Abstract
Objective
To evaluate the care status of the amyotrophic lateral sclerosis (ALS) patients with long-term use of tracheostomy tube by caregivers of ALS patients.
Methods
A survey was conducted in the form of questionnaires to ALS patients and their caregivers. All measurements were performed by two visiting nurses. For statistical analysis, SPSS ver. 22.0 and Mann-Whitney U test on non-normal distribution were used.
Results
In total, 19 patients (15 males and 4 females) and their caregivers participated in the survey. In the case of patients, the average duration of care was 5.9±3.7 years, and the mean periods of illness and tracheostomy were 5.3±3.2 years and 3.0±2.6 years, respectively. Replacement intervals were 14 days in 11 patients, 7 days in 4 patients, 28 days in 2 patients, and 21 days in 1 patient. One patient was unable to provide an accurate replacement interval. Eighteen (99%) caregivers had experience of adding volume to a cuff without pressure measure in the following instances: due to patients' needs in 7 cases, air leakage in 7 cases, and no reason in 4 cases. Mean pressure of tracheostomy cuff was 40±9.4 cmH2O, and air volume of tracheostomy cuff was 6.7±3.2 mL, but real mean volume was 7.0±2.9 mL. The number of suctioning for airway clearance was a mean 27.5±18.2 times a day.
Conclusion
According to this survey, we notice that almost all the patients and caregivers had an erroneous idea about cuff volume and pressure. Moreover, education and long-term professional care of tracheostomy cannot be overemphasized in this manner.
Keywords: Amyotrophic lateral sclerosis, Tracheostomy, Long-term care, Caregiver
INTRODUCTION
Amyotrophic lateral sclerosis (ALS) is characterized by progressive weakness and atrophy of muscles in the limbs, trunk, bulbar, and respiratory system [1]. Respiratory insufficiency is usually manifested in the late course of disease due to progressive dysphasia from bulbar muscle involvement, and hypoventilation from diaphragmatic involvement [1,2]. Therefore, most of ALS patients are assisted by non-invasive mechanical ventilation (NIV) or undergo tracheostomy with mechanical ventilation for life prolongation.
According to the study of Chio et al. [1], nearly 50% of ALS patients discharge for home, which is the preferred location for long-term mechanical ventilation since it enhances the quality of life and reduces the cost. Although family usually plays a role of the primary caregiver, care statue of patients and caregivers toward long-term tracheostomy have received limited attention, and only few studies have been investigated so far [3]. Furthermore, these caregivers are usually uneducated regarding the basic knowledge and care of tracheostomy, which are important in preventing late complications of tracheostomy care [4]. In the present survey too, we found that no individual had any information about the importance of tracheostomy tube management with appropriate cuff pressure of 20-25 mmHg (25-35 cmH2O) [5]. If problems arising due to the caregiver's ignorance can be detected early, numerous late complications of tracheostomy would be prevented. Prevention is also possible with educated and disciplined caregivers.
Considering this, we decided to conduct a survey to evaluate the care status of the ALS patients with long-term use of tracheostomy tube, by their caregivers.
MATERIALS AND METHODS
A survey was conducted in the form of questionnaires to ALS patients, who were receiving home nursing care and following up from Pusan National University Hospital, and their caregivers. We carried out a survey regarding ALS patients, who were supported by mechanical ventilation with tracheostomy, between October 2013 and April 2014. The information of the patient included the name, sex, age, size of tracheostomy tube, and type of tracheostomy tube.
The questionnaires included open and closed form of questions, and contained detailed queries about the following: mean period of illness, mean period of tracheostomy, experience of using NIV before tracheostomy, duration of providing care, working time of care, and relation with the patient. The questionnaires also included demographic items and details about tracheostomy tube and care status, such as tube replacement interval, any experience of adding volume to tracheostomy tube inflation, reason for extra volume, and the number of times of suctioning (with or without using a mechanical insufflation-exsufflation [MIE]). All measurements were performed by two visiting nurses from Pusan National University Hospital. The mean air volume of tracheostomy cuff was measured by a cuff pressure manometer, with modification of the technique used in the study of Sengupta et al. [6] This was as follows: first, the cuff pressure was measured (cmH2O) according to the mean air volume (mL); second, air was released by using a syringe and the volume was recorded; third, the real air volume was recorded and cuff pressure was re-measured, until the cuff pressure measured is the same as the first one.
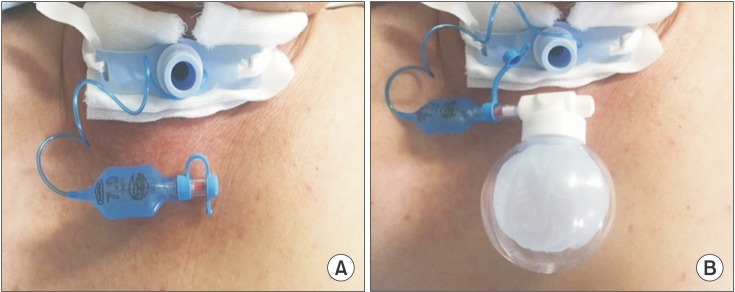
What's more, we primarily educated the caregiver's basic knowledge of tracheostomy tube management and applied a smart cuff manager which could adjust the cuff pressure automatically, if needed (Fig. 1). We also conducted education about proper suctioning as the American Association for Respiratory Care (AARC) guidelines; these included guidelines regarding adequate selection as deep suction and shallow suction, suctioning with less than 150 mmHg of negative pressure, and not more than 15 seconds [7].
Fig. 1. (A) Tracheostomy tube without smart cuff manager. (B) Tracheostomy tube with smart cuff manager which controls the cuff pressure continuously.
SPSS ver. 22.0 (IBM SPSS, Armonk, NY, USA) was used for data analysis, and comparisons between the mean volume of tracheostomy cuff by caregiver and by nurse were made using the Mann-Whitney U test because it showed non-normal distribution.
RESULTS
A total of 19 patients (15 men and 4 women) and their caregivers participated in the survey. Amongst the caregivers, 10 were spouses, 3 were professional caregivers, 3 were mothers, 2 were either son or daughter, and 1 was a sister. The average duration of providing care for their patients was 5.9±3.7 years, and the average working time was 12 hours per day.
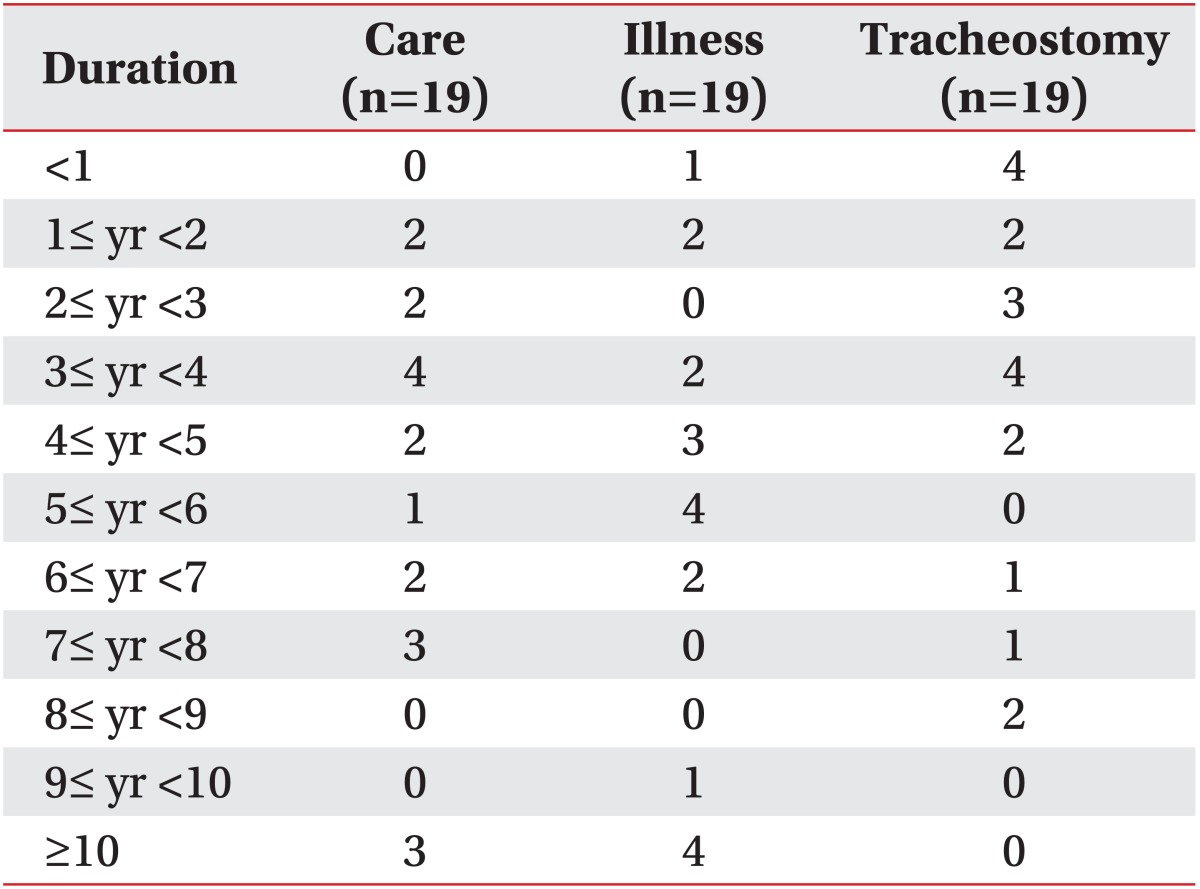
The mean periods of illness and tracheostomy for the patients were 5.3±3.2 and 3.0±2.6 years, respectively (Table 1). All patients were currently using a mechanical ventilator via a tracheostomy tube, 5 of whom had previously used a non-invasive ventilator through a nasal or full face mask before the tracheostomy, for different lengths of time, ranging from 1 month to 7 years.
Table 1. Duration of providing care, illness, and tracheostomy.
The inner diameter of the tracheostomy tubes were 7.5 mm in 11 patients, 8.0 mm in 7 patients, and 7.0 mm in 1 patient. The type or product name of the different tracheostomy tubes used were cuffed adjustable flange tracheostomy tube by Portex Blue Line (1 patient), silicone tracheostomy tube by Portex Bivona (1 patient), extra vertical length tracheostomy tube with double cuff by Portex Blue Line (1 patient), tracheostomy tube by Yushin (1 patient), tracheostomy tube by Covidien (1 patient), vocalaid cuffed tracheostomy tube by Portex Blue Line (2 patients), and cuffed tracheostomy tube by Portex Blue Line (12 patients). Because of the small sample size, it was hard to compare the cuff pressure between these products, or the differing pressure based on the inner diameter of tracheostomy.
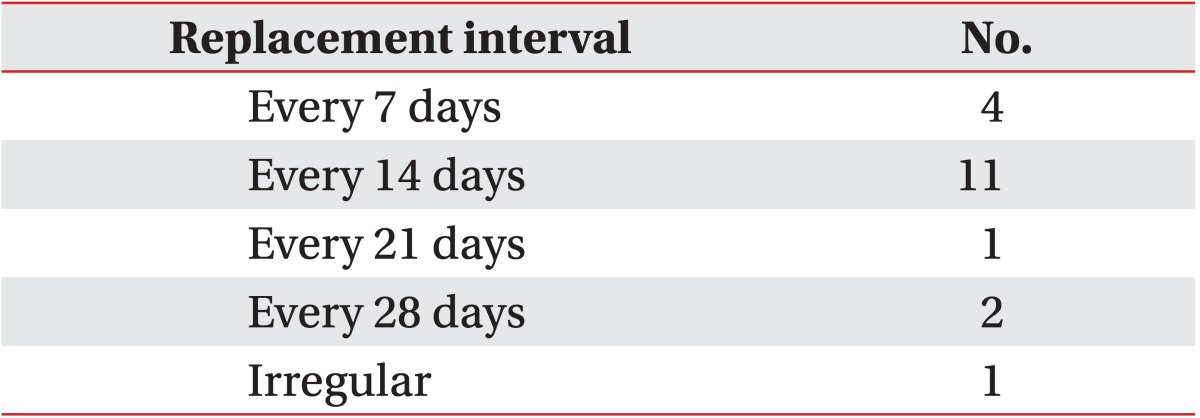
The tube replacement interval was 14 days in 11 patients, 7 days in 4 patients, 28 days in 2 patients, and 21 days in 1 patient (Table 2). One patient was unable to provide an accurate replacement interval. All tracheostomy tube replacements were performed by a visiting nurse; however, one caregiver did it by herself, and this was the case in which an accurate replacement interval was not provided.
Table 2. Replacement interval of tracheostomy tube, regardless of the type of cannula (n=19).
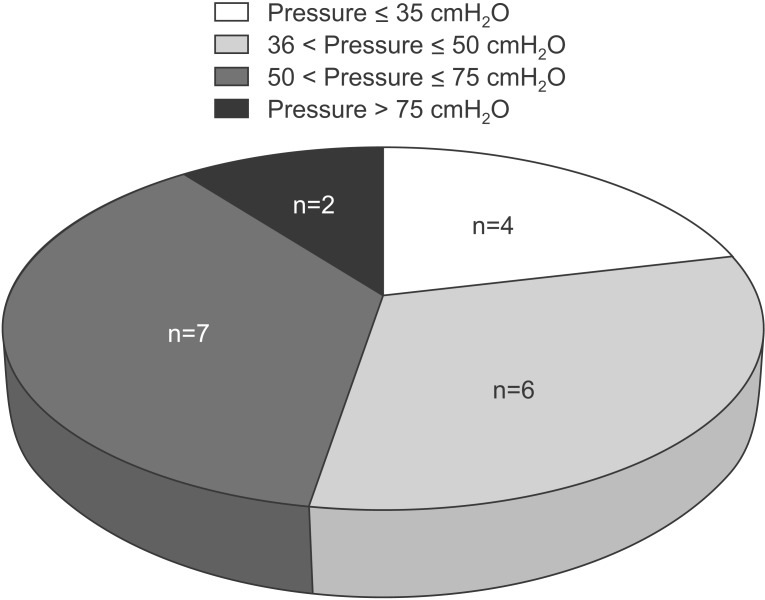
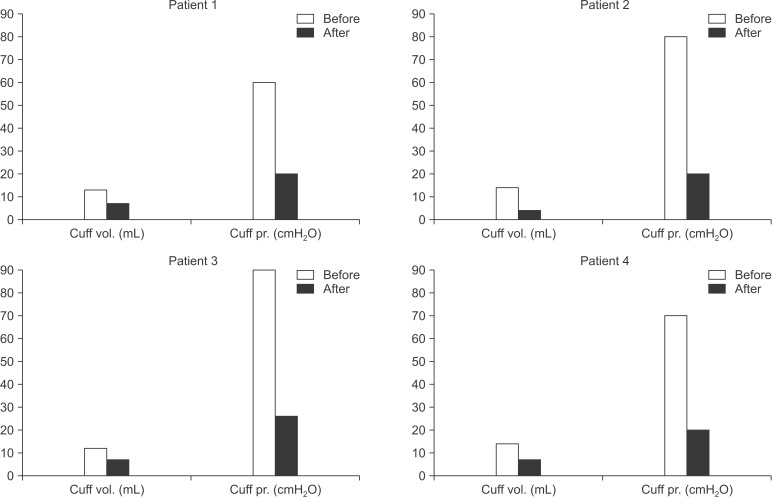
Eighteen (95%) caregivers had experience for addition of the tracheostomy cuff volume without measuring the pressure. Abnormal high cuff pressure was observed in 15 (78.9%) of the 19 patients (Fig. 2). The reasons for adding cuff volume were difficulty or discomfort in breathing, and air leakage around the tracheostomy site, in 7 cases each; 4 patients were unable to provide an accurate reason. Only 2 caregivers answered that there were 2 reasons for adding cuff volume: because it was requested by the patient, and because of air leakage. According to the caregivers' records, the mean air volume of the tracheostomy cuff was 6.7±3.2 mL. However, the mean pressure of tracheostomy measured by the visiting nurse was 40±9.4 cmH2O. Also, the real mean air volume of the tracheostomy cuff measured by the visiting nurse was 7.0±2.9 mL. It showed that the real mean volume of tracheostomy cuff as measured by the visiting nurse was higher than the caregiver's record. Although there was no difference of mean air volume by statistical analysis of Mann-Whitney U test, we should consider this to be an effect of small sample size. Some of ALS patients, who had received long-term tracheostomy care with mechanical ventilation, were admitted to our hospital and diagnosed as tracheomalacia due to the over-inflation of tracheostomy cuff. In those cases, we replaced their Portex tracheostomy tube to adjustable flange tracheostomy tube with a smart cuff manager for cuff pressure regulation, and imparted adequate instructions to the caregivers (Fig. 1).
Fig. 2. Most of caregivers experienced over-inflation on tracheostomy tube. The figure showed 78.9% of the patients have an abnormal high cuff pressure (normal range of cuff pressure, 25-35 cmH2O).
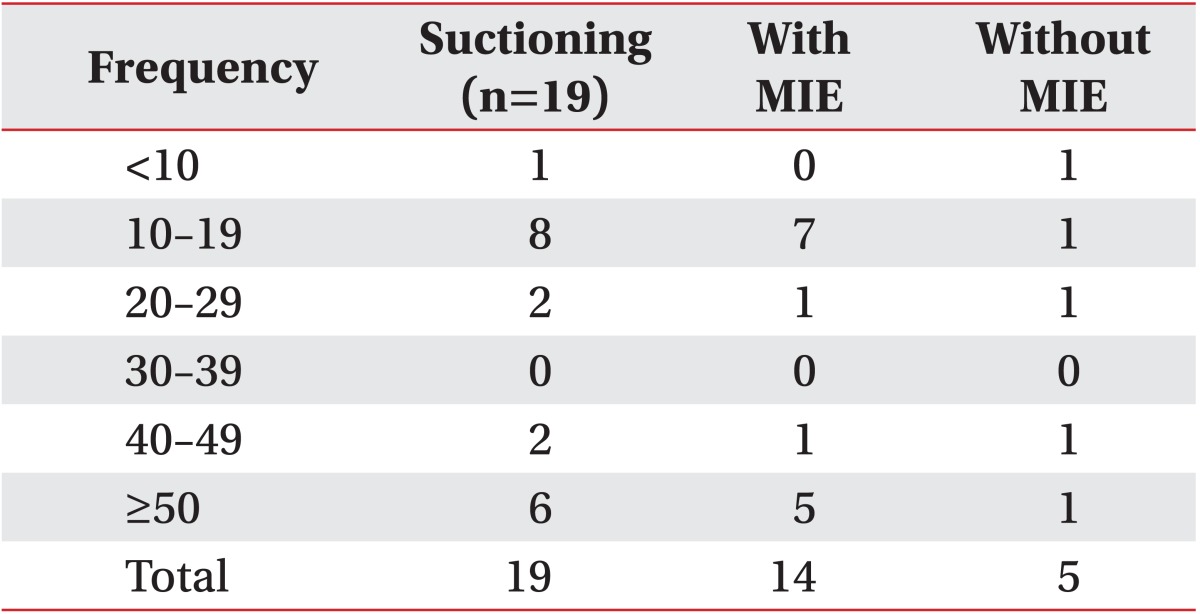
Recently, 4 patients were hospitalized; therefore, they could receive training about tracheostomy care. Among these 4 patients, the cuff volume and pressure immediately after admission was 13 mL and 60 cmH2O, 14 mL and 80 cmH2O, 12 mL and 90 cmH2O, and 14 mL and 70 cmH2O. However, after imparting training and given a discharge, a visiting nurse recorded the following decreased volume and pressure in the 4 patients: 7 mL and 20 cmH2O, 4 mL and 20 cmH2O, 7 mL and 26 cmH2O, and 7 mL and 20 cmH2O, respectively (Fig. 3). As the number of patients was small, no statistical analysis was carried out.
Fig. 3. Comparison of cuff inflation volume and pressure 4 patients, before and after imparting education.
The mean number of times in which suctioning was performed for airway clearance was 27.5±18.2 times per day; however, the results showed polarization, since two groups numbering 10 and 8 patients, suctioning were performed under 15 times and over 40 times, respectively (Table 3). Fourteen patients answered that suctioning was performed more often in the daytime, while only 4 patients required suctioning more frequently at night. One patient did not notice a difference in the frequency of suctioning between day and night.
Table 3. Frequency of suctioning with or without mechanical insufflation-exsufflation (MIE).
Fourteen patients reported using a MIE at home, but there was no difference in the frequency of suctioning between MIE users and non-users (27.5±18.8 times vs. 25.0±18.5 times, respectively) (Table 3).
DISCUSSION
Considering the recent study of Chio et al. [1] that the mean duration of ALS before tracheostomy was 2.4 years and mean survival time after tracheostomy was 253 days, the results of this survey showed a relatively longer care duration (average 5.9±3.7 years). However, the average working time (12 hours per day) was similar to the report (14.4 hours per day) of Kaub-Wittemer et al. [8]. Most of the caregivers were family, with the spouse (52.6%) being a major caregiver among family members; this result was similar to previous studies [8,9].
Numerous studies recommend that the changing interval of tracheostomy tube may require 7-10 days after first insertion, 10-14 days on single lumen tube, and not less than 30 days on double cannula tube [10]. All of these recommendations are for preventing tube blockage from excessive secretions and development of granulation tissue [8,11]. However, our results indicated 7 and 28 days intervals of changing tracheostomy tubes, regardless of the type of cannula, and irregular changing of the tracheostomy tube 1 patient.
This study highlights some interesting points about how much information the caregivers have for tracheostomy care, and how the caregivers actually care about tracheostomy tube. According to the survey, we realized that most of the caregivers had performed tracheostomy care without any basic knowledge or precaution regarding future complications.
Tracheostomy is performed for general clinical indications such as airway obstruction, to protect airway, to facilitate weaning of mechanical ventilation, to assist secretion removal, and to allow long-term ventilation [4,12]. Complications after tracheostomy can be divided into immediate, short-term and long-term complications [13]. Immediate complications include airway loss, obstruction of tracheostomy tube, and hemorrhage, whereas short-term complications include blockage or tracheostomy tube displacement [14]. Long-term complications include infection, tracheal stenosis due to development of granuloma tissue, skin breakdown due to downward traction, tracheoinnominate artery fistula, tracheomalacia, and tracheoesophageal fistula [4,15].
Among these, the long-term complications are directly related to the care imparted in patients having tracheostomy, who require long-term respiratory care. The relevant mechanism of long-term complications include cuff related problems, mostly with or without displacement of tube tip and abnormal healing of injured tracheal mucosa [16]. The cuff of tracheostomy allows for airway clearance, airway protection, and effective ventilation [5]. Although optimal tracheal capillary perfusion pressure is 25-35 mmHg, transmitted pressure to the trachea is less than the cuff pressure [5]. Therefore, the cuff pressure should be maintained at 20-25 mmHg (25-35 cmH2O) with most tracheostomy tubes, to prevent tracheal wall injury and aspiration, and intra-cuff pressure should be monitored [5]. Most caregivers have a tendency to overinflate the tracheostomy cuff, and even in this survey, most of caregivers (78.9%) experienced over-inflation on tracheostomy tube (mean pressure 40±9.4 cmH2O) because of the patient's request, air leakage or without any reason. Our results indicated that almost all patients and caregivers have an erroneous idea about cuff volume and pressure. Over-inflation of the tracheostomy tube could lead to ischemic injury on the tracheal mucosa wall, and prolonged ischemia could develop into tracheal stenosis due to the formation of granulation tissue [15]. If this condition proceeds to the weakened tracheal wall which have a loss of cartilaginous support, tracheomalacia may be occurred by airway collapse [15]. The posterior tracheal wall injury by persistence excessive cuff pressure could also result in tracheoesophageal fistula [15]. Moreover, excessive movement, lower placement, and overinflation of tracheostomy could develop into tracheoinnominate artery erosion [15]. As mentioned above, these long-term complications of tracheostomy are related to the tracheostomy cuff pressure care status. We could adjust tracheostomy cuff pressure by proper education of the patients and their caregivers.
We also observed that the frequency of suctioning varied between less than 15 times to over 40 times; the AARC clinical practice guideline has also not established an adequate frequency of suctioning [7]. Also, the frequency of suctioning was irrespective whether a MIE was used or not. This may be a result of the fact that MIE allows the caregivers to increase the number of shallow suctioning, while it enables decreasing the number of deep suctioning, enhancing the establishment of clear secretion. We also conducted an education about proper suctioning as the AARC guidelines; the guidelines included factors such as the adequate selection of deep suction and shallow suction, suctioning with less than 150 mmHg of negative pressure, and not more than 15 seconds [7].
Many ALS patients have been managed by invasive home ventilators, and therefore we need to educate proper tracheostomy care methods for patients and their caregivers [17]. We could not perform a limited statistical analysis due to the relatively small number of patients and caregivers recruited in this study. Nevertheless, we may emphasize how important it is to educate caregivers about appropriate tracheostomy cuff volume and pressure management, based on the results of the present study.
ACKNOWLEDGMENTS
The authors would like to thank Pusan National University Hospital Regional Center for Respiratory Diseases for their support in this work.
This work was supported by the year 2015 clinical research grant from Pusan National University Hospital.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Chio A, Calvo A, Ghiglione P, Mazzini L, Mutani R, Mora G, et al. Tracheostomy in amyotrophic lateral sclerosis: a 10-year population-based study in Italy. J Neurol Neurosurg Psychiatry. 2010;81:1141–1143. doi: 10.1136/jnnp.2009.175984. [DOI] [PubMed] [Google Scholar]
- 2.Escarrabill J, Estopa R, Farrero E, Monasterio C, Manresa F. Long-term mechanical ventilation in amyotrophic lateral sclerosis. Respir Med. 1998;92:438–441. doi: 10.1016/s0954-6111(98)90288-8. [DOI] [PubMed] [Google Scholar]
- 3.Marchese S, Lo Coco D, Lo Coco A. Outcome and attitudes toward home tracheostomy ventilation of consecutive patients: a 10-year experience. Respir Med. 2008;102:430–436. doi: 10.1016/j.rmed.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 4.Morris LL, Whitmer A, McIntosh E. Tracheostomy care and complications in the intensive care unit. Crit Care Nurse. 2013;33:18–30. doi: 10.4037/ccn2013518. [DOI] [PubMed] [Google Scholar]
- 5.Hess DR. Tracheostomy tubes and related appliances. Respir Care. 2005;50:497–510. [PubMed] [Google Scholar]
- 6.Sengupta P, Sessler DI, Maglinger P, Wells S, Vogt A, Durrani J, et al. Endotracheal tube cuff pressure in three hospitals, and the volume required to produce an appropriate cuff pressure. BMC Anesthesiol. 2004;4:8. doi: 10.1186/1471-2253-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Association for Respiratory Care. Endotracheal suctioning of mechanically ventilated patients with artificial airways 2010. AARC Clinical Practice Guidelines. Respir Care. 2010;55:758–764. [PubMed] [Google Scholar]
- 8.Kaub-Wittemer D, von Steinbuchel N, Wasner M, Laier-Groeneveld G, Borasio GD. Quality of life and psychosocial issues in ventilated patients with amyotrophic lateral sclerosis and their caregivers. J Pain Symptom Manag. 2003;26:890–896. doi: 10.1016/s0885-3924(03)00323-3. [DOI] [PubMed] [Google Scholar]
- 9.Rabkin JG, Albert SM, Tider T, Del Bene ML, O'Sullivan I, Rowland LP, et al. Predictors and course of elective long-term mechanical ventilation: a prospective study of ALS patients. Amyotroph Lateral Scler. 2006;7:86–95. doi: 10.1080/14660820500515021. [DOI] [PubMed] [Google Scholar]
- 10.Regan K, Hunt K. Tracheostomy management. Contin Educ Anaesth Crit Care Pain. 2008;8:31–35. [Google Scholar]
- 11.Yaremchuk K. Regular tracheostomy tube changes to prevent formation of granulation tissue. Laryngoscope. 2003;113:1–10. doi: 10.1097/00005537-200301000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Mallick A, Bodenham AR. Tracheostomy in critically ill patients. Eur J Anaesthesiol. 2010;27:676–682. doi: 10.1097/EJA.0b013e32833b1ba0. [DOI] [PubMed] [Google Scholar]
- 13.McGrath BA, Bates L, Atkinson D, Moore JA National Tracheostomy Safety Project. Multidisciplinary guidelines for the management of tracheostomy and laryngectomy airway emergencies. Anaesthesia. 2012;67:1025–1041. doi: 10.1111/j.1365-2044.2012.07217.x. [DOI] [PubMed] [Google Scholar]
- 14.Byard RW, Gilbert JD. Potentially lethal complications of tracheostomy: autopsy considerations. Am J Forensic Med Pathol. 2011;32:352–354. doi: 10.1097/PAF.0b013e31822abf4e. [DOI] [PubMed] [Google Scholar]
- 15.Epstein SK. Late complications of tracheostomy. Respir Care. 2005;50:542–549. [PubMed] [Google Scholar]
- 16.Sue RD, Susanto I. Long-term complications of artificial airways. Clin Chest Med. 2003;24:457–471. doi: 10.1016/s0272-5231(03)00048-0. [DOI] [PubMed] [Google Scholar]
- 17.Lewarski JS. Long-term care of the patient with a tracheostomy. Respir Care. 2005;50:534–537. [PubMed] [Google Scholar]