Abstract
Introduction
Diet and activity counseling is recommended during all well child visits to promote optimal health and prevent childhood obesity. The objective of this study was to determine the effectiveness of a novel Wellness Action Plan aimed at: 1) improving parent recall of diet and activity plans made during routine well child visits 2) increasing adherence with plans, and 3) enhancing parents' identification of their child's weight category.
Methods
Parents of children 2.5 to 14 years (n = 181) seen at a pediatric primary care clinic in Milwaukee, Wisconsin between March and August of 2013 received standard diet and activity counseling from their physician (both control and intervention groups). In addition, parents randomized to the intervention group were asked to complete a Wellness Action Plan, where established diet and activity goals were documented. Parents completed surveys about BMI identification, plan creation, and plan adherence pre visit, post visit, and at 1 and 3 months.
Results
Intervention parents were significantly more likely to recall diet (p = 0.003) and activity (p = 0.03) plans at 3 months and were also more likely to report adherence with diet (p = 0.006) and activity (p = 0.08) plans at three months. There was no difference between groups in their ability to correctly identify children's weight categories (p > 0.05).
Conclusion
The Wellness Action Plan was associated with higher parent diet and activity plan recall and self-reported adherence. The Wellness Action Plan is a potentially important counseling tool that can be used to help parents make lifestyle modifications for their children.
Clinical Trial Registration
ClinicalTrials.gov, Identifier NCT02185248.
Keywords: Health promotion, Pediatrics, Primary health care, Obesity, Diet, Physical fitness, Primary prevention, Preventive medicine
Highlights
-
•
We trialed a written Wellness Action Plan in pediatric primary care.
-
•
Plan use resulted in improved recall and adherence with diet and activity changes.
-
•
Improved adherence occurred for normal weight, overweight, and obese children.
-
•
The Wellness Action Plan can be used to engage parents in obesity prevention.
Introduction
Parental beliefs about what constitutes a healthy lifestyle behavior are influenced by multiple factors and are not always evidence-based. Common misperceptions include the nutritional value of juice (Munsell et al., 2015) and the educational value of television (Zimmerman et al., 2007). Given the prevalence of unhealthy behaviors in early childhood (Centers for Disease Control & Prevention (CDC, 2014)) and the magnitude of the childhood obesity epidemic (Skinner and Skelton, 2014, Ogden et al., 2014), preventive counseling to correct misperceptions and provide timely and appropriate guidance is crucial (Davis et al., 2007, Daniels and Hassink, 2015). Pediatric primary care is an ideal setting for health promotion counseling, given the skills of primary care physicians and the fact that children present to their primary care physicians for appointments that specifically focus on growth and development (well child visits). The American Academy of Pediatrics (AAP) recommends that all children, regardless of their body mass index (BMI), receive diet and activity counseling during well child visits (Tanski et al., 2010). Counseling should engage both the parent and the child and focus on making specific, measurable, and achievable plans for behavior change. In addition, every child should have their BMI calculated, classified (underweight, normal weight, overweight, or obese), and communicated to parents (Tanski et al., 2010, Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, 2011). Despite these recommendations, studies have demonstrated that as many as 60% of patients report not receiving counseling (Kallem et al., 2013, Liang et al., 2012). One potential explanation is that patients do not recall counseling. Research has shown that as little as 20% of medical information communicated by providers is actually remembered (Kessels, 2003). Patients' initial understanding of plans made with their physician and their ability to recall plans are essential components for self-management and adherence (Ley, 1982).
One strategy that could be used to improve initial understanding and recall of health goals is written action plans. Written action plans have been associated with caregivers' understanding of the disease (Tan et al., 2013) and medication adherence (Ducharme et al., 2011) for children with asthma. To our knowledge, however, no studies have examined action plans and parental recall of diet and activity goals in pediatric primary care. Several studies have reported interventions using goal establishment to improve adherence with changes in diet and activity regimens (Perrin et al., 2010, Schwartz et al., 2007, McCallum et al., 2007, Patrick et al., 2001, Stovitz et al., 2014). However, goal creation in these studies was largely based on parents choosing goals from predefined lists of suggested behavior changes, rather than composing goals from scratch. Predefined goals go against the notion of free choice, which is pertinent to patient engagement (Lorig et al., 2014). Additionally, past studies have focused largely on goal creation for children who are overweight or obese but not children of normal weight. As primary prevention is an essential part of effective primary care, obesity prevention efforts in children with normal weight but unhealthy lifestyle behaviors are pertinent as well (Daniels & Hassink, 2015). Lastly, interventions in low-income, African-American children, a population disproportionately burden by obesity (Skinner and Skelton, 2014, Ogden et al., 2014), are lacking.
We designed a tool called the Wellness Action Plan to help improve the effectiveness of health promotion counseling at a predominantly low-income, African-American, pediatric clinic. The primary aims of our study were to determine if use of the Wellness Action Plan could (1) improve parent recall of diet and activity plans made during the well child visit, (2) increase adherence with plans, and (3) enhance parents' identification of their child's BMI category. We hypothesized that parents who made written action plans following physician counseling would be more likely to understand and recall that a specific plan for diet and/or activity was made during the appointment and more likely to adhere with the plan(s). Additionally, we hypothesized that parents who were shown their child's weight category on a color-coded growth chart (alternate side of the Wellness Action Plan) would be more likely to correctly identify their child's weight category following the visit compared to parents who were shown the routine black-and-white growth chart (Perrin et al., 2010).
Methods
Participants
Eligible subjects were consecutive parent/child pairs who presented for a well child visit between March and August of 2013 at a resident-teaching clinic serving primarily Medicaid-insured, African-American children in Milwaukee, Wisconsin. Eligibility required the child to be between the ages of 2.5 to 14 years of age and living with a custodial parent, and the family to be English-speaking (approximately 95% of the clinic population). BMI was not an inclusion/exclusion criterion; however those children who were being seen by a specialist for weight management were excluded.
Procedures
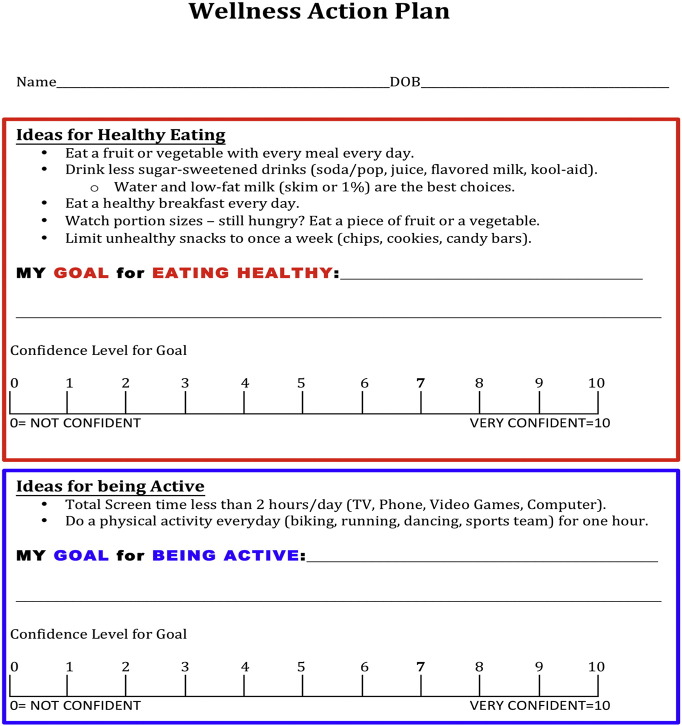
Three months prior to study commencement, and as part of a standard education series, all physician residents received a one-hour presentation regarding diet and activity counseling for parents and children during well child visits. Education included a review of the AAP recommendations for diet and activity (e.g. minimizing sugar sweetened beverages, getting one hour of physical activity daily) (Tanski et al., 2010), the importance of physicians actively engaging parents/children in counseling and plan creation, and a review of how to make diet and activity plans SMART (specific, measurable, achievable, relevant, timely). During this presentation, the Wellness Action Plan (Fig. 1) was introduced as a new tool that would be piloted with a random group of patients seen in clinic as part of a research protocol. Physicians were told that for these selected patients, a research assistant would provide them with the Wellness Action Plan at the time of the well child visit. The Wellness Action Plan is a two-sided worksheet. One side contains space for diet and activity plans to be recorded, and the alternate side contains the stoplight, color-coded, Centers for Disease Control and Prevention (CDC) BMI chart. Following routine counseling (including informing parents' of their child's BMI category), physicians were to help parents choose and record one diet and one activity goal on the Wellness Action Plan. In addition, parents would need to indicate their confidence in achieving each plan (scale 0–10). If confidence level was less than 7, physicians were told to help parents modify goals to increase the potential for success (Lorig et al., 2014). Physicians not present at the session received 1:1 education prior to study commencement from the study PI or the research assistant.
Fig. 1.
Wellness Action Plan tool desgined for randomized controlled trial in a primary care clinic in Milwaukee, WI from March to August of 2013.
The tool was created to help physicians with diet and activity health promotion counseling in pediatric primary care in order to promote optimal growth.
On the day of the study visit, parents and children were asked to provide written informed consent and assent (children age 7 and above if developmentally appropriate) for study participation. Subsequently, they were randomized to the control or intervention group. A research assistant referred to a computer-generated random number chart to determine group allocation for each enrollee. Parent/child pairs were blinded to group assignment.
Each child was weighed once by medical staff using an electronic medical-grade scale and measured once using a wall-mounted stadiometer (clinic protocol). BMI was calculated within the electronic medical record. Physicians were instructed to perform “routine” activity and diet counseling during the well child visit for parent/child pairs in the control group. Routine counseling included physicians showing parents the child's plotted BMI on a black-and-white, CDC BMI chart within the electronic medical record, making diet and activity recommendations based upon the child's current behaviors, and recording plans for lifestyle modification(s) in the patient's electronic chart. At the study clinic, a specific field where diet and activity plans can be recorded is present within all well child notes; however, completion of the field is not mandatory in order for the note to be considered complete. If a child was randomized to the intervention group, physicians were instructed to provide the same diet and activity counseling, in addition to having parents create a Wellness Action Plan. Providers were instructed to use the stoplight, color-coded, CDC BMI chart with the child's BMI plotted on it when informing parent's of their child's BMI category. On the chart, orange shading represents underweight, green represents normal weight, yellow represents overweight, and red represents obese (legend with terms included). Parent/child pairs were given a copy of the Wellness Action Plan to take home with them at the end of the visit, and a second copy was retained for the medical record. Similar to the control group, diet and activity plans were also recorded within the patient note in the electronic medical record.
Parent participants completed self-report questionnaires prior to seeing the physician (Parent Survey 1) and immediately following their appointment (Parent Survey 2). At one and three months post visit, the research assistant administered a follow up survey (Parent Survey 3) over the phone to parents in both groups. Phone contact was attempted up to seven times before the parent was deemed a non-respondent. Intervention parents were allowed to use the Wellness Action Plan worksheet to cue their memory to answer questions if it was accessible. All Parent Surveys were created for this study by the authors and were written at a second grade reading level.
A chart review was also performed within the electronic medical record to collect each child's date of birth, sex, race, and insurance provider. The encounter notes for both intervention and control children were also reviewed to determine whether a diet or activity plan was documented by the physician and what the plan was. All study data were stored and managed using the REDCap electronic database (Harris et al., 2009). The study was approved by the Institutional Review Board at the Children's Hospital of Wisconsin.
Measures
Parent Survey 1 asked parents to identify their child's BMI category (underweight, normal weight, overweight, obese). Parent Survey 2 asked parents whether plans were made for diet and/or activity changes during their visit that day (yes/no), what the plans were (open-ended), whether or not they intended to adhere with the plans (yes/no), whether the physician conveyed their child's BMI category (yes/no), and what their child's BMI category was (underweight, normal weight, overweight, obese). Parent Survey 3 was identical to Parent Survey 2 with the addition of two questions related to actual adherence with diet and activity plans: whether parents tried to adhere with plans (yes/no) and if so, how successful they were (11-point Likert scale: 0 = not successful, 10 = very successful).
Analysis
An intention-to-treat analysis was conducted for the post visit outcomes. All randomized subjects in the groups to which they were allocated were included in the analysis. For the 1 and 3 month follow-up outcomes, a complete case analysis was performed.
Demographic variables were summarized, using means and standard deviations or ranges for continuous measures and percentages for categorical variables. Differences between the control and intervention groups were evaluated using the two-sample t-test for age and BMI percentile and the chi-square test (or Fisher's exact test for expected cell counts less than 5) for sex, race, insurance type, and BMI category. The proportion of parents recalling and reporting adherence with diet plans and activity plans and the proportion correctly classifying their child's BMI were compared between intervention and control groups using the chi-square test (or Fisher's exact test when appropriate). To determine if differences in adherence may have been related to recall, a post-hoc chi-squared analysis was performed to compare reported adherence rates between intervention and control groups only for those parents that recalled a plan was made. Post-hoc analyses with the Wilcoxon–Mann–Whitney test was also performed to determine if self-reported success levels differed between the intervention and control groups for parents who reported following through with diet and activity changes at one and three months.
All tests were two-tailed, and p < 0.05 was considered statistically significant. The target sample size of 180 provided 80% power to detect a 20% difference between the intervention and control groups in the percent of parents able to correctly recall that a plan was made immediately following the visit. All data analysis was done using SAS Version 9.4 (SAS Institute, Cary, North Carolina).
Results
Participant characteristics
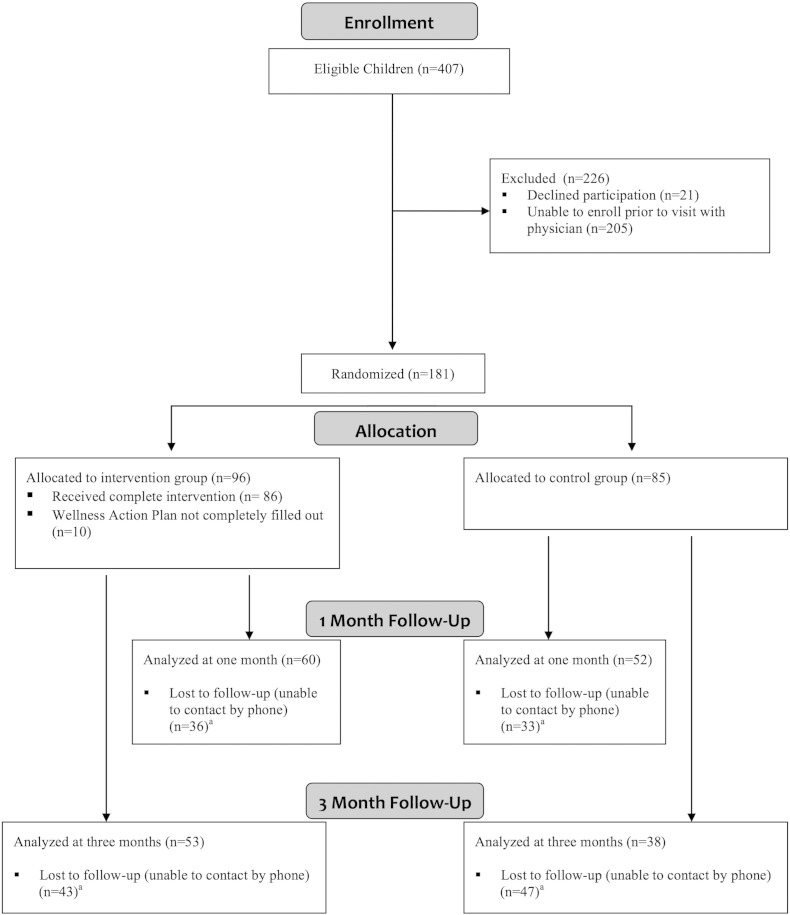
One hundred and eighty-one parent/child pairs were enrolled in the study (Fig. 2) (Moher et al., 2001). The demographic make-up of study participants was similar to the 2013 profile of clinic patients as a whole. There were no significant differences between the control and intervention groups at baseline with regards to age, gender, race, insurance type, or percent of children who were overweight/obese (Table 1).
Fig. 2.
CONSORT flow diagram (Harris et al., 2009) for Wellness Action Plan randomized controlled trial in a primary care clinic in Milwaukee, WI from March to August of 2013.
aThe demographic profile (age, gender, race, insurance type, and baseline BMI) of children who were lost to follow-up was not significantly different than the profile of those who had continued participation.
Table 1.
Demographic characteristics of child sample for Wellness Action Plan RCT in a primary care clinic in Milwaukee, WI from March-August of 2013.
| Characteristic | All participants | Control group | Intervention group | P valuea |
|---|---|---|---|---|
| N (%) | 181 | 85 (47%) | 96 (53%) | |
| Age in years, mean (range) | 7.1 (2.5 – 14.99) | 7.3 (2.5 –14.24) | 6.9 (2.6 –14.99) | 0.45 |
| Sex | 0.46 | |||
| Female | 45% | 48% | 43% | |
| Male | 55% | 52% | 57% | |
| Race | 0.12 | |||
| African American | 85% | 89% | 81% | |
| Otherb | 15% | 11% | 19% | |
| Medicaid | 94% | 96% | 92% | 0.18 |
| BMI Percentile, mean (SD) | 63% (28) | 66% (27) | 61% (29) | 0.26 |
| BMI Category | 0.84 | |||
| Underweight | 2% | 2% | 1% | |
| Normal | 70% | 67% | 72% | |
| Overweight | 14% | 15% | 12% | |
| Obese | 15% | 15% | 15% |
RCT = randomized controlled trial; BMI = body mass index.
Differences between the control and intervention groups were evaluated using the two-sample t-test for age and BMI percentile and the chi-square test (or Fisher's exact test for expected cell counts of less than 5) for sex, race, Medicaid insurance type, and BMI categories.
The “Other” group included the following race categories: American Indian or Alaskan Native, Asian, Native Hawaiian or other Pacific Islander, Other, or Unknown.
Ninety-six parent/child pairs (53%) were randomized to the control group, of which 79 made both a diet and an activity plan (4 diet only, 3 activity only, 10 action plans not completed). Plan specifics varied among participants; however, overall themes were similar. Decreasing sugar-sweetened beverage intake was the most common theme for diet plans, while doing a moderate to vigorous exercise (e.g. biking, dancing) was a common activity theme (Table 2).
Table 2.
Major themes of diet and activity plans made in Wellness Action Plan RCT in a primary care clinic in Milwaukee, WI from March–August of 2013.
| Diet |
Activity |
||
|---|---|---|---|
| Theme | Frequencya | Theme | Frequencya |
| Decrease sugar sweetened beverages | 35% | Increase activity | 58% |
| Increase fruit and vegetable consumption | 30% | • Walking/running (17%) | |
| Decrease unhealthy snacking (e.g. chips) | 24% | • Football/basketball (14%) | |
| Change to lower fat milk (1% or skim) | 4% | • Biking (14%) | |
| Regular meal patterns | 3% | • Dance/gymnastics (5%) | |
| Decrease frequency of fast food | 2% | • Gym equipment (5%) | |
| Decrease portion sizes | 1% | • Swimming (3%) | |
| Decrease screen time | 42% | ||
Percent of diet or activity plans that were classified under the corresponding theme (mutually exclusive).
Plan recall and self-reported adherence
The chart review revealed that every physician documented a plan for a change in diet and/or activity for all 181 participants in the study, as a part of routine clinical counseling that is performed at the clinic. Directly following the visit, intervention parents were significantly more likely to report that a plan was made during the visit compared to control parents for both diet (p < 0.001) and activity (p < 0.001) (Table 3). At one month post visit, intervention parents remained more likely to recall the plan that was made for both diet and activity and were more likely to report adherence with plans (all p values < 0.001) (Table 3). At three months post visit, plan recall remained higher for intervention parents for both diet (p = 0.003) and activity (p = 0.03) compared to control parents as was adherence with diet plans (p = 0.006). While activity plan adherence was also higher in the intervention versus the control group at three months (30% vs. 13%), the difference did not achieve statistical significance (p = 0.08). When comparing only those parents who were actually able to recall a plan, there was no statistical difference in self-reported adherence rates between the intervention and control groups (Table 3). Similarly, self-reported success scores were not statistically different at one or three months for either diet or activity when comparing the control and intervention groups (Table 3).
Table 3.
Parent plan recall,a adherence,b and success ratingsc for Wellness Action Plan RCT in a primary care clinic in Milwaukee, WI from March–August of 2013.
| Control group | Intervention group | P valued | |
|---|---|---|---|
| Post visit | N = 85 | N = 96 | |
| Made diet plan | 25% | 80% | < 0.001 |
| Made activity plan | 20% | 62% | < 0.001 |
| 1 month follow-up | N = 52 | N = 60 | |
| Recall diet plan | 25% | 78% | < 0.001 |
| Adherence diet plan (All) | 21% | 70% | < 0.001 |
| Adherence diet plan (Only recall group) | 85% (N = 13) | 89% (N = 47) | 0.6 |
| Success rating diet plan (mean, SD) | 7.9 (0.9) | 8.4 (1.8) | 0.2 |
| Recall activity plan | 15% | 57% | < 0.001 |
| Adherence activity plan (All) | 13% | 52% | < 0.001 |
| Adherence activity plan (Only recall group) | 87% (N = 8) | 91% (N = 34) | 1.00 |
| Success rating activity plan (mean, SD) | 8.0 (1.6) | 8.5 (1.7) | 0.4 |
| 3 month follow-up | N = 38 | N = 53 | |
| Recall diet plan | 29% | 62% | 0.003 |
| Adherence diet plan (All) | 29% | 58% | 0.006 |
| Adherence diet plan (Only recall group) | 100% (N = 11) | 94% (N = 33) | 1.00 |
| Success rating diet plan (mean, SD) | 8.2 (1.5) | 8.3 (1.6) | 0.7 |
| Recall activity plan | 13% | 34% | 0.03 |
| Adherence activity plan (All) | 13% | 30% | 0.08 |
| Adherence activity plan (Only recall group) | 100% (N = 5) | 89% (N = 18) | 1.00 |
| Success rating activity plan (mean, SD) | 7.8 (2.5) | 9.0 (1.3) | 0.3 |
RCT = randomized controlled trial.
Parents were included in the recall group if they said that they made a plan and could report the plan they made.
Adherence was calculated for all parent/child pairs who were contacted for follow-up regardless of whether they recalled a plan was made (“All”) and separately for only those parent/child pairs who actually recalled a plan (“Only recall group”). Separate sample sizes are included for “Only recall group” in parentheses under percent adherence.
Parents who reported adhering with plans were asked to rate how successful they were on a 0–10 Likert scale, with 0 representing not successful and 10 representing very successful.
Differences between the control and intervention groups were evaluated using the chi-square test (or Fisher's exact test when the expected counts were less than 5), with the exception of differences in success ratings which were analyzed with the Wilcoxon–Mann–Whitney test.
Parental BMI category recognition
Before the intervention, 66% of the intervention parents and 65% of the control parents correctly identified their child's BMI category (p = 0.90). Subgroup analyses are presented in Table 4. While intervention parents were more likely to correctly identify their child's BMI category compared to control parents at all time points (post visit, one month, and three months), the differences were small in magnitude and did not achieve statistical significance (Table 4).
Table 4.
Correct child body mass index category identification by parents in Wellness Action Plan RCT in a primary care clinic in Milwaukee, WI from March-August of 2013.
| Control group | Intervention group | P valueb | |
|---|---|---|---|
| Baseline category identification | |||
| All groups | 65% (55/85) | 66% (63/96) | 0.90 |
| Normal | 90% (53/59) | 86% (60/70) | 0.48 |
| Overweight & obese | 8% (2/26) | 12% (3/26) | 1.00 |
| Post visit category identification | |||
| Parents told categorya | 74% (63/85) | 92% (88/96) | 0.002 |
| All groups | 70% (44/63) | 77% (68/88) | 0.30 |
| Normal | 91% (40/44) | 94% (59/63) | 0.71 |
| Overweight & obese | 21% (4/19) | 36% (9/25) | 0.33 |
| 1 month category identification | |||
| Parents told categorya | 85% (44/52) | 88% (53/60) | 0.56 |
| All groups | 64% (28/44) | 75% (40/53) | 0.20 |
| Normal | 92% (24/26) | 97% (36/37) | 0.56 |
| Overweight & obese | 22% (4/18) | 25% (4/16) | 1.00 |
| 3 month category identification | |||
| Parents told categorya | 84% (32/38) | 91% (48/53) | 0.52 |
| All groups | 66% (21/32) | 69% (33/48) | 0.77 |
| Normal | 84% (16/19) | 94% (31/33) | 0.34 |
| Overweight & obese | 38% (5/13) | 13% (2/15) | 0.20 |
RCT = randomized controlled trial.
Percent of parents indicating that the physician told them their child's BMI category during the visit.
Differences between the control and intervention groups were evaluated using the chi-square test (or Fisher's exact test when the expected counts were less than 5).
Discussion
The Wellness Action Plan was effective in enhancing parents' initial understanding of diet and activity goals, as parents in the intervention group were more likely to report that diet and activity plans were made directly following the appointment compared to control parents. This was in spite of a plan being documented in the chart for every participant in both arms of the study. Use of the Wellness Action Plan was also associated with higher recall and parent-reported adherence with diet and activity goals at 1 and 3 months post visit. When comparing only those parents who were able to recall a plan in the control and intervention groups, there was no statistical difference in reported adherence rates, suggesting that the effect of the intervention was to increase plan recall. If parents could recall the plan, they were likely to report adherence, regardless of whether they were in the intervention or control group. These findings support Ley's theory that recall is an essential precursor to adherence to behavioral changes (Ley, 1982).
Several prior studies have shown behavioral improvements related to diet and activity interventions. Perrin et al. (2010) and Patrick et al. (2001) both used tools for behavior assessment and goal creation. Because neither study had a control group, it remains unclear whether outcomes were a result of the tool used or secondary to another facet of counseling. In our study, a control group was present, the group of physicians was the same in both arms, and the counseling provided (e.g. decrease sugar sweetened beverage consumption, get 60 min of activity per day) to both groups was similar, isolating the Wellness Action Plan tool as the variable of interest. McCallum et al. (2007) randomized participants to an intervention involving lifestyle contracts; however, the study population included overweight and obese children only, limiting the understanding of its potential relevance to normal weight populations.
Foregoing plan creation in normal weight children can lead to a missed opportunity to provide education about healthy behaviors that prevent obesity. To our knowledge, this is the first randomized controlled trial of a written action plan for diet and activity health promotion in pediatric primary care, and supports that brief, written action plans can lead to short-term, parent-reported behavior improvements in diet and activity for all children, regardless of BMI category.
Counter to past studies, use of the color-coded, BMI chart in the intervention group did not significantly improve parents' identification of their child's BMI category compared to use of a black-and-white growth chart (routine practice) (Perrin et al., 2010, Oettinger et al., 2009). We speculate that the lack of improvement could be secondary to the social and cultural contexts around weight classification. Our sample was predominantly African-American, low-income children. Oettinger et al. (2009) showed that African Americans are satisfied with their body image until their BMIs are well into the overweight range (BMI ≥ 25), compared to their Caucasian counterparts, who become concerned prior to becoming overweight (BMI < 25) (Fitzgibbon et al., 2000). Alternate perceptions of what qualifies as overweight and obese are also present in low-income populations (Baughcum et al., 1998, Jain et al., 2001).
The fact that parent-reported behavior change occurred for children who were in the normal weight category is a potentially important finding for future obesity prevention efforts. The health belief model suggests that perceived susceptibility and severity of a disease will dictate behavior change (Janz & Becker, 1984). In accordance, many have suggested that parental perception of their child being overweight or obese is a necessary prerequisite to diet and activity behavior changes (Lundahl et al., 2014). Our study suggests that parents of normal weight children can also be activated to make changes, implying that alternate motivations for engaging in healthy behaviors exist.
Use of the Wellness Action Plan also proved to be feasible for providing lifestyle counseling in a primary care clinic. This finding is supported by the high intervention completion rate (90%) and the minimal time necessary to complete the plan. While we did not systematically measure how long it took to create each Wellness Action Plan compared to routine care, physicians anecdotally reported action plan creation extended the visit between 1 and 5 minutes. This variability was attributed to the baseline emphasis placed on diet and activity counseling by individual physicians.
There are several study limitations that should be mentioned. Both the control and intervention groups were intended to receive diet and activity counseling. Confirmation that counseling was provided to intervention group participants was verified by the presence of a completed Wellness Action Plan. In order to determine whether control participants received counseling, physician encounter notes were reviewed. Reliance on physician notes as a fidelity check, however, is not ideal, as physician self-report leaves room for recall and/or report bias. Similarly, the outcome data were self-reported, thus potentially introducing social desirability and/or recall bias. Attrition rates were high, leading to small follow-up sample sizes. While this did not affect the power to detect differences related to recall, insufficient power remained at three months to detect a statistically significant difference in activity plan adherence. Another limitation is the homogeneity of the study population with regard to race and socioeconomic status. Also, the follow-up period was short, limiting the ability to monitor trends in BMI. Lastly, although BMI is a simple, commonly used measure and recommended for all children by the American Academy of Pediatrics to assess weight status (Tanski et al., 2010), BMI may not capture true fat mass. Future studies should consider videotaping physician encounters as a fidelity check, utilizing non self-reported adherence measures (e.g. use of electronic activity monitors), taking steps to minimize attrition (e.g. collecting detailed contact information and providing participation incentives), following children long-term to determine if parent-reported behavior changes are lasting and whether they translate to positive weight trends, and using bioelectric impedance analysis to discriminate between lean mass and fat mass. Additionally, the Wellness Action Plan should be trialed with other demographic groups to test its broader applicability.
To our knowledge, this is the first randomized controlled trial of a brief, written action plan targeting healthy eating and activity in pediatric primary care. Use of the action plan by parents resulted in improved recall and self-reported adherence with diet and activity changes for children. Adherence with behavior changes occurred for normal weight children as well as for overweight and obese children, highlighting that families can be motivated to improve diet and activity for children in all weight categories. Our brief, practical Wellness Action Plan is a potentially important tool that can be used to engage parents in health promotion and obesity prevention efforts.
Conflicts of interest statement
Dr. Kharofa reports receiving funding through two training grants from the National Institutes of Health during the conduct of this study (Medical College of Wisconsin T32-HP10030; Cincinnati Children's Hospital Medical Center T32-HP10027). The remaining authors declare that there are no conflicts of interest.
Acknowledgments
The authors would like to acknowledge Nick Organ for his significant role in data collection.
Contributor Information
Roohi Y. Kharofa, Email: Roohi.Kharofa@cchmc.org.
Kristen A. Copeland, Email: Kristen.Copeland@cchmc.org.
Heidi Sucharew, Email: Heidi.Sucharew@cchmc.org.
John R. Meurer, Email: Jmeurer@mcw.edu.
References
- Baughcum A., Burklow K., Deeks C., Powers S., Whitaker R. Maternal feeding practices and childhood obesity: a focus group study of low-income mothers. Arch. Pediatr. Adolesc. Med. 1998;152(10):1010–1014. doi: 10.1001/archpedi.152.10.1010. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) 2014. 1995–2013 Middle School Youth Risk Behavior Survey Data.http://nccd.cdc.gov/youthonline/ Available at: (Accessed on: September 18, 2015) [Google Scholar]
- Daniels S.R., Hassink S.G. The role of the pediatrician in primary prevention of obesity. Pediatrics. 2015;136(1):275–292. doi: 10.1542/peds.2015-1558. [DOI] [PubMed] [Google Scholar]
- Davis M.M., Gance-Cleveland B., Hassink S., Johnson R., Paradis G., Resnicow K. Recommendations for prevention of childhood obesity. Pediatrics. 2007;120(4):229–253. doi: 10.1542/peds.2007-2329E. [DOI] [PubMed] [Google Scholar]
- Ducharme F.M., Rl Zemek, Chalut D. Written action plan in pediatric emergency room improves asthma prescribing, adherence, and control. Am. J. Respir. Crit. Care Med. 2011;183(2):195–203. doi: 10.1164/rccm.201001-0115OC. [DOI] [PubMed] [Google Scholar]
- Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(5):213–256. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgibbon M.L., Blackman L.R., Avellone M.E. The relationship between body image discrepancy and body mass index across ethnic groups. Obes. Res. 2000;8(8):582–589. doi: 10.1038/oby.2000.75. [DOI] [PubMed] [Google Scholar]
- Harris P., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain A., Sherman S., Chamberlin L., Carter Y., Powers S., Whitaker R. Why don't low-income mothers worry about their preschoolers being overweight? Pediatrics. 2001;107(5):1138–1146. doi: 10.1542/peds.107.5.1138. [DOI] [PubMed] [Google Scholar]
- Janz N., Becker M. Health belief model: a decade later. Health Educ. Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Kallem S., Carroll-Scott A., Gildtad-Hayden K. Children's report of lifestyle counseling differs by BMI status. Child. Obes. 2013;9(3):216–222. doi: 10.1089/chi.2012.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessels R.P. Patients' memory for medical information. J. R. Soc. Med. 2003;96(10):520. doi: 10.1258/jrsm.96.10.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ley P. Satisfaction, compliance and communication. Br. J. Clin. Psychol. 1982;21(4):241–254. doi: 10.1111/j.2044-8260.1982.tb00562.x. [DOI] [PubMed] [Google Scholar]
- Liang L., Meyerhoefer C., Wang J. Obesity counseling by pediatric health professionals: an assessment using nationally representative data. Pediatrics. 2012;130(1):67–77. doi: 10.1542/peds.2011-0596. [DOI] [PubMed] [Google Scholar]
- Lorig K., Laurent D., Plant K., Krishnan E., Ritter P. The components of action planning and their associations with behavior and health outcomes. Chronic Illn. 2014;10(1):50–59. doi: 10.1177/1742395313495572. [DOI] [PubMed] [Google Scholar]
- Lundahl A., Kidwell K., Nelson T. Parental underestimates of child weight: a meta-analysis. Pediatrics. 2014;133(3):689–703. doi: 10.1542/peds.2013-2690. [DOI] [PubMed] [Google Scholar]
- McCallum Z., Wake M., Gerner B. Outcome data from the LEAP (Live, Eat and Play) trial: a randomized controlled trial of a primary care intervention for childhood overweight/mild obesity. Int. J. Obes. 2007;31:630–636. doi: 10.1038/sj.ijo.0803509. [DOI] [PubMed] [Google Scholar]
- Moher D., Schulz K., Altman D. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001;285(15):1987–1991. doi: 10.1001/jama.285.15.1987. [DOI] [PubMed] [Google Scholar]
- Munsell C.R., Harris J.L., Sarda V., Schwartz M.B. Parents' beliefs about the healthfulness of sugary drink options: opportunities to address misperceptions. Public Health Nutr. 2015;11:1–9. doi: 10.1017/S1368980015000397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oettinger M., Finkle J., Esserman D. Color-coding improves parental understanding of body mass index charting. Acad. Pediatr. 2009;5:330–338. doi: 10.1016/j.acap.2009.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden C., Carroll M., Kit B., Flegal K. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick K., Sallis J., Prochaska J. A multicomponent program for nutrition and physical activity change in primary care: PACE + for adolescen`ts. Arch. Pediatr. Adolesc. Med. 2001;155:940–946. doi: 10.1001/archpedi.155.8.940. [DOI] [PubMed] [Google Scholar]
- Perrin E., Jacobson Vann J., Benjamin J., Skinner A., Wegner S., Ammerman A. Use of a pediatrician toolkit to address parental perception of children's weight status, nutrition, and activity behaviors. Acad. Pediatr. 2010;10(4):274–281. doi: 10.1016/j.acap.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz R., Hamre R., Dietz W. Office-based motivational interviewing to prevent childhood obesity: a feasibility study. Arch. Pediatr. Adolesc. Med. 2007;161:495–501. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- Skinner A., Skelton J. Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012. JAMA Pediatr. 2014;168(6):561–566. doi: 10.1001/jamapediatrics.2014.21. [DOI] [PubMed] [Google Scholar]
- Stovitz S.D., Berge J.M., Wetzsteon R.J., Sherwood N.E., Hannan P.J., Himes J.H. Stage 1 treatment of pediatric overweight and obesity: a pilot and feasibility randomized controlled trial. Child. Obes. 2014;10(1):50–57. doi: 10.1089/chi.2013.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan N.C., Chen Z., Soo W.F., Ngoh A.S., Tai B.C. Effects of a written asthma action plan on caregivers' management of children with asthma: a cross-sectional questionnaire survey. Prim. Care Respir. J. 2013;22(2):188–194. doi: 10.4104/pcrj.2013.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanski S., Garfunkel L.C., Duncan P.M. Performing Preventive Services: A Bright Futures Handbook. American Academy of Pediatrics; Elk Grove Village, Illinois: 2010. [Google Scholar]
- Zimmerman F.J., Christakis D.A., Meltzoff A.N. Television and DVD/video viewing in children younger than 2 years. JAMA Pediatr. 2007;161(5):473–479. doi: 10.1001/archpedi.161.5.473. [DOI] [PubMed] [Google Scholar]