ABSTRACT
Sarah Buckley’s game-changing report, Hormonal Physiology of Childbearing: Evidence and Implications for Women, Babies, and Maternity Care, provides the evidence that supporting, promoting, and protecting the normal physiology of childbirth produces the best outcomes for mothers and babies. In this article, a childbirth educator recommends key points from Buckley’s report that should be included in Lamaze childbirth education classes.
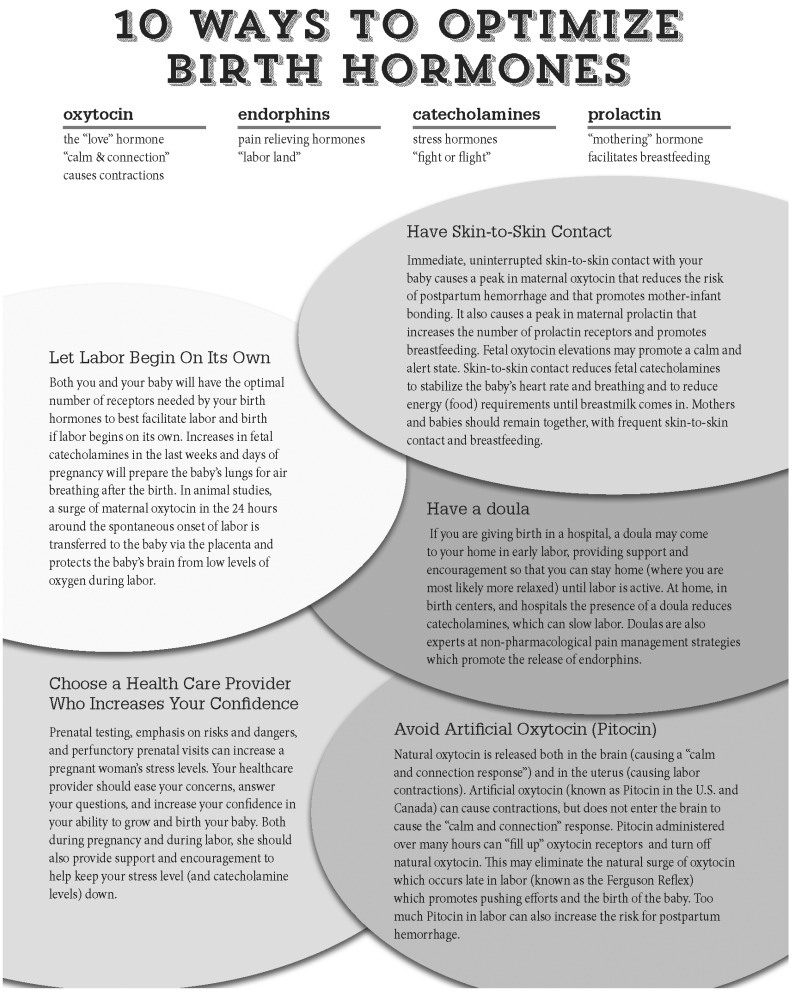
Keywords: hormonal physiology, oxytocin, endorphins, catecholamines, prolactin
When I finished reading Sarah Buckley’s game-changing report, Hormonal Physiology of Childbearing: Evidence and Implications for Women, Babies, and Maternity Care, I wanted to shout from the rooftop, “Yes! Here it is! We finally have the evidence for what we teach—that the safest and healthiest birth for both mother and baby is one in which we ‘allow’ innate, normal physiology to unfold as Mother Nature intends.” As Penny Simkin described in her Science and Sensibility post on January 13th, 2015, Buckley has given us a gift by synthesizing research from many diverse fields on the hormonal orchestration of pregnancy, labor and birth, breastfeeding, and mother–infant attachment. The information in the report is complex and not always 100% definitive. When it is not possible to conduct human trials (i.e., measuring brain levels of oxytocin during labor), Buckley shares animal research studies. Still, the conclusions are clear: In healthy pregnancies, hormonal processes foster readiness for birth, efficient labor, safety for mother and infant, successful breastfeeding, and optimal mother–infant bonding. The challenge is how the childbirth educator can share this critical information with students in Lamaze International classes. Here are some suggestions.
We finally have the evidence for what we teach—that the safest and healthiest birth for both mother and baby is one in which we “allow” innate, normal physiology to unfold as Mother Nature intends.
Excellent fact sheets for clinicians and policy makers, infographics, and a booklet designed specifically for women are available at http://www.childbirthconnection.org.
Visit Childbirth Connection at http://www.childbirthconnection.org to read the full report.
READ THE REPORT
It is challenging to read the full report. The information is dense and complex. Buckley has 1,141 references. The good news is that the report is beautifully organized. At least read the Executive Summary; the consumer pamphlet, Pathway to a Healthy Birth; Angela’s Birth Story; the seven fact sheets; and the infographics for consumers and for clinicians. In the full report, each section begins with an italicized paragraph that summarizes the major points of that section. Each section ends with a summary of that section. You can easily jump from the italicized opening paragraph to the summary. If you want more details, you can go back and read the relevant paragraphs. Handy charts in the “Conclusions” section summarize effects of common medical interventions on hormonal physiology.
DISTRIBUTE THE CONSUMER HANDOUTS FROM THE CHILDBIRTH CONNECTION WEBSITE TO YOUR STUDENTS
You can also refer your students to the Childbirth Connection website. However, you may increase the chances that your students will read the pamphlets if you give them copies. Or you can create a library by placing the pamphlets in folders and asking students to return them after reading. I have also included with this article a condensed, two-page handout on birth hormones (see Appendix). The reading level is a little higher than the consumer pamphlets on the Childbirth Connection website, so this handout is not appropriate for all childbirth classes.
INCORPORATE KEY INFORMATION INTO YOUR CURRICULUM
Obviously when and how much information you include is dependent on how many classes you teach and when during pregnancy those classes are offered. The Lamaze recommendation is that you offer classes throughout the childbearing year including the following topics:
Choosing a Health-Care Provider
Ideally in a preconception or early pregnancy class, discuss the importance of the health-care provider. Buckley emphasizes in the report the role of the health-care provider in increasing confidence rather than fear during pregnancy. Prenatal testing, emphasis on risks and dangers, and perfunctory prenatal visits can increase a pregnant woman’s stress levels. High levels of stress during pregnancy increase risks of premature birth, intrauterine growth retardation, and reduced newborn head size, reflecting suboptimal brain growth (Buckley, 2015, p. 115). Buckley (2015) quotes Michel Odent who recommends that maternity care providers “create such interactions that a pregnant woman feels even happier after a prenatal visit than before . . . or at least less anxious” (p. 126).
Choosing a Birth Location
Also, ideally in a preconception or early pregnancy class, discuss the importance of the birth location. Throughout her report, Buckley emphasizes the importance of the laboring woman feeling private, safe, and undisturbed. Homes and birth centers are more likely to provide such an environment. For those planning hospital births, childbirth educators can brainstorm with students strategies to create a quiet and safe environment and to keep interruptions and distractions to a minimum.
Relaxation Skills
Continue teaching or bring back relaxation skills in your Lamaze classes. Buckley (2015) cites a recent systematic review of effects of relaxation techniques in pregnancy that
found beneficial effects in relation to: women’s emotional state, maternal and fetal physiologic stress markers and/or hormones, hospital admission, premature birth and low birth weight, cesarean section rate, and newborn neurobehavior, among other pregnancy and postpartum benefits. Effective techniques included guided imagery (such as a guided relaxation audio program), progressive muscle relaxation, yoga, and massage. (p. 127)
Benefits of Exercise
Levels of endorphins rise during pregnancy and peak around the time of the spontaneous onset of labor. Women who exercise regularly throughout pregnancy have even higher levels of endorphins and shorter, less painful labors (Clapp & Cram, 2012). Research also shows that regular exercise decreases the risk of cesarean surgery (Domenjoz, Kayser, & Boulvain, 2014).
Encouraging Women to Let Labor Begin on Its Own
Buckley provides powerful evidence for the risks of not letting labor begin on its own. Many of the critical hormonal processes preparing both mother and baby for birth occur in the days or even hours before the spontaneous onset of labor. This includes increases in the number of hormone receptors, a surge in fetal catecholamines that prepares the fetus for air breathing after birth, and a surge in maternal oxytocin that is transferred to the baby and provides a neuroprotective effect during labor and birth (animal studies). In addition to the sections of the Buckley report on the “Physiologic Onset of Labor and Scheduled Birth” and on “Oxytocin,” see Lamaze International’s Healthy Birth Practice #1: Let Labor Begin on Its Own (Amis, 2014).
Doulas
John Kennell, one of the founders of DONA International, once said, “If a doula were a drug, it would be unethical not to use it.” Numerous studies have shown that outcomes are improved for laboring women who have continuous support from a doula during childbirth. The benefits are most likely because of the reduction in catecholamines that occur when a woman feels well supported and the increase in endorphins that come from many of the nonpharmacological pain management strategies often promoted by doulas.
Risks of Pitocin
If labor is induced, both the pregnant woman and the fetus may miss out on some of the hormonal preparation for birth such as having the optimal number of receptors, the fetal catecholamine surge that prepares the lungs for air breathing, and the maternal surge of oxytocin that provides a neuroprotective effect for the fetal brain. If labor has to be induced for medical reasons, it is best if induction can be delayed until the mother shows some symptoms of readiness of birth such as softening of the cervix. Pitocin administered over many hours can “fill up” oxytocin receptors and turn off natural oxytocin. This may eliminate the natural surge of oxytocin, which occurs late in labor (known as the Ferguson reflex), which promotes pushing efforts and the birth of the baby. Too much Pitocin in labor can also increase the risk for postpartum hemorrhage. Studies also show negative effects on breastfeeding with induction of labor, possibly because of a reduction in prelabor increases in prolactin and a decrease in the number of prolactin receptors.
Risks of Epidural Analgesia
Epidural analgesia reduces oxytocin levels, often leading to slowed labor and the need for artificial oxytocin (Pitocin). The laboring woman may miss out on the natural surge of oxytocin late in labor (the Ferguson reflex), which promotes pushing efforts and the birth of the baby. Administration of Pitocin also increases the risk for postpartum hemorrhage. Epidurals also reduce endorphin levels. Rather than experiencing the altered state of consciousness known as labor land common with endorphin release, the mother may remain in a more “normal, alert state.” A decrease in endorphins after birth may mean that the “reward–pleasure center” in the brain is not activated in the same way as is true with higher levels of endorphins after the birth.
Risks of Cesarean Surgery
If the cesarean surgery is done before the spontaneous onset of labor, both the pregnant woman and the fetus may miss out on some of the hormonal preparation for birth such as having the optimal number of receptors, the fetal catecholamine surge that prepares the lungs for air breathing, and the maternal surge of oxytocin that provides a neuroprotective effect for the fetal brain. Most cesarean surgeries are performed with epidural analgesia so the negative effects listed earlier also apply. Maternal–infant separation is more common after cesarean surgery, so mother and baby may not get the benefits of immediate, uninterrupted skin-to-skin contact. But the good news is that, as with labor induction and epidural analgesia, immediate, uninterrupted skin-to-skin contact will increase the release of oxytocin, endorphins, and prolactin and decrease the release of catecholamines.
Immediate, Uninterrupted Skin-to-Skin Contact
It is not possible to overemphasize the importance of skin-to-skin contact between mother and baby after the birth. Skin-to-skin contact with breastfeeding increases oxytocin and prolactin levels, possibly increasing the number of prolactin receptors which can influence breastfeeding success for months (and years) to come. Increases in oxytocin promotes vasodilation in the mother’s chest, warming the newborn, and decreases the risk for postpartum hemorrhage. Oxytocin in the maternal brain activates mothering behaviors. Fetal oxytocin elevations may promote a calm and alert state, which helps breastfeeding. Skin-to-skin contact reduces fetal catecholamines to stabilize the baby’s heart rate and breathing and to reduce energy (food) requirements until breastmilk comes in. For the laboring woman who has medical interventions during labor that disrupt hormonal physiology, immediate, uninterrupted skin-to-skin contact is an invaluable way to restore the flow of birth hormones.
Interactions and Redundancies
As I read the Buckley report, I was amazed at how one hormone very often promotes the release of another and at how the hormones work together to promote readiness for birth, progress and comfort in labor, efficient second stage, breastfeeding, and mother–infant bonding. Different hormones may have similar effects, such as oxytocin producing a “calm and connection” response and endorphins decreasing anxiety and relieving pain. Mother Nature has also created redundancies such as the oxytocin surge at the end of labor that promotes pushing and the birth of the baby (known as the Ferguson reflex) and the catecholamine surge (known as the fetal ejection reflex) that also occurs also at the end of labor to promote the birth of the baby.
Yes, the physiology is complex, yet at the same time, perfectly designed to promote optimal outcomes for both mother and baby, both in the short term and in the long term.
Yes, the physiology is complex, yet at the same time, perfectly designed to promote optimal outcomes for both mother and baby, both in the short term and in the long term.
CONCLUSION
In addition to synthesizing more than a thousand research studies to explain how hormonal physiology fosters readiness for birth, efficient labor, safety for mother and infant, successful breastfeeding, and optimal mother–infant bonding, Buckley also explores research about how what happens during labor and birth may cause epigenetic changes, affecting generations to come. Childbirth educators owe it to themselves, their students, and to future generations to learn from this report and to spread the word.
Biography
DEBBY AMIS is the coauthor of Prepared Childbirth—The Family Way, Prepared Childbirth—The Educator’s Guide, and The Lamaze Toolkit for Childbirth Educators. She is also codirector of The Family Way: Lamaze Childbirth Educator Program. She and her husband live close to their grandchildren in Houston, Texas.
APPENDIX
REFERENCES
- Amis D. (2014). Healthy Birth Practice #1: Let labor begin on its own. The Journal of Perinatal Education, 23(4), 178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley S. (2015). Hormonal physiology of childbearing: Evidence and implications for women, babies, and maternity care. Washington, DC: Childbirth Connections Programs, National Partnership for Women & Families. [Google Scholar]
- Clapp J., & Cram C. (2012). Exercising through your pregnancy: A compelling case for exercise before, during, and after pregnancy (2nd ed.). Omaha, NE: Addicus Books. [Google Scholar]
- Domenjoz I., Kayser B., & Boulvain M. (2014). Effect of physical activity during pregnancy on mode of delivery. American Journal of Obstetrics & Gynecology, 211(4), 401.e1–401.e11. [DOI] [PubMed] [Google Scholar]
- Simkin, P. (2015, January 13). Sarah Buckley’s “Hormonal Physiology of Childbearing: Evidence and Implications for Women, Babies, and Maternity Care”—A review for birth educators and doulas [Web log post]. Retrieved from http://www.scienceandsensibility.org/sarah-buckley-educators/