ABSTRACT
Research demonstrates that although many mothers initiate pumping for their critically ill children, few women are successful at maintaining milk supply throughout their infants’ entire hospital stay. At the Garbose Family Special Delivery Unit (SDU) at the Children’s Hospital of Philadelphia, we care for mothers who have critically ill infants born with complex cardiac and congenital anomalies. Human milk is viewed as a medical intervention at our institution. Therefore, nurses on the SDU wanted to ensure best practice in terms of pumping initiation. This article describes a continuous quality improvement project that ensured mothers pumped early and often. Childbirth educators can play a key role in preparing mothers who are anticipating an infant who will require hospitalization immediately post-birth.
Keywords: human milk, breastfeeding, milk expression, pumping, continuous quality improvement (CQI)
Human milk is the preferred form of nutrition for all infants. Research demonstrates that infants who receive human milk have better short- and long-term health outcomes (American Academy of Pediatrics [AAP], 2012). For infants who are born critically ill, human milk can make the difference between survival and death. Human milk feedings are associated with a decreased risk of late-onset sepsis, necrotizing enterocolitis, and protection from various infections (AAP, 2012). Infants fed human milk have better neurodevelopmental and cognitive outcomes (Spatz & Lessen, 2011). The AAP 2012 position statement clearly states that human milk is the preferred form of nutrition for infants in the neonatal intensive care unit (NICU).
Given the vital role of human milk for the health of critically ill children, childbirth educators and other health professionals must be equipped to educate mothers and their families with evidence-based education and intervention to ensure the establishment and maintenance of milk supply for pump-dependent mothers. For mothers who have infants requiring hospitalization, direct breastfeeding is usually not an option. Therefore, mothers must begin their lactation experience by mechanically expressing milk using a hospital-grade electric breast pump.
Although many mothers initiate pumping for their critically ill infants, national data demonstrate that few infants receive human milk through discharge. The major reason reported in the literature and by clinicians for mothers not continuing to pump through discharge is low milk supply. Research demonstrates that women who pump within 1 hour of birth (compared to those who start at 6 hours) produce significantly more milk at 3 weeks post-birth and achieve Lactogenesis II earlier (Parker, Sullivan, Krueger, Kelechi, & Mueller, 2012). Furthermore, milk volume and pumping frequency on Day 4 after birth are significant predictors of milk supply at 6 weeks (Hill & Aldag, 2005). Mothers who produce less than 500 ml/day by the end of Week 2 will have less than adequate milk production long term (Hill & Aldag, 2005). To improve expression of colostrum and facilitate mothers’ coming to full milk volume, a new pumping pattern, Medela’s Symphony Preemie+, has been examined with positive results (Meier, Engstrom, Janes, Jegier, & Loera, 2012). This breast pump suction pattern resulted in greater milk output of colostrum and increased pumping efficiency. In addition, mothers of hospitalized infants who use this pattern obtain a milk supply that is commensurate with that of milk volumes in healthy term breastfeeding dyads (Meier et al., 2012). To ensure an exclusive human milk diet for a hospitalized infant by postpartum Day 10–14, ideal maternal expressed milk volumes should be 750 ml or more per 24-hour period (Hill & Aldag, 2005).
Research demonstrates that women who pump within 1 hour of birth (compared to those who start at 6 hours) produce significantly more milk at 3 weeks post-birth and achieve Lactogenesis II earlier.
Given the science of human milk and what is known about milk expression in mothers of critically ill infants, childbirth educators and other health professionals should offer targeted prenatal education to women regarding human lactation, pumping initiation, and the benefits of human milk for their hospitalized infant (Spatz, 2012). In addition, birth hospitals should examine their current practices to ensure that women are receiving evidence-based education and support to pump early and often, so that they can reach their personal breastfeeding goals and optimize outcomes for their infants (Spatz, 2012). This article describes a continuous quality improvement project that was conducted at a children’s hospital that cares for the most vulnerable infants.
DESCRIPTION OF SETTING
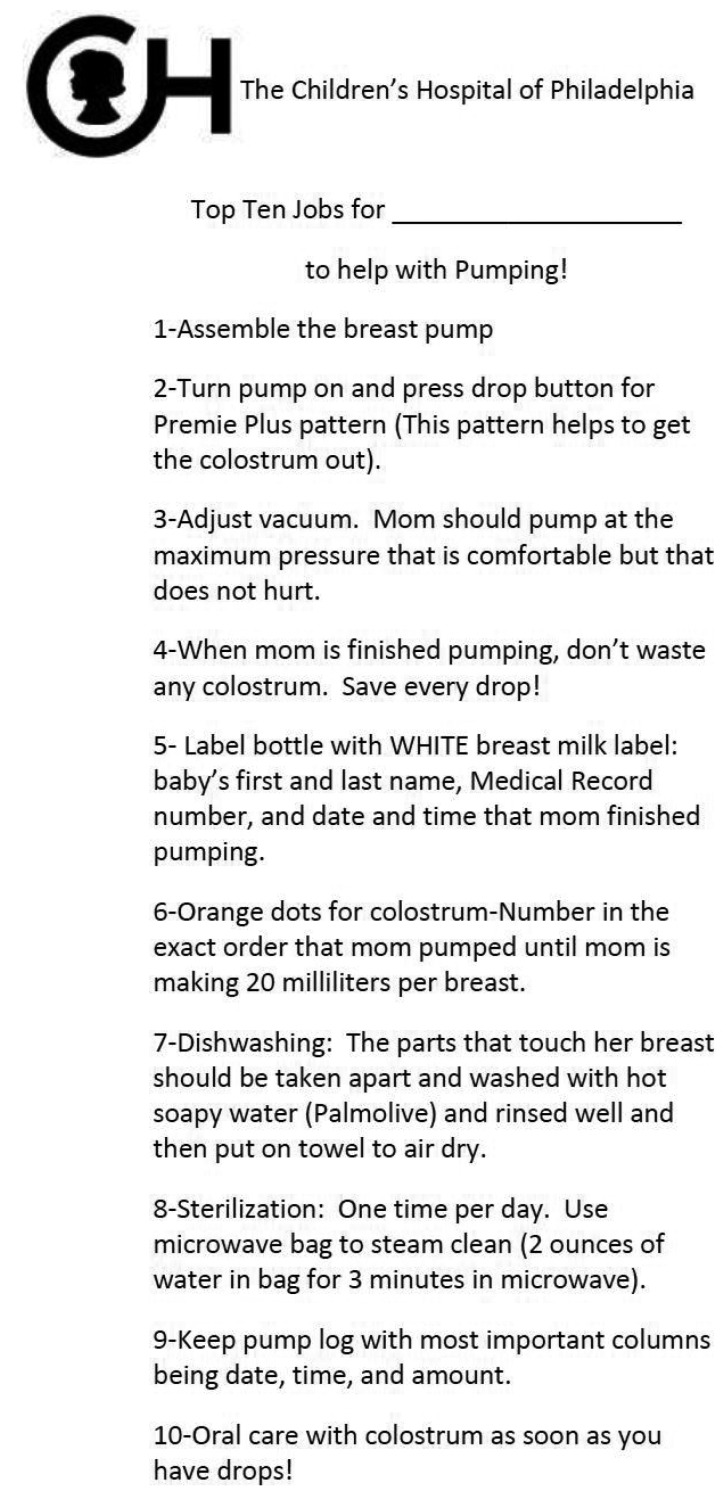
The Center for Fetal Diagnosis and Treatment (CFDT) at the Children’s Hospital of Philadelphia (CHOP) is a national and worldwide referral center for families of infants diagnosed with complex congenital anomalies and chromosomal abnormalities. There are two major categories of conditions: cardiac defects/anomalies and noncardiac congenital anomalies. Most mothers transfer care to the CFDT during their second or third trimester of pregnancy. Mothers who have fetuses with a prenatal diagnosis of spina bifida may transfer care earlier in gestation (between 19 and 24 weeks) to undergo fetal surgery. Most families relocate to the Philadelphia area 3–4 weeks prior to their expected birth date and remain until their infants are well enough to be discharged from CHOP. Because of the nature of infant diagnoses, approximately 60% of mothers who birth at the CHOP SDU will have cesarean surgeries. As a standard of care, all mothers receive a prenatal lactation consultation in conjunction with their prenatal visits (Spatz, 2012). This lactation consultation is provided by either a PhD nurse researcher (for mothers who will have infants being cared for in the NICU) or an International Board Certified Lactation Consultant (for mothers who will have infants being cared for the cardiac center.) Human milk is viewed as a medical intervention for hospitalized infants at CHOP. Therefore, all mothers are encouraged to initiate pumping for their infants, even if they did not plan to breastfeed or do not wish to breastfeed their child in the future (Spatz, 2012). The prenatal education focuses on the science of human milk and the initiation of Lactogenesis II. Education is individualized based on the infant’s diagnosis and planned course of stay in the hospital. The families also receive a gift bag during this prenatal consultation, which includes a sterile pump kit, colostrum containers, human milk labels, orange stickers to number the colostrum bottles, dish soap for cleaning the pump pieces, and a Medela Quick Clean Micro-Steam Bag for sterilization of the pumping equipment. The mother’s partner and/or support person is also given “Ten Steps for Partners/Families to Help With Pumping” (Figure 1). The role of the family is emphasized such that the mother’s only responsibility during the first week after birth is to eat, sleep, pump, and visit her infant. It is the expectation that the family or support person(s) will provide tangible assistance. The first author (DS) also recently developed an educational DVD, “Power of Pumping,” which all families receive when they transfer care to the CHOP CFDT. With this prenatal intervention, the SDU pumping initiation rates are quite high (98%–99%), and most mothers of NICU infants transition their infants to direct breast feeds prior to discharge (Edwards & Spatz, 2012).
FIGURE 1. Ten steps for partners/families to help with pumping.
In 2008, the CHOP Garbose Family Special Delivery Unit (SDU) opened, allowing mothers, under the care of the CFDT, to birth their infants on a unit designed specifically to meet their unique needs. Since its opening, there have been more than 2,000 births in the SDU. The SDU was opened with 9 beds and has since expanded to 12 beds. Each bed in the SDU is equipped with a hospital-grade Medela Symphony Breastpump with the Preemie+ pumping initiation pattern. Supplies for pumping and human milk storage are stocked in the SDU and are readily accessible to patients and families.
The staff of the SDU comprises maternal-fetal medicine physicians and attending obstetricians, certified nurse-midwives, nurse practitioners, registered nurses, obstetric and core technicians, and inpatient unit clerks. Postpartum lactation support on the SDU is largely provided by bedside nurses. In 2008, the SDU nursing staff was quite small but expanded to 16 staff nurses (including full-time, part-time, and per diem) in 2010 when this continuous quality improvement (CQI) project was initiated. Presently, there are 31 staff nurses and 7 certified nurse-midwives. Nurses at CHOP have the opportunity to take a 2-day continuing education course (Breastfeeding Resource Nurse [BRN] course) on the science of human milk and implementation of nurse-driven evidence-based lactation support and care (Spatz, 2005). Most (89%) SDU nurses and midwives have completed the BRN course. The unit has two primary breastfeeding champions who are staff nurses as well as one midwife champion. The role of the unit champions is to ensure dissemination of knowledge and training and to participate as a representative on the hospital-wide breastfeeding committee (Spatz, 2005).
METHODS
Based on the specific education that they receive in the BRN course, nurses in the SDU understand the significance of a mother’s ability to provide human milk for her critically ill infant. Therefore, this CQI project was developed and executed to ensure that families were receiving the best evidence-based education, care, support, and advice regarding lactation and/or breastfeeding. In undertaking this CQI project, the team examined the following metrics: (a) time to first pumping session following birth; (b) frequency of pumping sessions during the SDU stay, that is, number of pumping sessions per each 24-hour period; (c) pumping patterns during night shift; and (d) variations in pumping initiation and/or patterns between mothers who birthed vaginally versus those who required a cesarean surgery.
The ultimate goal of the project was to document improvement in the following areas: (a) compliance with pumping initiation within 2 hours of a vaginal birth and 4 hours of a cesarean surgery, (b) overall frequency of pumping sessions per each 24-hour period during the SDU stay, and (c) documentation of at least one pumping session between 0000 and 0700.
All mothers who birth in the SDU are given a pump log (developed by CHOP). Families are instructed to record the date and time of each pumping session as well as the volume of milk expressed at each session. For the CQI project, all pump logs were photocopied by nursing student interns employed by the lactation program. Student interns entered the pumping data into an Excel database, which was used by the SDU breastfeeding committee to track monthly and yearly trends.
Educational Intervention
The unit-based BRNs in the SDU developed the “Pumping Initiation Education Tool” to ensure that each nurse would be able to give clear and concise step-by-step education to families (Table 1). The unit-based BRN champions provided 1:1 instruction for all staff nurses, and each nurse was required to provide a return demonstration.
Table 1. Pumping Initiation Education Tool.
| Staff Name: ______________ Date:__________________ | |
| Instructor: ___________________ | |
| Steps | Return Demonstration/Knowledge Met Comments |
|---|---|
1. Gather supplies:
|
|
| 2. Sit patient in high Fowler’s position. Have partner sit in chair at bedside of patient. | |
| 3. Open pump kit and remove parts that are not currently to be used (manual pump, large bottles, extra filters). Place remaining parts and one pack of colostrum bottles in basin. | |
| 4. Explain each piece of equipment to patient and partner. | |
| 5. Place flange to connector piece. | |
| 6. Place filter and colostrum bottle on connector piece. | |
| 7. Take apart and request return demonstration from patient and partner. | |
| 8. Place suction pieces on breast pump. | |
9. Explain labeling bottles:
|
|
| 10. Help mom place flanges on breasts ensuring nipple is centered in middle of flange. | |
| 11. Start pump in Preemie+ mode. Turn pressure to highest level patient can tolerate without pain. | |
| 12. Ensure proper flange fit (nipple not rubbing side of flange). | |
| 13. Check in on patient at least once during pumping and at the end of the pumping session to assess breasts, nipples, and flange fit. Assess fit each shift. | |
| 14. Once patient is finished pumping, teach patient to clean parts with Palmolive in basin. Parts will be cleaned following each pump. | |
15. Instruct patient on use of sterilization bag:
|
|
16. Educate patient on pump log:
|
|
17. RN will document the following:
|
|
18. RN will note anything abnormal in pump log:
|
Note. RN = registered nurse.
Following completion of staff education, the unit-based BRN champions developed a “Breastfeeding Audit Tool” (Table 2). Audits were completed monthly by the BRN champions, and the results were regularly disseminated to the unit.
Table 2. Breastfeeding Audit Tool.
| Please review OBIX chart documentation to answer each question with yes/no and nurse who provided documentation. If no, please note if reason is documented and what that reason is. | ||||
| Delivery Date: ____________ | Delivery Time: __________ | |||
| Yes | No | If No, Reason? | Nurse Name | |
|---|---|---|---|---|
| 1. Breastfeeding plan documented on admit form | ||||
| 2. Is it documented that patient is pumping and/or breastfeeding? | ||||
| 3. Did the RN educate the patient pump initiation? | ||||
| 4. Is time of first pump documented? | ||||
| 5. If patient is not pumping, or first pump is delayed, did the RN document this and reason why? | ||||
Note. RN = registered nurse.
Data Management and Analysis
For each pumping mother, the student interns entered the following data points into an Excel database: mother’s name, mode of birth, time between birth and first pump (or breastfeed), number of pumping sessions per 24-hour period during the SDU stay, 24-hour milk production for each day prior to maternal discharge from the SDU, and number of pumping sessions between 0000 and 0700. The pump log is completed by the mother or family. For a volume recorded as “a few drops” or “<1 ml,” that volume data was documented by the team as 0 ml of volume.
At the end of each month, the student interns completed a basic descriptive data analysis for the month. Data was sorted by birth type. Pumping data collected from the pump logs was analyzed separately for vaginal birth mothers and cesarean surgery mothers. For each group, mean time (in hours) to first pump, mean number of pumping sessions per 24-hour period (birth day, Day 1, Day 2, and Day 3 for cesarean surgeries only), mean milk production in milliliters per 24-hour period, and mean number of pumps between the hours of 0000 and 0700 were calculated. Women who had a vaginal birth who did not pump within 2 hours of birth were identified as outliers, and women who had a cesarean surgery were identified as outliers if they did not initiate pumping within 4 hours of birth.
The first author (DS; manager of CHOP’s lactation program) met monthly with the SDU BRN champions, BRN midwife champion, and the nurse manager of the SDU to review the monthly data (including outliers). Each case identified as an outlier was individually discussed, and the chart audit tool was reviewed to determine the reasons for deviation from the expected standard. This allowed for monthly “in the moment” feedback to staff.
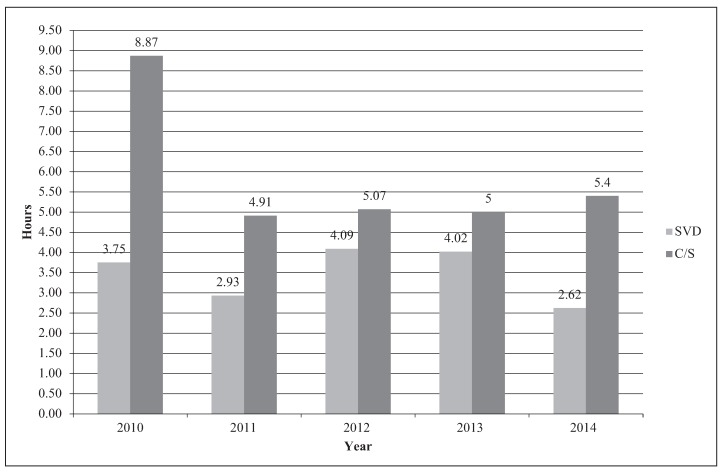
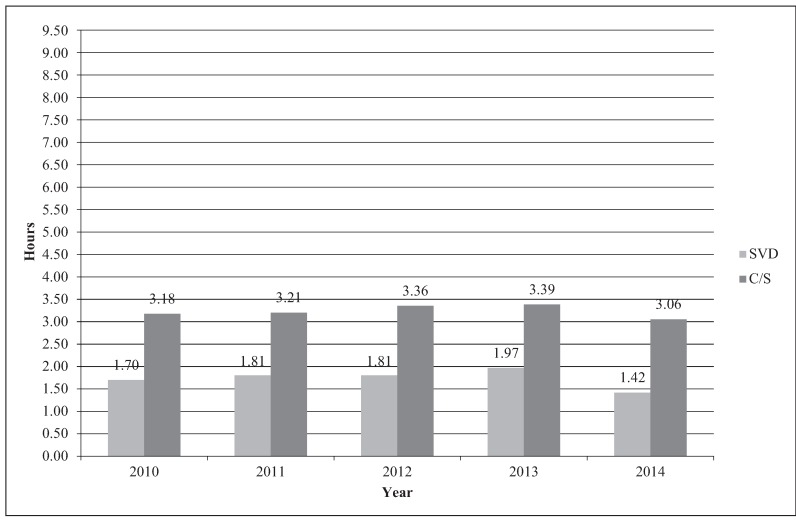
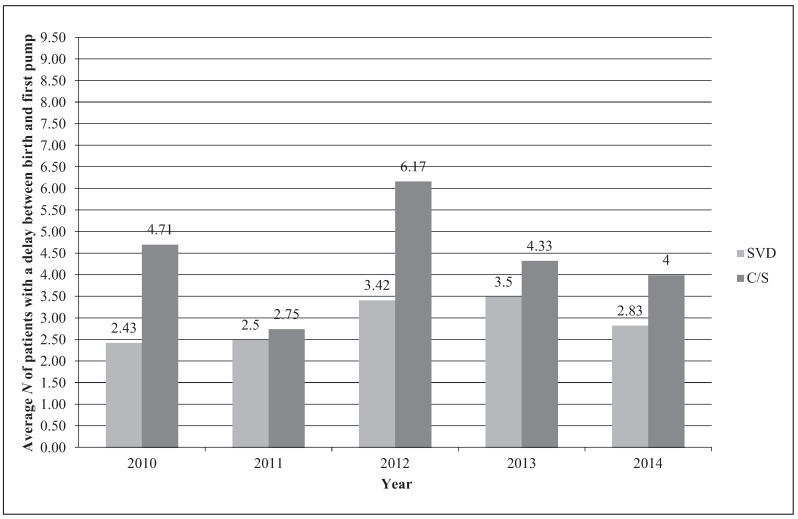
RESULTS
Every month, compliance and outlier data are reviewed and feedback is provided to the staff. For the purposes of this article, data were condensed to provide year-to-year comparisons from 2010 to present. It is the authors’ opinion, based on the research published by Parker and colleagues (2012), that the time to the first pump is the most critical variable that can be addressed through family education and staff education and training. Almost all of the vaginal birth mothers are pumping within 1–2 hours after birth (approximately 95%). Prior to the initiation of the project, vaginal birth mothers were pumping within 3–4 hours, and cesarean mothers within 5 hours. A dramatic improvement in the SDU pumping initiation times for cesarean mothers was noted after the first year of the CQI project; average time to first pump was 9 hours in 2010 and in subsequent years decreased to within 4–5 hours. On average, there were nine outliers (including both vaginal births and cesarean surgeries) identified monthly. When outliers are removed from the data, time to first pump is less than 2 hours for vaginal births and within about 3 hours for mothers with cesarean surgeries (Figures 2, 3, and 4).
FIGURE 2. Time (in hours) to first pump with outliers. SVD = spontaneous vaginal delivery; C/S = cesarean surgery.
FIGURE 3. Time (in hours) to first pump without outliers. SVD = spontaneous vaginal delivery; C/S = cesarean surgery.
FIGURE 4. Average number of mothers per year who are outliers. SVD = spontaneous vaginal delivery; C/S = cesarean surgery.
During the CQI project, improvement was also noted in maternal pumping patterns during night shifts (1900-0700). During the first year of the project, 0% of mothers who had cesarean surgeries pumped between the hours of 0000 and 0700. Significant improvement was noted following education, so that all women, regardless of mode of birth, pumped at least once between the hours of 0000 and 0700.
Women in the SDU are instructed to pump every 2–3 hours with a goal of eight pumping sessions per 24-hour period. During this CQI project, on birth day, following a vaginal birth, women pumped an average of 2 times, and women who had cesarean surgeries pumped on average 3 times per day. On Day 1 post-birth, both vaginal birth and cesarean mothers pumped on average 5–6 times per day. These data reflect the fact that even with continual prenatal and post-birth education regarding pumping schedule, achieving eight pumping sessions per day may not be feasible for all mothers.
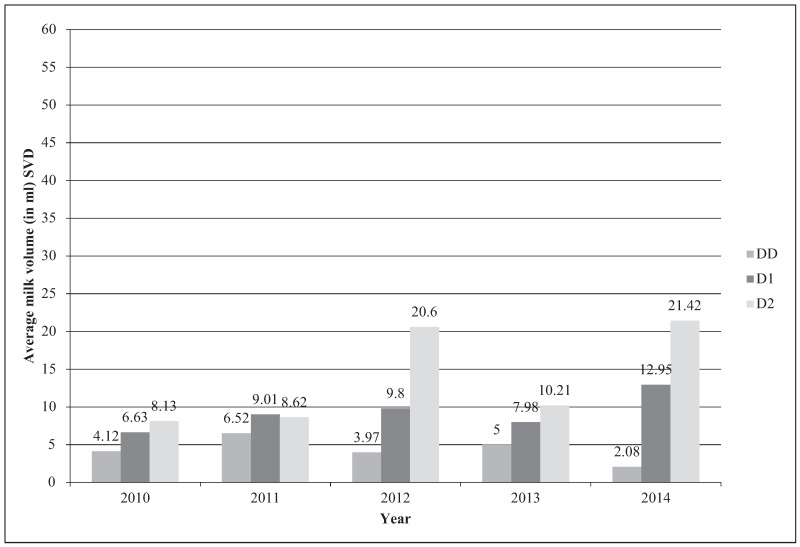
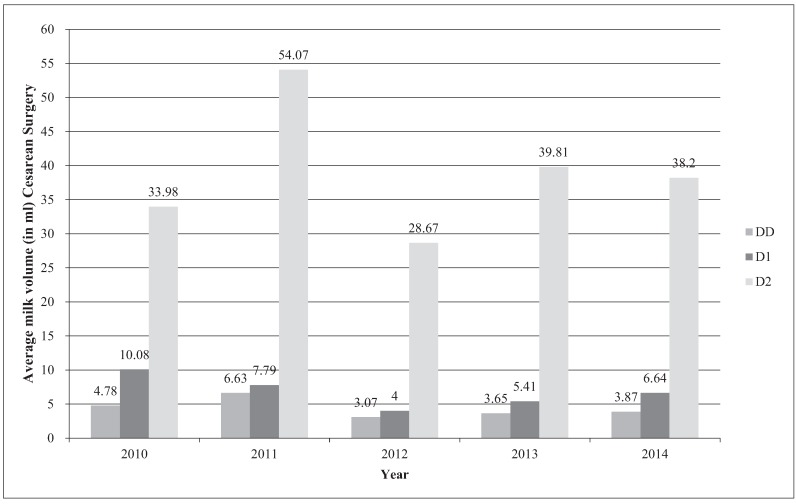
All of the mothers initiate pumping with the Medela Symphony Preemie+ initiation pattern and use this pumping pattern during the course of the SDU stay. On birth day, following a vaginal birth, mothers expressed between 2 and 6.5 ml of colostrum. By Day 1 post-birth, mothers had milk volumes in the range of 8–13 ml/day, and by Day 2 post-birth, those volumes increased to a range of 9–22 ml/day. Cesarean mothers had similar milk volumes on birth day: 3–7 ml. By Day 1 post-cesarean, mothers had milk volumes in the range of 4–10 ml/day. Day 2 post-cesarean, mothers produced, on average, a range of 29–54 ml/day (Figures 5 and 6).
FIGURE 5. Maternal milk volumes—vaginal birth mothers. SVD = spontaneous vaginal delivery; DD = delivery day; D1 = Postpartum Day 1; D2 = Postpartum Day 2.
FIGURE 6. Maternal milk volumes—cesarean surgery mothers. DD = delivery day; D1 = postpartum day 1; D2 = postpartum day 2.
DISCUSSION
Through monthly meetings of the SDU breastfeeding committee, several key issues were identified. First, the amount of new information staff nurses have to learn and use on a daily basis was daunting. To keep pumping initiation a priority, reeducation and reminders needed to occur on a quarterly basis. The SDU BRN champions provided ongoing monthly 1:1 education for staff. In addition, because outliers (those mothers who pumped later than 2 or 4 hours post-birth) were discussed on a monthly basis, trends in barriers to early pumping initiation were identified. Mothers requiring operative births were experiencing three major issues (nausea, vomiting, and pain control) that led to delays in initiation of pumping. This discovery allowed the team to consult with the SDU anesthesia and physician staff to develop methods to alleviate these concerns for mothers in the postpartum period.
This CQI project highlights the fact that with education and regular review of data and targeted feedback to staff (in real time), improved pumping practices can be noted. Although research has suggested that pumping within 1 hour of birth is optimal, this practice may not be feasible outside the framework of a research protocol (Parker et al., 2012). A key education and intervention strategy is to educate both staff and families regarding the necessity to “pump early and pump often” to ensure an adequate milk supply.
Although outside of the scope of this project, the first author (DS) reports that clinically, few women who birth on the SDU experience insufficient milk supply outside of anatomical reasons (breast reduction surgery, glandular hypoplasia). Most women who give birth on the SDU produce between 500 and 1,000 ml of milk per day, with many producing more than 1 L of milk per day. This is evidenced by the number of SDU mothers who have extra milk to donate to a Human Milk Banking Association of North America (HMBANA) milk bank. Mothers of infants at CHOP donate more than 25,000 oz of milk annually to HMBANA milk banks.
IMPLICATIONS FOR PRACTICE
Although the practice model of the CHOP CFDT offers a unique framework for providing lactation support prenatally, the authors suggest the benefits of prenatal lactation support and education may be achieved in other settings. Childbirth educators are, in many ways, the ideal providers to educate families antenatally regarding lactation initiation and maintenance in the case of potential maternal–infant separation. Standard prenatal lactation consultation, with a focus on the science of human milk and breastfeeding as well as an emphasis on pumping early and often in the event of maternal–infant separation, should be integrated into all prenatal care and/or childbirth education classes. Ideally, hospitals should purchase enough hospital-grade pumps to have a pump at every bedside. Of note, despite the name of the pumping initiation pattern described by Meier and colleagues (2012) being called Preemie+, the pattern is not just for mothers who birth preterm infants. In the SDU, most infants are born at term or close to term but still are separated from their mothers because of the infants’ diagnoses and need for intensive care. To facilitate milk production and access to colostrum, the Preemie+, initiation pattern is recommended any time there is maternal–infant separation.
Standard prenatal lactation consultation, with a focus on the science of human milk and breastfeeding as well as an emphasis on pumping early and often in the event of maternal–infant separation, should be integrated into all prenatal care and/or childbirth education classes.
When educating families about human milk and breastfeeding and early pumping initiation, it is critical to involve all members of the family (and/or support persons). Hospitals should provide mothers with pumping logs to record milk expression sessions and volumes, and these data should be reviewed daily by the bedside nurse to ensure that the mother comes to a full milk volume (goal = 750 ml per 24-hour period). There are also many phone apps available for pumping mothers; however, the authors of this manuscript have not been able identify any existing app that fully captures all data of interest.
Education provided to the mother and family should be multimodal (in person 1:1 or group education, written materials, the ability to demonstrate and redemonstrate use of the pump equipment) and audiovisual. Childbirth educators and other health-care professionals should emphasize education related to the value of colostrum. Every drop of colostrum is a vital medication for the vulnerable infant, and every drop should not only be saved but also celebrated. Even the smallest amounts of colostrum can be used immediately to initiate human milk oral care for the infant (Spatz, 2012).
Other important considerations for childbirth educators to discuss with families include structural and functional questions that the family should ask of staff at the birth hospital or hospital where the infant will be cared for. A few examples of key questions that families should ask include the following: Does the hospital have an adequate number of hospital-grade breast pumps to facilitate pumping immediately after maternal discharge and at the infant’s bedside? Does the hospital provide the family with all necessary supplies for pumping? Does the hospital have adequate storage for human milk (refrigerators and freezers)? Do hospital personnel receive education and training specifically regarding the protection of and promotion of human milk/breastfeeding for vulnerable infants (Spatz, 2004)?
For mothers and their families, having an infant that requires immediate hospitalization after birth is stressful and exhausting. Families need to hear consistent and continual messaging from all members of the health-care team, including childbirth educators, regarding the importance of early and frequent milk expression and the value of human milk for the hospitalized infant. Families should receive this education at multiple points in time (prenatally, in the birthing room, on the postpartum unit, and in the unit where the infant is being cared for) with an emphasis on the prenatal period.
Every drop of colostrum is a vital medication for the vulnerable infant, and every drop should not only be saved but also celebrated.
ACKNOWLEDGMENTS
Thank you to all of the University of Pennsylvania and Drexel University Nursing students who greatly assisted with collection of pump logs. Thank you to the nurses on the Garbose Family Special Delivery Unit, our lactation consultant staff, breastfeeding resource nurses, and most of all, our mothers and their families.
Biographies
DIANE L. SPATZ is a professor of Perinatal Nursing and the Helen M. Shearer professor of Nutrition at the University of Pennsylvania School of Nursing and a nurse researcher and manager of the lactation program at the Children’s Hospital of Philadelphia.
ELIZABETH FROH is the clinical supervisor of the Lactation Team and the Human Milk Management Center at the Children’s Hospital of Philadelphia.
JESSICA SCHWARZ is a master’s of science in nursing–prepared certified nurse-midwife and lead midwife breastfeeding resource nurse champion at the Children’s Hospital of Philadelphia.
KATHERINE HOUNG is a former student intern for Dr. Spatz and a BSN/MSN graduate of the University of Pennsylvania School of Nursing. She currently works as a primary care pediatric nurse practitioner for Greater Philadelphia Health Action, Inc.
ISABEL BREWSTER was a student intern for Dr. Spatz and Dr. Froh. She is a recent BSN graduate from the University of Pennsylvania School of Nursing.
CAREY MYERS is a staff nurse and breastfeeding resource nurse champion in the Garbose Family Special Delivery Unit at the Children’s Hospital of Philadelphia.
JUDY PRINCE is a staff nurse and breastfeeding resource nurse champion in the Garbose Family Special Delivery Unit at the Children’s Hospital of Philadelphia.
MICHELLE OLKKOLA is the nurse manager of the Garbose Family Special Delivery Unit at the Children’s Hospital of Philadelphia.
REFERENCES
- American Academy of Pediatrics. (2012). Breastfeeding and the use of human milk. Pediatrics, 129(3), e827–e841. 10.1542/peds.2011-3552 [DOI] [PubMed] [Google Scholar]
- Edwards T. M., & Spatz D. L. (2012). Making the case for using donor human milk in vulnerable infants. Advances in Neonatal Care, 12(5), 273–278. 10.1097/ANC.0b013e31825eb094 [DOI] [PubMed] [Google Scholar]
- Hill P. D., & Aldag J. C. (2005). Milk volume on day 4 and income predictive of lactation adequacy at 6 weeks for mothers of non-nursing preterm infants. Journal of Perinatal & Neonatal Nursing, 19(3), 273–282. [DOI] [PubMed] [Google Scholar]
- Meier P. P., Engstrom J. L., Janes J. E., Jegier B. J., & Loera F. (2012). Breast pump suction patterns that mimic the human infant during breastfeeding: Greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. Journal of Perinatology, 32(2), 103–110. 10.1038/jp.2011.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker L. A., Sullivan S., Krueger C., Kelechi T., & Mueller M. M. (2012). Effect of early breast milk expression on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants: A pilot study. Journal of Perinatology, 32(3), 205–209. [DOI] [PubMed] [Google Scholar]
- Spatz D. L. (2004). Ten steps for promoting and protecting breastfeeding in vulnerable populations. Journal of Perinatal & Neonatal Nursing, 18(4), 385–396. [DOI] [PubMed] [Google Scholar]
- Spatz D. L. (2005). Report of a staff program to promote breastfeeding in the care of vulnerable infants at a children’s hospital. Journal of Perinatal Education, 14(1), 30–38. 10.1624/105812405X23630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spatz D. L. (2012). Innovations in the provision of lactation support for infants requiring intensive care. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 41(1), 138–143. 10.1111/j.1552-6909.2011.01315.x [DOI] [PubMed] [Google Scholar]
- Spatz D. L., & Lessen R. (2011). The risks of not breastfeeding—position statement. Morrisville, NC: International Lactation Consultant Association. [Google Scholar]