Abstract
Objective
To validate, for the first time, the Risk Behaviour Diagnosis (RBD) Scale for Aboriginal Australian tobacco smokers, based on the Extended Parallel Process Model (EPPM). Despite high smoking prevalence, little is known about how Indigenous peoples assess their smoking risks.
Methods
In a cross-sectional study of 121 aboriginal smokers aged 18–45 in regional New South Wales, in 2014, RBD subscales were assessed for internal consistency. Scales included measures of perceived threat (susceptibility to and severity of smoking risks) and perceived efficacy (response efficacy and self-efficacy for quitting). An Aboriginal community panel appraised face and content validity. EPPM constructs of danger control (protective motivation) and fear control (defensive motivation) were assessed for cogency.
Results
Scales had acceptable to good internal consistency (Cronbach's alpha = 0.65–1.0). Most participants demonstrated high-perceived threat (77%, n = 93); and half had high-perceived efficacy (52%, n = 63). High-perceived efficacy with high-threat appeared consistent with danger control dominance; low-perceived efficacy with high-threat was consistent with fear control dominance.
Conclusions
In these Aboriginal smokers of reproductive age, the RBD Scale appeared valid and reliable. Further research is required to assess whether the RBD Scale and EPPM can predict quit attempts and assist with tailored approaches to counselling and targeted health promotion campaigns.
Keywords: Tobacco smoking, Australian Aborigines, Indigenous population, Risk behaviours, Behavioural medicine, Validation studies, Smoking cessation, Health promotion, Mass media, Health communication
Highlights
-
•
First study on the Risk Behaviour Diagnosis (RBD) Scale in an Indigenous population
-
•
Perceived efficacy and threat relate to intention to quit smoking in this sample.
-
•
High-threat high-efficacy had the strongest evidence for danger control responses.
-
•
The RBD Scale may help develop tailored anti-tobacco messages for Indigenous smokers.
Introduction
Tobacco smoking by Indigenous peoples is of major concern globally, with high prevalence rates showing little decline. The decline of smoking in the general population in Western nations is in part due to successful anti-tobacco campaigns. The small downward shift in Aboriginal Australian smoking rates over the last decade has not been replicated in the peak reproductive subgroup of 25–34 years (Australian Bureau of Statistics, 2014), when exposure is highest for babies and children. The disparity in daily smoking rates in Australia is stark at 12.8% for the general population (Australian Institute of Health and Welfare, 2013), versus 42% in Aboriginal Australians (Australian Bureau of Statistics, 2014), with remote community rates up to 85% (Robertson et al., 2013). This raises the question, how can we improve the effectiveness of tobacco control messages for Indigenous populations and in particular Aboriginal Australians?
Much is known about the historical antecedents of smoking in Aboriginal Australians (Brady, 2002), the impact of the social determinants of health (Shepherd et al., 2011), and the knowledge levels of Aboriginal Australians about smoking (Gould et al., 2013a). Little is known, in contrast, about how Indigenous populations, including Aboriginal Australians assess the threat of smoking, and their perceived efficacy for quitting. Such information is required to inform the development of targeted campaigns.
Indigenous peoples have good recall of mainstream campaigns (Boyle et al., 2010), and highly rate the message efficacy of mainstream campaigns (Stewart et al., 2011), but these campaigns have not translated into quitting behaviour (Gould et al., 2013b, Ivers et al., 2005). Anti-tobacco messages which are not pitched at the right level can fail or have unintended consequences (Witte and Allen, 2000). Fear-based campaigns, for example, have been found to be most effective for those who have high self-efficacy or high motivation (Wong and Cappella, 2009, Peters et al., 2013).
Targeted approaches are a key objective of Australian national tobacco strategies (Commonwealth of Australia, 2012), and the WHO Framework Convention on Tobacco Control (Article 4) (World Health Organization, 2003), and are preferred by Indigenous peoples (Gould et al., 2013b). In Australia, the majority of organisations developing culturally targeted anti-tobacco messages for Aboriginal smokers avoided fear campaigns and favoured positive and educational messages (Gould et al., 2014a), although the rationale for this approach has not been explored.
It is important to validate psychometric measures before use in a cross-cultural Indigenous context (Drew et al., 2010). Instruments to assess mental health and substance use (Stephens et al., 2013), have been recently validated for Aboriginal Australians, but not tobacco smoking. This study uses the findings from a cross-sectional study of Aboriginal Australians to validate risk assessment scales for tobacco smoking in this population.
Materials and methods
The protocol for the study has been published (Gould et al., 2014b), thus we provide a brief summary of methods.
Study setting and recruitment
In a regional area of New South Wales (NSW) on Australia's east coast, the cross-sectional study was conducted in a community sample of Aboriginal smokers aged 18–45 years from January to May 2014. Quota sampling was used by gender and age groups to represent the target population, calculated from the 2008 Aboriginal smoking prevalence (Australian Bureau of Statistics, 2009), and the 2011 Aboriginal population census (Table 1). Participants (N = 121) were recruited by personal intercept through community events, such as Aboriginal cultural festivals (n = 35) and cultural centres (n = 15), health days (n = 20), sporting events (n = 19), through community/health services (n = 15), street intercept (n = 8) and by personal contact (n = 9). An Aboriginal ‘Tackling Tobacco and Healthy Lifestyle Team’ facilitated the attendance of the interview team at several local events.
Table 1.
Stratified sampling strategy of target Aboriginal population on the Mid North Coast of New South Wales, and actual sample (N = 121).
| Target population (2011 census from regional LGA) |
Smoking prevalence (2008 NATSISS) |
% of target populations in regional city who smoke |
Proposed sample stratified by gender & age group |
Actual sample recruited |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age range (years) | Male N | Female N | Male % | Female % | Male N (% of total) | Female N (% of total) | Male N | Female N | Male N | Female N |
| 18–24 | 172 | 178 | 38.7 | 39.7 | 67 (13.9) | 71 (14.7) | 17 | 18 | 18 | 18 |
| 25–34 | 142 | 184 | 56 | 50.1 | 80 (16.6) | 92 (19) | 20 | 23 | 18 | 23 |
| 35–44 | 154 | 187 | 55.5 | 47.3 | 85 (17.6) | 88 (18.2) | 21 | 22 | 22 | 22 |
| Total | 468 | 549 | 232 (48.1) | 251 (51.9) | 58 | 63 | 58 | 63 | ||
Adapted with permission of the authors (Gould et al., 2014b).
Bold figures indicate total numbers of men and women proposed for the sample and actually recruited.
The interviewers included a non-Aboriginal female (author GG), a male Aboriginal research assistant, and a female Aboriginal volunteer who approached potential participants, informed them of the study and canvassed their interest in participating. Author GG trained all the interviewers. The study adhered to the guideline for ethical research in Indigenous populations, and relevant ethics committee approvals as detailed in the study protocol (Gould et al., 2014b).
Theory/calculation
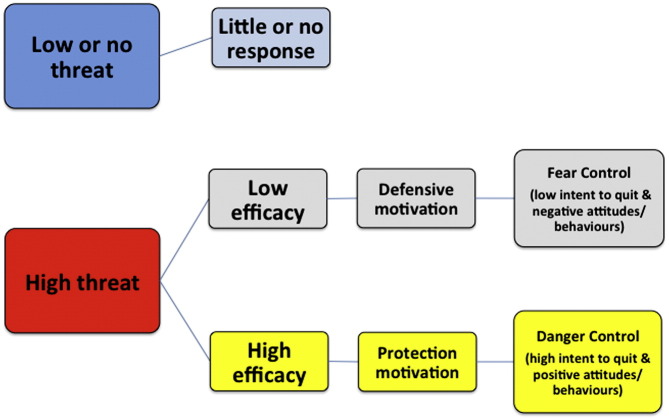
The survey included questions based on the Risk Behaviour Diagnosis (RBD) Scale (Witte et al., 1996, Witte et al., 2001), adapted for tobacco smoking, and the Aboriginal target populations from the Extended Parallel Process Model (EPPM) (Witte et al., 1996, Witte et al., 2001). The central premise of the EPPM is that when under a health risk threat people may control the danger by making a positive shift in attitude and behaviour, termed ‘danger control dominance’. Alternately they may feel fearful and try to control the emotion of fear by denial, reactance, or message derogation, called ‘fear control dominance’ (Witte et al., 2001). The pathways proposed by the EPPM are depicted in Fig. 1.
Fig. 1.
The extended parallel process model and expected responses to threat and efficacy levels.
Adapted from Witte.(Witte et al., 2001).
The level of perceived efficacy (response efficacy and self-efficacy) moderates responses to high threat. People with high efficacy are more likely to be in danger control and change their attitudes or behaviour (e.g. quit smoking). Alternatively, if efficacy is low, people are more likely to exhibit defensive avoidance and fear control. When the perceived threat is low or absent then people may be indifferent, and unlikely to change attitudes or behaviour.
The RBD Scale comprises questions to measure the EPPM constructs (Witte et al., 2001). The scale is used to calculate a discriminating value predicted to be diagnostic for danger vs. fear control. The EPPM has been validated and used for many health risks, including smoking (Wong and Cappella, 2009), and in a wide range of populations (including cross-cultural groups).
We conducted a process of Aboriginal community consultation to test the content and face validity, suitability, readability, cultural appropriateness, acceptability and feasibility of the survey instruments. The process of scale adaption for the Aboriginal target population is described in the study protocol (Gould et al., 2014b).
The RBD subscales and scales for protection responses and fear control responses (details in Supplementary Table A.1) were measured using 5 point Likert Scales. Intentions to quit smoking were measured using 4 point Likert Scales. The total score for each scale was divided by the number of questions in the scale to create mean indices. Median splits around the distribution of scale scores produced binary categories of high-low responses. This resulted in the following variables: total perceived threat (high vs low); total perceived efficacy (high vs low); protection responses (high vs low); fear control responses (high vs low); and danger control responses (intentions to quit: high vs low).
We grouped the responses to the RBD Scale into four quadrants as suggested by Popova (Popova, 2012), subtitled with descriptors from Rimal and Real (Rimal and Real, 2003), as follows:
-
•
I — high threat-high efficacy — responsive
-
•
II — high threat-low efficacy — pro-active
-
•
III — low threat-high efficacy — avoidant
-
•
IV — low threat-low efficacy — indifferent.
Discriminating value was calculated from the formula (∑ perceived efficacy) − (∑ perceived threat) = discriminating value, then categorised into positive (> 0) or negative (≤ 0) (Witte et al., 2001).
Statistical analysis
Analyses, including descriptive, were performed using SPSS v20. The internal reliability of the scales was assessed with Cronbach's alpha coefficient. A factor analysis explored the RBD subscale dimensions. Separate chi-squared analyses were performed stratified by each RBD quadrant to determine whether intentions to quit, protection responses, fear control responses and home smoking rules were associated with RBD quadrants.
Results
Internal reliability
Table 2 lists the internal reliability of each scale. A Cronbach's alpha of 0.7 or over demonstrates acceptable reliability (Tavakol and Dennick, 2011). Some scale results improved when items were removed, resulting in an acceptable reliability level of subscales (approximating r = 0.7). As the Cronbach's alpha was lower for the total perceived efficacy scale, this might indicate that response efficacy is slightly different to self-efficacy. The factor analysis revealed three components comprising response efficacy, self-efficacy, and perceived threat (included susceptibility and severity) (results not shown).
Table 2.
Internal consistency of the Risk Behaviour Diagnosis Scale and associated scales in Aboriginal smokers (N = 121) in regional New South Wales, Australia in 2014.
| Scale | Cronbach's alpha | Adjustments made | Median score (range) |
|---|---|---|---|
| Total perceived efficacy | 0.65 | 3.5 (1–5) | |
| Response efficacy | 0.69 | ||
| Self-efficacy | 0.71 | 0.82 with removal Q2c | |
| Total perceived threat | 0.79 | 0.81 with removal Q3c | 4 (1–5) |
| Susceptibility | 0.55 | 0.62 with removal Q3c | |
| Severity | 0.78 | ||
| Fear control response | 0.58 | 0.67 with removal Q6a | 2.3 (1–5) |
| Protection response | 0.67 | 4.3 (1–5) | |
| Danger control response | |||
| Intention to quit | 1.0 | 2.7 (1–4) |
Q2c — It is easy to stop smoking.
Q3c — I believe I am seriously at risk of getting ill from smoking.
Q6a — I prefer not to think about the health risks of smoking.
See Table A.1. for further details of scale questions.
Participants
The 121 participants included 116 (96%) tobacco smokers who self-identified as Aboriginal and five smokers (4%) who self-identified as Aboriginal and Torres Strait Islanders. Table 3 details the sample characteristics and scale responses.
Table 3.
Characteristics of Aboriginal participants from the Mid North Coast of New South Wales, Australia (N = 121) in 2014.
| Demographic characteristics | N (%) |
|---|---|
| Male | 58 (48%) |
| Female | 63 (52%) |
| Age group (years) | |
| 18–24 | 36 (30%) |
| 25–34 | 41 (34%) |
| 35–45 | 44 (36%) |
| Home smoking ban | |
| Complete ban | 96 (79%) |
| Partial/no ban | 25 (21%) |
| Variables from scales | N (%) |
| Total perceived efficacy | |
| High | 63 (52%) |
| Low | 58 (48%) |
| Total perceived threat | |
| High | 93 (77%) |
| Low | 28 (23%) |
| Protection responses | |
| High | 84 (69%) |
| Low | 37 (31%) |
| Fear control responses | |
| High | 63 (52%) |
| Low | 58 (48%) |
| Intention to quit | |
| High | 80 (66%) |
| Low | 41 (34%) |
The EPPM: danger control dominance and fear control dominance
Table 4 shows the four quadrants as divided according to the EPPM (Popova, 2012). Those in quadrant I with high-efficacy high-threat consistent with the EPPM theory showed high danger control responses i.e. intention to quit smoking (X2 = 16.67; df = 1; p < 0.001), illustrating danger control dominance. Participants in this quadrant were also significantly more likely to report home smoking bans (X2 = 24; df = 1; p < 0.001) and protection responses (X2 = 26.74; df = 1; p < 0.001).
Table 4.
Expected efficacy by threat associations according to the four quadrants of the EPPM in 121 Aboriginal smokers in regional New South Wales, Australia in 2014.
| High efficacy (n = 63) | Low efficacy (n = 58) | |
|---|---|---|
| High threat (n = 93) | Quadrant I: responsive Danger control expected n = 54; 45% |
Quadrant II: avoidant Fear control expected n = 39; 32% |
| Intention to quit | ✔*** | ✗ |
| Home smoking bans | ✔*** | ✔*** |
| Protection responses | ✔*** | ✗ |
| Fear control responses | ✗ | ✗ |
| Low threat (n = 28) | Quadrant III: pro-active Less danger control expected n = 9; 7% |
Quadrant IV: indifferent No response expected n = 19; 16% |
| Intention to quit | ✔a | ✗ |
| Home smoking bans | ✔a | ✗ |
| Protection responses | ✔a | ✗ |
| Fear control responses | ✗ | ✔* |
Legend: ✔* significant p < 0.05, ✔** significant p < 0.01, ✔*** significant p < 0.001, ✗ non-significant p > 0.05. ✔a Associated but significance non computable. Adapted from Popova (Popova, 2012).
Those with low efficacy and high threat (quadrant II) would be expected to be in fear control dominance according to the EPPM. These participants were significantly more likely to have a home smoking ban (X2 = 13.56; df = 1; p < 0.001), but there was no difference in relation to protection responses, or intention to quit (p > 0.05). Quadrant III with high efficacy and low threat consisted of only nine participants: eight of these had a high intention to quit and home smoking bans, and six had high protection responses. This suggests a pro-active response despite a lower threat from smoking.
The EPPM predicts that low threat combined with low efficacy (quadrant IV) would be associated with low danger control responses or no response. This was confirmed with no significant associations observed for these participants regarding intention to quit, home smoking bans, and protection responses in quadrant IV.
Participants with high fear control responses (denial, avoidance etc.) were significantly less likely to demonstrate an intention to quit smoking (X2 = 6.54; df = 1; p = 0.01). The only quadrant in which a significant association with fear control responses was demonstrated was quadrant IV, with 15/19 (79%) participants having high fear control responses (X2 = 6.37; df = 1; p = 0.01), giving evidence for avoidance and denial in this quadrant only (see Table 3). This suggests that the threat level, although classed as low here, was sufficiently high to produce fear control responses.
The majority (n = 102; 84%) of participants had a negative discriminating value. A negative discriminating value should, according to the RBD theory, imply ‘fear control dominance’. These participants should have a low intention to quit. Paradoxically ‘fear control dominance’ (negative discriminating value) was significantly associated with increased intention to quit (X2 = 5.49; df = 1; p < 0.05), with 63 (62%) of those with negative values having a high intention to quit. The anomaly, we believe, reflected the high levels of perceived threat compared to levels of perceived efficacy, in this population, giving mostly negative discriminating value scores. The discriminating value also was not associated with fear control responses.
Discussion
This was the first study known to the authors to investigate how Indigenous peoples assess their risks of smoking using the Risk Behaviour Diagnosis (RBD) Scale (Witte et al., 1996, Witte et al., 2001), developed from the Extended Parallel Process Model (EPPM) (Witte et al., 1996, Witte et al., 2001). In Aboriginal smokers aged 18–45 years in regional NSW the RBD Scale for tobacco smoking risk assessment appeared valid and reliable, as determined by face and content validity and tests of internal reliability.
The constructs of danger and fear control from the EPPM were tested to see if they applied to this population. The interaction between threat appraisal and coping appraisal appear to be important, giving support to the EPPM as a relevant model for this population. The discriminating value was not diagnostic for this sample. The discriminating value has been recently criticised by Popova (Popova, 2012), as it does not differentiate between low and high values of efficacy and threat but only the difference between them.
The division of efficacy and threat responses into quadrants was revealing. Quadrant I smokers with high-efficacy and high-threat gave the strongest indication of danger control dominance. Quadrant II smokers, with low-efficacy and high-threat, implied fear control dominance, but without direct evidence of high fear control responses. The absence of fear control responses for this quadrant is encouraging, as according to Witte once fear control responses such as denial or reactance set in, they can be difficult to reverse (Witte et al., 2001, p30). Quadrant II participants significantly imposed home smoking bans — demonstrating a protective response to passive smoking, suggesting perhaps a ‘partial danger control’. Quadrant III comprised an interesting group of nine individuals expected to demonstrate a lower level of danger control according to Popova (Popova, 2012). However Rimal and Real consider this quadrant pro-active (Rimal and Real, 2003), motivated by considerations other than perceived risk. Quadrant IV smokers unexpectedly showed high fear control responses such as avoidance, rather than indifference.
As fear messages are so ubiquitous in Australian tobacco control programmes, represented most obviously by graphic health warnings on plain packages, it is not surprising that levels of perceived threat were high in our sample. The high perceived threat may also reflect the locally-specific programmes operating in the region in 2010–2012 (Gould, 2013), recently followed by an Aboriginal ‘Tackling Tobacco and Healthy Lifestyle Team’, raising awareness of the impact of smoking on the Aboriginal community.
Increasing baseline fear levels in those with already high fear perceptions does not necessarily induce positive behaviours. Previous studies showed that using fear appeals in the context of high pre-existing fear is likely to be ineffective (Muthusamy et al., 2009). There is convincing support for high threat messages being effective for behavioural change only where efficacy is high, and vice-versa (Peters et al., 2013). Neurocognitive evidence shows that attention is automatically diverted from high threat messages in a high-risk population (Peters et al., 2013).
Our findings suggest a central role for perceived efficacy. If fear appeals are used they should be accompanied by high efficacy interventions (Witte and Allen, 2000, Peters et al., 2013) — something which may be lacking for Aboriginal smokers, with culturally targeted positively-framed approaches inconsistently available in Australia, especially in remote areas (Robertson et al., 2013, Gould et al., 2014a). The targeted national mass media ‘Break The Chain’ campaign, with an efficacy message, has been aired in Australia since 2011, but its reach may be inadequate in some areas. The campaign has relied on only one TV advertisement.
A body of knowledge has been built from the EPPM, which is the basis of previous research across many populations and different health behaviours, and informs the planning of tobacco counter-marketing (Witte and Allen, 2000). Witte recommends that interventions should be targeted to the levels of danger control and fear control on a population and individual basis (Witte et al., 1996, Witte et al., 2001). Translating this advice into practical strategies for our sample, we recommend for quadrants I and III ‘how to quit’ messages and access to smoking cessation support; for quadrant II messages to build efficacy and also support quitting; and for quadrant IV personalisation of the health risks and strategies to counter denial, reactance etc., and also messages to build efficacy.
Differences in risk assessment and motivation to quit smoking are valid concerns for marginalised populations with high prevalence, such as Indigenous and minority populations. Understanding these differences might have value for the development of tailored tobacco control and cessation interventions.
Study limitations and strengths
The study, with strong theoretical foundations, has laid the groundwork for this type of analysis to be done in a larger sample and in other Indigenous populations. We attempted to minimise bias in several ways: the survey was interviewer-administered so we could include those with low literacy levels; we recruited from a variety of sites to minimise selection bias. These features add to the strength of the study. The study had a number of limitations common to small samples. Response bias may have been operant e.g. some smokers may be unwilling to reveal attitudes of denial and avoidance. The Aboriginal regional sample may limit the generalisability to other Aboriginal peoples.
Conclusions
The RBD Scale may have important implications to fine-tune our approach to tobacco control in Aboriginal Australians through mass media campaigns and smoking cessation strategies. New strategies are especially important in the peak reproductive years, where other approaches do not seem to be working. By assessing smokers in a local area, anti-tobacco messages and mass media can be targeted to the need of the local audience for population based health promotion campaigns. Assessing a smoker using these scales may enable health professionals to offer tailored approaches to cessation. The RBD Scale may be valuable for other Indigenous populations globally and are worthy of further consideration. Further research is required to assess whether these scales can predict actual quit attempts, and assist with tailored approaches to counselling and local health promotion programmes, thus improve the response of Indigenous smokers to tobacco control interventions.
Funding statement
This work was supported by:
-
•
The National Health and Medical Research Council (Australia) and the National Heart Foundation (Australia) post-graduate scholarship for Indigenous health research — (grant numbers APP1039759 and PP 11S 6181)
-
•
The Royal Australian College of General Practitioners and Australian Primary Health Care Research Institute Indigenous Health Award 2013
-
•
James Cook University, Faculty of Medicine, Health & Molecular Sciences, Graduate Research Scheme grants 2013 and 2014
-
•
National Health and Medical Research Council (Australia) Career Development Award (grant number APP1046773)
-
•
None of the funding sources had any involvement with the study design, analysis or interpretation of data; nor in writing or publishing the report.
Contributor statement
GG was responsible for the concept and design of the project, developing and adapting the survey instruments and their digital format, testing the suitability of the survey for Indigenous participants, conducting surveys, training and supervising Indigenous research assistants, collating and analysing and interpreting results, writing the manuscript, and submitting the study. She takes overall responsibility for the content as guarantor. KW contributed to the research design and statistical analysis and critical review of manuscripts. YCJ as Aboriginal academic advisor advised on the Indigenous community consultation processes, recruitment strategy and the cultural interpretation of results, and provided critical review of the manuscript. ARC oversaw the study and advised on all aspects, and provided critical review of the manuscripts. All authors approved the final version.
The following is the supplementary data related to this article.
Risk Behaviour Diagnosis Scale and associated scales.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
Acknowledgments
We acknowledge the valuable input of the Aboriginal community panel and the support of the partnering Aboriginal Community Controlled Health Service, and their Tackling Tobacco and Healthy Lifestyle Team for this survey, the Aboriginal Health Worker who advised about the survey, the Aboriginal research assistant, and other volunteers, and the community participants — without them the study would not have been possible. We acknowledge the contribution of Dr. Andy McEwen who advised on aspects relating to tobacco smoking and smoking risk behaviours.
Contributor Information
Gillian Sandra Gould, Email: gillian.gould1@my.jcu.edu.au.
Kerrianne Watt, Email: kerrianne.watt@jcu.edu.au.
Yvonne Cadet-James, Email: yvonne.cadetjames@jcu.edu.au.
Alan R. Clough, Email: alan.clough@jcu.edu.au.
References
- Australian Institute of Health and Welfare . Australian Government; Canberra: 2013. National Drugs Strategy Household Surveys. (Available from: http://aihw.gov.au/alcohol-and-other-drugs/ndshs/2013/tobacco/ (accessed 19th July 2014)) [Google Scholar]
- Australian Bureau of Statistics . Australian Bureau of Statistics; Canberra: 2009. National Aboriginal and Torres Strait Islander Social Survey 2008. ( http://www.abs.gov.au/ausstats/abs@.nsf/mf/4714.0/ (accessed 19th July 2014)) [Google Scholar]
- Australian Bureau of Statistics . Australian Bureau of Statistics; Canberra: 2014. 4727.0.55.006 — Australian Aboriginal and Torres Strait Islander Health Survey: Updated Results, 2012–13. ([updated 06/06/2014]. Available from: http://www.abs.gov.au/ausstats/abs@.nsf/mf/4727.0.55.006 (accessed 19th July 2014)) [Google Scholar]
- Boyle T., Shepherd C.C.J., Pearson G. Awareness and impact of the ‘Bubblewrap’ advertising campaign among Aboriginal smokers in Western Australia. Tob. Control. 2010;19(1):83–86. doi: 10.1136/tc.2009.031856. [DOI] [PubMed] [Google Scholar]
- Brady M. Historical and cultural roots of tobacco use among Aboriginal and Torres Strait Island people. Aust. N. Z. J. Public Health. 2002;26(2):120–124. doi: 10.1111/j.1467-842x.2002.tb00903.x. [DOI] [PubMed] [Google Scholar]
- Commonwealth of Australia . Commonwealth of Australia; Canberra: 2012. National Tobacco Strategy 2012–2018 — A Strategy to Improve the Health of all Australians by Reducing the Prevalence of Smoking and its Associated Health, Social and Economic Costs, and the Inequalities it Causes. [Google Scholar]
- Drew N., Adams Y., Walker R. Issues in mental health assessment with Indigenous Australians. In: Purdie N., Dudgeon P., Walker R., editors. Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice. Department of Health and Ageing; Canberra: 2010. pp. 191–209. [Google Scholar]
- Gould G.S. 12th National Rural Health Conference. 2013. Making ‘Blow Away The Smokes’ DVD for Indigenous smokers — the journey and lessons learnt. ( http://nrha.org.au/12nrhc/wp-content/uploads/2013/06/Gould-Gillian_ppr.pdf (accessed 19th July 2014)) [Google Scholar]
- Gould G.S., Munn J., Watters T. Knowledge and views about maternal tobacco smoking and barriers for cessation in Aboriginal and Torres Strait Islanders: a systematic review and meta-ethnography. Nicotine Tob. Res. 2013;15(5):863–874. doi: 10.1093/ntr/nts211. [DOI] [PubMed] [Google Scholar]
- Gould G.S., McEwen A., Watters T. Should anti-tobacco media messages be culturally targeted for Indigenous populations? A systematic review and narrative synthesis. Tob. Control. July 1 2013;22(4):e7. doi: 10.1136/tobaccocontrol-2012-050436. [DOI] [PubMed] [Google Scholar]
- Gould G.S., Watt K., Stevenson L. Developing anti-tobacco messages for Australian Aboriginal and Torres Strait Islander peoples: evidence from a national cross-sectional survey. BMC Public Health. Mar 13 2014;14(1):250. doi: 10.1186/1471-2458-14-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould G.S., Watt K., McEwen A. Validation of risk assessment scales and predictors of intentions to quit smoking in Australian Aboriginal and Torres Strait Islander peoples: a cross-sectional survey protocol. BMJ Open. 2014;4(6) doi: 10.1136/bmjopen-2014-004887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivers R., Castro A., Parfitt D. Television and delivery of health promotion programs to remote Aboriginal communities. Health Promot. J. Aust. 2005;16(2):155–158. doi: 10.1071/he05155. [DOI] [PubMed] [Google Scholar]
- Muthusamy N., Levine T.R., Weber R. Scaring the already scared: some problems with HIV/AIDS fear appeals in Namibia. J. Commun. 2009;59(2):317–344. [Google Scholar]
- Peters G.-J.Y., Ruiter R.A., Kok G. Threatening communication: a critical re-analysis and a revised meta-analytic test of fear appeal theory. Health Psychol. Rev. 2013;7(Suppl. 1):S8–S31. doi: 10.1080/17437199.2012.703527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popova L. The extended parallel process model: illuminating the gaps in research. Health Educ. Behav. 2012;39(4):455–473. doi: 10.1177/1090198111418108. [DOI] [PubMed] [Google Scholar]
- Rimal R.N., Real K. Perceived risk and efficacy beliefs as motivators of change. Hum. Commun. Res. 2003;29(3):370–399. [Google Scholar]
- Robertson J., Conigrave K., Ivers R. Addressing high rates of smoking in remote Aboriginal communities: new evidence for GPs. Aust. Fam. Physician. 2013;42(7):492–496. [PubMed] [Google Scholar]
- Shepherd C.C.J., Li J., Zubrick S.R. Social gradients in the health of Indigenous Australians. Am. J. Public Health. 2011;102(1):107–117. doi: 10.2105/AJPH.2011.300354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens A., Bohanna I., Graham D. Screening and assessment instruments for use in Indigenous-specific alcohol and drug treatment rehabilitation. J. Trop. Psychol. 2013;3:e2. [Google Scholar]
- Stewart H.S., Bowden J.A., Bayly M.C. Potential effectiveness of specific anti-smoking mass media advertisements among Australian Indigenous smokers. Health Educ. Res. 2011;26(6):961–975. doi: 10.1093/her/cyr065. [DOI] [PubMed] [Google Scholar]
- Tavakol M., Dennick R. Making sense of Cronbach's alpha. Int. J. Med. Educ. 2011;2:53–55. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte K., Allen M. A Meta-analysis of fear appeals: implications for effective public health campaigns. Health Educ. Behav. 2000;27(5):591–615. doi: 10.1177/109019810002700506. [DOI] [PubMed] [Google Scholar]
- Witte K., Cameron K.A., McKeon J.K. Predicting risk behaviors: development and validation of a diagnostic scale. J. Health Commun. 1996;1:317–341. doi: 10.1080/108107396127988. [DOI] [PubMed] [Google Scholar]
- Witte K., Meyer G., Martell D. Sage Publications; Thousand Oaks, CA: 2001. Effective health risk messages: a step-by-step guide. [Google Scholar]
- Wong N.C.H., Cappella J.N. Antismoking threat and efficacy appeals: effects on smoking cessation intentions for smokers with low and high readiness to quit. J. Appl. Commun. Res. 2009;37(1):1–20. doi: 10.1080/00909880802593928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . WHO Document Production Services; Geneva, Switzerland: 2003. WHO Framework Convertion on Tobacco Control. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Risk Behaviour Diagnosis Scale and associated scales.