Abstract
Objective
To assess levels of physical activity the use of objective physical activity measures like accelerometers is promising. We investigated characteristics associated with non-participation in accelerometry within an apparently healthy sample.
Methods
Among German participants of a cardiovascular examination program (CEP; 2012–2013), 470 participants aged 40–75 years were invited to wear an accelerometer for 7 days. We used multivariate logistic regression to estimate the association between non-participation and the following characteristics of participants: sex, age, education, smoking, setting of recruitment for the CEP (general medical practices, job agencies, statutory health insurance), self-reported general health, and objective health criteria such as cardiorespiratory fitness and absolute number of cardiometabolic risk factors (elevated waist circumference, blood pressure, triglycerides, blood glucose, and reduced high-density lipoprotein). Subsequently, we stratified this analysis by sex.
Results
Among all invited individuals, N = 235 (60.0% women) gave consent to participate in accelerometry. Women were more likely to decline participation (odds ratio, 1.7; 95% confidence interval, 1.1–2.7) compared to men. Stratified analyses revealed the absolute number of risk factors as predictor of non-participation for men (1.4; 1.01–2.0), while there was no predictor found in women.
Conclusion
We found a self-selection bias in participation in accelerometry. Women declined study participation more likely than men. The number of cardiometabolic risk factors decreased compliance only in men. Future studies should consider strategies to reduce this bias.
Keywords: Physical activity, Accelerometer, Selection bias, Cardiometabolic risk factors
Highlights
-
•
We investigated characteristics associated with non-participation in accelerometry.
-
•
50% of participants agreed to wear an accelerometer for 7 days.
-
•
Women were more likely to decline participation in accelerometry compared to men.
-
•
The number of cardiovascular risk factors predicted non-participation for men.
-
•
None of the considered variables predicted non-participation for women.
Introduction
Measurement of physical activity is relevant for a variety of studies such as intervention studies aiming to enhance physical activity to reduce cardiovascular risks. Self-reported levels of physical activity differ substantially from directly measured levels of physical activity (Prince et al., 2008, Troiano et al., 2008). To assess physical activity accurately within populations or to evaluate precisely the effectiveness of interventions addressing physical activity the use of objective physical activity measures is seen as optimal by now (Davis and Fox, 2007, Prince et al., 2008, Reilly et al., 2008).
Objective measures, like accelerometric motion sensors, have the advantages to reduce reporting bias (Reilly et al., 2008) and recall bias (Brown and Werner, 2008). However, disadvantages include the possibility to increase selection bias, the self-selection of individuals to participate in a study. The use of accelerometers as assessment tools implies, for example, a higher burden for study participants compared to surveys and may lead to non-participation for different groups. So far only few studies investigated characteristics associated with consent to participate in an accelerometer study (Harris et al., 2008) or associated with valid participation in wearing an accelerometer according to the study protocol (4–7 days, 10 h per day; Inoue et al., 2010, Roth and Mindell, 2013). Analyses from Harris et al. (2008) revealed that participants 65 years of age or older who agreed to participate in an accelerometer study are more likely to be male, to have higher levels of physical activity, and to report poorer health, e.g., chronic pain or chronic diseases. To our knowledge, no study investigated differences between participants who agreed to participate in an accelerometer study and non-participants with respect to objectively assessed health criteria such as cardiorespiratory fitness (CRF) and the presence of cardiometabolic risk factors. Lower CRF measured as peak oxygen uptake during standardized exercise testing is associated with lower self-reported physical activity and a higher likelihood to show an unfavorable cardiovascular risk profile (Aspenes et al., 2011). Cardiometabolic risk factors that are also considered for the definition of the metabolic syndrome, such as elevated waist circumference, blood pressure, triglycerides, or blood glucose, and reduced high-density lipoprotein, are associated with a high risk for cardiovascular diseases (CVD) (Grundy et al., 2005).
Our purpose was to identify variables that are associated with non-participation in wearing an accelerometer for 7 days in a sample of subjects recruited from the general population, who already participated in a cardiovascular examination program. We considered objective health criteria such as objectively measurable cardiometabolic risk factors and CRF as well as parameters that have been previously considered as predictors for non-participation in accelerometer studies such as self-reported general health, smoking status, and socio-demographic variables.
Methods
Study population and design
This study was part in a series of studies to investigate reach of different German population groups (Glasgow et al., 1999) within a stepwise provided screening and examination program addressing cardiovascular health. Participants were recruited between June 2012 and December 2013 by different strategies in three settings (personal contact between study nurses and patients aged 40–75 years in general practices, clients aged 40–65 years in job agencies; at random invitation by letter of a statutory health insurer in a health insured population aged 40–75 years). The settings are described more precisely below. Recruitment of study participants included three steps. A total of 1150 individuals participated in a health screening (step 1) and completed a computerized questionnaire on cardiovascular risk factors, followed by facultative blood pressure measurement and blood sample taking. Furthermore, participants with characteristics as listed below were eligible for a cardiovascular examination program (CEP; step 2): no history of cardiovascular events (myocardial infarction, stroke), vascular interventions, or diabetes mellitus as well as self-reported body mass index (BMI) ≤ 35 kg/m2, no previous Methicillin-resistant Staphylococcus aureus (MRSA) infection and resident in a pre-defined zip-code area.
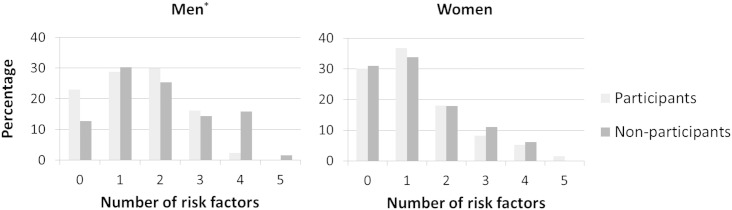
A total of 706 participants of the health screening were eligible for the CEP. Of these, 582 individuals (82.4%) participated in the CEP. It was conducted at the University hospital by trained study nurses and was supervised by study physicians. At the beginning of the CEP participants were informed about the modules of examination (e.g., blood pressure measurement, blood taking), data storage, and about the handling of potential medical findings. Accelerometry was offered as a further examination (step 3). Participants were provided with the information that physical activity would be recorded for 7 days by an acceleration sensor (ActiGraph, GT3X +), a small box on a belt that would have to be worn around the hip. Additionally, they were informed that a physical activity diary would have to be filled out during accelerometer wear time (capturing activity, time interval, and perceived effort). Finally, participants received the information that a written feedback about their physical activity would be provided. All individuals gave written informed consent for each examination separately. Detailed information concerning accelerometry, such as instructions for wearing the accelerometer, was given at the end of the CEP when participants received the device. Due to organizational reasons the accelerometer study was implemented with a temporal delay. Therefore, accelerometry was only offered to 470 participants (see Fig. 1). For each step of the study, participants could choose one of different gift vouchers for different shopping facilities worth €5 (step 1), €15 (step 2), and €15 (step 3). Participants in the accelerometer study had to return their accelerometer and the physical activity diary at the university hospital to receive their last gift voucher. This study was approved by the clinical ethical committee of the University Medicine Greifswald (protocol number BB64/07).
Fig. 1.
Flow of participation; CEP, cardiovascular examination program (Germany, 2012–2013).
*Ineligibility criteria: history of cardiovascular events (myocardial infarction, stroke), vascular interventions, diabetes mellitus, self-reported body mass index (BMI) > 35 kg/m2, previous Methicillin-resistant Staphylococcus aureus (MRSA) infection, no resident in a pre-defined zip-code area.
Settings of recruitment
Participants were recruited in three different settings: in general practices, in job agencies, and by a statutory health insurance. In Germany, job agencies are responsible for the implementation of basic security benefits for job seekers following the social security code. Regarding our statutory health insurance population, in Germany, employees up to a certain income limit (in 2013: 52.200 € gross annual income) are obliged to insure themselves in a statutory health insurance of their own choice. People who are not employed, e.g., self-employed persons, have the option to insure themselves in a statutory or in a private health insurance.
Measures
Socio-demographics and smoking
We collected information about sex, age, school education (common German types of school education; categorized as < 10 years, 10 years, > 10 years for international comparability), and current smoking (yes/no).
Self-reported general health
Self-reported general health was measured with the first item of the SF-36 Health Survey “In general, would you say your health is …” using a 5-point scale (excellent, very good, good, fair, poor) (McHorney et al., 1994).
Cardiorespiratory fitness
Cardiorespiratory fitness (CRF) was assessed on a cycle ergometer (Ergoselect 100; Ergoline, Bitz, Germany) via standardized cardiopulmonary exercise testing according to the Jones protocol (Jones et al., 1985). CRF was defined by peak oxygen uptake (O2peak). Detailed information about the assessment of CRF is published elsewhere (Koch et al., 2009). For main analyses, relative O2peak was used. Relative O2peak was calculated as absolute O2peak divided by body weight. For secondary analyses, O2peak expressed in percentages of the predicted values was used. Calculation of the predicted values was based on a SHIP equation from Gläser et al. (2013), which is based on a sample from our study region (northeast Germany).
Assessment of cardiometabolic risk factors
The following five parameters were considered for further analyses of cardiometabolic risk: elevated waist circumference, elevated resting blood pressure, elevated triglycerides, elevated blood glucose, and reduced high-density lipoprotein. These five factors constitute the metabolic syndrome (Grundy et al., 2005). Waist circumference was measured midway between the hipbone and the bottom of the ribs. Waist circumference was considered elevated if ≥ 102 cm for males or ≥ 88 cm for females (WHO, 2000). Systolic and diastolic blood pressure were measured after a five minute rest period three times at the right arm of seated participants using a digital blood pressure monitor (705IT, Omron Corporation, Tokyo, Japan), with each reading being followed by a further rest period of three minutes . The mean of the 2nd and 3rd measurements was used for the present analyses. Blood pressure was considered elevated if one or more of the three conditions were met: (1) systolic pressure ≥ 140 mm Hg, (2) diastolic pressure ≥ 90 mm Hg (Mancia et al., 2013), and (3) self-reported antihypertensive medication within the last 12 months. Blood samples were taken all-day in a non-fasting state. Glycated hemoglobin (HbA1c), high-density lipoprotein (HDL), and plasma triglycerides were determined by standard methodology at the clinical chemistry laboratories at the University Medicine Greifswald. HbA1c was used for analyses instead of blood glucose because samples were collected in the non-fasted state and glucose levels would be inaccurate. HbA1c was considered elevated at > 6.5% (WHO, 2011). HDL was considered reduced at < 50 mg/dL in women or < 40 mg/dL in men (Grundy et al., 2005). To account for non-fasted blood samples, triglycerides were considered elevated at ≥ 200 mg/dL (Wannamethee et al., 2005). We did not take into account if participants reported blood lipids lowering medication within the last 12 months because we did not ask participants for the exact kind of their medication. Therefore, we could not be certain whether the medication had an impact on HDL and/or triglycerides or not.
Data analysis
Analyses were performed using STATA 12.1 (StataCorp, 2011). We used multivariate logistic regression to generate odds ratios (OR) and 95% confidence intervals (CI) to estimate the association between non-participation in the accelerometer study and the following characteristics of participants: sex, age, education, current smoking, self-reported general health, CRF, number of cardiometabolic risk factors, and setting of recruitment. Subsequently, we stratified this analysis by sex. Finally, we used logistic regression to calculate OR of non-participation in the accelerometer study for each of the objectively measured cardiometabolic risk factors separately, stratified by sex. Models were adjusted for age, CRF, and setting of recruitment.
Results
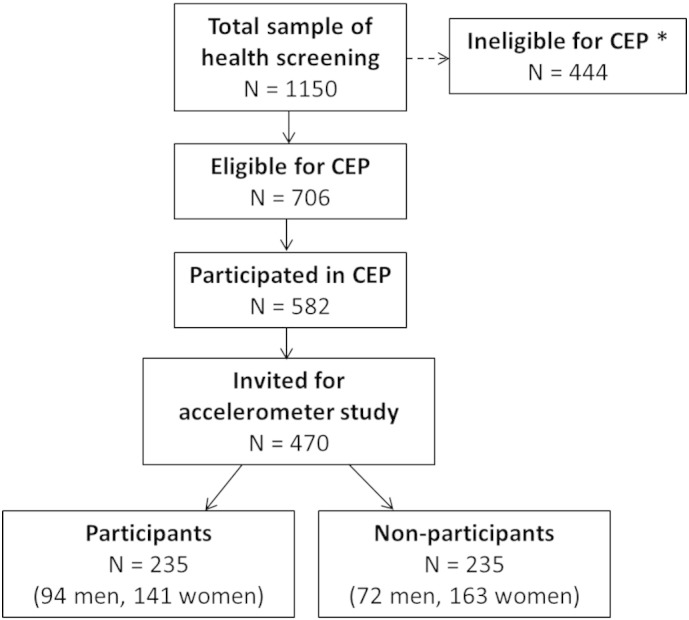
Among participants of the CEP who had been invited to take part in the accelerometer study [n = 470; 64.7% women; mean age 56.3 years (SD = 10.0)], 235 participants (50%; 60.0% women) agreed to wear an accelerometer for 7 days. Table 1 shows the characteristics of accelerometer study participants and non-participants stratified by sex. The distribution of the number of cardiometabolic risk factors is shown in Fig. 2.
Table 1.
Characteristics of study population stratified by sex and accelerometer study participation (Germany, 2012–2013).
| Women |
Men |
|||||
|---|---|---|---|---|---|---|
| Participants (n = 141) | Non-participants (n = 163) | p | Participants (n = 94) | Non-participants (n = 72) | p | |
| Sociodemographic variables | ||||||
| Age (years) | 56.26 (9.38) | 56.70 (10.33) | ns | 56.60 (9.79) | 54.81 (10.43) | ns |
| Education (years) | ns | ns | ||||
| ≤ 10 (%) | 11.35 | 14.37 | 19.35 | 13.89 | ||
| = 10 (%) | 51.77 | 50.00 | 47.31 | 55.56 | ||
| ≥ 10 (%) | 36.88 | 35.63 | 33.33 | 30.56 | ||
| No information (n = 4) | ||||||
| Current smoker (yes, %) | 22.70 | 22.09 | ns | 25.53 | 33.33 | ns |
| Self-reported health variable | ||||||
| Self-reported general health | 3.05 (0.66) | 3.09 (0.72) | ns | 2.95 (0.81) | 3.01 (0.62) | ns |
| Objective health variables | ||||||
| (mL∙kg− 1∙min− 1) | 24.12 (5.21) | 24.41 (6.07) | ns | 29.31 (6.53) | 28.71 (7.15) | ns |
| No information (n = 8) | ||||||
| Number of cardiometabolic risk factors | 1.26 (1.21) | 1.28 (1.19) | ns | 1.46 (1.09) | 1.95 (1.33) | .01 |
| No information (n = 42) | ||||||
| Single cardiometabolic risk factors | ||||||
| Elevated waist circumference (yes, %) | 46.10 | 36.02 | ns | 35.11 | 45.07 | ns |
| No information (n = 3) | ||||||
| Reduced high-density lipoprotein (yes, %) | 20.30 | 27.52 | ns | 30.68 | 34.38 | ns |
| No information (n = 36) | ||||||
| Elevated triglycerides (yes, %) | 15.79 | 17.45 | ns | 32.95 | 45.31 | ns |
| No information (n = 36) | ||||||
| Elevated blood pressure or meds (yes, %) | 41.13 | 44.38 | ns | 46.24 | 61.11 | ns |
| No information (n = 4) | ||||||
| Elevated HbA1c (yes, %) | 3.01 | 2.03 | ns | 2.30 | 6.15 | ns |
| No information (n = 37) | ||||||
| Blood lipids lowering meds (yes, %) | 9.22 | 7.36 | ns | 11.70 | 12.50 | ns |
| Blood pressure lowering meds (yes, %) | 34.04 | 35.58 | ns | 26.60 | 36.11 | ns |
| Setting of recruitment | ns | ns | ||||
| General practices (%) | 32.62 | 36.20 | 41.49 | 36.11 | ||
| Job agencies (%) | 17.02 | 16.56 | 21.28 | 29.17 | ||
| Health insurance (%) | 50.35 | 47.24 | 37.23 | 34.72 | ||
Abbreviations: , cardiorespiratory fitness measured as maximum oxygen uptake; HbA1c, glycated hemoglobin.
Data are presented as mean ± SD for continuous variables and as the number of subjects (%) for categorical variables; presented p-values are based on t-test for continuous variables and chi-square test for categorical variables.
Fig. 2.
Distribution of number of cardiometabolic risk factors by sex (Germany, 2012–2013).
*p < .05; the chi-square test was used to compare groups.
Multivariate logistic regression analysis with all predictor variables entered including a composite measure of cardiometabolic risk factors (number of cardiometabolic risk factors) revealed (Table 2) that women were more likely to decline participation (OR = 1.7, 95% CI = 1.06–2.74) compared to men. Setting of recruitment did not predict accelerometer study participation. Stratified analyses (Table 2) revealed the number of risk factors as predictor of non-participation for men (OR = 1.4, 95% CI = 1.01–1.95). Women did not differ on any entered variables.
Table 2.
Characteristics associated with non-participation in a 7-day accelerometer study (Germany, 2012–2013).
| Overall (n = 411) |
Women (n = 267) |
Men (n = 144) |
||||
|---|---|---|---|---|---|---|
| Odds ratioa | 95% CI | Odds ratioa | 95% CI | Odds ratioa | 95% CI | |
| Sex | ||||||
| Men | Ref. | |||||
| Women | 1.70 | (1.06–2.74)⁎ | ||||
| Age | 1.00 | (0.98–1.03) | 1.01 | (0.98–1.05) | 0.98 | (0.94–1.03) |
| Education | ||||||
| Less than 10 years | Ref. | Ref. | Ref. | |||
| 10 years | 0.95 | (0.50–1.80) | 0.81 | (0.35–1.85) | 1.07 | (0.37–3.12) |
| More than 10 years | 0.87 | (0.45–1.67) | 0.69 | (0.30–1.60) | 1.37 | (0.46–4.09) |
| Current smoker | ||||||
| Yes | Ref. | Ref. | Ref. | |||
| No | 0.96 | (0.58–1.60) | 0.98 | (0.52–1.85) | 1.09 | (0.44–2.70) |
| Self-reported general health | 1.08 | (0.81–1.44) | 1.11 | (0.76–1.62) | 1.17 | (0.73–1.86) |
| (mL∙kg− 1∙ min− 1) | 1.01 | (0.97–1.06) | 1.04 | (0.98–1.10) | 0.99 | (0.93–1.05) |
| Number of cardiometabolic risk factors | 1.11 | (0.92–1.33) | 1.01 | (0.81–1.26) | 1.40 | (1.01–1.95)⁎ |
| Setting of recruitment | ||||||
| General practices | Ref. | Ref. | Ref. | |||
| Job agencies | 1.13 | (0.64–1.99) | 0.90 | (0.43–1.88) | 1.65 | (0.64–4.30) |
| Health insurance | 0.98 | (0.62–1.57) | 0.92 | (0.52–1.63) | 1.04 | (0.43–2.53) |
Abbreviation: , cardiorespiratory fitness measured as maximum oxygen uptake.
Odds ratios were adjusted for all other variables shown in the table.
p < 0.05.
Considering the cardiometabolic risk factors separately, Table 3 shows results from logistic regression analyses adjusted for age, CRF, and setting of recruitment. Men with elevated blood pressure tended to decline participation more likely (OR = 1.9, 95% CI = 0.94–3.7) compared to men with normal blood pressure values, even though this result barely missed statistical significance (p = 0.07). Among women, those with elevated waist circumference were less likely to decline participation (OR = 0.6, 95% CI = 0.3–0.95) compared to women with values below the predefined cut-off of 88 cm.
Table 3.
Cardiometabolic risk factors associated with non-participation in a 7-day accelerometer study (Germany, 2012–2013).
| Women |
Men |
|
|---|---|---|
| Cardiometabolic risk factors | Odds ratioa (95% CI) |
Odds ratioa (95% CI) |
| Elevated waist circumference | ||
| No | Ref. | Ref. |
| Yes | 0.6 (0.3–.95)⁎ | 1.4 (0.7–3.0) |
| Elevated triglycerides | ||
| No | Ref. | Ref. |
| Yes | 1.2 (0.6–2.3) | 1.4 (0.7–2.9) |
| Reduced high-density lipoprotein | ||
| No | Ref. | Ref. |
| Yes | 1.5 (0.8–2.7) | 1.0 (0.5–2.1) |
| Elevated blood pressure or medication | ||
| No | Ref. | Ref. |
| Yes | 1.1 (0.6–1.8) | 1.9 (0.9–3.7) |
| Elevated HbA1c | ||
| No | Ref. | Ref. |
| Yes | 0.8 (0.2–4.0) | 3.1 (0.5–18.7) |
Abbreviation: HbA1c, glycated hemoglobin.
Odds ratios were adjusted for age, cardiorespiratory fitness, and setting of recruitment.
p < 0.05.
Secondary analyses in which O2peak expressed in percent of predicted values was used for all analyses yielded similar results.
Discussion
The three main findings of our study were that (1) more women declined participation in accelerometry than men, (2) men were more likely not to participate in the study if they had a higher number of cardiometabolic risk factors, and (3) waist circumference was negatively associated with non-participation for women.
Accelerometer study participants were more likely men. This finding supports results from Harris et al. (2008) for a sample of a comparable sample size of participants 65 years of age or older registered with a primary health care center and recruited by different recruitment strategies.
Men with higher cardiometabolic risk were more likely to decline participation. We assume that men of higher cardiovascular risk are already aware that they need to be more physically active to reduce their CVD risk (Pikala et al., 2011). Thus, these men might not see it as necessary or helpful to wear an accelerometer to get possibly known low levels of physical activity confirmed. Moreover, declining participation might also be information avoidance, behavior to prevent people from obtaining potentially unwanted information, such as non-participation in the accelerometer study to avoid unpleasant feelings based on expected negative feedback (Sweeny et al., 2010). In contrast, the CVD risk in women seemed to be lower compared to men (three or more risk factors: 16% in women vs. 24% men), which might explain why the number of risk factors does not predict non-participation in women.
Women declined participation more likely when their waist circumference was normal. A possible explanation for the association of elevated waist circumference and less rejection of study participation by women might be that women with normal waist circumference are more likely to be already physically active, and therefore do not see the necessity to get examined regarding their physical activity.
Further, our results revealed that CRF was not associated with non-participation in the accelerometer study. Prior research showed higher self-reported physical activity in accelerometer study participants compared to non-participants (Harris et al., 2008). However, we could not find differences in CRF as a proxy measure of physical activity.
Although we did not ask for reasons for non-participation, different barriers could be imagined. For example, people might see it impractical to wear an accelerometer because they have to remember to wear it for seven days, they have to take care of it (no showering, no swimming), it might be uncomfortable to wear it, etc. Furthermore, people might associate wearing of this device with unpleasant feelings because other people could see the accelerometer, it could get wet through with perspiration, it might influence sexual life, people may feel monitored or might not be interested in a potential negative feedback about their physical activity and avoid it by declining participation (information avoidance). Moreover, participating in the accelerometer study was a higher burden for participants because they had to bring the device back to the University hospital and were asked to complete a diary. Future research should address these questions to enhance participation in accelerometer studies. Findings about reasons, why people do not want to wear devices like accelerometers can give hints about necessary changes in, e.g., selections of kinds of devices, instructions or motivational strategies.
An important limitation of our study was the pre-selection occurring in earlier steps before our accelerometer study (see Fig. 1). We had no information on people who did not want to participate in the health screening and we had just limited information on people who were not interested to participate in the CEP. For example, prior analyses of subpopulations of our study population proved earlier occurring selection biases, e.g., non-smoking predicted participation in the CEP within the general practice patients sample as well as in the job agency client sample (Guertler et al., 2014). Moreover, we had a restricted sample according health because people of poorer health, such as individuals with prior CVD, self-reported BMI > 35 kg/m2, or diabetes, were not eligible for the CEP. Results cannot be generalized to a non-restricted sample.
Despite these limitations, our results have potential implications for future research using objective measures for physical activity like accelerometers because we found a selection bias according to sex and in men regarding their cardiometabolic risk factor profile. These aspects need to be considered in planning of future studies or in interpretation and generalization of future research results.
In conclusion, selection bias in accelerometer study participation was observed. Women were less likely to participate in accelerometry than men. Men were less likely to participate if they faced a higher cardiometabolic risk than if they had a lower risk. Especially the men at high risk would be the target group of primary interest in interventions aiming to reduce cardiovascular risks. Interventions addressing the enhancement of physical activity using accelerometers need to consider possible selection bias during recruitment and need to develop strategies to reduce this bias.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
Acknowledgments
This research was supported by the DZHK (German Centre for Cardiovascular Research; Grand No. 81/Z540100152). The authors wish to thank the statutory health insurance company, the 2 Job Agencies of Greifswald and the 11 participating general practices of Greifswald for supporting our recruitment of the participants.
References
- Aspenes S.T., Nilsen T.I.L., Skaug E.A. Peak oxygen uptake and cardiovascular risk factors in 4631 healthy women and men. Med. Sci. Sports Exerc. 2011;43:1465–1473. doi: 10.1249/MSS.0b013e31820ca81c. [DOI] [PubMed] [Google Scholar]
- Brown B.B., Werner C.M. Using accelerometer feedback to identify walking destinations, activity overestimates, and stealth exercise in obese and nonobese individuals. J. Phys. Act. Health. 2008;5:882–893. doi: 10.1123/jpah.5.6.882. [DOI] [PubMed] [Google Scholar]
- Davis M.G., Fox K.R. Physical activity patterns assessed by accelerometry in older people. Eur. J. Appl. Physiol. 2007;100:581–589. doi: 10.1007/s00421-006-0320-8. [DOI] [PubMed] [Google Scholar]
- Gläser S., Ittermann T., Schäper C. The Study of Health Pomerania (SHIP) reference values for cardiopulmonary exercise testing. Pneumologie. 2013;67:58–63. doi: 10.1055/s-0032-1325951. [DOI] [PubMed] [Google Scholar]
- Glasgow R.E., Vogt T.M., Boles S.M. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am. J. Public Health. 1999;89:1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundy S.M., Cleeman J.I., Daniels S.R. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- Guertler D., Braatz J., Weymar F. Estimating participation factors in a cardiovascular assessment program for general practice patients and job center clients. Eur. J. Prev. Cardiol. 2014;21:S135. [Google Scholar]
- Harris T.J., Victor C.R., Carey I.M., Adams R., Cook D.G. Less healthy, but more active: opposing selection biases when recruiting older people to a physical activity study through primary care. BMC Public Health. 2008;8:182. doi: 10.1186/1471-2458-8-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inoue S., Ohya Y., Odagiri Y. Characteristics of accelerometry respondents to a mail-based surveillance study. J. Epidemiol. 2010;20:446–452. doi: 10.2188/jea.JE20100062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones N.L., Makrides L., Hitchcock C., Chypchar T., McCartney N. Normal standards for an incremental progressive cycle ergometer test. Am. Rev. Respir. Dis. 1985;131:700–708. doi: 10.1164/arrd.1985.131.5.700. [DOI] [PubMed] [Google Scholar]
- Koch B., Schaper C., Ittermann T. Reference values for cardiopulmonary exercise testing in healthy volunteers: the SHIP study. Eur. Respir. J. 2009;33:389–397. doi: 10.1183/09031936.00074208. [DOI] [PubMed] [Google Scholar]
- Mancia G., Fagard R., Narkiewicz K. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur. Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- McHorney C.A., Ware J.E., Jr., Lu J.F., Sherbourne C.D. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med. Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- Pikala M., Kaleta D., Bielecki W., Maniecka-Bryla I., Drygas W., Kwasniewska M. Awareness of cardiovascular prevention methods among residents of post-communist Polish provinces with highest mortality rates. Cent. Eur. J. Public Health. 2011;19:183–189. doi: 10.21101/cejph.a3675. [DOI] [PubMed] [Google Scholar]
- Prince S.A., Adamo K.B., Hamel M.E., Hardt J., Connor Gorber S., Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int. J. Behav. Nutr. Phys. Act. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly J.J., Penpraze V., Hislop J., Davies G., Grant S., Paton J.Y. Objective measurement of physical activity and sedentary behaviour: review with new data. Arch. Dis. Child. 2008;93:614–619. doi: 10.1136/adc.2007.133272. [DOI] [PubMed] [Google Scholar]
- Roth M.A., Mindell J.S. Who provides accelerometry data? Correlates of adherence to wearing an accelerometry motion sensor: the 2008 Health Survey for England. J. Phys. Act. Health. 2013;10:70–78. doi: 10.1123/jpah.10.1.70. [DOI] [PubMed] [Google Scholar]
- StataCorp . StataCorp LP; College Station, TX: 2011. Stata Statistical Software: Release 12. [Google Scholar]
- Sweeny K., Melnyk D., Miller W., Shepperd J.A. Information avoidance: who, what, when, and why. Rev. Gen. Psychol. 2010;14:340–353. [Google Scholar]
- Troiano R.P., Berrigan D., Dodd K.W., Masse L.C., Tilert T., McDowell M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- Wannamethee S.G., Shaper A.G., Lennon L., Morris R.W. Metabolic syndrome vs Framingham Risk Score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch. Intern. Med. 2005;165:2644–2650. doi: 10.1001/archinte.165.22.2644. [DOI] [PubMed] [Google Scholar]
- WHO . WHO; Geneva, Switzerland: 2000. Obesity: preventing and managing the global epidemic: Report of a WHO Consultation. [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2011. Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: abbreviated report of a WHO consultation. (p. WHO/NMH/CHP/CPM/11.1) [PubMed] [Google Scholar]