Abstract
Objective:
This study was aimed to investigate the reliability of a computer application for assessment of the stages of cervical vertebra maturation in order to determine the stage of skeletal maturity.
Material and methods:
For this study, digital lateral cephalograms of 99 subjects (52 females and 47 males) were examined. The following selection criteria were used during the sample composition: age between 9 and 16 years, absence of anomalies of the vertebrae, good general health, no history of trauma at the cervical region. Subjects with lateral cephalograms of low quality were excluded from the study. For the purpose of this study a computer application Cephalometar HF V1 was developed. This application was used to mark the contours of the second, third and fourth cervical vertebrae on the digital lateral cephalograms, which enabled a computer to determine the stage of cervical vertebral maturation. The assessment of the stages of cervical vertebral maturation was carried out by an experienced orthodontist. The assessment was conducted according to the principles of the method proposed by authors Hassel and Farman. The degree of the agreement between the computer application and the researcher was analyzed using by statistical Cohen Kappa test.
Results:
The results of this study showed the agreement between the computer assessment and the researcher assessment of the cervical vertebral maturation stages, where the value of the Cohen Kappa coefficient was 0.985.
Conclusion:
The computer application Cephalometar HF V1 proved to be a reliable method for assessing the stages of cervical vertebral maturation. This program could help the orthodontists to identify the stage of cervical vertebral maturation when planning the orthodontic treatment for the patients with skeletal disharmonies.
Keywords: Orthodontics, Cervical vertebrae, Maturation, Lateral cephalograms, Computer application
1. INTRODUCTION
Optimal treatment time is a fundamental concept of orthodontic treatment of skeletal disharmonies. A successful correction of skeletal disharmonies is achieved by growth modification, which can be carried out in patients who have a certain amount of growth remaining. Therefore, the most favorable time for the treatment of skeletal disharmonies during pubertal growth spurt (1, 2, 3).
Studies of growth and development have shown that there are wide individual variations in the timing, duration and velocity of pubertal growth spurt (4, 5), which are need to assess the stage of skeletal maturity of each person. Assessment of individual skeletal maturity can be determined using a number of different, more or less reliable parameters such as: chronological age, body weight and height, secondary sexual characteristics, dental maturity, hand-wrist radiograph and cervical vertebrae maturation method (6, 7). The hand-wrist radiographs have been used as “gold standard” for determination of skeletal maturation for many years (8, 9). To avoid additional X-ray exposure of a patient, a new method for assessment of skeletal maturity based on the analysis of the morphology of the cervical vertebrae was developed (3). The cervical vertebrae are visible on the lateral cephalograms, which are routinely used in orthodontics diagnostic procedures, so that represents an additional advantage of this method. Several methods for assessment of skeletal maturity based on analysis of the cervical vertebra have been described in literature (3,10), and their reliability has been confirmed in numerous published studies (10, 11, 12, 13, 14). All methods are based on the analysis of morphological characteristics of the second, third and fourth cervical vertebrae (C2, C3, C4), such as the concavity of the lower border and the shape of a body of the cervical vertebrae, which change from birth until reaching the skeletal maturity. Hassel and Farman developed a cervical vertebral maturation index (CVMI) observed on the lateral cephalograms (10).
The assessment of cervical vertebral maturation can be performed on conventional or digital lateral cephalograms. The usage of digital radiography has several advantages–reduced radiation, there is no need for use of chemicals in order to make recordings, significantly improved precision of images, the possiblity of computer analysis of images, radiographs and the data analysis can be permanently stored (15). The usage of digital X-ray imaging in orthodontics has led to the development of several computer applications for assessing the cervical vertebral maturation (16, 17, 18).
This study was aimed to investigate the reliability of a computer application for assessment of the stages of cervical vertebra maturation for determining the stage of skeletal maturity.
2. MATERIALS AND METHODS
For this study, digital lateral cephalograms of 99 subjects (52 females and 47 males) were examined. All subjects were patients of the Department of Orthodontics, Faculty of Dentistry with Clinics, University of Sarajevo, who were seeking orthodontic treatment and who had never been treated. The following selection criteria were used during the sample composition: age between 9 and 16 years, absence of anomalies of the vertebrae, good general health, no history of trauma at the cervical region. Subjects with lateral cephalograms of low quality were excluded from the study. The study was approved by the Ethics Committee of the Faculty of Dentistry with Clinics, University of Sarajevo.
Assessment of individual skeletal maturity
Assessment of skeletal maturity was carried out using the cervical vertebral maturation index (CVMI), as proposed Hassel-Farman method(10), on digital lateral cephalograms. This method requires that the second, third and fourth cervical vertebrae (C2, C3 and C4) are analyzed according to their shape and classified into one of the six stages, which are defined as follows:
CVMI I – INITIATION – The lower borders of the second, third and fourth cervical vertebrae (C2, C3 and C4) are flat. The bodies of C3 and C4 are trapezoid in shap and the superior vertebral borders are tapered from posterior to anterior.
CVMI II – ACCELERATION – Concavities develop on inferior borders of C2 and C3, and inferior border of C4 is flat. The bodies of C3 and C4 are nearly rectangular in shape.
CVMI III – TRANSITION – Distinct concavities develop on inferior borders of C2 and C3, and concavity begins to develop on inferior border of C4. The bodies of C3 and C4 are rectangular.
CVMI IV – DECELERATION – Distinct concavities are seen on inferior borders of C2, C3 and C4. The vertebral bodies are becoming more square in shape.
CVMI V – MATURATION – More accentuated concavities are seen on inferior borders of C2, C3 and C4. The bodies of C3 and C4 are nearly square in shape.
CVMI VI – COMPLETION – Deep concavities are seen on inferior borders of C2, C3 and C4. The bodies of C3 and C4 are square, or greater in vertical dimension than in horizontal dimension.
An experienced orthodontist assessed the skeletal maturity, and after one month all measurements were repeated. The same orthodontist carried out the assessment of skeletal maturity with the computer application.
Computer application
In order to conduct the planned study, a computer application that enables to numerically assess the CVMI index was designed and developed (CephalometarHF V1, author:E.S.). The application was created using MATLAB programming language and deployed as a standalone executable file. The graphical user interface of the application is shown in Figure 1.
Figure 1.
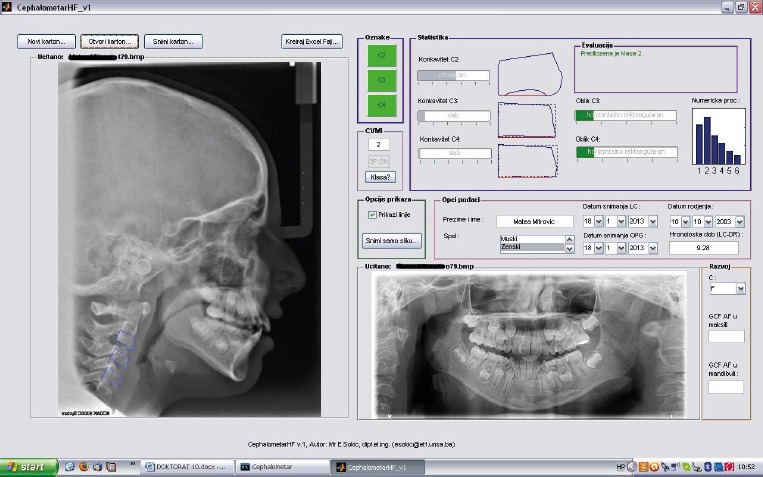
The graphical user interface of the computer application – CephalometarHF V1
The application can be used for collecting patient data in the form of a medical record. Patient generalities such as name, sex, birth date, radiographs (lateral cephalograms and orthopantomogram) are entered in the medical record by the doctor. The radiographs images are automatically presented in the application after loading. Moreover, some relevant patient information, such as his chronological age or name are preloaded or computed automatically from the available data (birth date, image file name), therefore the record fill-in time is significantly reduced. Medical records may be created, saved, loaded and edited at any time. In addition, records may be exported in MS Excel format, which facilitates the statistical analysis of the results.
In order to assess the correct CVMI stage, the previously acquired lateral cephalogram of the patient need to be loaded from the database. The application estimates the CVMI stage by analyzing the shapes and dimensions of the second, third and fourth cervical vertebrae.
The automatic cervical vertebrae shape extraction from radiological images is still a significantly hard technical task (19,20). Errors induced from inadequate image segmentation could lead to false CVMI class assessment, therefore we adopted the approach that the second, third and fourth vertebrae contours are marked manually by the doctor. Unlike similar developed application s(16,17,18), we propose to mark the entire contour instead of just few characteristical points. Thus, the shape features and characteristical points are extracted automatically and are more robust to marking errors.
The extracted contours are scale normalized and rotated for clearer presentation. The nominal orientation is determined using the axis of least inertia (21). The contours representing the cervical vertebrae (from C2 to C4) are rotated to vertical direction, in order to provide a more effective visualisation of the vertebrae shape. It is easier to assess the rectangularity of the shape if it is bounded by a horizontally placed box than if it is in its nominal orientation as on the original cephalometric image.
The application is able to independently propose a CVMI index based on the extracted vertebrae contours and it can be used to confirm or verify the doctor’s opinion. Therefore, the most important parameters for CVMI index assessment according to Hassel and Farman (10) are extracted and presented to the medical examiner: relative concavities of C2, C3 and C4, and shape rectangularity of C3 and C4. For the sake of simpler interpretation by the doctor, these measures are normalized and presented using filled bars and common language decription. For example, the concavity is described using: weak, developing, noticable, conspicouos, striking. Doctors found it extremely useful to operate with words than with parameters described by numbers. Other measures, such as the anterior and posterior height of C3 and C4, upper and lower length of C3 and C4, and lower length of C2 are extracted but not presented to the user.
The extracted parameters are used as inputs to the computer algorithm for automatic CVMI stage assessment. Due to the nature of computer processing which uses the exact bool logic and sharp mathematical relations in contrast to the frequent overlapping of CVMI stages (which are more frequently described using fuzzy logic instead of standard one), the procedure proposed by Hassel and Farman10 was slightly modified and adopted into a hybrid computer algorithm. The implemented algorithm of the application is presented in Figure 2. After contour extraction, the extracted parameters (C2,C3 and C4 concavities and C3 and C4 rectangularity) are used to classify the input image in two stages. First, the rectangularities of the shapes are used to roughly classify the input in one, two or three possible classes. In this stage, cases of patological shapes or errors in contour extraction may be detected and are classified as exceptions. Usually when an exception arise, the doctor simply repeats the contour tracing process more accurately. In the second stage, the image is further subclassified in the correct CVMI index based on the concavities of C2, C3 and C4. If a concavity measure does not match the class (e.g. no concavity on vertebrae exist while expecting CVMI VI), a correct CVMI index cannot be determined, hence an exception appears and the contour tracing should be repeated.
Figure 2.
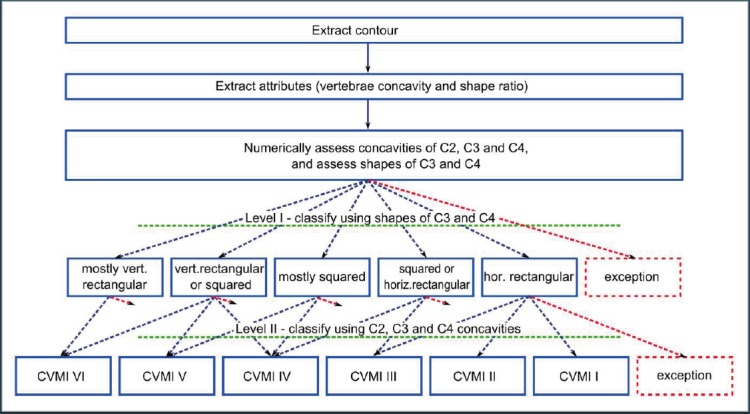
The simplified CVMI index determination algorithm
The assessment of the exact CVMI index can be impossible in some cases (patological case, or the patient is going through one CVMI index to another). Therefore, the patient does not seem to fit in one class only – it has some properties from one class and others from adjunct classes. As a consequence, the computer assessment, as well as the doctor assessment, may be uncertain to some level. In order to visually demonstrate the computer assessment to the doctor, the application uses a bar graph which indicated how reliable is the CVMI index determination.
For example, Figure 1. depicts the CVMI estimation results for one specific case. As it may be seen on the bargraph in upper-right part of the Figure 1., the application proposed CVMI stage II (dominantly based on slight concavity of C2 and C3, and rectangularity of C3 and C4). However, because of the noticeable concavity of C2 the CVMI could belong to stage III, or because of the missing concavity on C3 and C4 even in stage I. Therefore, the stage II is the recommended one, but the doctor should take the final decision. Nevertheless, the application assessment is that stages IV-VI are highly improbable.
3. RESULTS
Statistical analysis
SPSS software, version 20 was used to perform the statistical analyses. Evaluation of reliability analysis is tested by statistical Cohen Kappa test.
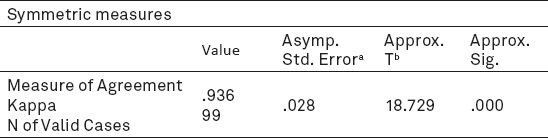
Kappa statistics testing the intra-examiner agreement, agreement between the first and second assessment of researcher, of the CVMI appraisal showed a value above 0.90 (Table 1).
Table 1.
Intra-examiner agreement.
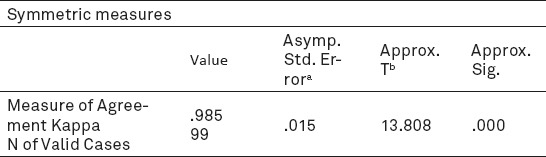
The analysis of compatibility assessment stage of maturation cervical vertebra between the computer application estimates and researcher’s estimates, revealed a almost perfect agreement, whereby the value of Cohen Kappa coefficient was k = 0.985. (Table 2).
Table 2.
Results of analysis of agreement between researcher and computer application
4. DISCUSSION
The hand-wrist radiograph has been used to assess stage of maturity of a child for a long time. To avoid taking additional radiographs, the cervical vertebral maturation method has become more popular method for assessment of skeletal maturity in recent years (3, 10, 11, 12, 13, 14, 16, 24).
In the present study the skeletal maturity was assessed on digital lateral cephalograms using CVMI method described by Hassel and Farman(10), which is designed to reliably ranking patients according to their remaining growth potential. This method takes into account morphological characteristics of the second, third and fourth cervical vertebrae (C2, C3 and C4).
All analyses were performed by one experienced orthodontist. To examine the intra-observer reliability, all radiographs were examined twice with an interval of one month between assessments.
The agreement evaluated using the statistical Cohen Kappa coefficient (k = 0.936) (Table 1). The results revealed that the reproducibility of the assessment of the cervical vertebral maturation in our rater was almost perfect, which indicates the precision of the examiner. Similar results have been shown in previous studies (12, 14, 18).
In addition, the assessment of skeletal maturity was performed using a computer application, specifically developed for this study. The aim of this study was to determine whether there exists agreement in the assessment of skeletal maturity between the computer application and the researcher, and to determine the reliability of computer assessment. The results showed that the assessment agree almost perfectly, with the value of Cohen Kappa coefficient k = 0.985 (Table 2).
Similar results were reported by Baptista et al., where the agreement between the classifier and researcher was almost perfect (k = 0.874), suggesting that the classifier is able to reproduce the estimate of researcher and evaluate stages of skeletal maturity, and moreover that the accurancy rate increases up to 90.42% when a deviation of one adjacent stage was taken into consideration (16). In contrast, our study have shown the disagreement between assessment of the computer application and the researcher in two cases, and it was deviation of one adjacent stage.
Hassel and Farman noted that in some cases it may be difficult to differentiate between two adjacent stages of skeletal bone maturation, and that this may not be clinically relevant. Skeletal maturation is a continuous process and skeletal maturity indicators (such as the hand-wrist radiograph and cervical vertebral maturation) are categorized by distinct events in this continuum. Each stage of maturation blends into the next, and it is sometimes difficult to differentiate borderline cases. Clinically, these differences should not be of great importance (10).
Future work
The application Cephalometar HF V1 may be improved in two directions.
First, additional efforts and testing need to be made in order to replace the manual cervical vertebrae contour tracing by an automatic one. However, simple image segmentation is not sufficient in this case. Cervical vertebrae image model needs to be developed in this case, accompanied by learning and adaptive mechanisms.
Secondly, the extracted shape contours allow to extract additional shape features (shape descriptors), which could give insight into vertebrae shape evolution through CVMI index. A mathematical model of shape evolution could be developed, therefore the proposed CVMI index10 would represent just discrete cases of such models.
5. CONCLUSION
Computer application Cephalometar HF V1 was developed with the intention to assist the orthodontist in the evaluation of cervical vertebral maturation index (CVMI). Study results indicate that the proposed computer application can help orthodontists to identify the stage of CVMI and can contribute toward greater diagnostic accuracy and better orthodontic treatment planning.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Malmgren O, Ömblus J, Hägg U, Pancherz H. Treatment with an orthopedic appliance system in relation to treatment intensity and growth periods. A study of initial effect. Am J Orthod Dentofacial Orthop. 1987;91:143–151. doi: 10.1016/0889-5406(87)90472-0. [DOI] [PubMed] [Google Scholar]
- 2.Faltin K, Faltin R, Baccetti T, Franchi L, Ghiozzi B, McNamara JA. Long-term Effectiveness and Treatment Timing for Bionator Therapy. Angle Orthod. 2003;73(3):221–230. doi: 10.1043/0003-3219(2003)073<0221:LEATTF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Baccetti T, Franchi L, McNamara JA. The Cervical Vertebral Maturation (CVM) Method for the Assessment of Optimal Treatment Timing in Dentofacial Orthopedics. Semin Orthod. 2005;11:119–129. [Google Scholar]
- 4.Silventoinen K, Haukka J, Dunkel L, Tynelius P, Rasmussen F. Genetics of Pubertal Timing and Its Associations With Relative Weight in Childhood and Adult Height:The Swedish Young Male Twins Study. Pediatrics. 2008;121:e885–e891. doi: 10.1542/peds.2007-1615. [DOI] [PubMed] [Google Scholar]
- 5.Parent AS, et al. The Timing of Normal Puberty and the Age Limits of Sexual Precocity:Variations around the World, Secular Trends, and Changes after Migration. Endocrine Reviews. 2003;24:668–693. doi: 10.1210/er.2002-0019. [DOI] [PubMed] [Google Scholar]
- 6.Proffit WR, Fields HW, Sarver DM. Ortodoncija. Zagreb: Naklada Slap; 2010. [Google Scholar]
- 7.Keresteš G, Brković I, Kuterovac Jagodić G. Mjerenje pubertalnog sazrijevanja u istraživanjima adolescenata. Društvena istraživanja. 2010;19(6(110)):933–951. [Google Scholar]
- 8.Fishman LS. Radiographic Evaluation of Skeletal Maturation. A Clinically Oriented Method Based on Hand-Wrist Films. Angle Orthod. 1982;52:88–112. doi: 10.1043/0003-3219(1982)052<0088:REOSM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Björk A, Helm S. Prediction of the Age of Maximum Pubertal Growth in Body Height. Angle Orthod. 1967;37(2):134–143. doi: 10.1043/0003-3219(1967)037<0134:POTAOM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Hassel B, Farman AG. Skeletal maturation evaluation using cervical vertebrae. Am J Orthod Dentofac Orthop. 1995;107:58–66. doi: 10.1016/s0889-5406(95)70157-5. [DOI] [PubMed] [Google Scholar]
- 11.Flores-Mir C, Burgess CA, Champney M, Jensen RJ, Pitcher MR, Major PW. Correlation of Skeletal Maturation Stages Detemined by Cervical Vertebrae and Hand-wrist Evaluations. Angle Orthod. 2006;76(1):1–5. doi: 10.1043/0003-3219(2006)076[0001:COSMSD]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Gandini P, Mancini M, Andreani F. A Comparasion of Hand-wrist Bone and Cervical Vertebral Analyses in Measuring Skeletal Maturation. Angle Orthod. 2006;76(6):984–989. doi: 10.2319/070605-217. [DOI] [PubMed] [Google Scholar]
- 13.Uysal T, Ramoglu SI, Basciftci FA, Sari Z. Chronological age and skeletal maturation of the cervical vertebrae and hand-wrist:Is there a relationship? Am J Orthod Dentofacial Orthop. 2006;130:622–628. doi: 10.1016/j.ajodo.2005.01.031. [DOI] [PubMed] [Google Scholar]
- 14.Mahajan S. Evaluation of skeletal maturation by comparing the hand wrist radiograph and cervical veretbrae as seen in lateral cephalogram. Indian J Dent Res. 2011;22:309–316. doi: 10.4103/0970-9290.84310. [DOI] [PubMed] [Google Scholar]
- 15.van der Stelt PF. Better Imaging:The Advantages of Digital Radiography. JADA. 2008;139(suppl.3):7S–13S. doi: 10.14219/jada.archive.2008.0357. [DOI] [PubMed] [Google Scholar]
- 16.Baptista RS, Quaglio CL, Mourad LMEH, Hummel AD, Caetano CAC, Ortolani CLF, Pisa IT. A semi-automated method for bone age assessment using cervical vertebral maturation. Angle Orthod. 2012;82:658–662. doi: 10.2319/070111-425.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sokic E, Tiro A, Sokic-Begovic E, Nakas E. Semi-automatic Assessment of Cervical Vertebral Maturation Stages using Cephalograph Images and Centroid-based Clustering. Acta Stomatol Croat. 2012;46(4):280–290. [Google Scholar]
- 18.Santiago RC, Cunha AR, Júnior GC, Fernandes N, Campos MJS, Costa LFM, Vitral RWF, Bolognese AM. New software for cervical vertebral geometry assessment and its relationship to skeletal maturation – a pilot study. Dentomaxillofaci Radiol. 2014;43:20130238. doi: 10.1259/dmfr.20130238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahmoudi A, Lecron F, Manneback P, Benjelloun M, Mahmoudi S. GPU-based segmentation of cervical vertebra in X-ray images. Proceedings of IEEE International Conference on Cluster Computing Wokshops and Poster. 2010 Sep 20-24; Heraklion, Crete. [Google Scholar]
- 20.Tezmol A, Sari-Sarraf H, Mitra S, Long R, Gururajan A. Customized Hough Transform for Robust Segmentation of Cervical Vertebrae from X-Ray Images. In: Proceedings of 5th IEEE. Southwest Symposium on Image Analysis and Interpretation. 2002 Apr 07-09;:224. Santa Fe, NM. [Google Scholar]
- 21.Yang M, Kpalma K, Ronsin J. A Survey of Shape Feature Extraction Techniques. Peng-Yang Yin. Pattern Recognition. IN-TECH. 2008:43–90. [Google Scholar]
- 22.Flores-Mir C, Nebbe B, Major PW. Use of Skeletal Maturation Based on Hand-Wrist Radiographic Analysis as a Predictor of Facial Growth:A Systematic Review. Angle Orthod. 2004;74(1):118–124. doi: 10.1043/0003-3219(2004)074<0118:UOSMBO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Lamparski DG. Skeletal Age Assessment Utilizing Cervical Vertebrae. [Master’s thesis] 1972. An Improved Version of the Cervical Vertebral Maturation (CVM) Method for the Assessment of Mandibular Growth. In: Baccetti T, Franchi L, McNamara JA, editors. Angle Orthod. Vol. 72. Pittsburgh, Penn: Deperatment of Orthodontics, The University of Pittsburgh; 2002. pp. 316–323. [DOI] [PubMed] [Google Scholar]
- 24.Perinetti G, Caprioglio A, Contardo L. Visual assessment of the cervical vertebral maturation stages. A study of diagnostic accurancy and repeability. Angle Orthod. 2014;84:951–956. doi: 10.2319/120913-906.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


