Abstract
In South Asians, a unique obesity phenotype of high abdominal fat is associated with increased cardiovascular risk. Low cardiorespiratory fitness (CRF) is associated with abdominal fat and an increased risk of cardiovascular disease. The purpose of this paper is to determine whether CRF as assessed by VO2 peak, in post-menopausal South Asian women, was associated with body fat distribution and abdominal fat. Physically inactive post-menopausal South Asian women (n = 55) from the Greater Vancouver area were recruited and assessed from January to August 2014. At baseline, VO2 peak was measured with the Bruce Protocol, abdominal fat with CT imaging, and body composition with dual energy X-ray absorptiometry. ANOVA was used to assess differences in subcutaneous abdominal adipose tissue (SAAT), visceral adipose tissue (VAT) and total abdominal adipose tissue (TAAT) between tertiles of CRF. Bivariate correlation and multiple linear regression analyses explored the association between VO2 peak with SAAT, VAT, TAAT and body composition. Models were further adjusted for body fat and body mass index (BMI). Compared to women in the lowest tertile of VO2 peak (13.8–21.8 mL/kg/min), women in the highest tertile (25.0–27.7 mL/kg/min) had significantly lower waist circumference, BMI, total body fat, body fat percentage, lean mass, SAAT, VAT and TAAT (p < 0.05). We found VO2 peak to be negatively associated with SAAT, VAT and TAAT, independent of age and body fatness but not independent of BMI. Further research is necessary to assess whether exercise and therefore improvements in CRF would alter SAAT, VAT and TAAT in post-menopausal South Asian women.
Keywords: Visceral adipose tissue, Cardiorespiratory fitness, South Asian, Maximal oxygen consumption, Postmenopausal
Highlights
-
•
South Asian women with higher cardiorespiratory fitness have lower abdominal fat.
-
•
This relationship is independent of age and body fat but not body mass index.
-
•
Role of exercise at altering abdominal fat in this population must be examined.
Introduction
South Asian ethnicity is associated with an increased prevalence of cardio-metabolic risk factors (such as dyslipidemia and impaired fasting glucose) which leads to a disproportionately greater risk of type 2 diabetes (T2D) (Garduno-Diaz and Khokhar, 2012) and cardiovascular disease (CVD) compared to Europeans (Joshi et al., 2007, Yusuf et al., 2001). For example, in the UK the prevalence of T2D in South Asians is five times higher (around 20%) than those of the indigenous European population (Gholap et al., 2011). In addition, the onset of T2D occurs approximately 5–10 years earlier in South Asians than persons of other ethnicities (Joshi et al., 2007), increasing the likelihood of associated complications such as CVD (Mather et al., 1998).
In South Asians, the rising prevalence of obesity and a preponderance of abdominal obesity are thought to be directly responsible for the increasing trend of T2D and CVD in this population (Anand et al., 2000, Lean et al., 2001, Misra and Khurana, 2011). South Asians have been shown to have greater visceral adipose tissue (VAT) at the same body mass index (BMI), waist circumference (WC) and body fat mass as Europeans (Lear et al., 2007) which contributes to a worsening cardio-metabolic profile (Lear et al., 2012). Of particular risk among the South Asian population are women after menopause as studies in post-menopausal women of other ethnicities have demonstrated that menopause is associated with increased risk for T2D and CVD (Rosano et al., 2007). This appears coincident with changes in body composition that include enlargement of the VAT depot (Janssen et al., 2015) and a reduction in cardiorespiratory fitness (CRF) (Lynch et al., 2002). However, to date this has not been shown in post-menopausal South Asian women.
Low CRF is a well accepted risk factor for T2D and CVD, and is influenced by physical activity as well as genetic heritability (Bouchard et al., 2011). In Europeans, CRF is negatively associated with the accumulation of VAT (Haufe et al., 2010, Janssen et al., 2004) and those categorized with high CRF have been shown to have lower amounts of VAT than those categorized with low CRF (Brock et al., 2011, O'Donovan et al., 2009). In a recent review by Gill et al., the authors suggested that a low fitness phenotype may play a role in explaining the increased risk of T2D and CVD in the South Asian population (Gill et al., 2014). This is supported by the lower CRF seen in South Asian men compared to European men (Ghouri et al., 2013). Given the unique obesity phenotype and its associated disease risk in South Asians, and the elevated disease risk in post-menopausal women, it is necessary to understand the association between CRF and body fat distribution in post-menopausal South Asian women. Therefore, the purpose of this study was to determine whether CRF, as determined by peak oxygen uptake (VO2 peak), was associated with body fat distribution and abdominal fat—specifically VAT—in physically inactive, post-menopausal South Asian women. Additionally, we aimed to explore whether CRF was associated with VAT independent of BMI. We hypothesized there would be a negative association between CRF and VAT and that this association would be independent of BMI.
Methods
This study was a cross-sectional baseline analysis of a registered randomized controlled trial (ClinicalTrials.gov #NCT01766453). Participants were recruited from the South Asian community in the Greater Vancouver area through local media. Individuals were eligible to participate in the study if they were post-menopausal (one year since their last menstrual cycle), had not engaged in regular physical activity in the previous 6 months (as defined by engaging in activity intended to increase heart rate) and had a WC of 80 cm or greater (cut off for abdominal obesity for South Asian women) (Alberti et al., 2005). Individuals were not eligible to participate if they reported having been diagnosed with CVD or T2D. All participants provided written informed consent, and this study was approved by the Simon Fraser University and Providence Health Care Research Ethics Boards.
Participants completed a treadmill test using the Bruce Protocol (Bruce et al., 1973). The test began at 1.7 mph and a 10% grade; the speed and grade were increased progressively until the participant reached volitional exhaustion. Prior to testing each participant, a gas calibration and volume calibration was completed using standard procedures. Heart rate was assessed by ECG throughout the test for safety purposes. Metabolic data were collected simultaneously during the treadmill test on a breath-by-breath basis using a calibrated metabolic system (VMax SensorMedics, Houston, Texas). VO2 was acquired as a 20-second average throughout the test. Participants were encouraged verbally throughout the test in an attempt to achieve a maximal effort. Those participants who reached volitional fatigue as well as either a respiratory exchange ratio of 1.05 at peak exercise or 85% of predicted maximal heart rate were considered to have achieved a VO2 peak. Eight of the 63 women who completed the treadmill test did not meet these criteria and were excluded from further analyses.
Abdominal fat was assessed through multi-slice computed tomography scanning with an initial image acquired at the L4–L5 interverterbral disk and four 10 mm slices taken every 5 cm above this landmark and two below this landmark. Scan parameters were set at 120kVp, 300 mA for one second, 10 mm thickness, 512 by 512 matrix using a 48 cm field of view. All seven CT slices were obtained at the same time. All scans were void of participant identity prior to assessment to avoid any interpretation bias. Using the standard attenuation range of − 190 to − 30 Hounsfield units for adipose tissue, the cross-sectional areas were determined using imaging software (SliceOmatic v4.2 Tomovision, Montreal, Quebec). Total abdominal adipose tissue (TAAT) was calculated as all pixels within this attenuation range in the abdominal image. VAT was calculated as all pixels in this attenuation range within the inner abdominal wall. Subcutaneuous abdominal adipose tissue (SAAT) was calculated as the difference between TAAT and VAT. Volumes were calculated as the average of the two closest scans divided by the distance between the scans. All areas were then added together for volume. Scan analyses were completed by the same individual, with a coefficient of variation based on repeat analysis of 1.21% at the L4–L5 scan.
Mass in kilograms and height in meters were assessed with participants in light clothing (or hospital gowns), footwear removed and pockets emptied. BMI was calculated as mass in kilograms over height in meters squared. WC was recorded in centimeters as the average of two measures taken against the skin at the point of maximal narrowing from the anterior view (midway between the top of the iliac crest and the bottom of the lowest rib) following a normal expiration. Body composition was assessed using a dual energy x ray absorptiometry (DXA) scanner (Hologic Discovery QDR 4500w, Bedford, Massachusetts) to determine lean body mass (kg), total body fat mass (kg), and percent body fat. The percentage of total body fat was calculated by dividing total body fat mass by total body mass.
Statistical analysis
The following data were natural log transformed following visual inspection of P–P plots: BMI, body mass, total body fat, body fat percentage, lean body mass, VAT, SAAT, TAAT, VO2 peak and time to exhaustion. Natural log transformed data are presented as geometric means with 95% confidence intervals while all remaining data are presented as means and standard deviations.
Next, Pearson correlations were used to assess the linear association between the dependent variable of VO2 peak, and the independent variables of WC, BMI, total body fat, body fat percentage, lean body mass, SAAT, VAT and TAAT. Participants were then categorized into tertiles of VO2 peak and separate ANOVAs were used to assess differences in each independent variable between tertiles of VO2 peak, with post hoc comparisons using the Bonferonni correction.
Finally, linear regression analyses were used to model the association between abdominal fat—SAAT, VAT and TAAT—and VO2 peak (mL/kg/min). Separate multiple linear regression models were constructed with, SAAT, VAT and TAAT as the predictor variables of interest and VO2 peak as the outcome variable. For each predictor, models were first adjusted for age and then separately for BMI and body fat percentage to examine these relationships independent of body size. BMI and body fat percentage were assessed for collinearity and it was not significant. Statistical analysis was completed using SPSS v. 19.0 and significance was set at p < 0.05.
Results
There were 55 women who completed aerobic fitness testing with a mean age of 57 years. Women had a mean BMI of 29 kg/m2, WC of 93.1 cm and body fat percentage of 42.0%. The mean VO2 peak obtained was 23.1 mL/kg/min, with 92% of participants reaching their predicted maximal HR (220-age). The average respiratory exchange ratio (RER) was 1.07, with 72% of women surpassing an RER of 1.0. All of the women reported having reached volitional exhaustion (Table 1).
Table 1.
Descriptive data of study participants in the Greater Vancouver area from January to August 2014 for Anthropometrics and Cardiorespiratory Fitness Testing.
| Variable | n = 55 |
|---|---|
| Age (years) | 57 ± 6 |
| Body mass index (kg/m2) a | 29.0 (28.0, 30.0) |
| Waist circumference (cm) | 93.1 ± 9.3 |
| Body mass (kg) a | 68.1 (62.0, 74.7) |
| Total body fat (kg) a | 29.8 (28.3, 31.4) |
| Body fat (%) a | 42.0 (40.9, 43.1) |
| Lean body mass (kg) a | 39.0 (37.7, 40.3) |
| Visceral adipose tissue (cm3) a | 3023 (2730, 3344) |
| Subcutaneous abdominal adipose tissue (cm3) a | 8467 (7895, 9082) |
| Total abdominal adipose tissue (cm3) a | 11,591 (10,829, 12,419) |
| VO2 peak (mL/kg/min) a | 23.1 (22.1, 24.2) |
| VO2 peak (mL/kg lean mass/min) a | 65.1 (61.6, 68.9) |
| VO2 peak (L/min) a | 1.67 (1.61, 1.73) |
| Measured maximal HR (bpm) | 150 ± 18 |
| Percent of predicted maximal HR at test completion | 92.0 ± 10.7 |
| Maximal respiratory exchange ratio | 1.07 ± 0.11 |
| Time to exhaustion (min) a | 5.2 (4.8, 5.5) |
Data are presented as geometric mean and 95% confidence interval. Predicted maximal heart rate determined by 220-age.
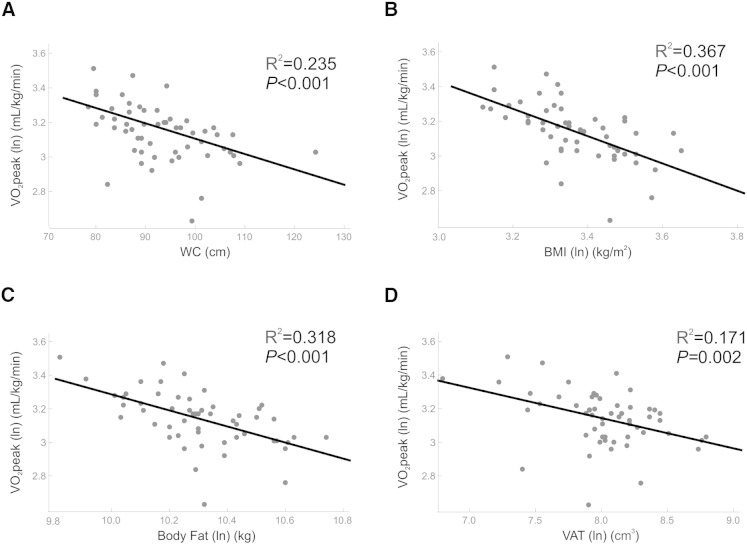
There were negative correlations between VO2 peak and lean body mass (r2 = 0.199, p < 0.001), SAAT (r2 = 0.299, p < 0.001), TAAT (r2 = 0.315, p < 0.001) and body fat percentage (r2 = 0.117, p = 0.011). Correlations between VO2 peak and WC, VAT, BMI and body fat are displayed in Fig. 1.
Fig. 1.
Pearson correlations between VO2 peak and selected body composition and abdominal fat variables.
VO2 peak: peak oxygen consumption, WC: waist circumference, BMI: body mass index, VAT: visceral adipose tissue.
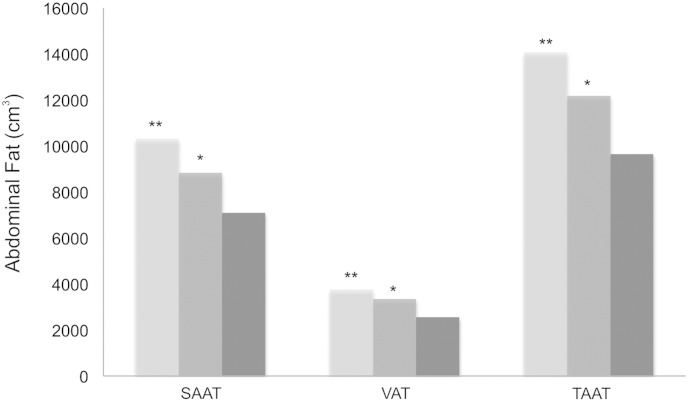
Compared to women in the lowest tertile of VO2 peak (13.8–21.8 mL/kg/min), women in the highest tertile (25.0–27.7 mL/kg/min) had significantly lower WC (p < 0.001), BMI (p < 0.001), total body fat (p < 0.001), body fat percentage (p = 0.004), and lean body mass (p = 0.017). Compared to women in the lowest tertile of VO2 peak, women in the middle tertile had significantly lower BMI (0.039) and women in the highest tertile compared to the middle tertile had significantly lower WC (P = 0.009), BMI (p = 0.002) and total body fat (p = 0.004). Compared to women in the lowest tertile of VO2 peak, women in the highest tertile had significantly lower inner-abdominal fat as measured by SAAT, VAT and TAAT compared to women in the highest tertile of VO2 peak (p < 0.001) (Fig. 2). Women in the highest tertile compared to the middle tertile had significantly lower inner-abdominal fat as measured by SAAT (p = 0.007), VAT (p = 0.002) and TAAT (p < 0.001) (Fig. 2).
Fig. 2.
Abdominal fat as assessed by tertiles of VO2 peak among participants in the Greater Vancouver area from January to August 2014.
Tertile 1 shown in light grey, tertile 2 in medium grey and tertile 3 in dark grey.
There was a significant difference in the amount of SAAT, VAT and TAAT between tertiles 1 and 3 (p < 0.001) as shown by * and between tertiles 2 and 3 (p < 0.01) as shown by **. SAAT: subcutaneous abdominal adipose tissue, VAT: visceral adipose tissue, TAAT: total abdominal adipose tissue
In linear regression analyses, all associations between VO2 peak and inner-abdominal fat variables (SAAT, VAT and TAAT) were significant after adjustment for age (Table 2).
Table 2.
Multiple linear regression analysis of the association between VO2 peak (dependent variable, mL/kg/min) and measures of inner-abdominal fat after adjustment for age, body fat percentage and BMI for entire cohort (n = 55) assessed in the Greater Vancouver area from January to August 2014.
| Abdominal adiposity | Standardized beta | P value |
|---|---|---|
| SAAT (cm3) * | ||
| Model 1: Adjusted for age only | − 0.549 | < 0.001 |
| Model 2: Adjusted for age and body fat percentage | − 0.552 | < 0.001 |
| Model 3: Adjusted for age and BMI | − 0.195 | 0.257 |
| VAT (cm3) * | ||
| Model 1: Adjusted for age only | − 0.410 | 0.002 |
| Model 2: Adjusted for age and body fat percentage | − 0.337 | 0.018 |
| Model 3: Adjusted for age and BMI | − 0.056 | 0.689 |
| TAAT (cm3) * | ||
| Model 1: Adjusted for age only | − 0.564 | < 0.001 |
| Model 2: Adjusted for age and body fat percentage | − 0.576 | < 0.001 |
| Model 3: Adjusted for age and BMI | − 0.209 | 0.254 |
Denoting variables that have been natural log transformed.
Associations between VO2 peak and inner-abdominal fat variables remained significant after adjustment for body fat percentage but were no longer significant after adjustment for BMI. When comparing the models with SAAT and the models with VAT, there were stronger associations for SAAT.
Discussion
In the current study of physically inactive post-menopausal South Asian women, we found VO2 peak was negatively associated with abdominal fat—SAAT, VAT and TAAT, as well as BMI, lean body mass, total body fat, body fat percentage and WC. Women in the highest tertile of VO2 peak had lower amounts of SAAT, VAT and TAAT as well as a lower body mass, WC, body fat and lean body mass than those in the lowest tertile of VO2 peak. Associations of VO2 peak with SAAT, VAT, and TAAT were independent of age and body fat percentage but not independent of age and BMI. Associations between VO2 peak and SAAT were somewhat stronger than associations between VO2 peak and VAT.
Our finding that CRF was negatively associated with SAAT, VAT and TAAT in physically inactive post-menopausal South Asian women is consistent with Janssen and Haufe who found men and women of European and African American origin with the highest CRF to have the lowest VAT (Haufe et al., 2010, Janssen et al., 2004). The results of our regression models suggest that SAAT may have a stronger relationship with VO2 peak than VAT and that this relationship remains even after accounting for VAT in the model.
While associations between abdominal fat (VAT, SAAT and TAAT) and VO2 peak were observed when adjusting for percent body fat, they were no longer apparent after adjusting for BMI. This is likely due to our observation of an inverse association between lean body mass and VO2 peak (i.e., women in our study in the lowest tertile of VO2 peak had the highest amount of lean body mass). Increased lean mass can be a result of additional body mass due to heightened load bearing requirements (Forbes and Welle, 1983) and may only be apparent when individuals are physically inactive as lighter individuals who engage in physical activity would increase their lean mass through the training effects of exercise. This finding is in contradiction to our other observations where those in the lowest tertile of VO2 peak had a body composition generally associated with more deleterious health; higher abdominal and body fat. In contrast to our findings in postmenopausal South Asian women, European men had higher lean body mass among those with the highest CRF (Arsenault et al., 2007). This may explain, at least in part, why the association between CRF and abdominal fat was independent of BMI in previous studies but not replicated in the current study (Arsenault et al., 2007, Haufe et al., 2010, Janssen et al., 2004).
We also found individuals in the highest tertile of VO2 peak to have lower SAAT, VAT and TAAT than those in the lowest and middle tertiles. Significantly lower amounts of VAT among those with a higher level of CRF have previously been found in both men (O'Donovan et al., 2009) and women (Brock et al., 2011) but not specifically in women of South Asian ethnicity, as measurement of CRF levels in the South Asian population is rare. It is unknown whether low levels of CRF may be causal to the unique obesity phenotype observed in the South Asian population of high VAT independent of BMI (Lear et al., 2007). Given the low CRF in the South Asian population (Hall et al., 2010), it is possible that there exists a genetic predisposition to lower CRF. Individuals who are predisposed to lower CRF through genetic heritability are more likely to show dysregulation in insulin, mitochondrial deficiencies and lipid oxidation (Bouchard et al., 2011). Interestingly, lipid oxidation has been shown to be lower during exercise in South Asian men compared to European men despite no differences observed at rest (Hall et al., 2010). This suggests that there may be an ethnic-specific response to exercise in regards to fat mobilization that may explain the link between CRF and body composition. This may be further supported by the observation that South Asian men need to undertake a higher level of physical activity to achieve the same level of cardio-metabolic risk as European men (266 min/week for the former compared to 150 min/week for the latter) (Celis-Morales et al., 2013) as lipid oxidation is associated with insulin sensitivity (Hall et al., 2010).
It has been well established that exercise is effective at reducing VAT in men and women of European origin (Arner, 1995, Mourier et al., 1997, O'Leary et al., 2006, Ross et al., 2004, Short et al., 2003). Exercise may preferentially target abdominal fat as VAT has an increased responsiveness to adrenergic activation (Arner, 1995) resulting in greater mobilization of triglycerides from this anatomical location. Women in our study were physically inactive and therefore we cannot draw the conclusion that lower VAT among those with higher CRF was due to an exercise training response; instead, lower VAT among those with higher CRF may have been due to genetic heritability. Further research is necessary to determine if exercise has a similar response on VAT in South Asian women, as previously seen in European populations.
We purposely targeted post-menopausal South Asian women as they have increased cardiovascular risk. This is important to note as menopause is associated with an increase in adiposity, specifically in the VAT depot. This is likely due to increases in bioavailable testosterone (Janssen et al., 2015) as well as a reduction in CRF (Lynch et al., 2002). Our finding of a negative association between body composition and abdominal fat with VO2 peak is similar to what has been shown in premenopausal European women (Abdulnour et al., 2012) although further research in premenopausal South Asian women would be necessary for ethnic-specific conclusions to be drawn.
This study has certain limitations. We aimed to recruit physically inactive women, and we relied on self-report of physical activity during eligibility screening. While objectively measured physical activity may have been more accurate, it is more common to over report rather than under report physical activity levels (Cleland et al., 2014); thus we believe that our methods were suitable to recruit a physically inactive study population. Participants were encouraged to exercise to volitional exhaustion during the treadmill test, but personal comfort level may have dictated the termination of the test. However, the average respiratory exchange ratio was 1.07, indicating that participants were relying on anaerobic metabolism and therefore working at a high intensity. In addition, women were encouraged throughout the test to continue to exercise until they no longer could therefore reaching volitional exhaustion. This was a cross-sectional study design and therefore causation cannot be determined, however, given the novelty of this research area this research design is well justified. Finally, the sample size was relatively small, and therefore, further research on a larger population as well as a comparison to an active control group should be conducted to try to replicate the current findings.
This is to our knowledge the first study to directly measure CRF in postmenopausal South Asian women and to examine the relationships between CRF and a variety of measures of body composition and inner-abdominal fat. This is unique as there is a paucity of research on CRF and obesity focusing on South Asian women of this age. Higher levels of CRF were associated with lower BMI, WC, body fatness and abdominal fat (SAAT, VAT and TAAT). We found a negative relationship between VO2 peak and abdominal fat independent of age and body fatness but not BMI. Further research is needed to examine the effectiveness of exercise at altering body composition and specifically abdominal fat in post-menopausal South Asian women (and to examine the effectiveness of exercise at altering VO2 peak). This would provide support for the role of exercise in altering disease prevalence in a high risk South Asian population. In addition, it is necessary to determine if SAAT is reduced to a greater extent than VAT with exercise in a South Asian population due to the stronger association of SAAT with CRF. In conclusion, cardiorespiratory fitness is associated with body composition and specifically abdominal fat in post-menopausal South Asian women.
Conflict of interest statement
The authors declare that there are no conflicts of interests.
Acknowledgments
IAL is supported by the SANSAR Young Investigator Award. SAL holds the Pfizer/Heart and Stroke Foundation Chair in Cardiovascular Prevention Research at St. Paul's Hospital. This study was funded through a CIHR operating grant (31-711309).
References
- Abdulnour J., Doucet E., Brochu M. The effect of the menopausal transition on body composition and cardiometabolic risk factors: a Montreal–Ottawa new emerging team group study. Menopause. 2012;19(7):760–767. doi: 10.1097/gme.0b013e318240f6f3. (Jul) [DOI] [PubMed] [Google Scholar]
- Alberti K.G., Zimmet P., Shaw J., IDF Epidemiology Task Force Consensus Group The metabolic syndrome—a new worldwide definition. Lancet. 2005;366(9491):1059–1062. doi: 10.1016/S0140-6736(05)67402-8. (Sep 24-30) [DOI] [PubMed] [Google Scholar]
- Anand S.S., Yusuf S., Vuksan V. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic Groups (SHARE) Lancet. 2000;356(9226):279–284. doi: 10.1016/s0140-6736(00)02502-2. (Jul 22) [DOI] [PubMed] [Google Scholar]
- Arner P. Impact of exercise on adipose tissue metabolism in humans. Int. J. Obes. Relat. Metab. Disord. 1995;19(Suppl. 4):S18–S21. (Oct) [PubMed] [Google Scholar]
- Arsenault B.J., Lachance D., Lemieux I. Visceral adipose tissue accumulation, cardiorespiratory fitness, and features of the metabolic syndrome. Arch. Intern. Med. 2007;167(14):1518–1525. doi: 10.1001/archinte.167.14.1518. (Jul 23) [DOI] [PubMed] [Google Scholar]
- Bouchard C., Rankinen T., Timmons J.A. Genomics and genetics in the biology of adaptation to exercise. J. Comp. Physiol. 2011;1(3):1603–1648. doi: 10.1002/cphy.c100059. (Jul) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brock D.W., Irving B.A., Gower B., Hunter G.R. Differences emerge in visceral adipose tissue accumulation after selection for innate cardiovascular fitness. Int. J. Obes. 2011;35(2):309–312. doi: 10.1038/ijo.2010.133. (Feb) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce R.A., Kusumi F., Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am. Heart J. 1973;85(4):546–562. doi: 10.1016/0002-8703(73)90502-4. (Apr) [DOI] [PubMed] [Google Scholar]
- Celis-Morales C.A., Ghouri N., Bailey M.E., Sattar N., Gill J.M. Should physical activity recommendations be ethnicity-specific? Evidence from a cross-sectional study of South Asian and European men. PLoS One. 2013;8(12) doi: 10.1371/journal.pone.0082568. (Dec 11) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleland C.L., Hunter R.F., Kee F., Cupples M.E., Sallis J.F., Tully M.A. Validity of the global physical activity questionnaire (GPAQ) in assessing levels and change in moderate–vigorous physical activity and sedentary behaviour. BMC Public Health. 2014;14(1) doi: 10.1186/1471-2458-14-1255. (Dec 10) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes G.B., Welle S.L. Lean body mass in obesity. Int. J. Obes. 1983;7(2):99–107. [PubMed] [Google Scholar]
- Garduno-Diaz S.D., Khokhar S. Prevalence, risk factors and complications associated with type 2 diabetes in migrant South Asians. Diabetes Metab. Res. Rev. 2012;28(1):6–24. doi: 10.1002/dmrr.1219. [DOI] [PubMed] [Google Scholar]
- Gholap N., Davies M., Patel K., Sattar N., Khunti K. Type 2 diabetes and cardiovascular disease in South Asians. Prim. Care Diabetes. 2011;5(1):45–56. doi: 10.1016/j.pcd.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Ghouri N., Purves D., McConnachie A., Wilson J., Gill J.M., Sattar N. Lower cardiorespiratory fitness contributes to increased insulin resistance and fasting glycaemia in middle-aged South Asian compared with European men living in the UK. Diabetologia. 2013;56(10):2238–2249. doi: 10.1007/s00125-013-2969-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill J.M., Celis-Morales C.A., Ghouri N. Physical activity, ethnicity and cardio-metabolic health: does one size fit all? Atherosclerosis. 2014;232(2):319–333. doi: 10.1016/j.atherosclerosis.2013.11.039. [DOI] [PubMed] [Google Scholar]
- Hall L.M.L., Moran C.N., Milne G.R. Fat oxidation, fitness and skeletal muscle expression of oxidative/lipid metabolism genes in South Asians: implications for insulin resistance? PLoS One. 2010;5(12) doi: 10.1371/journal.pone.0014197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haufe S., Engeli S., Budziarek P. Cardiorespiratory fitness and insulin sensitivity in overweight or obese subjects may be linked through intrahepatic lipid content. Diabetes. 2010;59(7):1640–1647. doi: 10.2337/db09-1200. (Jul) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen I., Katzmarzyk P.T., Ross R. Fitness alters the associations of BMI and waist circumference with total and abdominal fat. Obes. Res. 2004;12(3):525–537. doi: 10.1038/oby.2004.60. (Mar) [DOI] [PubMed] [Google Scholar]
- Janssen I., Powell L.H., Jasielec M.S., Kazlauskaite R. Covariation of change in bioavailable testosterone and adiposity in midlife women. Obesity (Silver Spring) 2015;23(2):488–494. doi: 10.1002/oby.20974. (Feb) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi P., Islam S., Pais P. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297(3):286–294. doi: 10.1001/jama.297.3.286. (Jan 17) [DOI] [PubMed] [Google Scholar]
- Lean M.E., Han T.S., Bush H., Anderson A.S., Bradby H., Williams R. Ethnic differences in anthropometric and lifestyle measures related to coronary heart disease risk between South Asian, Italian and general-population British women living in the west of Scotland. Int. J. Obes. Relat. Metab. Disord. 2001;25(12):1800–1805. doi: 10.1038/sj.ijo.0801823. (Dec) [DOI] [PubMed] [Google Scholar]
- Lear S.A., Chockalingam A., Kohli S., Richardson C.G., Humphries K.H. Elevation in cardiovascular disease risk in South Asians is mediated by differences in visceral adipose tissue. Obesity (Silver Spring) 2012;20(6):1293–1300. doi: 10.1038/oby.2011.395. (Jan 26) [DOI] [PubMed] [Google Scholar]
- Lear S.A., Humphries K.H., Kohli S., Chockalingam A., Frohlich J.J., Birmingham C.L. Visceral adipose tissue accumulation differs according to ethnic background: results of the multicultural community health assessment trial (M-CHAT) Am. J. Clin. Nutr. 2007;86(2):353–359. doi: 10.1093/ajcn/86.2.353. (Aug) [DOI] [PubMed] [Google Scholar]
- Lynch N.A., Ryan A.S., Berman D.M., Sorkin J.D., Nicklas B.J. Comparison of VO2max and disease risk factors between perimenopausal and postmenopausal women. Menopause. 2002;9(6):456–462. doi: 10.1097/00042192-200211000-00012. (Nov-Dec) [DOI] [PubMed] [Google Scholar]
- Mather H.M., Chaturvedi N., Fuller J.H. Mortality and morbidity from diabetes in south Asians and Europeans: 11-year follow-up of the Southall Diabetes Survey, London, UK. Diabet. Med. 1998;15(1):53–59. doi: 10.1002/(SICI)1096-9136(199801)15:1<53::AID-DIA521>3.0.CO;2-V. (Jan) [DOI] [PubMed] [Google Scholar]
- Misra A., Khurana L. Obesity-related non-communicable diseases: South Asians vs White Caucasians. Int. J. Obes. 2011;35(2):167–187. doi: 10.1038/ijo.2010.135. (Feb) [DOI] [PubMed] [Google Scholar]
- Mourier A., Gautier J.F., De Kerviler E. Mobilization of visceral adipose tissue related to the improvement in insulin sensitivity in response to physical training in NIDDM. effects of branched-chain amino acid supplements. Diabetes Care. 1997;20(3):385–391. doi: 10.2337/diacare.20.3.385. (Mar) [DOI] [PubMed] [Google Scholar]
- O'Donovan G., Thomas E.L., McCarthy J.P. Fat distribution in men of different waist girth, fitness level and exercise habit. Int. J. Obes. 2009;33(12):1356–1362. doi: 10.1038/ijo.2009.189. (Dec) [DOI] [PubMed] [Google Scholar]
- O'Leary V.B., Marchetti C.M., Krishnan R.K., Stetzer B.P., Gonzalez F., Kirwan J.P. Exercise-induced reversal of insulin resistance in obese elderly is associated with reduced visceral fat. J. Appl. Physiol. 2006;100(5):1584–1589. doi: 10.1152/japplphysiol.01336.2005. (May) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosano G.M., Vitale C., Marazzi G., Volterrani M. Menopause and cardiovascular disease: the evidence. Climacteric. 2007;10(Suppl. 1):19–24. doi: 10.1080/13697130601114917. (Feb) [DOI] [PubMed] [Google Scholar]
- Ross R., Janssen I., Dawson J. Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obes. Res. 2004;12(5):789–798. doi: 10.1038/oby.2004.95. (May) [DOI] [PubMed] [Google Scholar]
- Short K.R., Vittone J.L., Bigelow M.L. Impact of aerobic exercise training on age-related changes in insulin sensitivity and muscle oxidative capacity. Diabetes. 2003;52(8):1888–1896. doi: 10.2337/diabetes.52.8.1888. (Aug) [DOI] [PubMed] [Google Scholar]
- Yusuf S., Reddy S., Ounpuu S., Anand S. Global burden of cardiovascular diseases: Part I: General considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104(22):2746–2753. doi: 10.1161/hc4601.099487. (Nov 27) [DOI] [PubMed] [Google Scholar]