Abstract
Background
African-Americans (AA) who experience a first time stroke are younger, and have double the stroke rate and more post-stroke complications than other Americans.
Objective
To assess perceived post-stroke care barriers among younger AA men and their care partners (CPs) in order to inform development of acceptable and effective improvements in post-stroke care for this high-risk group.
Methods
Ten community-dwelling AA stroke survivors and 7 of their care partners (CPs) participated in focus groups and advisory board meetings. Survivors had stroke or transient ischemic attack within one year and a Barthel ADL Index >60. In focus groups, using a semi-structured interview guide, survivors and CPs identified self-perceived barriers and facilitators to post-stroke care. Thematic analysis of session transcripts and the constant comparative method were used to generate themes.
Results
Survivor age ranged from 34 to 64. Mean Barthel was 95.5. CPs, all AA women, ranged in age from 49–61. CPs were 5 wives, a fianceé and a niece. Participants cited multiple personal, social, and societal stroke recovery challenges. While hypertension and smoking risks were acknowledged, stress, depression, PTSD, anger/frustration, personal identity change, and difficulty communicating unique needs as AA men were much more frequently noted. Facilitators included family support, stress reduction and dietary changes.
Conclusions
Younger AA men and their CPs perceive multiple post-stroke care barriers. Biological risk reduction education may not capture all salient aspects of health management for AA stroke survivors. Leveraging family and community strengths, addressing psychological health, and directly engaging patients with healthcare teams may improve care management.
Keywords: stroke, transient ischemic attack, African-American men, recovery
INTRODUCTION
Stroke is the leading cause of disability, third leading cause of death, and one of the most resource-intensive diseases among Americans. African-Americans (AA) have a stroke rate nearly double that of Euro-Americans (EA), and AA who experience a first-ever stroke are younger, have greater stroke disability, more post-stroke complications, and slower recovery compared to EA. Age-adjusted stroke mortality rates are 43.7 percent higher in AA than in EA men.1–5
One-quarter of U.S. strokes each year are recurrent events.6 Recurrence risk increases over time, and one in four stroke survivors will die of a recurrent stroke.7 After a TIA, the risk for future strokes increases 12-fold.5 Interventions to control risk factors (e.g. hypertension, hyperlipidemia and diabetes mellitus) and make behavioral modifications (e.g. smoking cessation, dietary changes, weight loss, exercise and stress management) can drastically reduce recurrent stroke risk2 and improve health outcomes.3 Unfortunately, AA may have low stroke risk factor awareness and low use of risk reduction therapies.,4,8,9,10
Given the disproportionate burden of stroke, healthcare approaches that will improve health outcomes and reduce future risk in younger AA men who have had a stroke are critically needed. Improving post-stroke self-management may enhance health outcomes for AA men,11–15 but additional information is needed on salient and potentially modifiable barriers to inform the development of acceptable and effective interventions and reduce health disparities.
To address this need, we conducted a qualitative analysis of barriers to stroke care and recovery in younger (< age 65) AA men who have experienced a stroke or transient ischemic attack (TIA) as part of a larger National Institute of Health (NIH)- funded study to develop and pilot a nurse and peer led self-management intervention for AA men (R21NR013001-01A1 PI Sajatovic).
METHODS
Study Design
We used focus group methodology to collect data from homogenous groups of individuals using a predetermined structured sequence of questions in a focused discussion. According to Kreuger,16 focus groups are an appropriate strategy for learning the vocabulary and discovering the thinking patterns of the target audience, as well as for discovering unanticipated findings and exploring hidden meanings. It has the further advantage of guiding the design of health education and promotion programs for high risk groups.17–21
Sample and Setting
Ten AA survivors of ischemic stroke or TIA were enrolled within 12 months of discharge from an acute stroke program or within 12 months of Emergency Department/physician visit for TIA. Additional inclusion criteria were: self-identified AA male; age < 65 years; planned or recent home discharge; and Barthel Index (BI) score of > 60.22–24 Having an available care partner (CP) was preferred but not required and we enrolled 7 CPs. We recruited these community dwelling participants from a tertiary care medical center acute stroke unit, local primary care clinics, specialty stroke care programs as well as locations such as public libraries and senior centers.. The study was approved by the University Hospitals Case Medical Center Institutional Review Board (IRB) and all participants provided written informed consent.
We held the Focus groups in the evening in a small conference room of the participating institution and a light supper was served. A moderator (MS) facilitated focus group discussion using a semi-structured interview guide. Two facilitators (CB, AP) recorded observations regarding group dynamics and monitored the recording equipment. Although the moderator and facilitators were not race concordant with the focus group participants, they possessed extensive expertise in focus group methodology and work in health disparities research.
Participants were explicitly encouraged to express themselves openly without concern for whether other group members agreed with their opinions. We noted that the addition of CPs provided a more dynamic, interactive approach to the discussion and enabled the men to be more forthcoming about the issues being discussed. A debriefing session between the moderator and facilitators was held after each focus group session to provide an opportunity for sharing first impressions, summarize key findings, and compare each session with previous ones. Focus group sessions (3 in all) were conducted until little new information was provided.16 All focus group participants later joined a representative Advisory Board to help refine a stroke intervention for AA men that was part of the larger NIH-funded study.
Qualitative Data Collection and Analysis
During the focus groups we explored personal, family, and provider factors relevant to post-stroke care among AA men and their CPs. Additionaly, we elicited perceptions regarding barriers to addressing American Heart Association/American Stroke Association(AHA/ASA) modifiable risk factor reduction 25 as well as barriers to overall recovery
All focus groups were audio recorded and transcribed verbatim. Debriefing sessions among study staff after each focus group were also audio-recorded and transcribed. Transcript-based methodology26,28 was used for data analysis. We used a thematic content analysis approach, encompassing open, axial and sequential coding, and the constant comparative method to generate constructs (themes) and elaborate the relationship among constructs.26,27 Three qualitatively trained investigators (CB, MS, JC) independently coded each transcript to ensure consistency and transparency of the coding; discrepancies were resolved by discussion. We then constructed a coding dictionary with mutually exclusive code definitions. Coding structure was reviewed after a preliminary analysis of a sub- sample of transcripts, and the dictionary was refined through comparison, categorization and discussion of each code’s properties and dimensions.28 Significant statements and themes attached to the codes enabled identification/characterization of perceived barriers. Coding and analysis results were presented to the focus group members at an advisory board meeting where they were invited to critically evaluate and comment on the findings.29
RESULTS
Sample Characteristics
Stroke/TIA Survivors
Mean age of the stroke/TIA survivors was 53 (range =34–64). Seven had an ischemic stroke and 3 had a TIA. Mean Barthel index was 95.5 (SD=7.6). Education levels included post-graduate (n=1); college (n=1); some college (n=1); high school (n=5); and some high school (n=2). One of the men was employed full-time; three were retired and six were unemployed.
Care Partners (CPs)
All CPs were AA women, mean age 54 (range=49–61. Five CPs were wives, one a fiancée and one a niece. Education levels included post-graduate (n=1); college (n=2); some college (n=1); and high school (3). Two were employed full-time; two were retired; and three were unemployed.
Transcript based analysis generated three major domains of barriers to care and recovery: a) Personal Level Barriers, b) Family/Community Level Barriers, and C) Provider/Healthcare System Level Barriers.
Personal Level Barriers
Table 1 shows themes, descriptive codes, and illustrative quotations emerging from Personal Level Barriers. We classified these barriers into the five categories that reflected the personal issues that our respondents faced in their recovery: Psychological, Knowledge, Lifestyle, Functional Impairment, and Self-Identity.
Table 1.
Personal Level Barriers to Post Stroke Care and Recovery Among African-American Men (AA) and Their Care Partners (CPs) (n =17)
| Themes and Categories | Illustrative Quotations from Respondents |
|---|---|
|
Psychological Barriers Stress Anger/frustration Depression/PTSD Shame/stigma |
“The top concern is handling stress level, and I heard it mentioned here over and over.” Respondent P2 “I think about it (stroke) all the time; is that normal? I’m flying off the handle more now. I can’t concentrate; can’t remember.” Respondent P8 |
|
Knowledge Barriers Stroke terminology Risk factors Comorbid conditions Medications |
“What do they mean by diseases of the artery? What do they mean?” Respondent P4 “We found out he had diabetes and high blood pressure. We didn’t know that.” Respondent CP2 |
|
Lifestyle Barriers Life in the fast lane Smoking Alcohol Diet |
“One of the biggest things with me is the lifestyle I have; lots of money, big home, cars, and all that.” Respondent P1. “I grew up on soul food all my life and it’s kind of hard for me to change.” Respondent P5 |
|
Functional Impairment Barriers Fine motor skills Memory Vision Speech Mobility |
“I don’t remember staying overnight in the hospital; I can’t remember most things that happened in the hospital.” Respondent P7 “My left side is pretty much paralyzed, so I have a hard time getting around or using the whole left side of my body.” Respondent P4. |
|
Self-Identity Barriers Macho men Changes in body image Changes in role |
“I have always been in good health—I never even had a cold. Now I’m damaged!” Respondent P8 “He’s used to doing things but he can’t do what he used to do, like work, which was important to him.” Respondent CP5 |
Psychological Barriers
Stress
Stress was a commonly identified psychological barrier. One participant identified a very stressful day as the direct cause of his stroke, “I was in a lot of stress the day before I had the stroke. I had to coach football, and then had to rush to pick someone up at the airport and my car broke down,” (Respondent P1).
Some respondents felt that just being an AA man was stressful, “I think a lot of stuff is dealing with stress and social issues. I don’t drink, I don’t smoke, but that’s not out of the norm. So, once again that leads us right back to the stress issue. When you start talking about stress and African American men, the stress got to be at least 75 to 80 percent of why we even had a stroke.” (Respondent P6). Another participant felt that stress related to his race and environment led him to be paranoid and isolated, “I wanted to say mine is more paranoia, like if I walk out of here and I know I will be afraid of getting robbed, or different things like that. And then I’m already going through this situation with my health and I have to watch constantly where I’m going outside.” (Respondent P9). Others felt that black men got only negative attention and information on stroke risk factors for AA men was lacking.
Anger and Frustration
Many voiced anger and frustration at the disruption of their lives since the stroke, “It’s really frustrating. I played basketball a lot and now walking stairs kills me!” (Respondent P4). One man’s CP noticed that her kind and loving relative’s personality had changed: “There are some things, anger, that I’ve seen out of him that I’ve never experienced before, and it shocked me!” (Respondent CP5)
Some participants expressed strong feelings of frustration about lack of efficacy of treatments for stroke risk factors: “ How many blood pressure specialists do you think I been to since I’ve been first diagnosed at 28? It’s 20 years now and I still don’t have it under control!”(Respondent P6)
Depression/PTSD
Depression and re-living the stroke experience were also cited as psychological barriers to recovery. Some individuals described post-traumatic experiences: “when my husband first had his stroke that’s all we thought about, why did it happen to him? I would come home some nights and he would be so depressed. In the beginning he was very emotional. I mean his emotions would go from one extreme to the next and he wasn’t that type of guy. He would re-live what happened to him for a good year.” (Respondent CP2)
Knowledge Barriers
Risk Factors and Stroke Terminology
Many also cited lack of knowledge about cardiovascular risk factors and stroke-related medical terms as barriers: “The term, TIA, I never heard of that until I came here to this group.” (Respondent P6). Some individuals saw no connection between stroke and cardiovascular disease, “I’m thinking heart is one thing and stroke is something else.”(Respondent P9).
Medications
There was also confusion about purpose of medications and dissatisfaction due to side effects, “I’m very unhappy about taking 21 pills every day and I don’t really know what I’m taking.” (Respondent P9). One CP noted, “He hates taking medication. I knew before he came home, boy that’s going to really be something, and I was praying, Lord, how am I going to get this medicine down this man because he does not take it?!” (CP4)
Lifestyle Barriers
Lifestyle barriers included difficulty changing previous patterns of living and relating to others as well as using food, drugs or alcohol in ways that prevented recovery. One man, who was in a helping/care-giving profession, felt that his habit of always putting other people first was a time and energy impediment to his own recovery, “I’m always helping people, and I’m too available.” (Respondent P3). Some stroke survivors spoke about their difficulty changing ingrained habits like smoking, “I’m trying to wean myself off cigarettes” and drinking “Still drink my case of beer,” (Respondent P8). Adopting a healthier diet was difficult for many, “I eat out all the time at fast food places and I’d drink a liter or two of pop at a sitting.” (Respondent P7)
Functional Impairment Barriers
A number of participants reported functional barriers, such as diminished motor skills and cognitive problems: “I use his belt to tighten his pants because he has trouble buttoning them.” (Respondent CP3,) and “sometimes he’s discombobulated and it’s been almost 3 years now?” (Respondent CP4). Problems remembering events around stroke hospitalization were particularly relevant for most of the men: “I can’t remember most things that happened in the hospital.” (Respondent P2). Vision, speech and mobility problems were also reported and were felt to have negative effects on stroke recovery.
Self-Identity Barriers
Some saw equating being strong or manly (macho) with reluctance to seek medical care as preventing timely treatment of stroke: “The only thing I know is I came home from work and went to sleep. I had a stroke and when I woke up the next morning, and even though I was having complications, I fought my way through it for about 4 or 5 days.” (Respondent 6) In line with this idea, one individual described the change in role and perceived identity as a man after his stroke, “I noticed that they don’t call me as much to fix anything and I wondered if it’s because I had a stroke, or did they just forget to call me?” (Respondent 4) Change in body image was also a blow to identity, “your body was normal, and now your body don’t be normal no more…. I’m still trying to deal with it.” (Respondent 7)
Family and Community Level Barriers
Table 2 shows themes, descriptive codes, and illustrative quotations emerging from Family and Community Level Barriers. These barriers were classified into the two categories that reflected family and community level issues that our respondents faced in their recovery: Lack of support from family and friends and Care Partner/Family Stress
Table 2.
Family and Community Level Barriers to Post Stroke Care and Recovery Among African-American Men (AA) and Their Care Partners (CPs) (n=17)
| Themes and Categories | Illustrative Quotations from Respondents |
|---|---|
| Lack of Support from Family/Friends | “But see I grieved for many different reasons. It wasn’t just because of the stroke only. I grieved to see how people leave you when you’re distressed,. Not one soul showed up, and I helped many people.” Respondent P2 |
|
Care Partner/Family Stress Frustration/Fear Care partner risk factors Family interferences Role Changes |
“The caregivers have things too. I have diabetes and high blood pressure. I’ve taken care of him and I have a condition with my shoulder. I’m in a lot of pain.” Respondent CP5 “I guess well me and her sometimes, especially with her kids, people try to tell you what to do who have no idea what’s going on. We go to them and they try to tell us oh you shouldn’t be doing this, you shouldn’t be doing. We try to tell them we can do this, you know. We need to do this. It’s sort of difficult. That can really get on your nerves sometimes.” Respondent P9 |
Lack of Support from Family and Friends
Lack of support from family and friends was disappointing and sometimes emotionally devastating, “They couldn’t look at me, wouldn’t even come by. Had one friend tell me over the phone, I hate to see you in this situation so I don’t come by. I guess the people associate sickness with me!” (Participant 3) One man with a long road of rehabilitation and recovery reported lack of family support that he felt bordered on the criminal, “I did have some family problems, too. I had people steal from me and take from me. Some people thought I was dying and was trying to get me to sign over power of attorney.” (Respondent P1)
Care Partner/Family Stress
Family stress post-stroke was difficult to deal with and interfered with recovery. Two survivors without care partners lived with frail elderly mothers who needed support themselves. One of them also had a young son to care for that increased his burden, “He’s bringing me stress, yes he is!” (Respondent P8) Among CP’s, stress was very high on the list of the day-to-day challenges they faced in helping their family member recover. One CP spoke of her high stress level from living with the fear that her husband could have another event: “When he had his last heart attack, it was very different than the first and the second…I was so scared, I just broke down because when you go through it the first and second time and the third time you don’t know what’s going to happen next. It’s so stressful!” (Respondent CP4)
Another CP spoke about the change in roles that occurred in her family. “I’m his relative you know, and me having to bathe and dress him, although I try to make it as light as possible, it’s stressful. No man wants a female relative to see him like that.” (Respondent CP5). One CP spoke of the frustration she felt in dealing with her husband’s emotions: “I find myself really snapping sometimes. It just comes out of nowhere. You don’t want it to, it just happens.”(Respondent CP3)
Many CPs noted that they had their own stroke risk factors and sometimes neglected their own health because they were burdened with family care issues, “I am also at risk of having a TIA or heart attack because I have high blood pressure and diabetes also. So, I lean on him, he leans on me. I don’t go to the hospital on a regular basis, but he does and it’s scary for me and our children.” (Respondent CP4.)
Provider and Healthcare System Level Barriers
Table 3 shows themes, descriptive codes, and illustrative quotations emerging from Provider/Healthcare System Level Barriers. These barriers were classified into four categories that reflected provider and healthcare system issues that our respondents faced in their recovery: Loss of Identity, Patient/Clinician Relationships, Frustration with Lack of Efficacy of Treatment, and Access Difficulties.
Table 3.
Provider and Healthcare System Level Barriers to Post Stroke Care and Recovery among African-American Men (AA) and Their Care Partners (CPs) (n=17)
| Themes and Categories | Illustrative Quotations from Respondents |
|---|---|
| Loss of Identity | “So I dressed in my suit and tie one day, and I really realized, that’s when it really hit me, I’m just a number here. The doctor and nurses kept coming in and out looking for me but didn’t recognize me because I was sitting in the room and they were looking for somebody in a hospital gown. I just sat there listening and looking and they was talking, where did he go?” Participant 3 |
|
Patient/Clinician Relationships Distrust of provider Confusion about provider Lack of knowledge about black male stroke survivors Poor communication |
“Sometimes I think of the doctors as just using us as a paycheck. I think that all the while I smoked I didn’t see a lot of effort on his part to say don’t do this or you shouldn’t do that. I looked at it like if something happened because I smoked, if I got lung cancer or something like that, that’s a paycheck for the doctor. If you get sick who you gonna go see, your doctor, who gets paid, your doctor. If they write a prescription for you they get kickbacks on that from the drug companies.” Participant P2 |
| Frustration with Lack of Efficacy of Treatment | “And he has high blood pressure and the doctors got him on this medication. He started having tingling and numbness in his hands and arms, and he says the medicine seems like it’s not working. So I don’t know, everything they do is like they’re experimenting with new drugs and it seems like it’s not doing nothing for him.” Respondent CP6 |
| Access Difficulties | “Doctor X is always cancelling my appointments. You wait 35 minutes on the phone, and they’re like he’s not going to be able to see you for another 6 months!” Respondent P5 |
Loss of Identity
The loss of identity that can occur in the hospital was described vividly, and with great emotion, by one participant, who signed himself out of the hospital against medical advice post-stroke, “I said, I can’t be here because they don’t know me, and they weren’t trying to know me. They was doing a job, a service job to get me well but I know they had a lot of patients, and I was just a number to them. I had to get home to get myself better. I have to do it on my own. That was my main goal.” (Respondent P3).
Patient/Clinician Relationships
Distrust and Confusion
While some of the men felt that their doctor was just in it “for the money,” others did not even know who to follow up with for their post-stroke care: “I don’t know who my primary doc is!” (Respondent P8).
Communication and Frustration
Communication issues such as the provider using incomprehensible medical terminology to explain a health condition, and perceived indifference to their needs and problems were also identified as barriers to recovery. Other barriers were care provider unwillingness to consider or talk about alternative or complementary treatments, “I don’t like taking pills so there has to be something else you can take. I talked to my doctor about white willow bark and he kind of ridiculed what I was talking about (Respondent P2). Some participants felt that their care providers did not understand appropriate medications for high blood pressure related to the specific care needs of AA men: “So for the doctors to understand us black males as far as what medication to use, what rules to adopt, I don’t think that they know.” (Respondent 6)
Access Difficulties
Difficulty getting appointments, multiple provider cancellations, and too-short visits were other perceived barriers to recovery, “I don’t think that my doctor has enough time to explain these things, because he runs in the office. He doesn’t really have time to talk about different things, and he’s got a waiting room full of people. So he’s got to see all those people, so he comes in checks the blood pressure, and then he’s gone. And that’s it.” (Respondent 5)
Summary of findings
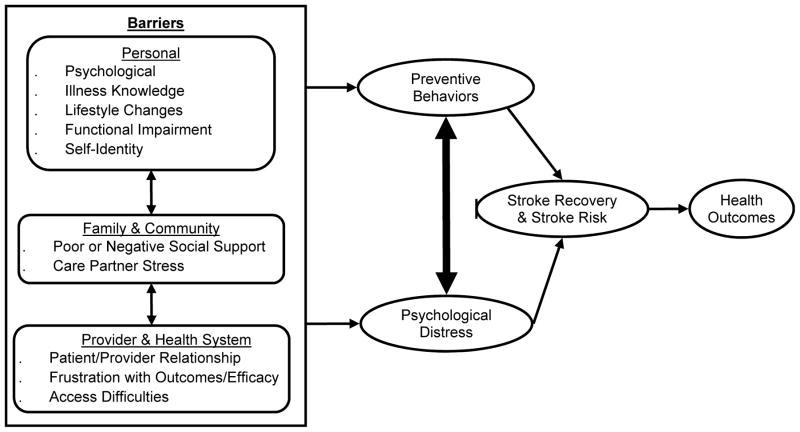
Results suggest three major thematic domains of barriers. Personal, Family/Community and Provider/Healthcare System, each represented by specific categories appeared to affect health behaviors and promote psychological distress in AA male survivors of stroke or TIA. As noted in our emergent conceptual model (Figure 1), stress was also identified as affecting self-management, and was perceived to elevate risk, affect recovery, and make adhering to guideline-concordant health behaviors more difficult.
Figure 1.
Conceptual Model of Barriers to Stroke Prevention and Recovery for African American Male Stroke Survivors
DISCUSSION
Despite stroke care advances, substantial evidence demonstrates that AA recover less completely than EA stroke patients.1–5 Racial disparities in stroke are greatest in men and in young people8, and younger AA men with stroke have much to lose with respect to future employment and social role. Current evidence-based guidelines for the prevention of stroke recurrence 25 recommend management of specific modifiable risk factors such as hypertension, hyperlipidemia and smoking, all of which are disproportionately common in AA.
Findings from our study of younger AA men with stroke/TIA identified barriers to recovery and stroke risk factor reduction spanning personal, family/community, and provider/health system domains is consistent with the McLeroy’s30 Social Ecological Model of health behavior. This model posits that behavior, actions, and events are influenced by individual, interpersonal, organizational, community and policy factors. Functional status and one’s role in personal relationships and the community are significant barriers as are dealing with anger and loss. A lack of access or knowledge about local, state or federal service programs may deter a stroke survivor from participating in programs that could help improve overall health and lessen the likelihood of rehospitalization.31 Care partners and others struggle with feeling overwhelmed and stressed, and the social environment and healthcare system are often not conducive to helping individuals deal with the multiple levels of care required (e.g., medication, doctor’s appointments, getting necessary health information).
This is the first reported qualitative study to inductively identify barriers to stroke recovery and prevention among younger AA men and their CPs. Our findings are important in that they will inform the development of a culturally sensitive self-management intervention that will be pilot tested in Phase 2 of our study. There are, however, some potential limitations in our study. Individuals did know that the study was specifically focused on AA men and it is possible that perceived barriers for AA men may differ from the broader populations. This is a limitation for stroke risk reduction/recovery broadly, but is a strength of the sample as it pertains to potentialy reducing health disparities in AA men. The use of CPs as focus group participants could potentially have had a negative impact on the AA men’s ability to be honest during the group sessions. However, we found the verbal interaction between the men and their CPs promoted open and honest dialogue which led to clarification of themes.
While our small sample size impacts broader generalization to all groups of AA men with stroke and TIA, this limitation is offset to some extent by use of rigorous qualitative research methods.26,27 The self-report method is direct and versatile. If we want to know what people think, feel, believe and experience, the most direct means of gathering information is to ask them. This method of collecting data yields information that would be difficult, if not impossible, to gather by other means. To increase validity and accuracy, findings were confirmed with participants at a follow-up Advisory Board meeting. 31 Despite these limitations, our findings have important clinical implications for health care providers.
Clinical Implications
Timing of intervention and involvement of family
Because AA are more likely to be discharged to home after a stroke rather than to rehabilitation facilities that provide intensive physical and other types of therapy13, involving spouses and other family members in recovery is likely to be particularly important for AA men. Our findings suggest that AA men may have poor recollection of care recommendations made around the time of hospital discharge. To be effective, recovery efforts will likely need to be implemented after, rather than prior to hospital discharge. Even men who had a stroke or TIA up to a year ago welcomed information on understanding stroke risk factors and dealing with barriers over time.
Acknowledge stress and target stress management and reduction
While biological risk reduction strategies are well described in AHA/ASA guidelines25 and improve stroke recovery, a primary focus on biomarkers may not fully capture the salient aspects of health management for AA stroke survivors. Young AA men in this study identified psychological barriers, in particular stress, as critical impediments to good health outcomes. While the data is somewhat inconsistent, there is a reasonable body of evidence associating stress with multiple health conditions including obesity, diabetes and cardiovascular disease.32,33 Manenshijn32 suggested that long-term elevated cortisol may be an important cardiovascular risk factor, and it is possible that clinical use of complementary and alternative stress reduction therapies could engage AA stroke survivors and reduce stroke risk
Post-stroke depression, seen in approximately one-third of stroke survivors, negatively impacts recovery. It may be under-recognized in AA men because of gender and culturally-related factors.35,36 In our sample, both stroke survivors and CPs clearly described depressive and post-traumatic stress disorder symptoms that were troubling to both patients and families. Care approaches that “normalize” such symptoms might reduce shame and stigma while also making treatment, if indicated, more acceptable.
Reducing isolation and feelings of exclusion
Attitudes towards treatment and self-management affect acceptance and use of post-stroke care14. Stroke survivors and care partners (CPs) who are supported and empowered may participate more fully in post-stroke care.37,38 Similar to our findings, others have reported that AA men tend to delay seeking medical care until symptoms arise or significantly interfere with their lives.38.39 Our participants described feeling under-valued and felt that providers and care teams did not understand their challenges and specific issues as AA men. Care approaches that directly involve patients in the care process might address these barriers. For example, another qualitative study of 13 stroke survivors (85% were AA) reported 3 key barriers to recommended post-stroke exercise (post-stroke physical impairments, lack of motivation, and environmental factors) and suggested that peer and provider social support may enhance AA stroke survivors’ physical activity.12 Consistent with the growing patient empowerment/consumer movement, involving patients in decision making and embedding patients themselves into clinical care teams may promote active and engaged care and could help address this important barrier and minimize health disparities for AA men.40
In sum, young AA men with stroke/TIA encounter personal, family/community and healthcare system barriers to stroke prevention and recovery. Biological risk reduction education may not capture all salient aspects of health management for AA stroke survivors. Leveraging the strengths of the family and community, incorporating psychological health considerations, and engaging patients more directly in healthcare teams may help reduce health disparities for AA men.
Acknowledgments
SOURCES OF FUNDING
Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number R21NR013001. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
DISCLOSURES: Non except for the following: Dr. Sajatovic has received Research grants from Pfizer, Merck, Ortho-McNeil Janssen, Reuter Foundation, Woodruff Foundation, Reinberger Foundation, National Institutes of Health (NIH), Centers for Disease Control (CDC). She has been a consultant to United BioSource Corporation (Bracket), Prophase, Otsuka, Pfizer, Amgen. She has received Royalties from Springer Press, Johns Hopkins University Press, Oxford Press, Lexicomp. Dr. Sila is a consultant to Medtronic, Abbott, Cleveland Clinic Cardiovascular Co-ordinating Center.
References
- 1.American Heart Association. Heart Disease and Stroke Statistics: 2007 Update: A Report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Dallas, TX: American Heart Association; 2007. [Google Scholar]
- 2.Kissela B, Schneider A, Kleindorfer D, et al. Stroke in a biracial population: the excess burden of stroke among blacks. Stroke. 2004 Feb;35(2):426–431. doi: 10.1161/01.STR.0000110982.74967.39. [DOI] [PubMed] [Google Scholar]
- 3.Eaves YD. ‘What happened to me’: rural African American elders’ experiences of stroke. The Journal of neuroscience nursing : journal of the American Association of Neuroscience Nurses. 2000 Feb;32(1):37–48. [PubMed] [Google Scholar]
- 4.Gillum RF. Secular trends in stroke mortality in African Americans: the role of urbanization, diabetes and obesity. Neuroepidemiology. 1997;16(4):180–184. doi: 10.1159/000109685. [DOI] [PubMed] [Google Scholar]
- 5.Roth DL, Haley WE, Clay OJ, et al. Race and gender differences in 1-year outcomes for community-dwelling stroke survivors with family caregivers. Stroke. 2011 Mar;42(3):626–631. doi: 10.1161/STROKEAHA.110.595322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2009 Apr 17;57(14):1–134. [PubMed] [Google Scholar]
- 7.Brown DL, Boden-Albala B, Langa KM, et al. Projected costs of ischemic stroke in the United States. Neurology. 2006 Oct 24;67(8):1390–1395. doi: 10.1212/01.wnl.0000237024.16438.20. [DOI] [PubMed] [Google Scholar]
- 8.Bian J, Oddone EZ, Samsa GP, Lipscomb J, Matchar DB. Racial differences in survival post cerebral infarction among the elderly. Neurology. 2003 Jan 28;60(2):285–290. doi: 10.1212/01.wnl.0000041492.58594.4d. [DOI] [PubMed] [Google Scholar]
- 9.Murray CJ, Lopez AD. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries and Risk Factors in 1990 and Projected to 2020. Boston, MA: Harvard School of Public Health; 1996. [Google Scholar]
- 10.Sowers JR, Ferdinand KC, Bakris GL, Douglas JG. Hypertension-related disease in African Americans. Factors underlying disparities in illness and its outcome. Postgraduate medicine. 2002 Oct;112(4):24–26. 29–30, 33–24. doi: 10.3810/pgm.2002.10.1331. passim. [DOI] [PubMed] [Google Scholar]
- 11.Battersby M, Hoffmann S, Cadilhac D, Osborne R, Lalor E, Lindley R. ‘Getting your life back on track after stroke’: a Phase II multi-centered, single-blind, randomized, controlled trial of the Stroke Self-Management Program vs. the Stanford Chronic Condition Self-Management Program or standard care in stroke survivors. International journal of stroke : official journal of the International Stroke Society. 2009 Apr;4(2):137–144. doi: 10.1111/j.1747-4949.2009.00261.x. [DOI] [PubMed] [Google Scholar]
- 12.Damush TM, Plue L, Bakas T, Schmid A, Williams LS. Barriers and facilitators to exercise among stroke survivors. Rehabilitation nursing : the official journal of the Association of Rehabilitation Nurses. 2007 Nov-Dec;32(6):253–260. 262. doi: 10.1002/j.2048-7940.2007.tb00183.x. [DOI] [PubMed] [Google Scholar]
- 13.Ottenbacher KJ, Campbell J, Kuo YF, Deutsch A, Ostir GV, Granger CV. Racial and ethnic differences in postacute rehabilitation outcomes after stroke in the United States. Stroke. 2008 May;39(5):1514–1519. doi: 10.1161/STROKEAHA.107.501254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stansbury JP, Jia H, Williams LS, Vogel WB, Duncan PW. Ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke. 2005 Feb;36(2):374–386. doi: 10.1161/01.STR.0000153065.39325.fd. [DOI] [PubMed] [Google Scholar]
- 15.Tuhrim S. Editorial comment--ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke. 2005 Feb;36(2):386–387. doi: 10.1161/01.STR.0000153060.06006.00. [DOI] [PubMed] [Google Scholar]
- 16.Krueger RA. Focus Groups: A Practical Guide for Applied Research. Thousand Oaks, CA: Sage Publications, Inc; 1994. [Google Scholar]
- 17.Anderson R, Barr P, Edwards Using focus groups to identify psychosocial issues of urban Black individual with diabetes. Diabetes Educator. 1996;(22):28–33. doi: 10.1177/014572179602200104. [DOI] [PubMed] [Google Scholar]
- 18.Dunn C, Pirie P, Lando H. Attitudes and perceptions related o smoking among pregnant and postpartum women in a low-income multi-ethnic setting. American Journal of Health Promotion. 1998;12:267–274. doi: 10.4278/0890-1171-12.4.267. [DOI] [PubMed] [Google Scholar]
- 19.Maillet N, Melkus G, Spollet Using focus groups to characterize the health beliefs and practices of Black women with non-insulin dependent diabetes. Diabetes Educator. 1996;(22):39–46. doi: 10.1177/014572179602200106. [DOI] [PubMed] [Google Scholar]
- 20.Manfredi C, Lacy L, Warnecke R, Balch G. Method effects in survey and focus group findings: Understanding smoking cessation in low SES African-American women. Health Education and Behavior. 1997;(24):786–800. doi: 10.1177/109019819702400612. [DOI] [PubMed] [Google Scholar]
- 21.Mein S, Winkleby M. Concerns and misconceptions about cardiovascular disease risk factors: A focus group evaluation with low income Hispanic women. Hispanic Journal of Behavioral Sciences. 1998;(20):192–211. [Google Scholar]
- 22.Kasner SE. Clinical interpretation and use of stroke scales. Lancet neurology. 2006 Jul;5(7):603–612. doi: 10.1016/S1474-4422(06)70495-1. [DOI] [PubMed] [Google Scholar]
- 23.Mahoney FI, Barthel DW. Functional Evaluation: The Barthel Index. Maryland state medical journal. 1965 Feb;14:61–65. [PubMed] [Google Scholar]
- 24.Wade DT, Collin C. The Barthel ADL Index: a standard measure of physical disability? International disability studies. 1988;10(2):64–67. doi: 10.3109/09638288809164105. [DOI] [PubMed] [Google Scholar]
- 25.Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2011 Jan;42(1):227–276. doi: 10.1161/STR.0b013e3181f7d043. [DOI] [PubMed] [Google Scholar]
- 26.Berg BL. Qualitative Research Methods for the Social Sciences. Boston, MA: Allyn & Bacon; 1998. [Google Scholar]
- 27.Ezzy D. Qualitative Analysis: Practice and Innovation. London [New York, NY]: Routledge; Crows Nest NSW: Allen & Unwin; 2002. [Google Scholar]
- 28.Morse J. Qualitative Health Research. Thousand Oaks, CA: Sage Publications, Inc; 2002. [Google Scholar]
- 29.Yanow D, Schwartz-Shea P. Interpretation and method: Empirical research methods and the interpretive turn. Armonk, New York: ME Sharpe, Inc; 2006. [Google Scholar]
- 30.McLeroy K, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Heal Ed Qu. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 31.Pang M, Harris J, Eng J. A community-based upper-extremity group exercise program improves motor function and performance of functional activities in chronic stroke: a randomized controlled trial. Archives of Phys Med Rehabil. 2006;87(1):1–9. doi: 10.1016/j.apmr.2005.08.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manenschijn L, Schaap L, van Schoor NM, et al. High long-term cortisol levels, measured in scalp hair, are associated with a history of cardiovascular disease. The Journal of clinical endocrinology and metabolism. 2013 May;98(5):2078–2083. doi: 10.1210/jc.2012-3663. [DOI] [PubMed] [Google Scholar]
- 33.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999 Apr 27;99(16):2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 34.Cardiovascular Disease Deaths Among African Americans. Illinois Department of Public Health; [Google Scholar]
- 35.McGruder HF, Malarcher AM, Antoine TL, Greenlund KJ, Croft JB. Racial and ethnic disparities in cardiovascular risk factors among stroke survivors: United States 1999 to 2001. Stroke. 2004 Jul;35(7):1557–1561. doi: 10.1161/01.STR.0000130427.84114.50. [DOI] [PubMed] [Google Scholar]
- 36.Hassaballa H, Gorelick PB, West CP, Hansen MD, Adams HP., Jr Ischemic stroke outcome: racial differences in the trial of danaparoid in acute stroke (TOAST) Neurology. 2001 Aug 28;57(4):691–697. doi: 10.1212/wnl.57.4.691. [DOI] [PubMed] [Google Scholar]
- 37.Jia H, Chumbler NR, Wang X, et al. Racial and ethnic disparities in post-stroke depression detection. International journal of geriatric psychiatry. 2010 Mar;25(3):298–304. doi: 10.1002/gps.2339. [DOI] [PubMed] [Google Scholar]
- 38.Allen JD, Kennedy M, Wilson-Glover A, Gilligan TD. African-American men’s perceptions about prostate cancer: implications for designing educational interventions. Social science & medicine. 2007 Jun;64(11):2189–2200. doi: 10.1016/j.socscimed.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 39.Ravenell JE, Whitaker EE, Johnson WE., Jr According to him: barriers to healthcare among African-American men. Journal of the National Medical Association. 2008 Oct;100(10):1153–1160. doi: 10.1016/s0027-9684(15)31479-6. [DOI] [PubMed] [Google Scholar]
- 40.Oliver S, Clarke-Jones L, Rees R, et al. Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach. Health technology assessment. 2004 Apr;8(15):1–148. III–IV. doi: 10.3310/hta8150. [DOI] [PubMed] [Google Scholar]