicians with imaging rates significantly higher or lower than average, at a significance level of 0.05.31 We then plotted the PCP-level adjusted rates of imaging, ranking from low to high.
We also evaluated the stability of the PCP-level profiling by comparing the imaging rates for each PCP in two periods (1/1/2007–6/30/2009 and 7/1/2009–12/31/2011), using the Spearman rank correlation. This analysis included only the 1142 PCPs with 20 or more patients with low back pain in each period.
SAS software version 9.2 (SAS Institute Inc., Cary, NC. USA) was used for the statistical analyses.
Sensitivity Analysis
We repeated the above-described analyses for another two cohorts. Given the variability in physician coding practice, we analyzed a cohort excluding patients with a red flag code within 30 days after the initial visit. The 127,226 patients in this cohort saw 2990 PCPs for acute low back pain in 2007–2011. Our study subjects were older adults. Older patients may receive imaging for suspicion of cancer.15 To test the impact of patient age, we also restricted the analyses to the 24,413 patients aged 66–69 years cared for by 1568 PCPs for acute low back pain.
RESULTS
Of 145,320 patients with non-specific acute low back pain, 27.2 % received radiography and 11.1 % received CT/MRI within 4 weeks of the initial visit. The proportion of patients receiving imaging from the same PCP seen at the initial visit was 23.6 % for radiography and 8.1 % for CT/MRI.
Table 2 presents the percentage of patients who received imaging within 4 weeks from the same PCP as was seen at the initial visit, stratified by patient characteristics. Also shown are the odds ratios generated from multilevel logistic regression modeling, adjusted for patient characteristics and the clustering of patients within physicians. Older age and less frequent visits to the PCP in the prior year were associated with a higher likelihood of receiving radiography. Factors associated with higher likelihood of receiving CT/MRI include younger age, male gender, non-Hispanic white race, fewer comorbidities, ineligibility for Medicaid, and greater number of visits to the PCP in the prior year.
Table 2.
Use of Imaging Within 4 Weeks of the Initial Visit for Patients with Acute Low Back Pain, by Patient Characteristics
| Patient characteristics | Number of patients | Received radiography | Received CT/MRI | ||
|---|---|---|---|---|---|
| Percentage (%) | Adjusted OR (95 % CI)* | Percentage (%) | Adjusted OR (95 % CI)* | ||
| All | 145,320 | 23.55 | 8.10 | ||
| Age (years) | |||||
| 66–69 | 37,517 | 21.33 | Reference | 8.49 | Reference |
| 70–74 | 37,807 | 22.47 | 1.08 (1.04–1.12) | 8.36 | 0.96 (0.91–1.01) |
| 75–79 | 30,336 | 24.54 | 1.22 (1.17–1.27) | 8.58 | 0.98 (0.92–1.03) |
| 80–84 | 22,448 | 25.77 | 1.31 (1.26–1.37) | 7.86 | 0.87 (0.82–0.93) |
| ≥ 85 | 17,212 | 26.15 | 1.34 (1.28–1.41) | 6.14 | 0.67 (0.62–0.72) |
| Sex | |||||
| Female | 95,004 | 23.81 | Reference | 7.80 | Reference |
| Male | 50,316 | 23.07 | 0.98 (0.95–1.01) | 8.65 | 1.11 (1.07–1.16) |
| Race | |||||
| Non-Hispanic white | 102,448 | 24.33 | Reference | 8.93 | Reference |
| Non-Hispanic black | 9132 | 21.46 | 0.91 (0.86–0.97) | 6.08 | 0.76 (0.69–0.83) |
| Hispanic | 28,875 | 22.61 | 1.02 (0.97–1.07) | 6.37 | 0.82 (0.77–0.89) |
| Other/unknown | 4865 | 16.59 | 1.01 (0.91–1.11) | 4.50 | 0.75 (0.64–0.87) |
| Comorbidity score | |||||
| 0 | 86,300 | 23.80 | Reference | 8.31 | Reference |
| 1 | 35,076 | 23.24 | 1.00 (0.97–1.03) | 8.10 | 0.97 (0.92–1.02) |
| 2 | 13,185 | 23.62 | 1.02 (0.97–1.07) | 7.69 | 0.96 (0.90–1.04) |
| ≥3 | 10,759 | 22.50 | 0.98 (0.93–1.04) | 6.87 | 0.85 (0.78–0.93) |
| Percentage of patients in ZIP Code area with high school education | |||||
| Q1 (≤72 %) | 38,103 | 23.79 | Reference | 6.96 | Reference |
| Q2 (73–81 %) | 37,129 | 23.65 | 1.02 (0.97–1.07) | 8.71 | 1.03 (0.96–1.10) |
| Q3 (82–89 %) | 35,040 | 23.82 | 1.01 (0.96–1.06) | 8.45 | 1.02 (0.95–1.09) |
| Q4 (≥90 %) | 35,048 | 23.05 | 1.03 (0.98–1.08) | 8.26 | 1.02 (0.95–1.09) |
| Medicaid eligibility | |||||
| Yes | 27,511 | 21.02 | Reference | 5.62 | Reference |
| No | 117,809 | 24.14 | 1.05 (1.00–1.09) | 8.67 | 1.27 (1.19–1.36) |
| Urban/Rural | |||||
| Rural | 2224 | 21.22 | Reference | 8.05 | Reference |
| Metro | 114,580 | 23.66 | 1.12 (0.99–1.27) | 7.79 | 0.96 (0.81–1.15) |
| Non-metro | 28,516 | 23.31 | 1.07 (0.94–1.21) | 9.32 | 1.11 (0.93–1.33) |
| Number of physician visits in prior year | |||||
| 0 | 26,967 | 24.83 | Reference | 7.59 | Reference |
| 1 | 18,269 | 24.04 | 0.92 (0.88–0.97) | 7.75 | 1.03 (0.95–1.11) |
| 2 | 20,629 | 24.25 | 0.95 (0.91–1.00) | 8.25 | 1.11 (1.03–1.20) |
| 3 or more | 79,455 | 22.83 | 0.89 (0.85–0.93) | 8.31 | 1.20 (1.13–1.27) |
*Estimated from a multilevel model with patient characteristics but without specific physician characteristics. The multilevel model adjusted for the clustering of patients within providers
Table 3 shows the percentage of patients who received imaging within 4 weeks, stratified by PCP characteristic. Unadjusted rates are presented, along with adjusted odds ratios generated from multilevel logistic regression modeling. Patients were more likely to receive radiography or CT/MRI if the PCP was trained in the US, was board-certified, had more years in practice, and had a higher volume of Medicare patients. PCPs in family medicine were more likely to order radiography but less likely to order CT/MRI. The intraclass correlation coefficient was 0.251 based on a random intercept-only model for imaging within 4 weeks, implying that 25.1 % of the variation in whether a patient received imaging was attributable to variation among physicians. In contrast, only 0.44 % of the variation was explained by known patient characteristics and 1.41 % by known physician characteristics.
Table 3.
Use of Imaging Within 4 Weeks of the Initial Visit for Patients with Acute Low Back Pain, by Primary Care Physician Characteristics
| Physician characteristics | Number of physicians | Number of patients | Radiography | CT/MRI | ||
|---|---|---|---|---|---|---|
| Patients receiving radiography (%) | Adjusted OR (95 % CI)* | Patients receiving CT/MRI (%) | Adjusted OR (95 % CI)* | |||
| All | 3297 | 145,320 | 23.55 | 8.10 | ||
| Specialty | ||||||
| Internal medicine | 1435 | 67,867 | 22.71 | Reference | 8.58 | Reference |
| Family practice | 1862 | 77,453 | 24.29 | 1.08 (1.01–1.17) | 7.67 | 0.87 (0.81–0.94) |
| Gender | ||||||
| Male | 2711 | 123,751 | 23.56 | Reference | 8.25 | Reference |
| Female | 586 | 21,569 | 23.52 | 1.06 (0.97–1.17) | 7.24 | 0.90 (0.82–1.00) |
| Years in practice | ||||||
| Q1 (≤14 years) | 899 | 35,566 | 22.30 | Reference | 7.93 | Reference |
| Q2 (15–22 years) | 844 | 37,459 | 23.99 | 1.07 (0.97–1.18) | 8.14 | 1.04 (0.94–1.15) |
| Q3 (23–29 years) | 743 | 35,454 | 23.52 | 1.02 (0.92–1.13) | 8.01 | 1.00 (0.90–1.11) |
| Q4 (≥30 years) | 811 | 36,841 | 24.35 | 1.12 (1.01–1.24) | 8.30 | 1.08 (0.98–1.20) |
| US-trained | ||||||
| Yes | 2458 | 104,765 | 4.12 | Reference | 8.42 | Reference |
| No | 839 | 40,555 | 22.10 | 0.89 (0.82–0.97) | 7.27 | 0.78 (0.72–0.85) |
| Board certification | ||||||
| Yes | 2558 | 113,605 | 23.83 | Reference | 8.20 | Reference |
| No | 739 | 31,715 | 22.55 | 0.88 (0.81–0.96) | 7.73 | 0.94 (0.81–0.94) |
| Volume of Medicare patients | ||||||
| Q1 (≤276) | 815 | 24,100 | 23.06 | Reference | 6.90 | Reference |
| Q2 (267–394) | 821 | 28,882 | 23.06 | 0.99 (0.89–1.10) | 7.36 | 1.06 (0.95–1.18) |
| Q3 (395–565) | 826 | 36,555 | 23.92 | 1.05 (0.95–1.16) | 8.64 | 1.24 (1.11–1.37) |
| Q4 (≥566) | 835 | 55,783 | 23.76 | 1.06 (0.96–1.18) | 8.61 | 1.26 (1.13–1.40) |
*Estimated from a multilevel model with both patient and physician characteristics. All characteristics listed in Table 2 were adjusted for in this analysis
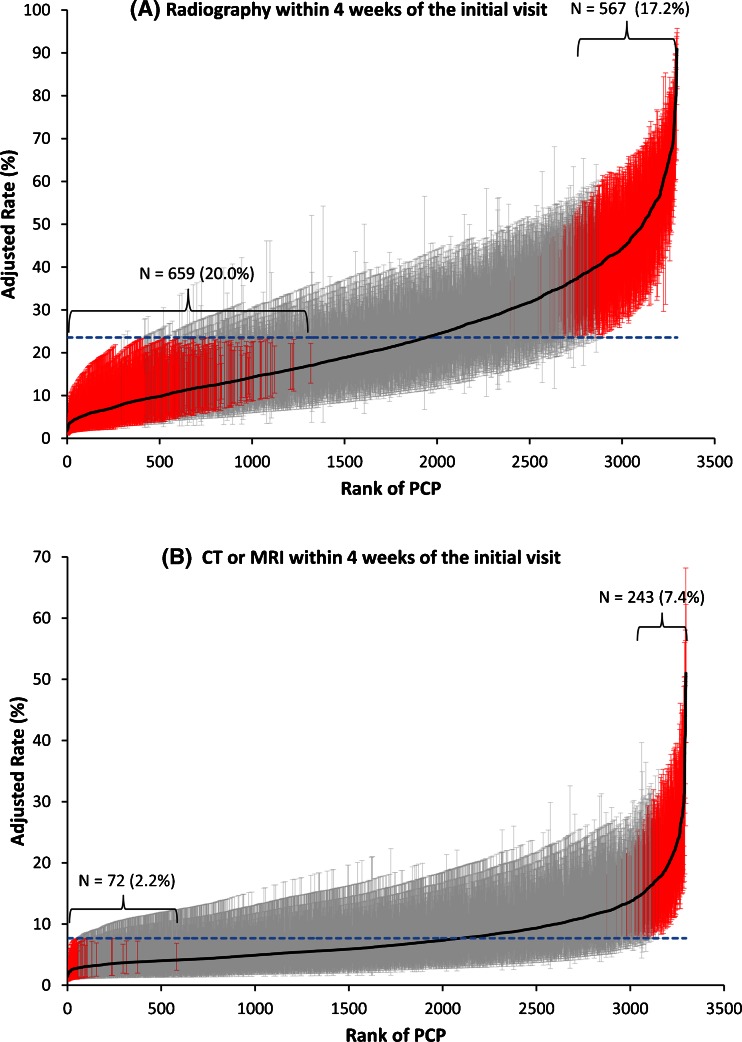
Figure 1(A) presents a cumulative distribution of rates for each PCP in obtaining radiography within 4 weeks of the initial visit, adjusted for patient characteristics. The average rate of radiography use at the physician level was 23.6 %. Among the 3297 physicians, 659 (20.0 %) had significantly lower rates and 567 (17.2 %) had significantly higher rates than the average. There was a ninefold difference in the average rate for physicians in the highest versus lowest deciles (53.9 % vs. 6.1 %). With an intraclass correlation coefficient of 0.25 and ≥ 20 patients per physician, the reliability of physician-level estimates is ≥ 0.87.
Figure 1.
Variation among 3297 primary care physicians (PCPs) in rates of imaging use within 4 weeks of an initial visit for non-specific acute low back pain. Adjusted rates (solid black line) and 95 % confidence intervals (vertical lines around the solid black line) for each PCP are shown. Estimates were adjusted for patient characteristics and clustering of patients within physicians using multilevel logistic regression modeling. PCPs were ranked from 1 to 3297 (horizontal axis) according to their adjusted rates of imaging use (vertical axis), with a rank of 1 indicating lowest use and 3297 indicating highest use. Outlier PCPs with adjusted rates significantly different from the average rate (horizontal blue dashed line) are indicated in red.
Figure 1(B) illustrates the variation among PCPs in ordering a low-back CT/MRI within 4 weeks of the initial visit, adjusted for patient characteristics. The average rate at the physician-level was 7.7 %. Among the 3297 physicians, only 72 (2.2 %) had significant lower and 243 (7.4 %) had significant higher rates than the average. The average rate was 18.5 % for physicians in the highest decile, compared to 3.2 % for physicians in the lowest decile.
We also examined stability over time in the PCP rates of obtaining imaging, comparing rates for two periods (1/1/2007–6/30/2009 vs. 7/1/2009–12/31/2011). Of the physicians ranked in the lowest quartile in the first period, over 75 % (83.5 % for radiography and 75.3 % for CT/MRI) were ranked in the lowest two quartiles in the second period. Of physicians ranked in the highest quartile in the first period, over 70 % (79.3 % for radiography and 70.2 % for CT/MRI) were ranked in the highest two quartiles in the second period. The Spearman rank correlation between the PCP rates for the two periods were highly correlated (r = 0.72 and 0.51 for radiography and CT/MRI, respectively).
Compared to the primary analysis, the sensitivity analysis had slightly lower imaging rates. For the cohort excluding patients with a red flag code within 30 days after the initial visit, 25.6 % received radiography and 9.6 % received CT/MRI within 4 weeks of the initial visit. For the cohort of patients aged 66–69 years, 23.6 % received radiography and 10.3 % received CT/MRI within 4 weeks of the initial visit. Sensitivity analysis revealed the same patient and physician characteristics associated with imaging use as in the primary analysis. The substantial variation among PCPs (intraclass correlation coefficients = 0.26 and 0.25) and the high correlation between PCP-level rates for the two time periods (r = 0.70 and 0.60, respectively) were also similar to those in the primary analysis.
DISCUSSION
Among Texas Medicare patients with non-specific acute low back pain during the period 2007–2011, almost one-third received radiography and 11 % received CT or MRI within 4 weeks of the initial visit. A national sample of Medicare claims data for 2000–2005 yielded similar rates.22 Imaging for patients with acute low back pain without a “red flag” indicates potential overuse, and should be avoided.14,22
We found substantial variation among PCPs in imaging for older patients with acute low back pain, with between-physician variation accounting for 25.1 % of total variation. This degree of variability is consistent with the concept of preference-based rather than evidence-based practice as described by Wennberg and colleagues.25 A recent study found a growing gap between guideline recommendations and actual clinical management of back pain.32 Doctors with financial ties to MRI scanner businesses tend to refer more patients for imaging,33 but we were unable to examine this association in our analysis. Nevertheless, design and use of provider performance measures is an important strategy for curbing the influence of such financial ties and to promote high-value, cost-conscious care.34
Initial enthusiasm about physician-level quality measures has been tempered by several concerns, including the reliability of these measures and their stability over time.35,36 For many quality measures, provider variation is low, with intraclass correlation coefficients of <0.10.35,37 This in turn leads to low reliability of provider performance estimates, unless the number of patients per provider is larger than is feasible for most measures. However, the high physician variability in early imaging for acute low back pain allows for generation of estimates with reliability of >0.80 for physicians with at least 20 such patients. Also, the majority of top and low performers in one period were also top and low performers in the subsequent period. Our study suggests that it is feasible to generate provider-level estimates of imaging use with high reliability and stability. Such measures can then provide feedback to physicians to modify overuse.
The Healthcare Effectiveness Data and Information Set quality measures, most derived from administrative claims data, are widely used to compare performance across health plans. Physician-level measures can be similarly employed. One barrier to quality improvement is that physicians are generally unaware of their quality relative to their peers. Feedback raises awareness and motivates physician to improve. A meta-analysis found that physician feedback is more effective when provided frequently, in writing, with an explicit action plan, and tied to incentives or accountability.38 Future studies are needed to translate our proposed physician measures of imaging for low back pain into plans for actual interventions and then to assess the effectiveness of such interventions.
One should not assume that the percentage of patients with low back pain receiving imaging should ideally be zero. Several considerations might lead a physician to order such imaging; not all can be captured in Medicare billing data. Instead, our assumption is that the percentage of patients for whom such considerations are relevant is relatively low, and that these cases should average out among PCPs. It is improbable that patients with acute complex low back pain would cluster within individual PCPs. The focus is on performance relative to other PCPs rather than on the absolute percentage of patients who undergo imaging.
Compared to the large between-physician variation, the variance explained by measured patient and physician characteristics was minimal (<2 %). Of note, the risk of receiving CT/MRI was higher for younger, healthier patients. Physicians with more years in practice were more likely to order imaging. This finding resonates with the call for continuing medical education targeting older physicians.39
Our study has several limitations. First, physician coding practice varies. Indications for imaging may appear after the index visit. We conducted sensitivity analysis by excluding patients with a red flag code within 30 days after the initial visit; the high variation among PCPs remained. Second, the study included older patients. Our sensitivity analysis in patients aged 66–69 years can partially mitigate concerns with the effect of age. Nevertheless, studies including younger patients are needed to confirm our findings. Moreover, administrative claims data cannot capture patient preference. Physicians may order imaging at the patient’s request in order to increase patient satisfaction.40 We also could not completely exclude patients with certain red flags (e.g., weight loss or remote history of cancer) using administrative claims data. However, these cases should average out among PCPs, and were unlikely to explain the marked variation among PCPs in imaging use. The present study focused on PCPs. Higher rates of imaging use, especially CT/MRI for acute low back pain, have been reported for specialists.23 Nevertheless, restricting the analyses to PCPs with >20 patients captured 85 % of Medicare patients with non-specific acute low back pain in the primary care setting. Another limitation is that our findings may be not generalizable to regions outside Texas, given differences in population composition and healthcare utilization patterns.41 Nevertheless, our estimated imaging rates are comparable to those from the national data.22 Future studies in other geographic regions are needed.
In conclusion, despite guideline recommendations, a substantial proportion of patients with acute low back pain receive imaging. The use of imaging varied greatly among PCPs, and this high level of variability permits generation of provider-level measures with good reliability. Such measures can be employed to provide feedback to physicians to modify overuse.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOC 33 kb)
Acknowledgments
This study was supported by the National Institutes of Health (K05CA134923, UL1TR000071 and P30AG024832) and the Agency for Healthcare Research and Quality (1R24HS022134-01). The funding agency had no role in the study design, conduct, analysis, or interpretation of data or in the preparation, review, or approval of the manuscript.
Sarah Toombs Smith, PhD, Science Editor and Assistant Professor at the Sealy Center on Aging, University of Texas Medical Branch at Galveston, provided editorial assistance in manuscript preparation. Dr. Toombs Smith received no compensation for her assistance apart from her employment at the institution where the study was conducted.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author Contributions
Dr. Zhou had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Tan and Goodwin. Acquisition of data: Goodwin. Analysis and interpretation of data: All authors. Drafting of the manuscript: Tan. Critical revision of the manuscript for important intellectual content: Goodwin and Kuo. Statistical analysis: Zhou. Obtained funding: Goodwin. Administrative, technical and material support: Tan, Kuo and Goodwin. Study supervision: Goodwin
REFERENCES
- 1.Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. National survey. Spine (Phila Pa 1976) 1995;20(1):11–9. doi: 10.1097/00007632-199501000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Atlas SJ, Deyo RA. Evaluating and managing acute low back pain in the primary care setting. J Gen Intern Med. 2001;16(2):120–31. doi: 10.1111/j.1525-1497.2001.91141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henley E. Understanding and treating low back pain in family practice. J Fam Pract. 2000;49(9):793–5. [PubMed] [Google Scholar]
- 4.Pengel LH, Herbert RD, Maher CG, Refshauge KM. Acute low back pain: systematic review of its prognosis. BMJ. 2003;327(7410):323. doi: 10.1136/bmj.327.7410.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chou R, Fu R, Carrino JA, Deyo RA. Imaging strategies for low-back pain: systematic review and meta-analysis. Lancet. 2009;373(9662):463–72. doi: 10.1016/S0140-6736(09)60172-0. [DOI] [PubMed] [Google Scholar]
- 6.Gilbert FJ, Grant AM, Gillan MG, et al. Low back pain: influence of early MR imaging or CT on treatment and outcome--multicenter randomized trial. Radiology. 2004;231(2):343–51. doi: 10.1148/radiol.2312030886. [DOI] [PubMed] [Google Scholar]
- 7.Kendrick D, Fielding K, Bentley E, Kerslake R, Miller P, Pringle M. Radiography of the lumbar spine in primary care patients with low back pain: randomised controlled trial. BMJ. 2001;322(7283):400–5. doi: 10.1136/bmj.322.7283.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Webster BS, Cifuentes M. Relationship of early magnetic resonance imaging for work-related acute low back pain with disability and medical utilization outcomes. J Occup Environ Med. 2010;52(9):900–7. doi: 10.1097/JOM.0b013e3181ef7e53. [DOI] [PubMed] [Google Scholar]
- 9.Deyo RA. Cascade effects of medical technology. Annu Rev Public Health. 2002;23:23–44. doi: 10.1146/annurev.publhealth.23.092101.134534. [DOI] [PubMed] [Google Scholar]
- 10.Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med. 2009;361(9):849–57. doi: 10.1056/NEJMoa0901249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith-Bindman R, Miglioretti DL, Larson EB. Rising use of diagnostic medical imaging in a large integrated health system. Health Aff (Millwood) 2008;27(6):1491–1502. doi: 10.1377/hlthaff.27.6.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berrington de González A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169(22):2071–7. doi: 10.1001/archinternmed.2009.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Medical Specialty Societies. Choosing Wisely Campaign: Five Things Physicians and Patients Should Question. Available at: http://www.choosingwisely.org/doctor-patient-lists/. Accessed July 7, 2015.
- 14.National Committee for Quality Assurance. NQA-Endosed national voluntary concensus standards for physician-focused ambulatory care: Appendix A -Natinal Committee for Quality Assurance measure technical specifications, April, 2008 V.7. Available at: http://www.ncqa.org/Portals/0/HEDISQM/NQF_Posting_Appendix.pdf. Accessed July 7, 2015.
- 15.Davis PC WFI, Cornelius RS, Angtuaco EJ, Broderick DF, Brown DC, Garvin CF, Hartl R, Holly L, McConnell CT Jr, Mechtler LL, Rosenow JM, Seidenwurm DJ, Smirniotopoulos JG. Expert Panel on Neurologic Imaging. ACR Appropriateness Criteria® low back pain. Reston, VA: American College of Radiology (ACR); 2011.
- 16.Chou R, Qaseem A, Owens DK, Shekelle P. Physicians CGCotACo. Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians. Ann Intern Med. 2011;154(3):181–9. doi: 10.7326/0003-4819-154-3-201102010-00008. [DOI] [PubMed] [Google Scholar]
- 17.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–91. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 18.Casazza BA. Diagnosis and treatment of acute low back pain. Am Fam Physician. 2012;85(4):343–50. [PubMed] [Google Scholar]
- 19.Delitto A, George SZ, Van Dillen LR, et al. Low back pain: clinical practice guidlines linked to the international classification of functioning, disability and health from the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2012;42(4):A1–57. doi: 10.2519/jospt.2012.42.4.A1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Chronic Pain Association. Consumers guide: Practice guidelines for low back pain. Available at: http://theacpa.org/uploads/documents/Consumer%20Guidelines%20for%20Low%20Back%20PainFinal%202-6-08.pdf. Accessed July 7, 2015.
- 21.Kale MS, Bishop TF, Federman AD, Keyhani S. Trends in the overuse of ambulatory health care services in the United States. JAMA Intern Med. 2013;173(2):142–8. doi: 10.1001/2013.jamainternmed.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pham HH, Landon BE, Reschovsky JD, Wu B, Schrag D. Rapidity and modality of imaging for acute low back pain in elderly patients. Arch Intern Med. 2009;169(10):972–81. doi: 10.1001/archinternmed.2009.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cherkin DC, Deyo RA, Wheeler K, Ciol MA. Physician variation in diagnostic testing for low back pain. Who you see is what you get. Arthritis Rheum. 1994;37(1):15–22. doi: 10.1002/art.1780370104. [DOI] [PubMed] [Google Scholar]
- 24.Jaramillo E, Tan A, Yang L, Kuo YF, Goodwin JS. Variation among primary care physicians in prostate-specific antigen screening of older men. JAMA. 2013;310(15):1622–4. doi: 10.1001/jama.2013.277514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wennberg J. Tracking medicine. New York: Oxford University Press; 2010. pp. 117–155. [Google Scholar]
- 26.Carey TS, Garrett J. Patterns of ordering diagnostic tests for patients with acute low back pain. The North Carolina Back Pain Project. Ann Intern Med. 1996;125(10):807–14. doi: 10.7326/0003-4819-125-10-199611150-00004. [DOI] [PubMed] [Google Scholar]
- 27.US Department of Agriculture. Rural–urban Continuum Codes. Available at: http://www.ers.usda.gov/data-products/rural–urban-continuum-codes/documentation.aspx. Accessed July 7, 2015.
- 28.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 29.Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53(12):1258–67. doi: 10.1016/S0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 30.Leyland A, Goldstein H, editors. Multilevel modelling of health statistics. New York: Wiley; 2001. [Google Scholar]
- 31.Normand S-LT, Glickman ME, Gatsonis CA. Statistical methods for profiling providers of medical care: issues and applications. J Am Stat Assoc. 1997;92(439):803–14. doi: 10.1080/01621459.1997.10474036. [DOI] [Google Scholar]
- 32.Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med. 2013;173(17):1573–81. doi: 10.1001/jamainternmed.2013.8992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lungren MP, Amrhein TJ, Paxton BE, et al. Physician self-referral: frequency of negative findings at MR imaging of the knee as a marker of appropriate utilization. Radiology. 2013;269(3):810–15. doi: 10.1148/radiol.13130281. [DOI] [PubMed] [Google Scholar]
- 34.Baker DW, Qaseem A, Reynolds PP, Gardner LA, Schneider EC. Design and use of performance measures to decrease low-value services and achieve cost-conscious care. Ann Intern Med. 2013;158(1):55–9. doi: 10.7326/0003-4819-158-1-201301010-00560. [DOI] [PubMed] [Google Scholar]
- 35.Hofer TP, Hayward RA, Greenfield S, Wagner EH, Kaplan SH, Manning WG. The unreliability of individual physician “report cards” for assessing the costs and quality of care of a chronic disease. JAMA. 1999;281(22):2098–2105. doi: 10.1001/jama.281.22.2098. [DOI] [PubMed] [Google Scholar]
- 36.Parry GJ, Gould CR, McCabe CJ, Tarnow-Mordi WO. Annual league tables of mortality in neonatal intensive care units: longitudinal study. International Neonatal Network and the Scottish Neonatal Consultants and Nurses Collaborative Study Group. BMJ. 1998;316(7149):1931–5. doi: 10.1136/bmj.316.7149.1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nelson EC, Gentry MA, Mook KH, Spritzer KL, Higgins JH, Hays RD. How many patients are needed to provide reliable evaluations of individual clinicians? Med Care. 2004;42(3):259–66. doi: 10.1097/01.mlr.0000114914.32196.c7. [DOI] [PubMed] [Google Scholar]
- 38.Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;6 doi: 10.1002/14651858.CD000259.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005;142(4):260–73. doi: 10.7326/0003-4819-142-4-200502150-00008. [DOI] [PubMed] [Google Scholar]
- 40.Rosenbaum L. The whole ball game--overcoming the blind spots in health care reform. N Engl J Med. 2013;368(10):959–62. doi: 10.1056/NEJMms1301576. [DOI] [PubMed] [Google Scholar]
- 41.Kaiser Family Foundation. Texas: Demographics and the economy indicators. Available at: http://kff.org/state-category/demographics-and-the-economy/?state=TX. Accessed July 7, 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC 33 kb)