Abstract
Objectives:
This study was conducted to assess the clinic-epidemiological profile of snakebite cases admitted at a Tertiary Care Centre in South India.
Materials and Methods:
A record based retrospective study was carried out at Kasturbha Medical College affiliated hospitals in Mangalore. All the snakebite cases admitted to the hospitals from January 2007 to December 2011 were included in the study. Data were collected using a pretested semi-structured questionnaire and analyzed using Statistical Package for Social Sciences (SPSS version 11.5). The results are expressed as percentages.
Results:
The study included 198 cases of snakebite victims. The majority of the cases were males (68.2%). The mean age of the study population was 34.8 years. Maximum numbers of snakebite cases were reported during the month of September to December (47.9%). The peak time of snakebite was between 18.01 and 24.00 h which was reported in 40.5% of the cases. Lower extremities were the most common site of bite in more than three-fourth of the cases (80.9%). The most common symptoms were a pain (45.9%) and swelling (44.9%). The case fatality rate was observed to be 3.0%.
Conclusion:
Snakebite still remains a major public health problem in this part of the world. Knowledge must be imparted regarding the prevention of snakebites through community health programs. Messages regarding prompt reporting of such cases and importance of effective treatment must be disseminated among people through mass media and role plays.
Keywords: Mangalore, public health, snakebite, South India
INTRODUCTION
Snakebite is one of the neglected tropical diseases that World Health Organization (WHO) aimed to eradicate.[1] However, it has been excluded from WHO report of 2010 and 2013 on neglected tropical diseases. Currently, snakebite has been included along with other neglected non-tropical diseases such as strongyloidiosis, scabies, mycetoma, etc.[2,3] The problem of snakebites has been persistently neglected by public health personnel, clinicians and policy makers even though its social and economic impact are wide-spread.[4]
Around 4.2 lakh cases of snakebite envenomation and 20,000 deaths have been reported globally, but the actual figures may be much higher. Estimations did conservatively have revealed the death rate to be 0.297/lakh population ranging from 0.001 in North American region to 2.434 in Oceania region.[5] The regions mainly affected by snakebites are South Asia, South East Asia and Sub-Saharan Africa.[1] Envenomation in India is estimated to be at 81,000/year, which is highest in the world, followed by Sri Lanka, Vietnam and Brazil.[5] In India, Uttar Pradesh, Andhra Pradesh and Bihar are the worst affected states, with the majority of the deaths being reported in Andhra Pradesh.[6]
The increased mortality and morbidity in tropical countries is attributed to the scarcity of anti-snake venoms, minimal access and poor quality of healthcare services.[7] People in countries like India prefer traditional healers rather than trained doctors, mainly because of ignorance and monetary issues as a result of which 77% of the snakebite victims in rural areas die outside the health care set up.[8] Snakebites can cause severe complications like shock, systemic bleeding, respiratory muscle paralysis, acute renal failure and necrosis of tissue at the site of the bite. Snakes from the family Viperidae and Elapidae are known to cause more severe consequences. Since complications of snakebite develop rapidly and irreversibly, medical intervention must be prompt and appropriate.[9]
Even though deaths due to snakebite can be prevented, the mortality continues to be high because of lack of knowledge among doctors regarding the management of snakebite cases. This along with a delay in conventional treatment, lack of anti-snake venom and lack of facilities of tracheal intubation and ventilation by the bag-valve mask in neuro-toxic cases have been major factors for death due to snakebites.[10]
Unlike the other public health problems, which have received a lot of attention from both the policymakers and healthcare providers, snakebite has been grossly neglected by many. Hence, the current study was conducted with the objective of assessing the clinical and epidemiological profile of snakebite victims admitted to a tertiary care hospital in a coastal part of south India.
MATERIALS AND METHODS
The present record based retrospective study was carried out at Kasturbha Medical College (KMC) affiliated hospitals in Mangalore. These are referral hospitals in coastal Karnataka where patients come from nearby districts and neighboring states.
A prior approval was obtained from the Institutional Ethics Committee of Kasturba Hospital, Mangalore before the commencement of the study. Permission was then obtained from the Department of Medicine and Medical Superintendent of respective hospitals to access registries of snakebite patients from the medical records department.
All snakebite cases admitted at KMC hospitals during a 5 years period extending from January 01, 2007 to December 31, 2011 were included in the study. The case records were reviewed and detailed information regarding sociodemographic profile, time and site of the bite, presenting complaints and time interval between snakebite and receiving medical treatment was recorded in a data capture sheet. Data collected was entered and analyzed using Statistical Package for Social Sciences (SPSS version 11.5; SPSS Inc., 233 South Wacker Drive, 11th floor, Chicago, IL 60606-6412). The analysis of data was carried out after entering the coded information and tables were generated. The results are expressed as percentages in the presented tables.
RESULTS
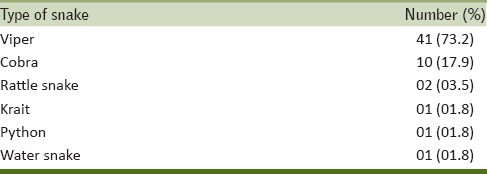
A total of 198 cases of snakebites were reported during the study period. The majority of the cases were males (n = 135, 68.2%) with the male to female ratio being 2.1:1. The mean age of the study population was found to be 34.8 years. The highest proportion of snakebite was observed in the age-group of 21–30 years (n = 50, 25.2%), followed by 41–50 years [Table 1]. The maximum number of snakebite cases (n = 95, 47.9%) were reported during the month of September to December followed by the months of May–August (n = 55, 27.7%). The peak time of snakebite was between 18.01 and 24.00 h, which was reported in 40.5% of the cases (n = 80). Lower extremities were the most common site of bite in more than three-fourth of the cases (n = 160, 80.9%). Details of snakebites in the study sample are shown in Table 2. Pain (n = 91, 45.9%) and swelling (n = 89, 44.9%) were the most common symptoms as reported by the patients at the time of admission [Table 3]. Both local and systemic envenomation was present in 51.6% (n = 102) of the cases and in 18.1% (n = 36) of the cases only local envenomation was observed. No envenomation was observed in 30.3% (n = 60) of the cases. The time interval between snakebite and reporting of the patient to the health unit was <24 h in 80.8% (n = 160) of the cases. The case fatality rate in our study was observed as 3.0%. The species of the snake responsible for the bite was not identified in the majority (n = 142, 72.4%) of the cases. Among the other cases, the most common species of snake identified was viper (n = 41, 73.2%), followed by cobra (n = 10, 17.9%) as shown in Table 4.
Table 1.
Age and sex distribution of snakebite victims (n=198)
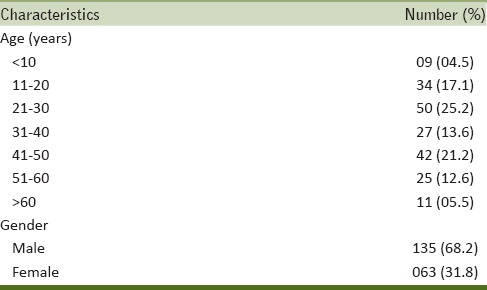
Table 2.
Details of snakebite in the study sample (n=198)
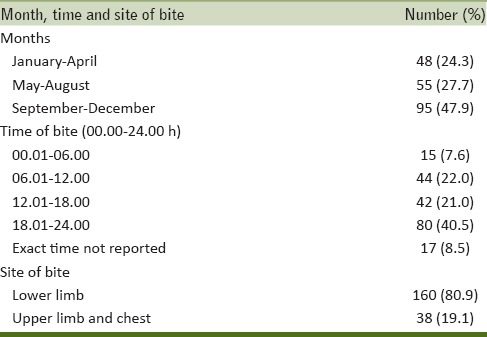
Table 3.
Profile of symptoms among snakebite victims (n=198)
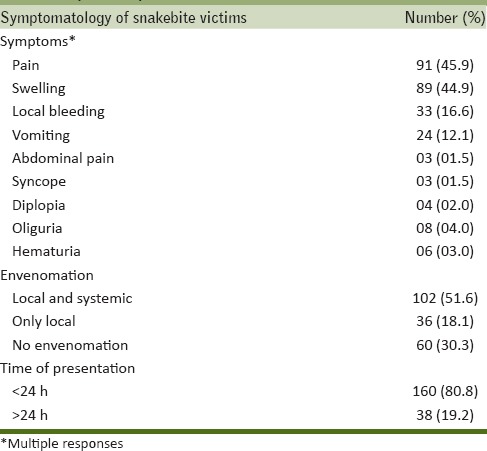
Table 4.
Species of snake identified (n=56)
DISCUSSION
Snakebite is one of the medical emergencies, most commonly reported from the developing countries of the tropical region. It predominantly affects the young working population. As a result of under-reporting, the actual pattern of morbidity and mortality pattern remains vastly unknown. Persistent efforts thus have been made to make it a notifiable disease in the South East Asian Region (SEAR) of the WHO.[11]
This study explored the profile of 198 snakebite victims and analyzed their sociodemographic and epidemiological details. The male to female ratio of the study participants was 2.1:1. Similar findings have been reported from the studies conducted in different parts of India and in SEAR.[12,13,14,15,16] A higher male-female ratio was noted in studies conducted in Gujarat[17] and Andhra Pradesh[18] whereas studies conducted in other parts of Karnataka showed a lower male-female ratio.[19,20,21] Agriculture is the predominant occupation in this part of the country that requires outdoor activities mainly. Males are usually involved in agriculture related activities than females and hence, the predominance of male victim of snakebites in the study when compared to females.[22] Three-fourth of the cases in our study were in the age group between 11 and 50 years. Very few cases were observed in the extremes of the ages, with maximum cases clustering around the age group of 30 years, which was in congruence to the findings of studies conducted elsewhere in India and abroad.[5,23,24,25,26]
The maximum incidence of snakebites in the present study was reported during the post-monsoon months of September to December which is further in support of findings of other studies.[27,28,29] Contrastingly, studies conducted in different parts of India[12,30] have shown a higher incidence of snakebites during the monsoon months. A study from Iran observed increased snakebite incidence during summers when compared to other time of the year.[31] The reason for increased incidence of snakebites in the post monsoon season in our study could be due to the fact that there is an increase in agricultural and constructional activities during this period.
Our study revealed that maximum cases of snakebite occurred between 6 pm and 12 am which is similar to the observations made elsewhere.[21,30,32] It is during the time of dusk that snakes come out in search of their prey and become active during this period. Due to diminished vision during dusk and at night, people may accidentally step on the snakes resulting in bites. Most common site of the bite was lower extremities. Rarely, people were bitten on forearms and chest while sleeping on the floor when snakes enter the human habitat in search of their prey or sometimes when the snake is accidentally handled while lifting the vegetations. In the present study, the majority of the victims were bitten in the lower limb which is in conformity with the findings of several other studies.[12,14,15,17,19,20,22,32,33,34,35]
Type of snake was identified by only 28.2% of the victims in the present study. Most of the snakebites in India are a result of bites of Cobra, Russels Viper and Common Krait that are the more commonly encountered species among the 13 known species of poisonous snakes. Our observations are in accordance with the studies conducted in Thailand[36] and India.[18,21,22,34,35] The most common symptom reported was local pain followed by swelling which is similar to those reported in other studies.[15,19,33,37] More than three-fourth of the victims were admitted in a hospital within 24 h of snakebite. The majority (69.6%) of the victims received anti-snake venom after admission to the hospital. Consistent with our findings, similar pattern of admission has been reported in other similar studies.[18,33,37] It has been emphasized that immobilization and prompt hospitalization, with timely medical intervention in the form of anti-snake venom, holds significance in reducing the mortality associated with snakebites.[22,34,35] Case fatality rate in the present study was observed as 3.0% which is much lower than that reported in other studies conducted in other parts of India.[12,33,37] Lack of awareness on snakebites and its potential hazards, delay in seeking timely medical advice, difficulty in identification of snakes, and lack of health care facilities in remote areas are some of the issues that need to be highlighted in tackling with the problem of snakebite and its treatment.[38] The lower case fatality can be attributed to higher literacy and education rate, and increased awareness on the issue of snakebites among people in Mangalore.Availability of excellent healthcare facilities in the region with a sea of medical colleges and private clinics may be a predominant factor for the lower case fatality rates reported in the present study.
CONCLUSIONS AND RECOMMENDATION
Snakebite still remains a major public health problem in this part of the world which mainly affects people from productive age group. Viper and cobra are the most common snakes among the identified cases of snakebites. Snakebite cases occur more commonly reported in post-monsoon season and during the dusk.
People must be advised to use long pants and gumboots while working outdoors and to wear gloves while handling debris. Knowledge must be imparted regarding the prevention of snakebites through community health programs. Messages regarding prompt reporting of such cases and importance of effective treatment must be disseminated among people through mass media and through role plays and puppet shows at the village level. In this regard, social media can be used effectively to promote the message among younger generations.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.World Health Organization. Neglected Tropical Diseases. [Last cited on 2014 Aug 07]. Available from: http://www.who.int/neglected_diseases/diseases/snakebites/en/
- 2.Crompton DW, Peters P, editors. World Health Organization. Working to overcome the global impact of neglected tropical diseases: First WHO report on neglected tropical diseases. Geneva: Department for the Control of Neglected Tropical Diseases, WHO; 2010. p. 172. [Google Scholar]
- 3.Crompton DW, editor. World Health Organization. Sustaining the drive to overcome the global impact of neglected tropical diseases: Second WHO report on neglected tropical diseases. Geneva: Department for the Control of Neglected Tropical Diseases, WHO; 2013. p. 172. [Google Scholar]
- 4.Bhaumik S. Snakebite: A forgotten problem. BMJ. 2013;346:f628. doi: 10.1136/bmj.f628. [DOI] [PubMed] [Google Scholar]
- 5.Kasturiratne A, Wickremasinghe AR, de Silva N, Gunawardena NK, Pathmeswaran A, Premaratna R, et al. The global burden of snakebite: A literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 2008;5:e218. doi: 10.1371/journal.pmed.0050218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mohapatra B, Warrell DA, Suraweera W, Bhatia P, Dhingra N, Jotkar RM, et al. Snakebite mortality in India: A nationally representative mortality survey. PLoS Negl Trop Dis. 2011;5:e1018. doi: 10.1371/journal.pntd.0001018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hansdak SG, Lallar KS, Pokharel P, Shyangwa P, Karki P, Koirala S. A clinico-epidemiological study of snake bite in Nepal. Trop Doct. 1998;28:223–6. doi: 10.1177/004947559802800412. [DOI] [PubMed] [Google Scholar]
- 8.Warrell DA, Gutiérrez JM, Calvete JJ, Williams D. New approaches and technologies of venomics to meet the challenge of human envenoming by snakebites in India. Indian J Med Res. 2013;138:38–59. [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Rabies and Envenoming's: A Neglected Public Health Issue. 2007. [Last accessed on 2008 May 01; Last cited on 2014 Jul 10]. Available from: http://www.who.int/bloodproducts/animal_sera/Rabies.pdf .
- 10.Bawaskar HS, Bawaskar PH. Envenoming by the common krait (Bungarus caeruleus) and Asian cobra (Naja naja): Clinical manifestations and their management in a rural setting. Wilderness Environ Med. 2004;15:257–66. doi: 10.1580/1080-6032(2004)015[0257:ebtckb]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 11.Warell D. Guidelines for the management of snake-bites. Geneva: WHO Regional Office for South-East Asia; 2010. [Last cited on 2014 Aug 26]. Available from: http://www.apps.searo.who.int/PDS_DOCS/B4508.pdf . [Google Scholar]
- 12.Inamdar IF, Aswar NR, Ubaidulla M, Dalvi SD. Snakebite: Admissions at a Tertiary Health Care Centre in Maharashtra, India. S Afr Med J. 2010;100:456–8. doi: 10.7196/samj.3865. [DOI] [PubMed] [Google Scholar]
- 13.Whitehall JS, Yarlini M, Arunthathy M, Varan, Kaanthan, Isaivanan, et al. Snake bites in north east Sri Lanka. Rural Remote Health. 2007;7:751. [PubMed] [Google Scholar]
- 14.Joshi HS, Mahmood SE, Joshi MC, Shaifali I, Srivastava PC. Clinico-epidemiological profile of snake bite cases in Western Nepal. TAF Prev Med Bull. 2012;11:57–62. [Google Scholar]
- 15.Logaraj M, Thirumavalavan R, Gopalakrishnan S. Epidemiology of snake bite reported in a Medical College Hospital in Tamil Nadu. Int J Health Allied Sci. 2013;2:53–5. [Google Scholar]
- 16.Suchithra N, Pappachan JM, Sujathan P. Snakebite envenoming in Kerala, South India: Clinical profile and factors involved in adverse outcomes. Emerg Med J. 2008;25:200–4. doi: 10.1136/emj.2007.051136. [DOI] [PubMed] [Google Scholar]
- 17.Jarwani B, Jadav P, Madaiya M. Demographic, epidemiologic and clinical profile of snake bite cases, presented to emergency medicine department, Ahmedabad, Gujarat. J Emerg Trauma Shock. 2013;6:199–202. doi: 10.4103/0974-2700.115343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brunda G, Sashidhar RB. Epidemiological profile of snake-bite cases from Andhra Pradesh using immunoanalytical approach. Indian J Med Res. 2007;125:661–8. [PubMed] [Google Scholar]
- 19.Halesha BR, Harshavardhan L, Lokesh AJ, Channaveerappa PK, Venkatesh KB. A study on the clinico-epidemiological profile and the outcome of snake bite victims in a Tertiary Care Centre in Southern India. J Clin Diagn Res. 2013;7:122–6. doi: 10.7860/JCDR/2012/4842.2685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shetty AK, Jirli PS. Incidence of snake bites in Belgaum. J Indian Acad Forensic Med. 2010;8:139–41. [Google Scholar]
- 21.Saravu K, Somavarapu V, Shastry AB, Kumar R. Clinical profile, species-specific severity grading, and outcome determinants of snake envenomation: An Indian Tertiary Care Hospital-based prospective study. Indian J Crit Care Med. 2012;16:187–92. doi: 10.4103/0972-5229.106499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Monteiro FN, Kanchan T, Bhagavath P, Kumar GP, Menezes RG, Yoganarasimha K. Clinico-epidemiological features of viper bite envenomation: A study from Manipal, South India. Singapore Med J. 2012;53:203–7. [PubMed] [Google Scholar]
- 23.de Silva A. Snake bite in Anuradhapura District. Snake. 1981;13:117–30. [PubMed] [Google Scholar]
- 24.Sharma SK, Khanal B, Pokhrel P, Khan A, Koirala S. Snakebite-reappraisal of the situation in Eastern Nepal. Toxicon. 2003;41:285–9. doi: 10.1016/s0041-0101(02)00289-1. [DOI] [PubMed] [Google Scholar]
- 25.Suleman MM, Shahab S, Rab MA. Snake bite in the Thar Desert. J Pak Med Assoc. 1998;48:306–8. [PubMed] [Google Scholar]
- 26.Ariaratnam CA, Sheriff MH, Theakston RD, Warrell DA. Distinctive epidemiologic and clinical features of common krait (Bungarus caeruleus) bites in Sri Lanka. Am J Trop Med Hyg. 2008;79:458–62. [PubMed] [Google Scholar]
- 27.Lal P, Dutta S, Rotti SB, Danabalan M, Kumar V. Epidemiological profile of snakebite cases admitted in JIPMER Hospital. Indian J Community Med. 2001;26:36. [Google Scholar]
- 28.Buranasin P. Snakebites at Maharat Nakhon Ratchasima Regional Hospital. Southeast Asian J Trop Med Public Health. 1993;24:186–92. [PubMed] [Google Scholar]
- 29.Rano M. A study of snake bite cases. J Pak Med Assoc. 1994;44:289. [PubMed] [Google Scholar]
- 30.Sharma N, Chauhan S, Faruqi S, Bhat P, Varma S. Snake envenomation in a north Indian hospital. Emerg Med J. 2005;22:118–20. doi: 10.1136/emj.2003.008458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dehghani R, Rabani D, Panjeh Shahi M, Jazayeri M, Sabahi Bidgoli M. Incidence of snake bites in Kashan, Iran during an eight year period (2004-2011) Arch Trauma Res. 2012;1:67–71. doi: 10.5812/atr.6445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chew KS, Khor HW, Ahmad R, Rahman NH. A five-year retrospective review of snakebite patients admitted to a tertiary university hospital in Malaysia. Int J Emerg Med. 2011;4:41. doi: 10.1186/1865-1380-4-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wanje SD, Rambhau DG. Clinical profile of snake bite cases in Marathwada, India. Indian J Fundam Applied Life Sci. 2011;1:93–9. [Google Scholar]
- 34.Monteiro FN, Kanchan T, Bhagavath P, Kumar GP. Epidemiology of Cobra bite in Manipal, Southern India. J Indian Acad Forensic Med. 2010;32:224–7. [Google Scholar]
- 35.Monteiro FN, Kanchan T, Bhagavath P, Kumar GP. Krait bite poisoning in Manipal region of Southern India. J Indian Acad Forensic Med. 2011;33:43–5. [Google Scholar]
- 36.Viravan C, Looareesuwan S, Kosakarn W, Wuthiekanun V, McCarthy CJ, Stimson AF, et al. A national hospital-based survey of snakes responsible for bites in Thailand. Trans R Soc Trop Med Hyg. 1992;86:100–6. doi: 10.1016/0035-9203(92)90463-m. [DOI] [PubMed] [Google Scholar]
- 37.Anjum A, Husain M, Hanif SA, Ali SM, Beg M, Sardha M, et al. Epidemiological profile of snake bite at Tertiary Care Hospital, North India. J Forensic Res. 2012;3:146. [Google Scholar]
- 38.Shetty BS, Kanchan T, Shrinidhi, Shetty AJ, Monteiro FN. Snake bite and its treatment – The essential awareness. Indian J Forensic Med Pathol. 2011;4:79–81. [Google Scholar]


