ABSTRACT
Newborn breastfeeding behaviors have not been characterized in children later diagnosed with autism spectrum disorder (ASD). In a qualitative interview, 16 mothers (28–56 years) of children with ASD described their 19 full-term infants’ (38–42 weeks’ gestational age) breastfeeding behaviors. Nine mothers described their infants as demonstrating a dysregulated breastfeeding pattern of sucking without stopping of their own volition. The infants’ latch, weight gain, and other behaviors were recalled as not problematic. This feature of dysregulated feeding pattern in infancy has not been reported previously for children with ASD. If supported by future research, the pattern of a dysregulated feeding pattern in newborns could be evaluated by clinicians in the general pediatric population and/or at-risk infant siblings of children with ASD.
Keywords: autism, autism spectrum disorder, infants, breastfeeding, maternal recall
Several types of social interactions during the first year of life are delayed or altered in children subsequently diagnosed with autism spectrum disorder (ASD; Clifford & Dissanayake, 2008; Ozonoff et al., 2010). Beginning as early as 2–6 months, infants demonstrate decreasing eye contact; by 10 months, differences in social interactions of joint attention, mutual gaze, reciprocal vocalizations, and feeding behaviors may be observed (Clifford & Dissanayake, 2008; Emond, Emmett, Steer, & Golding, 2010; Jones & Klin, 2013; Landa, 2007). In feeding, infants later diagnosed with ASD, when compared to a control group of infants in the general population, demonstrate slower motor anticipation during spoon-feeding, idiosyncratic food choices, and challenging behaviors during mealtime (Brisson, Warreyn, Serres, Foussier, & Adrien-Louis, 2012; Marquenie, Rodger, Mangohig, & Cronin, 2011; Martins, Young, & Robson, 2008). The earliest social feeding behavior, breastfeeding, has been described with respect to duration, but neither latch nor feeding patterns have been described in infants later diagnosed with ASD (Al-Farsi et al., 2012; Schultz et al., 2006).
ASD affects 1 of 50 children, diagnosed in 1 of every 31 boys and 1 in 143 girls (Blumberg et al., 2013). A spectrum of disorders that include autism and Asperger’s syndrome, ASD commonly presents with persistent deficits in social interaction and communication and restricted and repetitive patterns of behaviors (American Academy of Pediatrics, 2007; American Psychiatric Association, 2013). Although the developmental screening for ASD is recommended beginning at age 2 years, the average age of diagnosis is 4 years, when children begin schooling and difficulties with social interactions are assessed (Maenner et al., 2013). Early identification of relevant behavioral markers in infants and referral for early intervention could be beneficial because children with ASD respond well to social and behavioral intervention (American Academy of Pediatrics, 2007; Lord & Bishop, 2010).
Newborn breastfeeding behaviors have not been characterized in children later diagnosed with autism spectrum disorder.
LITERATURE REVIEW
Breastfeeding Is a Neurodevelopmental Behavior
One of an infant’s first social interaction behaviors is breastfeeding (Brazelton, Koslowski, & Main, 1974; Kaye & Wells, 1980). Unique among breastfeeding mammals, human infants during breastfeeding will pause and wait for the mother to move the breast, talk to, or touch them (Brown, 1973). Breastfeeding is a complex neurodevelopmental behavior that requires an infant to create and sustain an effective latch (oral seal to create negative intraoral pressure) and maintain an efficient breastfeeding pattern that provides sufficient milk volume for satiation to support consistent weight gain (Al-Farsi et al., 2012; Kaye & Wells, 1980; Schultz et al., 2006). During the newborn period, breastfeeding sessions occur every 1.5–4 hours and range on average between 5 and 30 minutes (Hill & Johnson, 2007; Lucas, Lucas, & Baum, 1979). In 2009 in the United States, 76.9% of all newborn infants were introduced to breastfeeding at birth, but within 2 weeks, only 50% of mothers reported exclusively breastfeeding their infants (Li, Fein, Chen, & Grummer-Strawn, 2008; Odom, Li, Scanlon, Perrine, & Grummer-Strawn, 2013). Problems with an infant’s latch and dysregulated feeding patterns may be assessed by trained caregivers who are the first to observe consecutive breastfeeding sessions during the newborn period.
In case-controlled and dose-response studies, shorter breastfeeding duration has been found to be predictive of ASD diagnosis in infants (Al-Farsi et al., 2012; Schultz et al., 2006). Prenatal risk factors for diagnosis of ASD are maternal history of obesity, diabetes or episodes of high fever, maternal exposure to high levels of air pollution, maternal diet low in folic acid, and advanced maternal or paternal age (Grether, Anderson, Croen, Smith, & Windham, 2009; Hertz-Picciotto et al., 2006). However, for full-term infants who are routinely evaluated in well-baby care, there are no behavioral risk factors.
Among full-term newborns who breastfeed, it is unknown what breastfeeding behaviors besides duration might serve as early warning signs of diagnosis with ASD. The identification of such behaviors in full-term infants would support early screening and referral for the social and behavioral interventions successful with infants and children diagnosed with ASD (American Academy of Pediatrics, 2007).
THEORETICAL MODEL
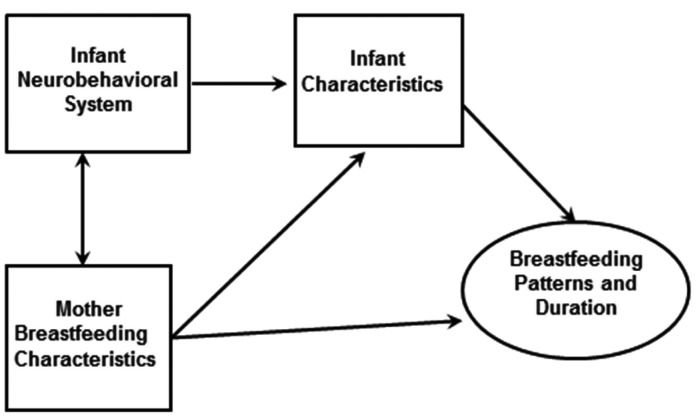
The theoretical model of the study is adapted from the developmental science paradigm. The model was chosen to guide this study and theorizes that infants actively participate with the environment (Magnusson & Cairns, 1996). For newborns who are breastfeeding, the environment is their mother (Figure 1; Bell, Lucas, & White-Traut, 2008). Most infants at birth have a neurobehavioral system that supports typical development (meeting expected developmental milestones), demonstrate behavioral cues to initiate breastfeeding, respond to maternal regulation, and breastfeed with an effective latch and efficient pattern (Hill & Johnson, 2007; Kaye & Wells, 1980). One observable feature of mother–infant dyadic interactions is infant breastfeeding behavior (Bell et al., 2008; Brazelton et al., 1974; Kaye & Wells, 1980). All infants at birth are affected in their ability to breastfeed by the characteristics of gestational age, route of birth, and medical complications (American Academy of Pediatrics, 2012). Maternal breastfeeding characteristics, such as age, antenatal intention, ethnicity, and education, will also affect breastfeeding behaviors (U.S. Department of Health and Human Services, 2011). The dyadic interactions of the infant’s neurobehavioral system and characteristics with the mother’s breastfeeding behaviors may be observed in breastfeeding patterns and duration (Figure 1; Brazelton et al., 1974; Hill & Johnson, 2007). Currently, the evaluation of breastfeeding patterns for the full-term infant is based on infant satiation and consistent weight gain (American Academy of Pediatrics, 2012). Breastfeeding patterns, including coordination and regulation of milk flow patterns, are evaluated only if there is an issue with inadequate weight gain in the infant (American Academy of Pediatrics, 2012; Hill & Johnson, 2007).
FIGURE 1. Model of mother–infant interaction during breastfeeding.
For infants with an altered neurodevelopment at birth, mother–infant interactions may differ from those of typically developing infants. Infants may demonstrate inconsistent behavioral cues to initiate breastfeeding, decreased response to maternal regulation, and an ineffective latch and dysregulated feeding pattern (Li et al., 2008; Odom et al., 2013), but there is an absence of research on early breastfeeding behaviors among children diagnosed with ASD. The purpose of this study was to report retrospective maternal descriptions of specific newborn behaviors during breastfeeding initiation and the first month of life among children later diagnosed with ASD.
METHODS
Design and Sample
This study employed a qualitative design using structured interviewing with descriptive statistics to present demographic and clinical information. A convenience sample was acquired through posters, flyers, an information table at ASD community events, and two community clinics that serve families with ASD. Mothers included were between ages 18 and 64 years, initiated breastfeeding after birthing, and were able to fully comprehend and use English. Infants had a gestational age of 38–42 weeks, clinical diagnosis of ASD from a university medical center using the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM IV-TR), and admission to the routine care newborn nursery (American Academy of Pediatrics, 2007). Infants with a diagnosis of a genetic anomaly, for example, Down syndrome, were excluded. The total sample was 16 mothers and 19 infants, with 1 mother reporting on 2 infants and another on 3. Infants included 18 boys and 1 girl and 11 first-born and 8 later born infants.
For infants with an altered neurodevelopment at birth, mother–infant interactions may differ from those of typically developing infants.
Participants were interviewed in locations selected by the participants. These included offices, homes, restaurants, libraries, and shopping malls throughout a midwestern metropolitan area. The University of Illinois Institutional Review Board approved the study, which required written informed consent.
Measures
The measures included a semistructured self-report interview and interview guide based on selected demographic and clinical characteristics of early breastfeeding and the child’s ASD diagnosis. The self-report interview and interview guide were developed by the authors. The primary investigator pilot tested the measures with two mothers before interviewing all of the mothers in the study. The interview questions included prompts about the child at the present time, how and when the child was diagnosed, and if and how long before the diagnosis the mother noticed anything different about the child’s behavior or communication. Mothers were then asked to describe their pregnancy, birth, hospital stay, and first breastfeeding experiences. Mothers were probed with specific questions about the infant’s latch and pattern of feeding, satiation after feeding, and general breastfeeding experience. These probes aligned with the following intervals: the birth, the hospital stay, the first week at home, the first month after birth, and the cessation of breastfeeding. The interview guide is presented in the Appendix. Each interview was digitally recorded and lasted approximately 1 hour.
Data Management
Interviews were recorded and transcribed verbatim, proofread for accuracy, and coded. Codes were developed in context of the theoretical model focusing on latch and breastfeeding behaviors at the time intervals of birth, hospital stay, the first week at home, the first month after birth, and after the first month of birth. Some behavioral codes were collapsed into more general breastfeeding behaviors after the first three interviews. For example, latch at each time point was nested into general infant breastfeeding behaviors during each time point. The codes were revised after a consensus was reached with breastfeeding and qualitative methods experts.
The first five interviews were independently coded by the primary investigator and a research team member for interrater reliability. Thirty percent of the codes were randomly selected, and interrater reliability was 95%. Three additional interviews were double coded with interrater reliability of 95% (Dallas, Norr, Dancy, Kavanaugh, & Cassata, 2005). The research team placed thematic codes, breastfeeding behaviors, or maternal recall of ASD diagnosis in separate tables to insert and compare significant quotes on each subject, then developed a summary of each participant’s interview, an analysis across participants’ summaries, and a synopsis of the overall study. The final synopsis was reviewed by both breastfeeding and qualitative methods experts for clarity. Individual summaries were sent to each mother to verify congruence with the participant’s experience and to increase the validity of the data (Ayres, Kavanaugh, & Knafl, 2003). Twelve mothers responded and agreed that the summary was accurate; the other four mothers could not be reached.
RESULTS
Demographic and clinical characteristics of the mothers and fathers are presented in Table 1. Mothers reported a perinatal history of preeclampsia (n = 6) and gestational diabetes (n = 2). Fifteen mothers received epidural anesthesia, and 1 received general anesthesia (data not tabulated here).
Table 1. Characteristics of Mothers (N =16) at Birth, at Child’s Diagnosis of Autism Spectrum Disorder, and at Interview.
| Maternal Variable | Birth | Diagnosis | Interview | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Range | M | (SD) | Range | M | (SD) | Range | M | (SD) | |
| Maternal age (years) | 22–39 | 30.4 | (3.6) | 28–45 | 34.5 | (4.5) | 28–56 | 39.63 | (9.6) |
| Maternal education (years) | 10–18 | 16.2 | (2.1) | 10–18 | 16.2 | (2.1) | |||
| Paternal education (years) | 12–18 | 15.8 | (2.8) | ||||||
| Marital status | |||||||||
| Married | 15 | 94% | 15 | 94% | 14 | 88% | |||
| Stable partner | 1 | 6% | 1 | 6% | 0 | 0 | |||
| Single | 0 | 0 | 0 | 0 | 1 | 6% | |||
| Divorced | 0 | 0 | 0 | 0 | 1 | 6% | |||
| Ethnicity | |||||||||
| Asian | 1 | 6% | |||||||
| Black | 2 | 13% | |||||||
| Hispanic | 4 | 25% | |||||||
| White | 9 | 56% | |||||||
| Route of birth | |||||||||
| Vaginal | 13 | ||||||||
| Cesarean surgery | 5 | ||||||||
| Vaginal birth after cesarean | 1 | ||||||||
All infants were 38–42 weeks’ gestation (M = 40, SD = 0.82), with a birth weight from 3,033 to 4,224 g (M = 3,637, SD = 362). Thirteen infants transitioned to extrauterine life without intervention, and 7 infants received minimal medical interventions within 6 hours of birth. All infants breastfed within 24 hours after birth: 11 infants immediately at birth, 6 infants within 2 hours, and 5 infants within 6 hours.
At the time of the interview, children were aged 5–16 years (M = 8.68, SD = 3.90): 5–9 years (n = 13) and 10–16 years (n = 6). At the time of their diagnosis, the children’s ages ranged from 18 months to 8 years (M = 4.01, SD = 2.00). ASD diagnoses included autism (n = 12), Asperger’s syndrome (n = 6), and pervasive developmental disorder—not otherwise specified (n = 1). Five children had comorbidities of attention deficit disorder, seizures, and hypotonia. Four themes emerged from the interviews: establishing an effective latch, infant feeding patterns over time, health weight gain, and maternal recall of early signs of ASD.
Establishing an Effective Latch
Twelve infants were described as able to establish a latch and initiate breastfeeding without difficulty. This was detailed by mothers who said, “He was able to nurse; it seemed like he was able to nurse right away,” and “He nursed for about 5–7 minutes on each side. So, okay, he knows what he’s doing. And I had no problems with him initially after birth.”
However, five infants were unable to establish an effective latch during hospitalization because of anatomical/physiological barriers (maternal flat nipples or short frenulum). For example, one mother noted, “He found the nipple he started feeding . . . I was never able to successfully feed with my right breast.” Another mother described how her infant had difficulty relearning to breastfeed on a flat nipple after a circumcision:
Initially he latched beautifully . . . but after the circumcision he was a beast . . . [the hospital staff] kept me another day, and the [lactation consultants] worked with me and they worked with me . . . but [after discharge] it took me a long time to figure out how to breastfeed this baby . . . I had flat nipples, which was a problem, he’d keep sliding off.
One mother recalled breastfeeding her infant before and after a short frenulum was clipped at 3 weeks:
I remember there was one side that he preferred . . . I always dreaded moving him to the other one. And then I had to do it by myself . . . I thought [after it was clipped] it was going to turn into night and day. And it wasn’t.
Mothers and infants were described as able to establish an effective latch without difficulty if there were no anatomical/physiological barriers. However, mothers with anatomical/physiological barriers required professional lactation support and needed to pump to sustain their milk supply until the infant was able to latch consistently. Many mothers in the general population with anatomical/physiological barriers report similar experiences and a need for professional support in establishing breastfeeding during the first month of life (Hanna, Wilson, & Norwood, 2013; Segal, Stephenson, Dawes, & Feldman, 2007).
Infant Feeding Patterns Over Time
Fourteen mothers described their infants as successfully establishing breastfeeding, and 9 mothers breastfed beyond 6 months of age. However, mothers recalled nine infants as demonstrating a dysregulated feeding pattern of vigorous sucking that did not stop with satiation.
On average, mothers in this study recalled breastfeeding their infants for 8.87 months (SD = 6.30). Many mothers described no issue with breastfeeding their infant over time. One first-time mother said, “It was good. That is all I can say. I had no problems, and he was swallowing, he was drinking, everything was fine.” A second-time mother said, “He never really had a bottle, because I was at home.”
The mothers described 9 infants with a dysregulated feeding pattern during hospitalization and 12 infants after discharge:
Right after birth, within in the first hour, I think he was okay. But he seemed like, I guess those first two days, he seemed hungry all the time. Like I was like a human, you know, I guess it took forever, so I just felt like I was just sitting there, and I couldn’t do anything else. I couldn’t go to the bathroom, I couldn’t eat and if, you know, you unhooked him then, you know, he would just scream and cry.
A second-time mother recalled,
So, he didn’t have a problem latching on, or he didn’t have a problem starting to suck. Actually he was very, very vigorous sucker. So, he didn’t, he was pretty good for that. He, what he did do, some kids know they are done and kind of push the nipple away, “I’m done, I’m kind of full” kind of deal. [He] never showed up full, kind of thing. He just would go and go and go . . . And eventually he would just go and fall asleep, but he would keep sucking. But he would just keep sucking, there was no “I’m full” kind of thing that I could see . . . he doesn’t seem to have an on/off as it were.
Ten mothers recalled changing how they fed their infant within 1 week after discharge. One first-time mother recalled of her son,
The first problem I had might have been 3 or 4 days after I was at home, that I was, whenever he would cry I was breastfeeding him. So, I think I was breastfeeding him more than he needed. And he just wanted to drink, so I thought it was okay, and it was too much for him . . . I started just breastfeeding him on a real schedule, like every 3 hours, I started breastfeeding you at 3 hours and then I would make him wait a little bit and then I, I would give him and he started being much better. Like more, he would be calm and he would be okay unless he was just too hungry and he would break my heart to see him like that so I would come a little bit earlier and then that or sooner, but. Yeah, I would say 3 hours.
A second-time mother who had successfully breastfed her first child described her daughter’s breastfeeding pattern, “It seemed like she still wanted to be breastfed even though she was full. But since I noticed, you know, that she was full so I, I didn’t give her more.” Two mothers, who recalled their infants continuing the dysregulated feeding pattern beyond the first week, stopped breastfeeding within 6 weeks. One first-time mother recalled, “In the coming weeks after that, he was nursing 45 minute stretches, every 2 hours on the hour. So I was not sleeping, and I chose at that time to end the breastfeeding. He was gaining enough weight.” A second-time mother who had successfully breastfed recalled, “He feed till I bleed, which is why I stopped earlier than I planned to . . . I don’t know what would cause it to bleed? Or if it was the, because he was sucking too hard.”
Mothers were asked specific questions about when and if there were any challenges with initiating breastfeeding and if breastfeeding challenges continued after discharge. Mothers described two challenges: the anatomical barrier and the dysregulated feeding pattern. Most mothers recalled overcoming both barriers with lactation support or drawing on previous breastfeeding experience. Five mothers stopped breastfeeding within 3 months, two because of anatomical barriers and three because of the dysregulated feeding pattern. Only one mother–infant dyad with anatomical/physiological barriers recalled an infant demonstrating dysregulated feeding pattern. The other mother–infant dyads with anatomical/physiological barriers may have regulated the feeding pattern while addressing the latch barriers; thus, the number of infants with dysregulated feeding pattern may be underreported in the infants in our sample.
Healthy Weight Gain
Mothers reported weight gain during the first month of life. Two mothers whose infants fed with a dysregulated feeding pattern visited the pediatrician’s office for well-baby care. One observed, “He was gaining enough weight. The doctors were amazed at how much weight he was gaining. I had a scale at home. I knew he was gaining weight.” The second mother, who was a medical professional, said, “He would eat, because he was like pretty like 98th percentile, like prior to 6 months.”
All of the mothers reported adequate weight gain at 1 month. As one observed, “He had gained. I thought he had gone from 9 lb 5 oz to 10 lb in a week . . . he was thriving.” Many mothers spoke with pride about their milk supply and their infant’s weight gain, as did this mother: “The doctor said I had atomic milk because my kids would, they would like weigh them . . . . they would be like, ‘Oh so what formula do you have?’ and I would say, ‘Nah, he’s a breast baby.’”
Maternal Recall of Early Signs of Autism Spectrum Disorder
Mothers were asked to describe when they were first concerned about their child’s behaviors. Four mothers recalled their infants demonstrating different behaviors after 6 months. One said, “I would say for his first 6 months old of life, I never saw anything that would show me that he had something. Everything started after he was 6 months.” Another mother reported,
Like all along he wouldn’t snuggle with [his father]. We found out later it’s because [his father] has facial hair and he doesn’t like the feel of that. But we didn’t know that and at the time, we were like. “That’s weird.” Or he wouldn’t . . . he would sit in his little high chair and kick it, I would say compared to all the other four kids to compare, and he would just kick it uncontrollably, we couldn’t eat dinner because he was so loud. We were like “What the heck! That’s weird.” Or he wouldn’t go from different surfaces when he was walking on other surfaces and we were like “What the heck, that’s just a weird kid!” And then, or he did everything at the last possible minute.
Many mothers described breastfeeding as a wonderful time in their infant’s life. One said, “It was perfect, and I felt very good. I felt a connection with him; it was a really nice time . . . I breastfed him for 9 months.” One mother, who was not concerned until after her sons were 2 and 3 years of age, remarked,
I [have] very fond memories of, sometimes you think back on them [breastfeeding] and then if you knew the things you knew. What would happen now? Then? But I am glad that we didn’t. We enjoy them, they were typical infants, they weren’t difficult as kids or as infants . . . They’re very pleasant memories [breastfeeding her sons], you know, we’ve, we’ve been through a lot harder things, and we will be. But, yeah there, I enjoy all that.
A first-time mother, whose son was diagnosed after age 2 years and did not successfully breastfeed because of a short frenulum, reflected back on the first year:
Because he was my first, I was just . . . Why isn’t my son, you know, following the ball like all the other kids around at Gymboree time? Why isn’t my son trying to do this when everybody else is doing it? I couldn’t put two and two. But I wasn’t really worried . . . Obviously difficult breastfeeding but also eating. He didn’t eat till after he was a year old . . . it was like a battle . . . you thought somebody was beating him up. He was just crying hysterically when I would try to feed him and not even take it. So he didn’t eat for the first year. It was only milk, formula.
Seven mothers reported seeking professional counsel when their children did not develop language after 18 months. As one said, “After that about 18 months, still no real language . . . like no words, some sounds, grunting sounds but nothing in terms of real words.” Eight mothers were not concerned until after their children were in preschool or elementary school and school officials approached them about testing. As one reported,
The school had mentioned at an IEP meeting, autism. I was completely blown out of the water. I was very offended, and this was how this was dropped on my lap. They mentioned autism. And I walked out of the meeting before the meeting was done.
Four mothers recalled a behavior of concern after their infants were 6 years of age. Fifteen mothers recalled their children demonstrating behaviors of concern after 1 year of age.
DISCUSSION
This study reports maternal descriptions of newborn breastfeeding behaviors of children later diagnosed with ASD. Fifteen mothers recalled their newborns as able to establish a latch at breastfeeding initiation and successfully breastfed to 6 months. Nine mothers recalled that nine infants demonstrated a dysregulated breastfeeding pattern of vigorous sucking without stopping of their own volition. All of the mothers reported adequate weight gain during the first month of life. No mothers reporting recalled breastfeeding behaviors as the first behaviors that led them to seek professional assessment for the child’s diagnosis of ASD. The dysregulated infant breastfeeding pattern of vigorous sucking without stopping has not been described in the breastfeeding literature before.
The authors theorized during the development of this study that infants would have difficulty with creating a latch (needing lactation support or a nipple shield) because of an alteration in neuromotor function. We also theorized, based on the limited literature, that infants later diagnosed with ASD would have shorter breastfeeding duration. In our study, mothers reported no issue with latch except for expected challenges of managing anatomical/physiological barriers seen in the general population. Instead, mothers reported a dysregulated feeding pattern during the first 2 weeks after discharge, which diminished by 1 month. Mothers also reported maintaining breastfeeding beyond the first month of life, and infants gaining clinical appropriate weight. If mothers were able to manage their infants’ initial difficult breastfeeding behaviors, they reported maintaining breastfeeding longer than the case-controlled study (Al-Farsi et al., 2012). A persistent repetitive behavior, such as the dysregulated feeding pattern, is one of the diagnostics for ASD. In the infant period, sucking constitutes a repetitive behavior under the infants’ volitional control. However, prolonged sucking would not normally be a clinical concern because the infant would be consistently gaining weight.
CLINICAL IMPLICATIONS
During the first weeks of breastfeeding, mothers experience many challenges to establishing breastfeeding. While supporting mothers, clinicians observe many different patterns of breastfeeding behaviors. Although infants in our study were successful at sucking, many mothers needed support to manage the prolonged sucking or, based on their own experience, regulated their infants’ sucking patterns. Mothers not successful at regulating their infants’ prolonged sucking experienced trauma, fatigue, and stopped breastfeeding by 6 weeks. Effective prolonged feeding would not be of clinical note unless mothers described physical trauma, as several of the mothers did in our study. These mothers needed support to regulate the prolonged sucking to prevent trauma and allow time for maternal milk supply to be replenished. The clinical implications of our findings are limited because a larger prospective study is needed to validate these mothers’ experiences. However, these infants would benefit from greater surveillance for soft clinical signs of altered neurodevelopment during the first year to support early intervention.
Despite the current findings, the results of this study are preliminary and should not be interpreted yet as suggesting early signs of ASD. To assess the predictive value of this pattern among infants later diagnosed with ASD, further study is needed to estimate the prevalence of early dysregulated feeding patterns among children currently 18 months to 5 years old who were diagnosed with ASD and among the general pediatric population.
This study has several limitations. First is the potential for maternal recall bias of breastfeeding experiences. Because of the nature of a retrospective study, mothers did not recall details of breast softening or weight changes after breastfeeding that could rule out a slow infant feeder, an infant sucking for comfort, or an infant with a dysregulated vigorous pattern. Although maternal report of breastfeeding initiation has been found to be accurate up to 50 years later, maternal recall of breastfeeding duration is consistently overestimated (Li et al., 2008). The interview guide had many probes related to breastfeeding to clarify any issues and often included references to places and times to support recall, but reliability of the reports is unknown. If their recall of duration is reliable, then the relatively long average of breastfeeding duration found in this study may reflect a skewed population of breastfeeding mothers who participated because they had positive memories of successful breastfeeding.
In summary, the mothers of children later diagnosed with ASD reported that their infants had no difficulty establishing a latch or with early weight gain nor did they recall concerns about the infants’ behavior prior to 6 months of age. However, more than half of our mothers described their infants as demonstrating a dysregulated feeding pattern of vigorous sucking without stopping of their own volition during the first weeks of life, which decreased in occurrence with maternal regulation of breastfeeding and infant breastfeeding experience. Because a vigorous sucking pattern without stopping is a new descriptor for a dysregulated breastfeeding pattern, this study has identified a behavior that—if future research is supportive—care providers and lactation specialists should assess.
Further study is needed to estimate the prevalence of early dysregulated feeding patterns among children currently 18 months to 5 years old who were diagnosed with ASD and among the general pediatric population.
Biographies
RUTH FITTS LUCAS is passionate about mother–infant breastfeeding dyads after 23 years at the bedside. Dr. Lucas’ research focuses on infant breastfeeding behaviors and how these behaviors affect breastfeeding success and duration.
ANN CUTLER is a developmental pediatrician with a focus on autism spectrum disorder identification and intervention. Dr. Cutler is influential in national policy making to support families and their children diagnosed with autism spectrum disorder.
APPENDIX: SEMISTRUCTURED INTERVIEW QUESTIONS
Infant History of Autism
-
1
How did you find out about this study?
-
2
Tell me, what made you choose to participate in this study?
-
3
Tell me about NAME. I want to get to know your child (NAME). Tell me about the time when NAME was diagnosed with autism?
-
4
Did you as a parent suspect that something was wrong?
-
5
If yes, when did you suspect something?
-
6
Do you recall why you felt that something was not right with NAME?
Breastfeeding Following Birth and During Hospitalization
-
1
Please describe for me your first breastfeeding experience with NAME.
-
a
How did it go?
-
b
When did it occur?
-
c
Were there any concerns?
-
a
-
2
How would you describe NAME’s sucking behavior?
-
3
Do you remember hearing NAME swallow your milk while breastfeeding?
-
4
Did NAME have any trouble latching-on to the breast?
-
5
Did NAME have any trouble opening mouth wide?
If NAME had trouble then used probes below:
-
6
Do you recall NAME having any difficulty, such as:
-
a
Latching on to the breast?
-
b
Placement of his or her tongue?
-
c
Placement of his or her lips?
-
d
Creating suction?
-
a
-
7
Did NAME need help with stimulation to the palate, tongue, lips?
-
8
Did you experience any trauma during breastfeeding such as pain, cracked nipples, bleeding, bruising?
-
9
Did you ask for lactation consultant help?
-
10
Did staff recommend a lactation consultant help?
-
11
Did you use a nipple shield during breastfeeding with NAME?
REFERENCES
- Al-Farsi Y. M., Al-Sharbati M. M., Waly M. I., Al-Farsi O. A., Al-Shafaee M. A., Al-Khaduri M. M., . . . Deth R. C. (2012). Effect of suboptimal breast-feeding on occurrence of autism: A case-control study. Nutrition, 28(7–8), e27–e32. 10.1016/j.nut.2012.01.007 [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. (2007). Identification and evaluation of children with autism spectrum disorders. Pediatrics, 120(5), 1183–1215. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. (2012). Breastfeeding and the use of human milk. Pediatrics, 129(3), 600–603. h-3552 [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Ayres L., Kavanaugh K., & Knafl K. (2003). Within-case and across-case approaches to qualitative data analysis. Qualitative Health Research, 13, 871–883. [DOI] [PubMed] [Google Scholar]
- Bell A., Lucas R., & White-Traut R. (2008). Concept clarification of neonatal neurobehavioral organization. Journal of Advanced Nursing, 61(5), 570–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumberg S., Bramlett M., Kogan M., Schieve L. A., Jones J. R., & Lu M. C. (2013). Changes in prevalence of parent-reported autism spectrum disorder in school-aged U.S. children: 2007 to 2011–2012. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Brazelton T., Koslowski B., & Main M. (1974). The origins of reciprocity: The early mother-infant interaction In Lewis M. & Rosenblum L. (Eds.), The effect of the infant on its caregiver (pp. 49–76). New York, NY: Wiley. [Google Scholar]
- Brisson J., Warreyn P., Serres J., Foussier S., & Adrien-Louis J. (2012). Motor anticipation failure in infants with autism: A retrospective analysis of feeding situations. Autism, 16(4), 420–429. 10.1177/1362361311423385 [DOI] [PubMed] [Google Scholar]
- Brown J. (1973). Non-nutritive sucking in great ape and human newborns: Some phylogenetic and ontogenetic characteristics In Bosma J. (Ed.), Fourth symposium on oral sensation and perception: Development in the fetus and infant (pp. 118–134). Bethesda, MD: U.S. Department of Health, Education, and Welfare. [PubMed] [Google Scholar]
- Clifford S., & Dissanayake C. (2008). The early development of joint attention in infants with autistic disorder using home video observations and parental interview. Journal of Autism and Developmental Disorders, 38(5), 791–805. [DOI] [PubMed] [Google Scholar]
- Dallas C., Norr K., Dancy B., Kavanaugh K., & Cassata L. (2005). An example of a successful research proposal: Part II. Western Journal of Nursing Research, 27(3), 210–231. [DOI] [PubMed] [Google Scholar]
- Emond A., Emmett P., Steer C., & Golding J. (2010). Feeding symptoms, dietary patterns, and growth in young children with autism spectrum disorders. Pediatrics, 126, e337–e342. [DOI] [PubMed] [Google Scholar]
- Grether J., Anderson M., Croen L., Smith D., & Windham G. (2009). Risk of autism and increasing maternal and paternal age in a large North American population. American Journal of Epidemiology, 170, 1118–1126. [DOI] [PubMed] [Google Scholar]
- Hanna S., Wilson M., & Norwood S. (2013). A description of breast-feeding outcomes among U.S. mothers using nipple shields. Midwifery, 29(6), 616–621. 10.1016/j.midw.2012.05.005 [DOI] [PubMed] [Google Scholar]
- Hertz-Picciotto I., Croen L., Hansen R., Jones C., van de Water J., & Pessah I. (2006). The CHARGE study: An epidemiologic investigation of genetic and environmental factors contributing to autism. Environmental Health Perspectives, 114, 1119–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill P., & Johnson T. (2007). Assessment of breastfeeding and infant growth. Journal of Midwifery & Women’s Health, 52(6), 571–578. [DOI] [PubMed] [Google Scholar]
- Jones W., & Klin A. (2013). Attention to eyes is present but in decline in 2–6-month-old infants later diagnosed with autism. Nature, 504, 427–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye K., & Wells A. (1980). Mothers’ jiggling and the burst–pause pattern in neonatal feeding. Infant Behavior & Development, 3, 29–46. [Google Scholar]
- Landa R. (2007). Early communication development and intervention for children with autism. Mental Retardation & Developmental Disabilities Research Reviews, 13, 16–25. 10.1002/mrdd.20134 [DOI] [PubMed] [Google Scholar]
- Li R., Fein S., Chen J., & Grummer-Strawn L. (2008). Why mothers stop breastfeeding: Mothers’ self-reported reasons for stopping during the first year. Pediatrics, 122, S69–S76. [DOI] [PubMed] [Google Scholar]
- Lord C., & Bishop S. (2010). Autism spectrum disorders: Diagnosis, prevalence, and services for children and families. Social Policy Report, 24(2), 1–27. Retrieved from http://www.srcd.org/sites/default/files/documents/24-2.pdf [Google Scholar]
- Lucas A., Lucas P., & Baum J. D. (1979). Pattern of milk flow in breast-fed infants. Lancet, 2, 757–758. [DOI] [PubMed] [Google Scholar]
- Maenner M. J., Schieve L. A., Rice C. E., Cunniff C., Giarelli E., Kirby R. S., . . . Durkin M. S. (2013). Frequency and pattern of documented diagnostic features and the age of autism identification. Journal of American Academy of Child Adolescent Psychiatry, 52(4), 401–413.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnusson D., & Cairns R. (1996). Developmental science: Toward a unified framework In Cairns R., Elder G., & Costello E. J. (Eds.), Developmental science (pp. 7–30). Cambridge, United Kingdom: Cambridge University Press. [Google Scholar]
- Marquenie K., Rodger S., Mangohig K., & Cronin A. (2011). Dinnertime and bedtime routines and rituals in families with a young child with an autism spectrum disorder. Australian Occupational Therapy Journal, 58(3), 145–154. 10.1111/j.1440-1630.2010.00896.x [DOI] [PubMed] [Google Scholar]
- Martins Y., Young R. L., & Robson D. C. (2008). Feeding and eating behaviors in children with autism and typically developing children. Journal of Autism Developmental Disorders, 38(10), 1878–1887. h-008-0583-5 [DOI] [PubMed] [Google Scholar]
- Odom E. C., Li R., Scanlon K. S., Perrine C. G., & Grummer-Strawn L. (2013). Reasons for earlier than desired cessation of breastfeeding. Pediatrics, 131(3), e726–e732. h-1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozonoff S., Iosif A., Baguio F., Cook I., Hill M., Hutman T., . . . Young G. S. (2010). A prospective study of the emergence of early behavioral signs of autism. Journal of American Academy of Child Adolescent Psychiatry, 49(3), 256–266. [PMC free article] [PubMed] [Google Scholar]
- Schultz S., Klonoff-Cohen H., Wingard D., Akshoomoff N., Macera C., Ji M., & Bacher C. (2006). Breastfeeding, infant formula supplementation, and autistic disorder: The results of a parent survey. International Breastfeeding Journal, 1(16). Retrieved from http://www.internationalbreastfeedingjournal.com/content/1/1/16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal L., Stephenson R., Dawes M., & Feldman P. (2007). Prevalence, diagnosis, and treatment of ankyloglossia: Methodologic review. Canadian Family Physician, 53(6), 1027–1033. [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2011). The Surgeon General’s call to action to support breastfeeding. Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General. [Google Scholar]