Abstract
Immunoglobulin G4 (IgG4)-related disease is an autoimmune disease that forms tumorous lesions. Several cases involving various organs are reported, however, IgG4-related disease involving appendix has not been reported yet. In this report, we presented a case of IgG4-related disease of appendix, which raised a suspicion of appendiceal tumor or usual appendicitis and, therefore, led to unnecessary surgical resection. IgG4-related disease should be considered in the differential diagnosis for a mass-like swelling of the appendix, in order to avoid unnecessary surgery.
Keywords: IgG4-related disease, Appendix, CT
INTRODUCTION
Gastrointestinal tract involvement of immunoglobulin G4 (IgG4)-related disease is rare. To the best of our knowledge, IgG4-related disease that mimics appendiceal pathology such as appendiceal tumor or usual appendicitis has never been reported. We reported a case of IgG4-related disease of the appendix that was misdiagnosed as appendiceal tumor or usual appendicitis and, thus, led to surgical resection. The review of this report was exempted by the Institutional Review Board of our institution.
CASE REPORT
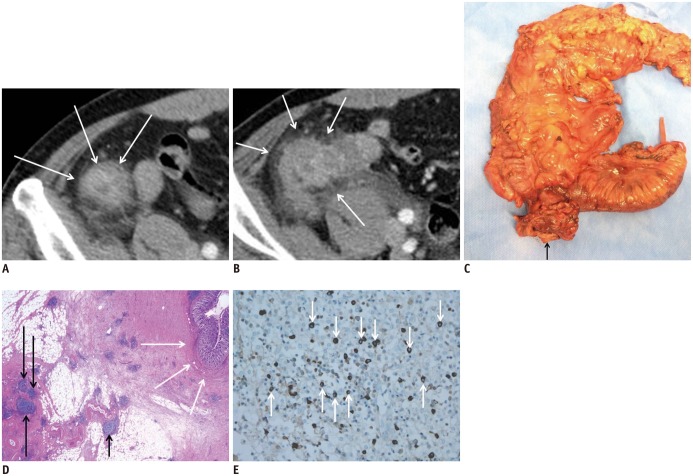
A 51-year-old man visited the emergency room of our institution with right lower quadrant abdominal pain that 58had persisted for 2 days without fever. Initial blood tests showed no abnormalities other than mild elevation of erythrocyte sedimentation rate (22 mm/h) and C-reactive protein (19.01 mg/L). However, abdominal CT scan showed a solid mass-like swelling at the appendiceal tip. The mass was approximately 3.6 cm in size and well enhanced. Accompanying perimesenteric fat haziness suggested that the mass could be inflammatory (Fig. 1A), but malignancy could not entirely be ruled out.
Fig. 1. Immunoglobulin G4-related disease in 51-year-old man.
A. Axial contrast-enhanced CT image shows 3.6 cm solid mass at appendiceal tip (arrows). Associated periappendiceal fat infiltrations suggest that mass is inflammatory. B. Axial contrast-enhanced CT taken 21 days after initial CT (A). No significant change in mass is noted. However, periappendiceal fat haziness is aggravated (arrows). C. Right hemicolectomy includes 29 cm of ascending colon and 21 cm of ileum. Appendix forms mass sized 4.3 × 2.8 × 1.7 cm with fat proliferations on surface (arrow). D. Hematoxylin-eosin staining shows plasmacytic infiltration in subserosa of appendix (black arrows). Mucosal layer and muscle layer of appendix (white arrows) are intact suggesting that main pathology lies in mesentery rather than appendix (× 12.5). E. Immunoglobulin G4 (IgG4) stain shows IgG4-positive plasmacytes. Brown pigmented cells (arrows) are IgG4-positive cells. On IgG staining, > 50% of IgG-positive cells are IgG4 positive (not presented) (× 400).
After 3 days of antibiotics therapy, the patient was symptom-free and discharged. During the follow-up, the patient suffered another episode of abdominal pain and a second abdominal CT scan was done at 21 days after the first scan. The second CT scan did not show a significant change in the solid mass at the appendiceal tip, but the periappendiceal mesenteric fat haziness was aggravated (Fig. 1B). After 3 days of antibiotics use, the patient underwent surgery. Right hemicolectomy was done because malignancy could not be ruled out.
Resected appendix measured 4.3 × 2.8 × 1.7 cm forming a mass consistent with CT findings (Fig. 1C). Microscopically, there was no evidence of acute appendicitis. Muscle layer of the appendix was intact, but subserosal inflammatory cell infiltration was noted (Fig. 1D). Magnification of inflammatory cells showed that they were mostly plasmacytes. Storiform fibrosis or obliterative phlebitis was absent; however, immunohistochemical (Fig. 1E) revealed that > 50% of IgG cells were IgG4 cells, consistent with IgG4-related disease.
DISCUSSION
Immunoglobulin G4-related disease is a newly recognized immune-mediated condition that can involve various sites (1). Inflammatory-cell infiltration leads to tumorous lesions of the affected organ. Autoimmunity is regarded as the initial trigger of a type 2 helper T cell immune response. Activated type 2 helper T cells produce interleukin-5, which stimulates eosinophils to proliferate, as observed in our case. Type 2 helper T cells also directly activate regulatory T cells. Activated regulatory T cells produce tumor growth factor β, which leads to fibrosis. Regulatory T cells also stimulate B cells to differentiate into plasma cells, followed by excessive secretion of IgG4 antibodies. The inflammatory cell infiltrate results in tumefactive enlargement of the affected site. IgG4 antibodies produced in this process behave as tissue-destructive immunoglobulins (1).
Immunoglobulin G4-related disease is described in almost every organ system (1). The pancreas was the first organ reported to be involved in IgG4-related disease, and is perhaps the most frequently involved site reported in the literature (2). Involvement of biliary tree is the second most frequent, followed by the major salivary glands, kidney, gall bladder, and retroperitoneum (2). Although IgG4-related disease involving the gastrointestinal tract is very rare, there are reports of IgG4-related disease involving the esophagus, stomach, duodenum, ileum, and colon (3,4,5).
Gastrointestinal IgG4-related lesions are difficult to diagnose because symptoms vary and CT findings are nonspecific (3,4,5). Two cases involving the esophagus presented with esophageal wall thickening (6,7). Several case studies have reported involvement of the gastric mucosa associated with autoimmune pancreatitis, but not all cases showed dense fibrosis or obliterative phlebitis with a high serum IgG4 level (5). Cases consistent with IgG4-related disease either presented as a well-circumscribed nodular mass (3 cases) or ulcer (2 cases) (5). IgG4-positive plasma cells sometimes infiltrate the colonic mucosa in ulcerative colitis patients, but the mechanisms are unknown (8). Two cases involving the sigmoid flexure and cecum without associated autoimmune pancreatitis are reported. These 2 cases presented as a well-circumscribed fibrous nodular lesion in the gastro-intestinal tract (9). There are 3 previously reported cases of IgG4-related disease involving the small bowel. Two presented as bowel wall thickening (4,10), and 1 as multiple pelvic masses obstructing the bowel lumens (3). Despite the few reports of IgG4-related disease involving the gastrointestinal tract, there appear to be 2 types of IgG4-related gastrointestinal disease. One is a gastrointestinal lesion showing marked thickening of the wall of the esophagus and stomach, consisting of dense fibrosis with abundant infiltration of IgG4-positive plasma cells that usually show submucosal spreading. The other is an IgG4-related pseudotumor that occurs in gastrointestinal regions such as the stomach, colon, and major duodenal papilla, appearing as a polypoid or mass-like lesion (5). In our case, an appendiceal mass-like lesion with an increase in periappendiceal fatty strands was observed on abdominal CT scan.
Greater fat infiltration than bowel wall thickening implies that the main pathology lies in the mesentery rather than the gastrointestinal tract (11). Subserosal plasmacyte infiltration also indicates that the disease originates from the mesentery and involves the gastrointestinal tract (10). In this case, these factors may have collectively caused periappendiceal fatty strands.
Symptoms vary according to the organs affected. Aggressive treatment including endovascular intervention is needed in life-threatening conditions (12), but the mainstay of treatment is pharmaceutical (1). In our case, unnecessary surgery was performed.
Immunoglobulin G4-related disease is a rare disease, especially involving the gastrointestinal tract. Although only a handful of cases are reported, IgG4-related disease involving the gastrointestinal tract either spreads through the submucosa or forms tumorous lesions (5). In our case, IgG4-related disease presented as perilesional fat infiltrations in CT scans due to the inflammatory nature of the disease. IgG4-related disease should be considered in the differential diagnosis for a mass-like swelling of the appendix.
References
- 1.Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012;366:539–551. doi: 10.1056/NEJMra1104650. [DOI] [PubMed] [Google Scholar]
- 2.Brito-Zerón P, Ramos-Casals M, Bosch X, Stone JH. The clinical spectrum of IgG4-related disease. Autoimmun Rev. 2014;13:1203–1210. doi: 10.1016/j.autrev.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 3.Coulier B, Montfort L, Beniuga G, Pierard F, Gielen I. Small bowel obstruction caused by peritoneal immunoglobulin g4-related disease mimicking carcinomatosis: case report. Korean J Radiol. 2014;15:66–71. doi: 10.3348/kjr.2014.15.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ko Y, Woo JY, Kim JW, Hong HS, Yang I, Lee Y, et al. An immunoglobulin G4-related sclerosing disease of the small bowel: CT and small bowel series findings. Korean J Radiol. 2013;14:776–780. doi: 10.3348/kjr.2013.14.5.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koizumi S, Kamisawa T, Kuruma S, Tabata T, Chiba K, Iwasaki S, et al. Immunoglobulin G4-related gastrointestinal diseases, are they immunoglobulin G4-related diseases? World J Gastroenterol. 2013;19:5769–5774. doi: 10.3748/wjg.v19.i35.5769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee H, Joo M, Song TJ, Chang SH, Kim H, Kim YS, et al. IgG4-related sclerosing esophagitis: a case report. Gastrointest Endosc. 2011;73:834–837. doi: 10.1016/j.gie.2010.08.043. [DOI] [PubMed] [Google Scholar]
- 7.Lopes J, Hochwald SN, Lancia N, Dixon LR, Ben-David K. Autoimmune esophagitis: IgG4-related tumors of the esophagus. J Gastrointest Surg. 2010;14:1031–1034. doi: 10.1007/s11605-010-1172-4. [DOI] [PubMed] [Google Scholar]
- 8.Raina A, Yadav D, Regueiro M, Krasinskas AM, Saul MI, Sapienza DA, et al. Mucosal IgG4 cell infiltration in ulcerative colitis is linked to disease activity and primary sclerosing cholangitis. Inflamm Bowel Dis. 2013;19:1232–1237. doi: 10.1097/MIB.0b013e318281344d. [DOI] [PubMed] [Google Scholar]
- 9.Chetty R, Serra S, Gauchotte G, Märkl B, Agaimy A. Sclerosing nodular lesions of the gastrointestinal tract containing large numbers of IgG4 plasma cells. Pathology. 2011;43:31–35. doi: 10.1097/PAT.0b013e328340e450. [DOI] [PubMed] [Google Scholar]
- 10.Hiyoshi Y, Oki E, Zaitsu Y, Ando K, Ito S, Saeki H, et al. IgG4-related disease of the ileocecal region mimicking malignancy: a case report. Int J Surg Case Rep. 2014;5:669–672. doi: 10.1016/j.ijscr.2014.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pereira JM, Sirlin CB, Pinto PS, Jeffrey RB, Stella DL, Casola G. Disproportionate fat stranding: a helpful CT sign in patients with acute abdominal pain. Radiographics. 2004;24:703–715. doi: 10.1148/rg.243035084. [DOI] [PubMed] [Google Scholar]
- 12.Rossi M, Virgilio E, Laurino F, Orgera G, Menè P, Pirozzi N, et al. Giant hepatic artery aneurysm associated with immunoglobulin G4-related disease successfully treated using a liquid embolic agent. Korean J Radiol. 2015;16:953–954. doi: 10.3348/kjr.2015.16.4.953. [DOI] [PMC free article] [PubMed] [Google Scholar]