Abstract
Introduction
Exercise is Medicine™ (EIM) is an approach to clinic-based physical activity (PA) promotion. Study aims were to 1) assess the acceptability of current EIM protocols among healthcare providers (providers) and health and fitness professionals (fitness professionals); and 2) pilot test the resultant modified EIM protocols comparing patients referred to community PA programming with patients exposed to the EIM protocols alone.
Methods
During 2012–2013 in Chattanooga, Tennessee, USA, 30/80 invited providers and 15/25 invited fitness professionals received training and provided feedback in the use of the EIM protocols. Following EIM use, feedback from providers and fitness professionals about acceptability of EIM protocols resulted in the adaptation of EIM protocols into the electronic health record. Subsequently, 50 providers and 8 fitness professionals participated in the intervention phase of the pilot study. Healthy and/or disease managed adults 18 years and older were enrolled with a sample of patients exposed to both the EIM protocols and community PA programming (EIM +) while another sample was exposed to the EIM protocols only (EIM). All patients were assessed for physical activity and Health-related Quality of Life. Measures were repeated ~ 3 months later for each patient.
Results
Eighteen EIM + and 18 EIM participants were studied. The EIM + participants had a greater net increase in total PA (∆ = + 250 min/week) vs. EIM participants (∆ = − 38.6 min/week) (p = 0.0002).
Conclusions
EIM + participation significantly increased PA levels among participants, suggesting this approach significantly impacts the PA of inactive adults more than just EIM only.
Keywords: Physical activity, Community health, Prevention, Healthcare, Health promotion, Exercise
Highlights
-
•
Providers found EIM protocols acceptable and recommended it to be part of the EMR.
-
•
Fitness professionals found EIM acceptable but it needed to improve contact with providers.
-
•
EIM + patients had a greater net increase in total physical activity vs. EIM patients.
-
•
EIM + patients reported fewer disability days compared with EIM patients.
-
•
EIM + patients had fewer bad physical health days compared with EIM patients.
Introduction
Regular physical activity (PA) is associated with enhanced health and reduced risk for all-cause mortality (Hahn et al., 1990, McGinnis and Foege, 1993, Pate et al., 1995, Powell et al., 1987). Beyond the effects on mortality, PA has many health benefits, including reducing the risk of cardiovascular disease (CVD), diabetes, obesity, musculoskeletal conditions, and selected key cancers (Lee et al., 2012, McGinnis, 1992). Even with all the benefits of regular PA, only 47% of adults in the United States report engaging in a sufficient dose of moderate-intensity PA (150 min per week) to accrue any of the above health benefits (Haskell et al., 2007). Most alarming is that 25% report no leisure-time regular PA (Haskell et al., 2007). In addition, there are significant reported disparities in PA patterns, with African-American and Latino men and women less likely to engage in health promoting amounts of PA compared to Caucasian men and women (Ham et al., 2007, Whitt-Glover et al., 2007). These patterns of physical inactivity have also been reported worldwide (Hallal et al., 2012, Kohl et al., 2012). In Healthy People 2020, PA is ranked as one of the leading health indicators. Goals have been developed to improve levels of PA among adults, adolescents, and children, and to reduce sedentary behavior among adolescents (U.S. Department of Health and Human Services, 2014).
Recent reports have identified evidence-based PA behavior change interventions that can be successfully implemented in a clinical setting (Calfas et al., 1996, Heath et al., 2012, Kahn et al., 2002a, Kahn et al., 2002b, Kahn et al., 2005, Long et al., 1996). In addition, evidence-based community programming designed to increase PA has also been recommended (Heath et al., 2006, Task Force on Community Preventive Services, 2001). Based on these findings, Exercise is Medicine™ (EIM), a systematic and comprehensive clinic-based approach to PA assessment and promotion, was developed initially for primary care physicians and other primary healthcare providers (Lobelo et al., 2014). Primary Aims: The primary aims of this pilot study were to conduct: 1) an acceptability phase, to evaluate the acceptability and provide improved modifications of the current EIM healthcare provider and health & fitness professional Action Guides (protocols); and 2) an intervention phase, to pilot test the resultant modified EIM protocols comparing patients referred to community PA programming (EIM +) with patients exposed to the clinic-based EIM protocols alone (EIM only). It was hypothesized that patients exposed to the EIM + would have a greater increase in PA levels compared with patients exposed to EIM without participation in community-based PA programming.
Methods
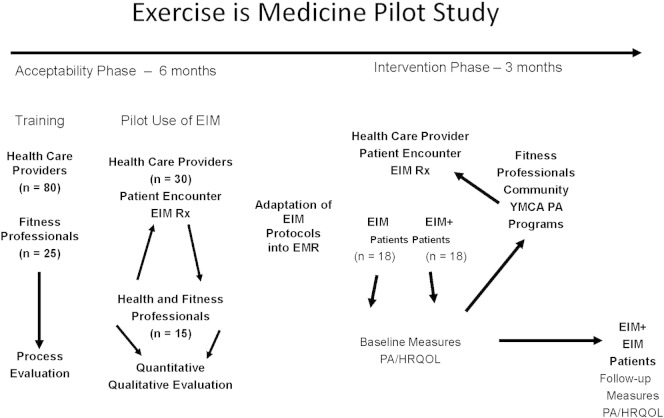
Acceptability phase: study population
In the spring of 2013, five primary care clinics and four health and fitness centers located within the greater metropolitan area of Chattanooga, Tennessee, USA were selected to be enrolled in the study. Through email and in-service solicitations, a total of 80 healthcare providers (providers) were initially recruited for orientation and training in the use of the EIM Healthcare Provider Action Guide (i.e., protocols); 25 health and fitness professionals (fitness professionals) were recruited for the initial orientation and training in the use of the EIM Health and Fitness Professional Action Guide (i.e., protocols). These fitness professionals represented a variety of local facilities and programs. Informed consent to participate in the acceptability phase of this pilot study was obtained from all providers and fitness professionals at the time of the initial EIM training and orientation (See Fig. 1).
Fig. 1.
Exercise is Medicine (EIM) pilot study design: acceptability and intervention phases, 2013–2014, Chattanooga, Tennessee, USA.
Acceptability phase design
Briefly, separate training sessions were held in several locations for the providers and fitness professionals. The training sessions were divided into modules, which included a review of physical activity and health outcomes, an understanding of the physical activity assessment (i.e., physical activity level, physical activity readiness questionnaire — PARQ), counseling, and referral portions of the EIM protocols. The training sessions were tailored for providers and fitness professionals in accordance with their respective EIM Action Guides. An evaluation of the training experience of both groups was conducted by onsite surveys. In addition, clinical support staff received a brief orientation to the principles of EIM at each clinical site. Following the initial trainings, each of the providers were visited at their clinical sites routinely by research assistants to update EIM protocol files, provide logistical support to staff, and collect exercise prescription and referral recording forms. We sought to solicit both quantitative and qualitative information from both providers and fitness professionals who underwent training in the use of EIM protocols and had used the protocols over a period of 6 months. Follow-up sessions were conducted among the providers at each of the clinical sites and among the fitness professionals at a common community site. During these sessions assessments addressing implementation, acceptability, self-efficacy in the use of EIM, and overall satisfaction of the EIM process were conducted among all participating providers and fitness professionals. Based upon feedback from these sessions, we modified the EIM protocols to be more user-friendly for both the providers and fitness professionals. The modifications of the EIM protocols included 1) adaptation of the physical activity assessment and counseling portions of the provider EIM protocols for use in the electronic medical record (EMR); and 2) adaptation of the provider referral letter from hardcopy form to an EMR-generated referral letter for the patient and community PA program.
Intervention phase: study population
During late summer and early fall, 2013, two academic primary care clinics from our original pool of 5 clinical sites were selected for this phase of the pilot study. The combined number of providers included 50 resident and attending physicians between both sites. These were previously trained in the use of the EIM protocols and for this phase were oriented to the EMR-modified EIM assessment and referral protocols which generated letters of referral to one of four YMCA branches associated with the Chattanooga Metropolitan YMCA (Y) (See Fig. 1). Eight (two from each Branch) Y-trained fitness professionals were oriented to the modified EIM protocols and the process of enrolling patients referred to their respective Y Branches. Apparently clinically healthy adult and/or disease-managed patients, aged 18 years or older and seen at either of the participating clinical sites were eligible to participate in the intervention portion of the EIM pilot study. Over 50% of the patients served by these clinical sites represented low-income and/or racial/ethnically diverse populations. Patients with uncontrolled hypertension, poorly controlled diabetes, and unstable coronary artery disease were excluded from the study, along with patients who were unable to walk at least 400 m unassisted. All eligible patients were provided with the option following their initial EIM assessment to be referred to the Y for PA programming.
Intervention measures
At the time of a clinic appointment each patient was initially assessed using the EIM physical activity assessment questions via the EMR. In addition, each patient completed at baseline and at follow-up the International Physical Activity Questionnaire (IPAQ) short form and the Centers for Disease Control and Prevention (CDC) Health-Related Quality of Life (HRQOL); they also self-assessed health status. Clinical information for each patient was abstracted from the EMR at baseline and follow-up, this included weight, height, calculated BMI, chronic disease history, and the behavioral risk factors of tobacco and alcohol use. An incentive of 12 weeks of complimentary Y membership was offered to each EIM-assessed and referred patient. Patients who did not enroll in any Y sessions were identified as EIM patients; patients who attended one or more Y sessions were identified as EIM + participants. EIM + participants were provided with personal PA plans and met regularly with the fitness professional, usually a personal trainer, or were enrolled in ongoing PA programming. EIM patients were provided with PA information only. The intervention portion of the pilot study was conducted over a total of 16 weeks. EIM trainers were available to both providers and Y fitness professionals to address questions and serve as a resource for EIM throughout the study. Following the intervention period, a comparison sample of EIM patients from each of the clinical sites was contacted by telephone and/or email and had their physical activity levels assessed by self-report using the IPAQ short form and HRQOL and health status assessed by the CDC survey instrument. Informed Consent: All protocols for the EIM study were approved by the Institutional Review Boards at both the University of Tennessee at Chattanooga and the University of Tennessee College of Medicine Chattanooga. Informed consent was obtained from all patients at the time of the initial clinical visit.
Statistical methods
All statistical analyses were conducted using IBM SPSS Statistics 22©. Means and standard errors were calculated for all continuous variables. Comparisons of continuous variables at baseline were assessed by applying paired ‘t’ tests with significance noted at p < 0.05. Net between pre–post measures were assessed through the use of either the Mann Whitney Test or the Kruskal–Wallis Test for independent samples, with significance noted at p < 0.01.
Results
EIM acceptability phase, provider results
A total of 30 out of the original 80 providers invited to participate (37.5%) provided survey responses to the EIM acceptability phase evaluation surveys following ~ 6 months of use of the EIM protocols (Table 1). Ninety percent of respondents were physicians (27/30). The majority of patients seen by these providers were middle to older in age, more likely to be women, and to have a chronic disease (Table 1). Forty percent (12/30) of providers reported that the EIM Health Care Provider Action Guide was easy to use, with 50% (15/30) neutral. In terms of practice, exposure to the use of the EIM protocols did not appear to impact the amount of time providers spent talking to their patients about physical activity, with 30% (9/30) spending from 0–1 min, and 70% (21/30) spending greater than 1 min but less than 5 min talking to their patients about physical activity. Fifty-three percent (Table 1) of providers indicated that the use of the EIM protocols improved their counseling skills, while the group was split between feeling neutral and being helped by EIM in overcoming barriers for assessment and counseling about PA among their patients (Table 1). Almost 60% of providers (Table 1) were neutral as to whether the EIM process helped to increase their patients' physical activity, with 30% responding in the affirmative. Providers remained neutral relative to whether EIM was helpful with record keeping, staff development, or increasing personal PA. However, the majority of respondents agreed that they would recommend EIM to other providers, and that their patients liked the EIM experience (Table 1). Providers were unified in their qualitative recommendation to integrate the EIM protocols of PA assessment and referral into the EMR in response to questions about how to improve the EIM process (data not shown).
Table 1.
EIM acceptability phase: summary results among healthcare providers and health and fitness professionals.
| Characteristic | n (%) |
|---|---|
| Type of provider | |
| Physician | 27 (90) |
| Nurse practitioner | 2 (7) |
| Physician assistant | 1 (3) |
| Proportion of practice chronic disease patients | |
| Less than 20% | 7 (23) |
| Greater than 20% | 23 (77) |
| Proportion of practice older adult patients | |
| Less than 20% | 12 (40) |
| Greater than 20% | 18 (60) |
| Use of provider action guide | |
| Difficult to use | 3 (10) |
| Neutral | 15 (50) |
| Easy to use | 12 (40) |
| Use of physical activity assessment tools | |
| Difficult to use | 2 (6.6) |
| Neutral | 14 (46.7) |
| Easy to use | 14 (46.7) |
| EIM helps counseling skills | |
| Neutral to not helpful | 14 (46.7) |
| Helpful to very helpful | 16 (53.3) |
| EIM increases patient physical activity | |
| No | 4 (13.3) |
| Neutral | 17 (56.7) |
| Yes | 9 (30) |
| Recommend EIM to other providers | |
| No | 4 (13.3) |
| Neutral | 9 (30) |
| Yes | 17 (56.7) |
| Type of fitness professional | |
| Exercise physiologist | 1 (6.7) |
| Physical educator | 2 (13.3) |
| Parks and recreation specialist | 2 (13.3) |
| Personal trainer | 10 (66.7) |
| EIM helps with provider communication | |
| Neutral to not helpful | 7 (46.7) |
| Helpful to very helpful | 8 (53.3) |
| EIM helps with the referral to provider process | |
| Neutral to not helpful | 0 |
| Helpful to very helpful | 15 (100) |
| EIM enhanced communication with provider | |
| Yes | 15 (100) |
| No | 0 |
| Participants like EIM | |
| Yes | 12 (80) |
| No | 3 (20) |
| Recommend EIM to other fitness professionals | |
| Neutral | 2 (13.3) |
| Yes | 13 (86.7) |
| No | 0 |
EIM acceptability phase, fitness professional results
A total of 15 of the original 18 (60%) fitness professionals completed the EIM acceptability phase evaluation surveys following ~ 6 months of exposure and use of the EIM protocols. Two-thirds of these fitness professionals were employed as personal trainers, with the remainder of respondents representing positions such as exercise physiologists and park and recreational specialists (Table 1). Over 70% (11/15) of all fitness professionals held some level of certification from either the American College of Sports Medicine (ACSM), American Council on Exercise (ACE), or the National Association of Strength and Conditioning. Over 80% (13/15) of the fitness professionals reported that the EIM Health and Fitness Professional Action Guide were well to very well organized. This response was similar for each of the Action Guide sections including the provider communication, introduction letter, sample medical history and informed consent forms, Starting an Exercise Program patient handout, and Prescription for Health Series. To the extent that EIM materials were perceived as helpful, the fitness professionals responded accordingly: 53% (8/15) found the communication strategies somewhat helpful to helpful; 46% (7/15) reported the procedures for handling referrals helpful to very helpful; 40% (6/15) found the use of the Physical Activity Guidelines for Americans (PAGS) helpful to very helpful in their practice; 66% (10/15) found that EIM was somewhat to very helpful in formulating their recommendations for patient/client exercise programming; while 47% (7/15) found the EIM guidance about communicating with providers helpful to very helpful in their practice. Use of the EIM materials was reported to be easy to very easy to use by more than 80% (12/15) of respondents; however, in practice only 26% (4/15) of fitness professionals reported receiving 1 or more patient referrals from providers during the EIM acceptability phase of the study. Over 85% of fitness professionals indicated they would recommend the EIM materials to other fitness professionals (Table 1). Most of the fitness professionals indicated that EIM was liked by participants (Table 1) and positively improved participant levels of PA as well as positively influencing their personal levels of PA. The majority of these professionals reported that EIM had become a routine part of their practice during the study period (13/15). Qualitative responses indicated a desire to improve communication skills and techniques with providers, improve the referral process, and the need to learn more about marketing their skills as fitness professionals to providers (data not shown).
EIM intervention phase results
During the 3 month pilot intervention period a total of 170 patients were exposed to the EIM protocols with 60 patients referred to the community PA Y program. From among these 60 patients, a total of 18 EIM + patients enrolled in the community PA programming and completed both baseline and follow-up assessments. A comparison group of 18 from among the 110 EIM patients was selected to match the 18 EIM + as closely as possible with respect to sex, age, and race/ethnicity (Table 2). The mean age of both groups was 53 and 46 years, respectively (Table 2); most participants were female. The measures of weight, BMI, and all modes of PA did not differ statistically between the EIM + and EIM only patients at baseline. However, the proportion of patients reporting a history of asthma was significantly higher among the EIM + compared with EIM only patients, while in contrast there was a significant difference among the two groups by self-reported health status, with 78% of EIM + patients reporting good to excellent health status compared to 38% of EIM only patients reporting this level (Table 2). Comparing the follow-up and change in baseline to follow-up PA assessments among the EIM + and the EIM only patients revealed significantly greater increases from baseline to 3 months at follow-up in self-reported moderate, vigorous, and total physical activity among the EIM + patients compared with the EIM only patients (Fig. 1). Examining changes in the HRQOL and self-assessed health status measures, the EIM + patients reported significantly fewer disability days compared with the EIM only patients from baseline to follow-up at 3 months (Fig. 2). In addition, EIM + patients reported a net decrease in the number of bad physical health days at follow-up compared with the EIM only patients (Fig. 3). There were, however, no significant differences noted for number of bad mental health days, with a net zero difference for each group (Fig. 3).
Table 2.
Patient characteristics at baseline, intervention phase, Exercise is Medicine pilot study.
| Characteristic | EIM + PA program | EIM |
|---|---|---|
| Age (years, mean ± se) | 53 ± 2.39 | 46 ± 3.65 |
| Weight (kg, mean ± se) | 103.1 ± 6.90 | 106.91 ± 10.96 |
| BMI (kg/m2, mean ± se) | 36.56 ± 2.45 | 39.86 ± 4.55 |
| Moderate PA min/week | 132.78 ± 34.37 | 201.11 ± 46.39 |
| Vigorous PA min/week | 13.61 ± 7.34 | 14.44 ± 8.10 |
| Total PA min/week | 234.44 ± 57.91 | 291.11 ± 68.42 |
| HRQOL physical days Not good/30 days |
14.44 ± 2.89 | 14.83 ± 3.00 |
| HRQOL mental days Not good/30 |
4.28 ± 1.89 | 4.76 ± 2.47 |
| Gender, percent (n) | 72% female (13) | 89% female (16) |
| Race/ethnicity, % (n) | 55% (10) AA⁎; 45% (8) W⁎⁎ | 60% (11) AA; 40% (7) W |
| Current smoker, % (n) | 11% (2) | 11% (2) |
| Use alcohol, % (n) | 22% (4) | 0% (0) |
| Known hypertension, % (n) | 33% (6) | 11% (2) |
| Known asthma, % (n) | 66% (12) | 22% (4)a |
| Overall health, good to excellent, % (n) | 78% (14) | 39% (7)b |
BMI = body mass index [weight (kg)/height (m2)].
PA = physical activity.
HRQOL = Health-related Quality of Life.
AA = African-American/black.
W = Caucasian/white.
p = .008.
p = .020 (Mantel–Haenszel Chi Square).
Fig. 2.
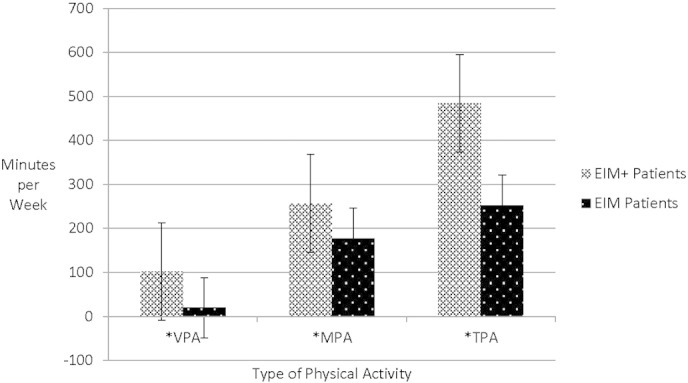
Physical activity in minutes per week: at follow-up and by change from baseline to follow-up among EIM + patients and EIM patients, 2013–2014, Chattanooga, Tennessee, USA.
MPA = moderate physical activity.
VPA = vigorous physical activity.
TPA = total physical activity.
ap = .003, independent samples, Mann–Whitney U test.
bp = .019, independent samples, Mann–Whitney U test.
cp = .000, independent samples, Mann–Whitney U test.
Fig. 3.
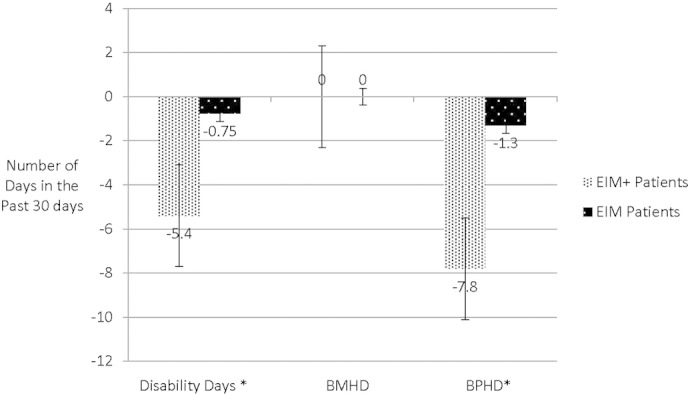
Number of days per month for: Disability Days; BMHD; and BPHD among EIM + patients and EIM patients, change from baseline to follow-up, 2014, Chattanooga, Tennessee, USA.
BMHD = bad mental health days.
BPHD = bad physical health days.
EIM = Exercise is Medicine.
EIM + = EIM assessed patients + referred and enrolled in a community Y physical activity program.
EIM only = EIM assessment alone with no enrollment into community Y physical activity program.
ap = .040, independent samples, Kruskal–Wallis test.
Discussion
The results from this EIM study suggest that providers and fitness professionals exposed to the training and use of EIM protocols found EIM protocols useful in their respective practices. The extent that the training and use of the EIM facilitated practice behavior changes among HCP appears equivocal, since almost half of HCP registered a neutral response to the set of questions regarding practice behavior changes following training and use of the EIM protocols. The content material of the EIM protocols used in the pilot study for both the providers and fitness professionals was perceived as important, helpful, and relevant to their practice settings.
Following 6 months of use of the EIM protocols, both providers and fitness professionals found the EIM protocols useful overall, but identified some significant barriers to their use in their current form and format. Namely the providers perceived the use of hardcopy paper materials as cumbersome and disruptive to the flow of the daily practice of primary care medicine via EMR. These findings tend to support the current trend in integrating the EIM assessment and referral protocols into the EMR, as reported in the work of Coleman et al. (2012). The fitness professionals, although supportive of the concept of the EIM focus on health fitness professionalism and routine communication with providers, found these additional tasks cumbersome and awkward. These findings suggest the current practice culture of fitness professionals is limited in its routine exposure to and communication with providers. This apparent deficit in communication between providers and fitness professionals was reported in a review by Patrick et al. (2009). Indeed, except for those fitness professionals associated with therapeutic exercise programming (e.g., cardiac and pulmonary rehabilitation), few of these professionals have any type of routine professional contact with providers. Health care providers also noted through the evaluation surveys that a very low proportion of them had routine professional contact with fitness professionals. Hence, when faced with the decision of where to refer a patient for exercise/PA programming, providers often were unlikely to refer simply because of a lack of knowledge about quality and accessible programs and/or fitness professionals.
Adaptation of the EIM protocols from online and hardcopy format to EMR-based use was easily facilitated within our two academic primary care practices. Adapting the efforts of Kaiser Permanente of Southern California (Coleman et al., 2012) all patients appeared very satisfied with assessment and referral portion of the EIM protocols, with over 170 patients assessed during the 16-week intervention phase. However, of these 170 patients who underwent the EIM protocol assessment, only 60 patients were actually referred to the community PA programs offered through the Y. Through qualitative and quantitative assessments, barriers to patient participation in community PA programs were partially attributed to lack of transport and reported lack of time which are common barriers identified among previous studies (Pavey et al., 2011, van Sluijs et al., 2005). Since almost half of our clinic patients represented persons from low income neighborhoods, this too, may have contributed to a lack of interest for the Y programs by some patients as documented in previous studies (Ham et al., 2007, Whitt-Glover et al., 2007). The offered incentive of 12 weeks of complimentary Y membership apparently did not overcome these barriers among a number of patients exposed to the EIM protocols. Comparing the EIM + patients with EIM only patients consistently demonstrated significantly more reported PA among the EIM + patients across all domains of PA including transport, recreation, planned exercise, total moderate intensity, and vigorous intensity PA.
The results from the intervention phase of this pilot study which documented increased PA among EIM + patients compared with EIM only patients is subject to several limitations: 1) potential self-selection cannot be ruled out when comparing the EIM + and the EIM only patients, since randomization was not employed in assigning patients to either EIM + or EIM only; 2) sample size was limited during the intervention phase of the pilot study, due in part to the logistics of conducting follow-up assessments among EIM patients in the non-experimental context of regular primary care practice; 3) duration of the intervention phase and follow-up limited to 3 months (12 weeks), which has been shown to be of limited generalizability (Heath et al., 2012); and 4) limited access to clinical and biomedical data for each of the EIM patient participants.
Conclusions
The use of EIM PA assessment and referral protocols, especially when adapted and embedded in the EMR, appear to be both feasible and adaptable to the health care setting. Furthermore, the use of the EIM protocols when successful in facilitating referral to community PA programming seem to be an emerging approach that may increase the PA levels among adult primary care patients. However, larger, more well controlled studies are needed to confirm the EIM approach as an effective strategy for improving PA behaviors among previously inactive adults who are seen by providers and successfully assessed and referred to community PA programming.
Funding
This study was generously supported in part by funding from the American College of Sports Medicine (5U58DP001132-05 CDC).
Disclaimer
The views and interpretation of these data are solely those of the authors and do not represent an official statement or rendering by the American College of Sports Medicine.
Disclosure
The authors declare that there are no conflicts of interests.
Acknowledgments
The authors wish to thank Robert Fugatt, Michael Min, and Cullen Black for their contribution to this research effort while serving as student research assistants. Data collection, data organization, and selected data analysis were carried out by this team of students. A special thank you is offered to Bill Rush, Program Director of Community Programs for the Metropolitan YMCA of Chattanooga.
References
- Calfas K.J., Long B.J., Sallis J.F., Wooten W.J., Pratt M., Patrick K. A controlled trial of physician counseling to promote the adoption of physical activity. Prev. Med. 1996;25:225–233. doi: 10.1006/pmed.1996.0050. [DOI] [PubMed] [Google Scholar]
- Coleman K.J., Ngor E., Reynolds K. Initial validation of an exercise “vital sign” in electronic medical records. Med. Sci. Sports Exerc. 2012;44(11):2071–2076. doi: 10.1249/MSS.0b013e3182630ec1. [DOI] [PubMed] [Google Scholar]
- Hahn R.A., Teutsch S.M., Rothenberg R.B., Marks J.S. Excess deaths from nine chronic diseases in the United States, 1986. JAMA. 1990;264:2654–2659. [PubMed] [Google Scholar]
- Hallal P.C., Andersen L.B., Bull F.C. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- Ham S.A., Yore M.M., Kruger J. Physical activity patterns among Latinos in the United States: putting the pieces together. Prev. Chronic Dis. 2007;4(4) [PMC free article] [PubMed] [Google Scholar]
- Haskell W.L., Lee I.-M., Pate R.R. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007;39:1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- Heath G.W., Brownson R.C., Kruger J., Miles R., Powell K.E., Ramsey L.T. The effectiveness of urban design and land use and transport policies and practices to increase physical activity: a systematic review. J. Phys. Act. Health. 2006;1:S55–S71. doi: 10.1123/jpah.3.s1.s55. [DOI] [PubMed] [Google Scholar]
- Heath G.W., Parra D.C., Sarmiento O.L. Evidence-based intervention in physical activity: lessons from around the world. Lancet. 2012;380:272–281. doi: 10.1016/S0140-6736(12)60816-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn E.B., Ramsey L.T., Brownson R.C. The effectiveness of interventions to increase physical activity. A systematic review(1,2) Am. J. Prev. Med. 2002;22(4 Suppl. 1):73–107. doi: 10.1016/s0749-3797(02)00434-8. (May) [DOI] [PubMed] [Google Scholar]
- Kahn E.B., Ramsey L.T., Brownson R.C. The effectiveness of interventions to increase physical activity: a systematic review. Am. J. Prev. Med. 2002;22(4S):73–107. doi: 10.1016/s0749-3797(02)00434-8. [DOI] [PubMed] [Google Scholar]
- Kahn E.B., Ramsey L.T., Brownson R.C. Chapter 2, Physical Activity. In: Zaza S., Briss P.A., Harris K.W., editors. The Guide to Community Preventive Services: What Works to Promote Health. Oxford University Press; Boston: 2005. pp. 80–113. [Google Scholar]
- Kohl H.W., III, Armstrong T., Craig C.L. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380:294–305. doi: 10.1016/S0140-6736(12)60898-8. [DOI] [PubMed] [Google Scholar]
- Lee I.-M., Shiroma E.J., Lobelo F. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobelo F., Stoutenberg M., Hutber A. The Exercise is Medicine Global Health Initiative: 2014 update. Br. J. Sports Med. 2014;48:1627–1633. doi: 10.1136/bjsports-2013-093080. [DOI] [PubMed] [Google Scholar]
- Long B.J., Calfas K.J., Patrick K. A multisite field test of the acceptability of physical activity counseling in primary care: Project PACE. Am. J. Prev. Med. 1996;12(2):73–81. [PubMed] [Google Scholar]
- McGinnis J.M. The public health burden of a sedentary lifestyle. Med. Sci. Sports Exerc. 1992;6:S196–S200. (Suppl.) [PubMed] [Google Scholar]
- McGinnis J.M., Foege W.H. Actual causes of death in the United States. JAMA. 1993;270:2207–2212. [PubMed] [Google Scholar]
- Pate R.R., Pratt M., Blair S.N. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- Patrick K., Pratt M., Sallis R.E. The healthcare sector's role in the U.S. National Physical Activity Plan. J. Phys. Act. Health. 2009;6(Suppl. 2):S211–S219. [PubMed] [Google Scholar]
- Pavey T.G., Taylor A.H., Fox K.R. Effect of exercise referral schemes in primary care on physical activity and improving health outcomes: systematic review and meta-analysis. BMJ. 2011;343:d6462. doi: 10.1136/bmj.d6462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell K.E., Thompson P.D., Caspersen C.J., Kendrick J.S. Physical activity and the incidence of coronary heart disease. Annu. Rev. Public Health. 1987;8:253–287. doi: 10.1146/annurev.pu.08.050187.001345. [DOI] [PubMed] [Google Scholar]
- Task Force on Community Preventive Services Increasing physical activity. A report on recommendations of the Task Force on Community Preventive Services. MMWR Morb. Mortal. Wkly Rep. 2001;50(RR-18):1–16. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion; Rockville, MD: 2014. Healthy People 2020 Leading Health Indicators: Progress Update. (Available from: U.S. GPO, Washington) [Google Scholar]
- van Sluijs E.M., van Poppel M.N., Twisk J.W. Effect of a tailored physical activity intervention delivered in general practice settings: results of a randomized controlled trial. Am. J. Public Health. 2005;95:1825–1831. doi: 10.2105/AJPH.2004.044537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitt-Glover M.C., Taylor W.C., Heath G.W., Macera C.A. Self-reported physical activity among blacks: estimates from national surveys. Am. J. Prev. Med. 2007;33(5):412–417. doi: 10.1016/j.amepre.2007.07.024. (Nov) [DOI] [PubMed] [Google Scholar]