Abstract
Background and Objectives
Prognostic value of additional carotid Doppler evaluations to carotid intima-media thickness (IMT) and plaque has not been completely evaluated.
Subjects and Methods
A total of 1119 patients with risk factors for, but without, overt coronary artery disease (CAD), who underwent both carotid ultrasound and Doppler examination were included in the present study. Parameters of interest included peak systolic and end-diastolic velocities, resistive indices of the carotid arteries, IMT, and plaque measurements. The primary end-point was all-cause cerebro-cardiovascular events (CVEs) including acute myocardial infarction, coronary revascularization therapy, heart failure admission, stroke, and cardiovascular death. Model 1 covariates comprised age and sex; Model 2 also included hypertension, diabetes and smoking; Model 3 also had use of aspirin and statin; and Model 4 also included IMT and plaque.
Results
The mean follow-up duration was 1386±461 days and the mean age of the study population was 60±12 years. Amongst 1119 participants, 43% were women, 57% had a history of hypertension, and 23% had diabetes. During follow-up, 6.6% of patients experienced CVEs. Among carotid Doppler parameters, average common carotid artery end-diastolic velocity was the independent predictor for future CVEs after adjustments for all models variables (HR 0.95 per cm/s, 95% confident interval 0.91-0.99, p=0.034 in Model 4) and significantly increased the predictive value of Model 4 (global χ2=59.0 vs. 62.8, p=0.029).
Conclusion
Carotid Doppler measurements in addition to IMT and plaque evaluation are independently associated with future CVEs in asymptomatic patients at risk for CAD.
Keywords: Carotid arteries, Doppler, Events
Introduction
Common carotid artery (CCA) intima-media thickness (IMT) and the presence of plaque have been accepted as good vascular prognostic biomarkers, not only for future cerebrovascular events, but also for cardiovascular events in patients with coronary risk factors.1,2,3) However, the internal carotid artery (ICA) and external carotid artery (ECA) comprise a significant portion of the carotid arterial system. In particular, the ICA is a critically essential component of the cerebral circulation, and complete evaluation of the ICA is therefore important. A comprehensive carotid Doppler evaluation is commonly included in the protocol of screening carotid evaluations, in addition to CCA-IMT and CCA plaque assessments.4) It can provide information about pulsatility3) of the carotid arterial system and resistance of the intracerebral circulation, which cannot easily be evaluated with brain magnetic resonance imaging or magnetic resonance angiography. Although velocity in the ICA has been shown to predict significant stenosis in the distal ICA, and pulsatility measured by resistive index has been used in cerebral blood flow evaluations, even in patients without previous cerebrovascular events,5) some guidelines insist against screening carotid Doppler evaluations in addition to CCA-IMT and plaque evaluations.6) However, its role as an imaging biomarker of future cerebro-cardiovascular events (CVEs) has not been fully studied, and whether it can provide additional information to CCA-IMT and plaque evaluations has not been reported. In this study, we therefore sought to evaluate the prognostic value of comprehensive carotid Doppler measurements obtained in addition to CCA-IMT and plaque measurements in patients without coronary artery disease (CAD).
Subjects and Methods
Study population and study protocols
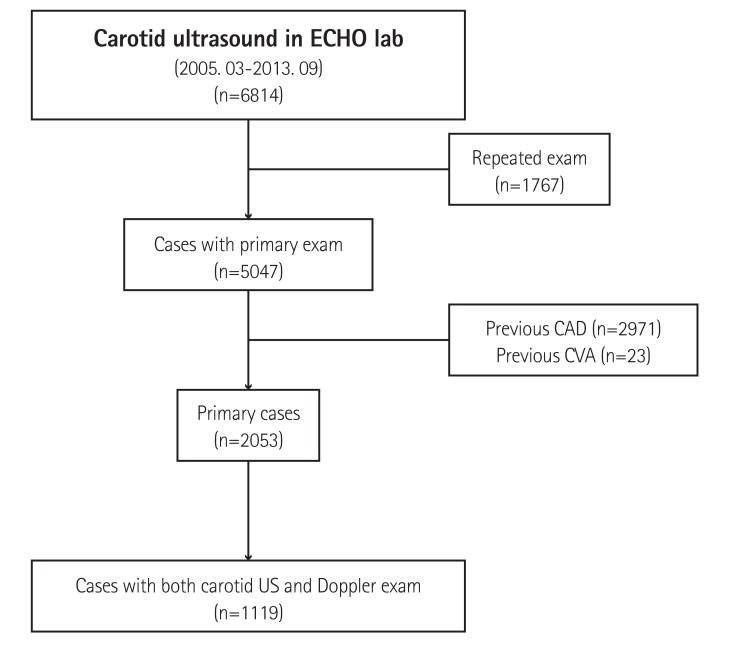
This was a single center registry study. Carotid ultrasound image acquisition was conducted between March 2005 and September 2013. During this period, all carotid ultrasounds and Doppler evaluations were conducted in the echocardiography laboratory at the Gangnam Severance Hospital, Yonsei University. A total of 6814 carotid ultrasound evaluations were undertaken, and after excluding patients, who underwent repeat examinations (n=1767), a total of 5047 patients underwent carotid IMT with plaque evaluations of the CCA and full carotid Doppler evaluations. Patients who had previously documented CAD (n=2971) or stroke (n=23) were also excluded from the investigation, and the remaining 2053 patients were enrolled in this study. Among them, 1119 patients had data for carotid IMT, plaque, and full carotid Doppler evaluations (Fig. 1); 991 patients had data for conventional echocardiography performed within 1 month of carotid ultrasound evaluations; and 603 patients underwent C-reactive protein level assessments. Clinical history, medications, and medical records were reviewed and collected by a study coordinator who was blinded to the carotid Doppler data. Clinical follow-ups were conducted by reviewing medical records or through telephone interview. The primary end-point was all-cause CVEs including acute myocardial infarction, coronary revascularization therapy, heart failure admission, stroke, and cardiovascular death. The study protocol was approved by the institutional review board of our hospital, and the need for informed consent was waived due to the retrospective nature of this study.
Fig. 1. Schematic presentation of study population. ECHO: echocardiography, CAD: coronary artery disease, CVA: cerebrovascular accident, US: ultrasound.
Carotid ultrasonography
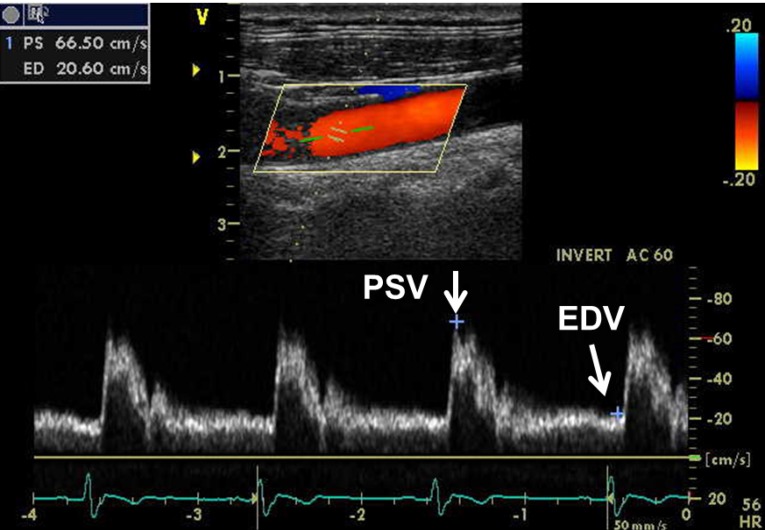
The carotid arteries were examined using a standardized protocol.7) Ultrasonographic images were acquired in end-diastole (defined as the R wave of an electrocardiogram) by sonographers certified by the Registry of Diagnostic Cardiac Sonographers, equipped with an 11-MHz imaging transducer (Vivid-7, Vivid E9 [GE, Milwaukee, WI, USA], SC2000 [Siemens, Mountain View, CA, USA], Sonos 7500 or iE33 [Philips, Andover, MA, USA]). With the subject in the supine position and with slight hyperextension of the neck, the CCA, carotid bulb, extracranial ICA, ECA, and vertebral arteries were identified. All carotid measurements were performed by semi-automated vessel-wall detection software. Following short-axis 2D image acquisition of the CCA, long-axis B-mode ultrasound images were acquired for the subsequent measurements. Carotid measurements included IMT of the far vessel wall at a site approximately 1 cm in distance, proximal to the carotid bulb. Averaged IMT values of the left and right CCAs were subsequently used in all analyses. Plaque was defined as a protrusion of the vessel wall into the arterial lumen of at least 0.5 mm, with an IMT 50% that of the surrounding sites or an IMT>1.5 mm. Peak systolic velocity and end-diastolic velocity were measured in the CCA, ECA, and ICA using a semi-automatic analysis system. The resistive index (RI) was calculated as PSV-EDV/PSV, where PSV indicates peak systolic velocity and EDV indicates end-diastolic velocity5),8) (Fig. 2). In cases with atrial fibrillation, average values of consecutive five beats were used for the analysis. To evaluate reliability between two different vendors (iE33 [Philips, Andover, MA, USA] and Vivid E9 [GE, Milwaukee,WI, USA]), we performed repeated carotid examination for CCA-IMT, CCA-PSV and CCA-EDV in five cases.
Fig. 2. Schematic presentation of Doppler findings of common carotid artery. PSV: peak systolic velocity, EDV: end-diastolic velocity.
Statistical analysis
Continuous variables are expressed as mean±standard deviation and categorical variables are expressed as frequencies (percentage). The intraclass correlation coefficient was obtained for the reliability test. For correlation analysis, Pearson correlation coefficient was used. Receiver operating characteristic (ROC) analysis was used to determine optimal cut-off values for all composite CVEs. The best cut-off value was defined as the point with the highest sum of the sensitivity and specificity. The overall event-free survival rates were calculated using Kaplan-Meier analysis and the event rates were compared using a log-rank test. Multivariable Cox proportional-hazards models were generated with the candidate variables and for probability distribution of the carotid ultrasound time to composite CVEs, the models included conventional risk factors and carotid ultrasound-derived indices (with continuous variable) as covariates. Significant variables identified in univariate analysis (p<0.05), or clinically important variables were included in the multiple Cox regression analysis. The incremental prognostic value of covariates was assessed by monitoring step-wise changes in Chi-square values of the Cox proportional-hazards model. We evaluated and compared the fitness, statistical results, and interpretation of findings obtained using the following models. Model 1 included age and sex (demographics); Model 2 included history of hypertension, diabetes, and smoking status (risk factors) in addition to Model 1 variables; Model 3 included aspirin use and statin use (medications) in addition to Model 2 variables; and Model 4 included IMT and presence of plaque (imaging markers) in addition to Model 3 variables. All statistical analyses were performed using SPSS (version 20.0, IBM Inc., Chicago, IL, USA). Two-sided p<0.05 were considered significant.
Results
Baseline characteristics
The mean age of the study population was 60.3±12.4 years. Of the participants, 483 (43%) were women, 637 (57%) had a history of hypertension and 262 (23%) had diabetes. Fifty-eight cases (5%) had atrial fibrillation and mean LV ejection fraction was 65.4±8.7 % in 988 cases based on echocardiography data. Of them, 46 (4.6%) cases had LV ejection fraction lower than 50%. Baseline characteristics and medical history of the study population are described in Table 1.
Table 1. Baseline clinical characteristics of subjects.
| Total | Women (n=483) |
Men (n=636) |
p | |
|---|---|---|---|---|
| Age (years) | 60.3±12.4 | 61.8±12.1 | 59.1±12.5 | <0.001 |
| BUN (mg/dL) | 16.5±8.9 | 14.9±5.5 | 17.6±10.6 | <0.001 |
| Cr (mg/dL) | 1.01±0.73 | 0.81±0.23 | 1.16±0.91 | <0.001 |
| HDL-C (mg/dL) | 46.5±12.6 | 50.3±12.4 | 43.7±12.1 | <0.001 |
| LDL-C (mg/dL) | 107.0±33.5 | 110.2±34.0 | 104.7±33.1 | 0.023 |
| SBP (mmHg) | 127.1±19.5 | 127.3±19.5 | 127.0±19.5 | 0.846 |
| DBP (mmHg) | 76.6±13.0 | 75.5±12.3 | 77.3±13.5 | 0.053 |
| Pulse pressure (mmHg) | 50.5±14.3 | 51.7±14.8 | 49.6±13.8 | 0.042 |
| Diabetes | 262 (23) | 105 (22) | 157 (25) | 0.255 |
| Hypertension | 637 (57) | 273 (57) | 364 (57) | 0.855 |
| Current smoking | 214 (20) | 14 (3.1) | 200 (33) | <0.001 |
| Aspirin use | 676 (60) | 269 (56) | 407 (64) | 0.005 |
| Statin use | 437 (39) | 184 (38) | 253 (40) | 0.578 |
Data are expressed as mean±standard deviation or number (%). BUN: blood urea nitrogen, Cr: creatinine, HDL-C: high-density lipoprotein cholesterol, LDLC: low-density lipoprotein cholesterol, SBP: systolic blood pressure, DBP: diastolic blood pressure
Carotid ultrasound and Doppler indices
The averages of the right and left CCA-IMT were 0.68±0.18 mm and 0.69±0.17 mm, respectively. The average value of both-sides of the CCA-IMT of men was thicker than women (0.70±0.16 mm vs. 0.67±0.14 mm, respectively, p=0.004). Plaques were present in 539 (48%) cases, with a higher prevalence in men than in women (340 [54%] vs. 199 [41%], p<0.001). Average PSV, EDV, and RI values of the CCA were 75.3±19.8 cm/s, 18.7±6.8 cm/s, and 0.75±0.07, respectively, and those of the ICA were 59.7±20.6 cm/s, 21.7±8.3 cm/s, and 0.63±0.08, respectively. In comparison to women, PSVs of the CCA and ICA were higher in men, while the EDV-CCA was lower, and therefore the RI of the CCA and ICA was higher in men. All carotid ultrasound and Doppler parameters are described in Table 2. CCA-EDV was inversely correlated with age (r=-0.390, p<0.001) and IMT (r=-0.222, p<0.001). Patients with any carotid plaque had significantly lower CCA-EDV (p<0.001). CCA-EDV was significantly lower and RI was significantly higher in patients with diabetes (16.36±6.23 cm/s vs. 19.41±6.81 cm/s; 0.77±0.07 vs. 0.74±0.07, all p<0.001; respectively) and hypertension (17.7±6.41 cm/s vs. 20.1±7.1 cm/s, p<0.001; 0.76±0.07 vs. 0.74±0.07, p=0.002; respectively). Additionally, CCA-EDV was significantly correlated with left ventricular mass index (r=-0.246, p<0.001), left atrial volume index (r=-0.252, p<0.001), E/e' (r=-0.315, p<0.001), and right ventricular systolic pressure (r=-0.195, p<0.001). In sub-group analysis, CCA-EDV was significantly correlated with C-reactive protein levels (r=-0.202, p<0.001).
Table 2. Carotid ultrasound indices.
| Total | Women (n=483) |
Men (n=636) |
p | |
|---|---|---|---|---|
| Carotid IMT-right (mm) | 0.68±0.18 | 0.67±0.15 | 0.69±0.19 | 0.019 |
| Carotid IMT-left (mm) | 0.69±0.17 | 0.68±0.15 | 0.71±0.18 | 0.004 |
| Carotid IMT-average (mm) | 0.69±0.15 | 0.67±0.14 | 0.70±0.16 | 0.004 |
| Presence of plaques | 539 (48) | 199 (41) | 340 (54) | <0.001 |
| CCA-PSV-average (cm/s) | 75.3±19.8 | 71.8±17.1 | 77.9±21.2 | <0.001 |
| CCA-EDV-average (cm/s) | 18.7±6.8 | 19.5±6.9 | 18.1±6.7 | <0.001 |
| CCA-RI-average | 0.75±0.07 | 0.73±0.07 | 0.77±0.06 | <0.001 |
| ICA-PSV-average (cm/s) | 59.7±20.6 | 58.3±17.1 | 60.8±22.9 | 0.034 |
| ICA-EDV-average (cm/s) | 21.7±8.3 | 21.8±7.9 | 21.6±8.5 | 0.635 |
| ICA-RI-average | 0.63±0.08 | 0.62±0.08 | 0.64±0.08 | 0.005 |
| ECA-PSV-average (cm/s) | 75.0±25.6 | 70.1±22.4 | 78.8±27.2 | <0.001 |
| ECA-EDV-average (cm/s) | 13.7±6.0 | 13.2±6.1 | 14.1±6.0 | 0.026 |
| ECA-RI-average | 0.81±0.07 | 0.81±0.07 | 0.81±0.07 | 0.138 |
Data are expressed as mean±standard deviation or number (%). IMT: intima-media thickness, CCA: common carotid artery, PSV: peak systolic velocity, EDV: end-diastolic velocity, RI: resistive index, ICA: internal carotid artery, ECA: external carotid artery
Follow-up results
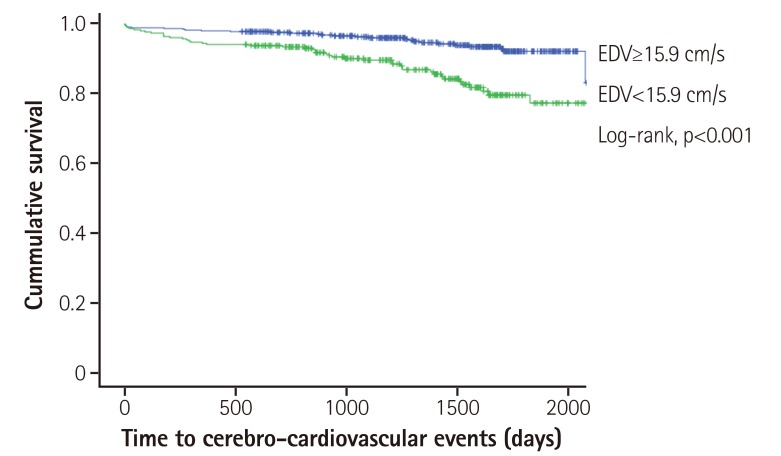
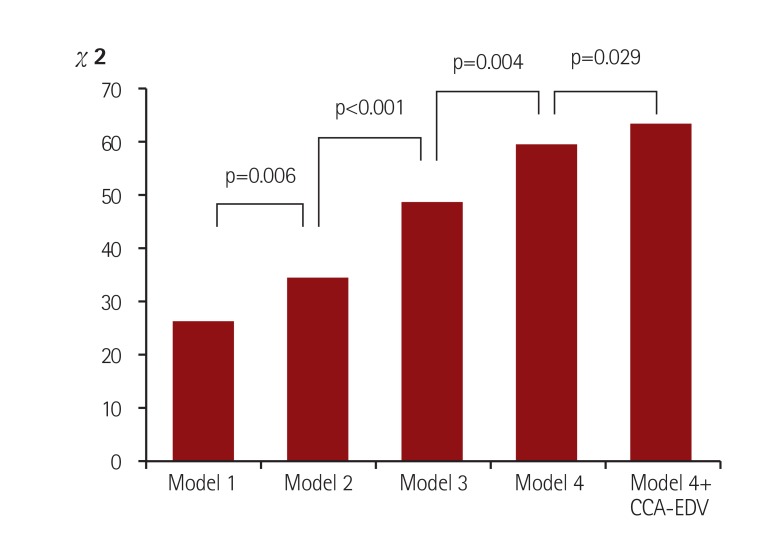
The mean duration of follow-up was 1386±461 days. During the follow-up period, 74 (6.6%) composite CVEs occurred. Among these cases, four were newly developed acute myocardial infarctions, six were classified as unstable angina, 28 included those that needed additional coronary revascularization therapy without acute coronary syndrome, 23 were classified as cerebral infarctions or transient ischemic attacks, eight were admitted due to heart failure, and five were cardiovascular-related deaths. In univariate analysis, older age, male sex, smoking, aspirin use, and statin use were significantly related to all CVEs. Among carotid ultrasound-related parameters, presence of CCA-plaque, lower CCA-PSV and CCA-EDV, and higher RI were related to future CVEs. Thicker CCA-IMT was marginally related to CVEs (Table 3). In ROC analysis, area under curve was 0.658 and the optimal cut-off CCA-EDV was 15.9 cm/s (sensitivity=0.624 and specificity=0.622). On Kaplan-Meier analysis, the group with lower CCA-EDV (<15.9 cm/s) demonstrated higher CVEs (p<0.001 on Log-Rank test; Fig. 3). In multivariable analysis, smoking, statin use, presence of CCA-plaque, and lower CCA-EDV (with continuous variable) were independently related to composite CVEs (Table 3). With step-wise adjustment in multiple modeling, CCA-EDV exhibited significance in all the Models (Table 4). In addition, CCA-EDV provided incremental prognostic value in addition to Model 4 variables (demographics, clinical risk factors, medications, and carotid imaging markers) (global χ2 of Model 4 vs. Model 4+CCA-EDV was 59.0 vs. 62.8, respectively, p=0.029) (Fig. 4). CCA-EDV also remained significant in univariate analysis and after adjustment for Model 1 and Model 2 variables, but was less significant after adjustment for Model 3 and Model 4 variables for cardiovascular events without cerebrovascular events (Supplementary Table in the online-only Data Supplement). However, CCA-EDV did not reach statistical significance for the prediction of cerebrovascular events (p=0.060). In subgroup analysis in each sex, although CCA-EDV was related to CVEs in univariate analysis (p=0.004 in men and p=0.002 in women), it was not significant in multivariable analysis (p=0.067 in Model 3 in men; p=0.471 in Model 1 in women).
Table 3. Predictors for all composite cerebro-cardiovascular events.
| Univariate analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | |
| Age (per 1 year) | 1.05 | 1.03-1.07 | <0.001 | 0.74 | 0.40-1.37 | 0.341 |
| Sex (1=men) | 1.65 | 1.01-2.69 | 0.044 | 1.03 | 1.01-1.06 | 0.020 |
| Hypertension | 1.38 | 0.84-2.25 | 0.203 | 0.89 | 0.53-1.51 | 0.668 |
| Diabetes | 1.51 | 0.93-2.32 | 0.097 | 1.16 | 0.70-1.93 | 0.568 |
| Smoking | 1.48 | 1.13-1.93 | 0.005 | 1.79 | 1.26-2.54 | 0.001 |
| Aspirin use | 2.61 | 1.46-4.68 | 0.001 | 1.55 | 0.82-2.93 | 0.195 |
| Statin use | 2.75 | 1.70-4.46 | <0.001 | 1.96 | 1.17-3.28 | 0.010 |
| Presence of plaque (0, 1) | 4.59 | 2.60-8.10 | <0.001 | 0.31 | 0.06-1.71 | 0.313 |
| IMT (per 1 mm) | 3.64 | 0.95-14.0 | 0.060 | 2.77 | 1.45-5.23 | 0.002 |
| CCA-PSV (per cm/s) | 0.98 | 0.97-0.99 | 0.002 | 0.95 | 0.91-1.00 | 0.032 |
| CCA-EDV (per cm/s) | 0.92 | 0.88-0.95 | <0.001 | 0.99 | 0.97-1.00 | 0.044 |
| CCA-RI | 74.27 | 2.52-2184.91 | 0.013 | 2.07 | 0.04-101.32 | 0.714 |
| ICA-PSV (per cm/s) | 1.01 | 0.99-1.02 | 0.268 | |||
| ICA-EDV (per cm/s) | 0.99 | 0.97-1.03 | 0.806 | |||
| ICA-RI | 8.69 | 0.55-138.21 | 0.126 | |||
HR: hazard ratio, CI: confidence interval, IMT: intima-media thickness, CCA: common carotid artery, PSV: peak systolic velocity, EDV: end-diastolic velocity, RI: resistive index, ICA: internal carotid artery
Fig. 3. Kaplan-Meier survival curve. The group with lower CCA-EDV (<15.9 cm/s) has higher cerebro-cardiovascular events. CCA: common carotid artery, EDV: end-diastolic velocity.
Table 4. Predictive value of CCA-EDV for composite cerebro-cardiovascular events after adjustment for model variables.
| HR | 95% CI | p | |
|---|---|---|---|
| Model 1 | 0.946 | 0.905-0.988 | 0.012 |
| Model 2 | 0.947 | 0.906-0.990 | 0.016 |
| Model 3 | 0.950 | 0.909-0.993 | 0.023 |
| Model 4 | 0.953 | 0.911-0.996 | 0.032 |
Model 1 included CCA-EDV, age and sex (demographics); Model 2 included history of hypertension, diabetes, and smoking status (risk factors) in addition to Model 1 variables; Model 3 included aspirin use and statin use (medications) in addition to Model 2 variables; and Model 4 included IMT and presence of plaque (imaging markers) in addition to Model 3 variables. In all the models, CCA-EDV was included. CCA: common carotid artery, EDV: end-diastolic velocity, HR: hazard ratio, CI: confidence interval
Fig. 4. Incremental prognostic value of CCA-EDV for cerebro-cardiovascular events. Model 1 included age and sex (demographics); Model 2 included history of hypertension, diabetes, and smoking status (risk factors) in addition to Model 1 variables; Model 3 included aspirin use and statin use (medications) in addition to Model 2 variables; and Model 4 included IMT and presence of plaque (imaging markers) in addition to Model 3 variables. CCA: common carotid artery, EDV: end-diastolic velocity, IMT: intima-media thickness.
Inter-test reliability
Average intraclass correlation coefficient of CCA-IMT was 0.945 (p=0.008), CCA-PSV was 0.854 (p=0.044) and CCA-EDV was 0.901 (p=0.023).
Discussion
In this study, we found that among the carotid Doppler indices assessed, higher RI, and lower CCA-PSV and CCA-EDV, but not ICA Doppler indices, were related to future CVEs. In addition, CCA-EDV was related to future CVEs in a manner independent of clinical risk factors, CCA-IMT, and presence of plaque in the CCA. Our results support full carotid Doppler evaluation in addition to CCA-IMT and carotid plaque evaluation as a screening tool for risk stratification in patients without previous CAD.
Additional prognostic value of carotid Doppler index
In this study, the strongest predictor for future CVEs was the presence of carotid plaques. As expected, IMT was also marginally significant in addition to age, smoking, aspirin use, and statin use. Although carotid Doppler indices are related to age, sex, blood pressure, carotid IMT, and the presence of carotid plaque, CCA-EDV is independently related to composite vascular events. Few studies have dealt with the predictive value of carotid Doppler findings for future cardiovascular events. In a previous meta-analysis study, carotid bruit, which is indicative of carotid stenosis, has been shown to be related to cardiovascular events, although this analysis did not include measurements of carotid Doppler indices.9) In another study, it was shown that CCA-EDV is related to future ischemic stroke in a Taiwanese population.10) Nevertheless, the evidence provided by existing studies is limited. Previous guidelines that advise against carotid Doppler evaluations for screening are based on meta-analysis results on screening asymptomatic carotid artery stenosis for the prediction of cerebrovascular events. The main reason for this exclusion likely stems from a low overall prevalence rate of treatable disease in the general asymptomatic population and harms from treatment such as carotid endarterectomy.6) Therefore, the significance of full carotid-Doppler evaluations for total atherosclerotic cerebro-cardiovascular disease, and not just for cerebrovascular disease, has not been well evaluated. Our results suggest that the negative indications for a screening carotid Doppler examination, based on a low incidence of pure cerebrovascular disease in other studies, can be overcome when extended to total CVEs.
Potential mechanisms related to prognosis
CCA-EDV, as an index of intracerebral artery resistance, can be an additive prognostic marker, as it reflects intracerebral atherosclerosis. Although CCA-IMT and plaque can be easily measured, the degree of atherosclerosis in the distal cerebrovascular system cannot easily be evaluated with conventional 2D ultrasound systems due to limited range of tracking and limited windows for accurate visualization of the distal ICA or intracranial circulation. Instead, Doppler examination of the CCA is easily measured in subjects, with good reproducibility. This merit might induce better results from CCA Doppler examination rather than ICA Doppler examination. Although CCA-EDV was significantly affected by age, hypertension, CCA-IMT, and the presence of CCA-plaque in this study, its prognostic value was found to be independent of them. Our result is consistent with that of a previous study undertaken in an Asian population,10) in which lower CCA-EDV was related to a higher incidence of ischemic stroke. Our result may be driven by the inclusion of ischemic cerebrovascular events as a component of the composite end-point; however, even after excluding new onset cerebrovascular events, the relationship remained significant. A potential explanation is that lower EDV may be a sign of aging. Indeed, vascular aging is thought to be associated with the deterioration of elastic wall properties with vascular stiffening.11) Therefore, EDV can be regarded as an index of carotid arterial stiffness as it modulates afterload and affects the ventricular-vascular relationship. Our results of significant correlations between CCA-EDV and diastolic functional parameters such as the left atrial volume index, left ventricular mass index, and E/e' support the theory of ventricular-vascular coupling. In our study, CCA-EDV was more relevant to CVEs than ICA-EDV, which could partly be explained by the elastic arterial wall properties of the CCA as compared to the muscular arterial wall properties of the ICA.12) Therefore, CCA-EDV can be a surrogate marker of early elastic artery stiffening even without increases in IMT or plaque. A more recent study showed that lower EDV in CCA, at least in part, depends on the degree of peripheral arterial stiffness.13) In addition, CCA hemodynamics has been shown to be associated with serum interleukin-6 and high-sensitivity C-reactive protein levels in hypertensive patients. These results indicate that hemodynamic alterations of the carotid artery can also be a useful marker of atherosclerosis, which is as an inflammatory disease,14) and our study result of a significant correlation between C-reactive protein level and CCA-EDV also supports this possible explanation.
Study limitations
Although the present study results support the significant prognostic implications of additional carotid Doppler evaluations in asymptomatic individuals, some study limitations remain to be addressed. First, as this was not a prospectively designed and conducted study, some patients might have had missing values or might have been lost to follow-up. Second, because this study was conducted in a tertiary referral hospital, the ratio of associated risk factors and medication use would be higher than that expected in the general population. The applicability of the present findings to general population screening programs therefore requires further, well-controlled, prospective population-based studies. Third, due to relatively small number of events, number of covariates in model 4 is quite high that might have over-fitting problem. Fourth, evaluation for true predictive value or prognostic value of carotid Doppler index needs well controlled prospective study and additional discrimination analysis.
Acknowledgments
This work was supported with a research grant (2012) from the Korean Society of Circulation (201203-11).
Footnotes
The authors have no financial conflicts of interest.
Supplementary Materials
The online-only Data Supplement is available with this article at http://dx.doi.org/10.4070/kcj.2016.46.1.72.
Predictive value of CCA-EDV for composite cardiovascular events, in which cerebrovascular events were excluded
References
- 1.Polak JF, Pencina MJ, Pencina KM, O'Donnell CJ, Wolf PA, D'Agostino RB., Sr Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med. 2011;365:213–221. doi: 10.1056/NEJMoa1012592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK., Jr Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 3.Yuk HB, Park HW, Jung IJ, et al. Analysis of carotid ultrasound findings on cardiovascular events in patients with coronary artery disease during seven-year follow-up. Korean Circ J. 2015;45:28–37. doi: 10.4070/kcj.2015.45.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grant EG, Benson CB, Moneta GL, et al. Carotid artery stenosis: gray-scale and Doppler US diagnosis--Society of Radiologists in Ultrasound Consensus Conference. Radiology. 2003;229:340–346. doi: 10.1148/radiol.2292030516. [DOI] [PubMed] [Google Scholar]
- 5.Bai CH, Chen JR, Chiu HC, Pan WH. Lower blood flow velocity, higher resistance index, and larger diameter of extracranial carotid arteries are associated with ischemic stroke independently of carotid atherosclerosis and cardiovascular risk factors. J Clin Ultrasound. 2007;35:322–330. doi: 10.1002/jcu.20351. [DOI] [PubMed] [Google Scholar]
- 6.Wolff T, Guirguis-Blake J, Miller T, Gillespie M, Harris R. Screening for carotid artery stenosis: an update of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2007;147:860–870. doi: 10.7326/0003-4819-147-12-200712180-00006. [DOI] [PubMed] [Google Scholar]
- 7.Stein JH, Korcarz CE, Hurst RT, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008;21:93–111. doi: 10.1016/j.echo.2007.11.011. quiz 189-90. [DOI] [PubMed] [Google Scholar]
- 8.Beach KW, Leotta DF, Zierler RE. Carotid Doppler velocity measurements and anatomic stenosis: correlation is futile. Vasc Endovascular Surg. 2012;46:466–474. doi: 10.1177/1538574412452159. [DOI] [PubMed] [Google Scholar]
- 9.Pickett CA, Jackson JL, Hemann BA, Atwood JE. Carotid bruits as a prognostic indicator of cardiovascular death and myocardial infarction: a meta-analysis. Lancet. 2008;371:1587–1594. doi: 10.1016/S0140-6736(08)60691-1. [DOI] [PubMed] [Google Scholar]
- 10.Chuang SY, Bai CH, Chen JR, et al. Common carotid end-diastolic velocity and intima-media thickness jointly predict ischemic stroke in Taiwan. Stroke. 2011;42:1338–1344. doi: 10.1161/STROKEAHA.110.605477. [DOI] [PubMed] [Google Scholar]
- 11.Dijk JM, Algra A, van der Graaf Y, Grobbee DE, Bots ML SMART study group. Carotid stiffness and the risk of new vascular events in patients with manifest cardiovascular disease. The SMART study. Eur Heart J. 2005;26:1213–1220. doi: 10.1093/eurheartj/ehi254. [DOI] [PubMed] [Google Scholar]
- 12.Janzen J. The microscopic transitional zone between elastic and muscular arteries. Arch Mal Coeur Vaiss. 2004;97:909–914. [PubMed] [Google Scholar]
- 13.Barutcu I, Esen AM, Degirmenci B, et al. Acute cigarette smoking-induced hemodynamic alterations in the common carotid artery--a transcranial Doppler study-- Circ J. 2004;68:1127–1131. doi: 10.1253/circj.68.1127. [DOI] [PubMed] [Google Scholar]
- 14.Manabe S, Okura T, Watanabe S, Higaki J. Association between carotid haemodynamics and inflammation in patients with essential hypertension. J Hum Hypertens. 2005;19:787–791. doi: 10.1038/sj.jhh.1001898. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Predictive value of CCA-EDV for composite cardiovascular events, in which cerebrovascular events were excluded