Abstract
Objective
Research suggests that schools can play a key role in obesity prevention by implementing evidence-based strategies promoting student health. This study explores school climate factors underlying implementation of evidence-based health and wellness policies and practices in Kindergarten–8th grade programs in the Southwestern United States.
Method
Utilizing a participatory research survey approach conducted in December 2011 with school health professionals (N = 62) and a multiple regression design, a moderated predictive model of implementation climate (i.e., attitudes and beliefs about prevention, school commitment to prevention, barriers, and stakeholder collaboration) was tested.
Results
Barriers to obesity prevention efforts, such as lack of resources, support, or strategy clarity, hinder implementation of healthy food policies despite strong school commitment to prevention. Along with the commitment to prevention, stakeholder collaboration predicts physical education strategies, specifically reducing restricted access to physical education as a punishment for student misconduct.
Conclusion
Obesity prevention strategy implementation relies on the supportiveness and structure of school climates. Barriers to prevention can impede efforts despite school commitment toward prevention, while stakeholder collaboration can enhance the likelihood that practices are in place.
Keywords: Pediatric obesity, School health services, Prevention and control, Health services research, Program evaluation
Highlights
-
•
This study explored school implementation climate for obesity prevention.
-
•
Barriers are associated with lower implementation of healthy food policies.
-
•
Commitment and collaboration predict less restricted access to physical education.
-
•
School prevention beliefs predict lower student access to physical education.
-
•
Obesity prevention implementation depends on the supportiveness of school climates.
Introduction
Nationally, obesity is a growing concern with nearly two-thirds of adults overweight or obese (Centers for Disease Control and Prevention, 2012).3 Youth obesity rates are especially alarming with almost one-third of youth ages 10 to 17 overweight or obese (Centers for Disease Control and Prevention National Center for Health Statistics, 2013, Whitaker et al., 1997). Although rates in several states have fallen slightly among certain children (Centers for Disease Control and Prevention, 2013), obesity continues to disproportionately affect Hispanic and Black youth (39.9% and 41.6%, respectively) and youth under the federal poverty level (44.7%). Consequently, being overweight or obese is associated with significant health problems, such as type-2 diabetes and hypertension, which are estimated to cost between $147 billion and $210 billion per year for adults nationally. Childhood obesity is responsible for upwards of $14 billion in direct costs nationally (Trasande and Chatterjee, 2009, Trust for America's Health, Robert Wood Johnson Foundation, 2012).
School consequences of obesity and obesity-related conditions include decreased mental acuity due to poor nutrition, behavioral health concerns, and peer victimization (Griffiths et al., 2006). Furthermore, being overweight or obese is associated with school absenteeism and indicators of achievement, including lower grade point averages, standardized test scores, and perceived academic performance (Geier et al., 2007, Taras and Potts-Datema, 2005). Considering schools have a significant role in providing youth with daily meals and physical activity opportunities, and that poor nutrition and obesity have the potential to negatively impact academic performance, schools are optimal settings for the implementation of obesity prevention efforts (Agron et al., 2010).
There is broad agreement that evidence-based environmental strategies (i.e., policies and systemic practices) to support healthy eating and active living should be considered in schools in order to have a meaningful, wide-ranging impact on obesity rates (Brownson et al., 2006, McGraw et al., 2000, Story et al., 2009). Within schools, these approaches can include practices for improved student and staff health services through body mass index (BMI) screenings and education, access to healthy foods, food preparation and procurement standards, and physical education and recess policies (Centers for Disease Control and Prevention, 2011). Environmental strategies are intended to be more sustainable and affect a larger, more diverse range of people than individual-level approaches.
Several studies have supported school-based environmental strategies for childhood obesity prevention. For instance, policies that limit student access to foods and beverages that are high in fat and sugars are related to decreased consumption of these items during the school day (Kubik et al., 2003, Neumark-Sztainer et al., 2005, Woodard-Lopez et al., 2010). School-based efforts to increase physical activity have contributed to lowered body mass index (Brown and Sumerbell, 2009) and improved cognitive abilities (Hillman et al., 2014), especially in younger children. Additionally, integrating physical education within classrooms was positively associated with student performance, such as time-on-task and standardized test scores (Centers for Disease Control and Prevention, 2010). Furthermore, students from schools with comprehensive, coordinated health and nutrition initiatives were generally less overweight or obese, demonstrated healthier eating habits, and participated in more physical activity than those from schools without nutrition programming (Hoelscher et al., 2004, Veugelers and Fitzgerald, 2005). Finally, a recent review found robust effects for policies that set nutrition standards in improving student dietary behaviors (Jaime and Lock, 2009). Despite some promising findings for school obesity prevention, more work needs to be done in evaluating the climate of implementation in schools in order to promote these strategies. Specifically, researchers, practitioners, and policymakers must better understand the relationship(s) among micro- and macro-level organizational factors within schools that create an amenable climate for implementation (Taras and Potts-Datema, 2005), in which obesity prevention strategies can be effectively introduced.
Research has shown that the success of prevention strategies is reliant on the supportiveness of the climate of implementation (Fixsen et al., 2005, Matthews et al., 2006, Totura et al., 2010). Successful implementation is defined as strategic action taken to achieve an intended outcome (Brynard, 2009). Assessment of implementation climate is essential to school obesity prevention efforts in order to gauge effective levels of adoption, fidelity, and success (McGraw et al., 2000). Multiple elements illustrate the climate for strategy implementation, including attitudes and beliefs about the strategy, clarity and adaptability of strategy goals and operations, resource allocation, and strategy alignment with existing practices and the needs of those intended to benefit (Brynard, 2009, Fixsen et al., 2005, O'Toole, 1986, Panzano et al., 2007). Schools differ in their implementation capacity, suggesting that the success of obesity prevention is dependent on drivers such as attitudes and beliefs about prevention, school-level commitment, collaboration with individuals who have a stake in school programming, and reduction of barriers (Agron et al., 2010, Giacchino and Kakabadse, 2003).
Among these drivers, research consensus suggests that organizational commitment and collaboration with stakeholders, especially frontline implementers, are central factors to successful prevention work (Brynard, 2009, Cho and Nadow, 2004, Aarons et al., 2014, Rodriguez et al., 2014). Commitment (schools expressing motivation and desire beyond strict mandate for strategy assimilation and sustainability within typical operations) is the lynchpin to implementation and it is most effective following collaboration, or meaningful commitment to and participation in strategy decision-making, with stakeholders within the school (i.e., health professionals, teachers, other school staff) who are essential to putting an effort in place and seeing it through (Fixsen et al., 2005, Panzano et al., 2007).
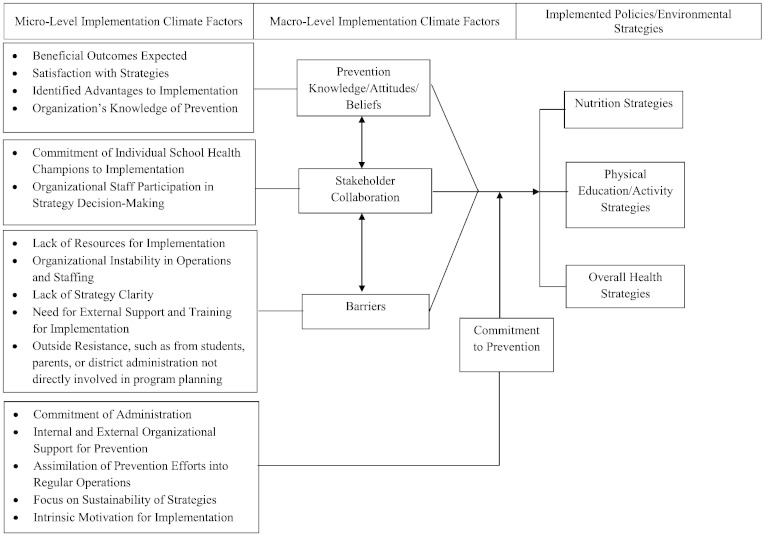
This study tests a research-supported conceptual model of school implementation climate (Fig. 1) in order to identify the factors that are important in predicting whether health, nutritional, and physical activity promotion strategies are in place in elementary and middle schools. Consistent with leading research on obesity prevention in schools (Kubik et al., 2007, Stang et al., 1997, Story, 1999), policy implementation was assessed via the perspective of school nurses and health professionals. Research suggests that school commitment, stakeholder collaboration, and barriers are the strongest predictors of implementation success (Brynard, 2009). This study clarifies the mechanism by which these factors may influence school obesity prevention strategy implementation. Schools with higher levels of commitment to prevention, supportive attitudes and beliefs about the benefits of prevention, collaboration among key staff, and fewer barriers to implementation were hypothesized to have more environmental policies and practices in place. As past research suggests that organizational commitment is the cornerstone of effective implementation, it was hypothesized that commitment would moderate the associations of prevention attitudes and beliefs, collaboration, and barriers in either promoting or hindering the likelihood that strategies were in place.
Fig. 1.
Conceptual model of school-based obesity prevention policy and practice implementation.
Materials and methods
Participants and procedures
Health professionals (N = 62) representing 12% of public elementary/middle schools and 29.4% of districts within a targeted Southwestern county completed an anonymous and confidential online survey administered via a state department of education listserv.4 The survey's instructions described its purpose, that is was voluntary, and restricted responses to participants' primary school affiliation. Represented schools were identified as public (95.2%) with free/reduced lunch rates between 26% and 92%. Data were collected over a two-week period in December 2011. University Institutional Review Board approval was secured for this study.
Measures
The 149-item online School Health Survey, designed by researchers and county public health and education professionals as part of a county-funded needs assessment of obesity prevention initiatives and informed by previous school-based prevention studies (Centers for Disease Control and Prevention, 2011, Totura et al., 2010), included open-ended and scaled response questions assessing knowledge of policies/practices (e.g., has this policy or practice been implemented in your school?), and the climate of implementation. Responses to the knowledge of policies item checklist (1 = knowledge; 0 = no knowledge) were summed across strategy areas to create a frequency/breadth of implementation score. Items were aggregated into broad policy categories based on results from factor and reliability analyses (Table 1). Implementation was conceptualized as the respondents' ready knowledge about strategies across multiple policy categories. Higher knowledge scores were conceptualized to indicate greater awareness and broader implementation of recommended strategies. Items assessing implementation climate (e.g., school is mandated to offer obesity prevention; administrators have been very supportive of prevention; lack of resources for prevention) were measured on 7-point scales (1 = strongly disagree/no extent to 7 = strongly agree/very great extent). Per previous evaluations (i.e., Totura et al., 2010) and reliability analyses, these items were aggregated into narrow micro-level implementation climate factor mean scores (in parentheses), which were then further aggregated into four broad macro-level factor mean scores: 1) attitudes and beliefs toward prevention (α = .81; satisfaction with strategies, beneficial outcomes expected, advantages to implementation, organization's prevention knowledge), 2) commitment to prevention (α = .81; internal and external organizational support for prevention, sustainability of strategies, intrinsic motivation for strategy implementation, commitment of administration to prevention, and assimilation of prevention into regular school operations), 3) stakeholder collaboration (α = .75; commitment of individual school health professionals to implementation, staff participation in strategy decision-making), and 4) barriers (α = .67; lack of strategy clarity, outside resistance to prevention, organizational instability in staffing and operations, need for external support for implementation, need for formal training for implementation).
Table 1.
Policy and environmental prevention strategy categories, items, and implementation rates (% with policy).
| Policy/strategy category | Category content | Category items | % with policy | Mean sum of strategy frequency (standard deviation) | Scale range |
|---|---|---|---|---|---|
| Food service practices (α = .70) | Procurement and preparation standards for meals and snacks | This school has a food procurement policy in place that sets/follows nutrition standards for school meals and snacks | 66.1% | 1.85 (0.25) | 0–2 |
| Food service staff follow practices for healthy preparation of school meals | 75.8% | ||||
| Physical education (PE) policies (α = .82) | Regulations around the time requirements and standards for physical education | This school follows national and/or state physical education guidelines and standards | 85.5% | 3.83 (0.65) | 0–4 |
| Students at this school regularly participate in physical activity | 95.2% | ||||
| This school offers regular physical education | 95.2% | ||||
| This school has specified time requirements for PE | 91.9% | ||||
| Teachers at this school sometimes exclude students from PE as punishment for bad behaviora, b | 17.8% | ||||
| Healthy food policies (α = .73) | Formal or informal policies on access to healthy food options (and discouragement of unhealthy options) | This school has a formal or informal policy or practice requiring or recommending that fruits and vegetables be made available to students whenever food is sold | 66.1% | 4.78 (1.58) | 0–7 |
| This school has a formal or informal policy or practice requiring or recommending that healthful beverages be made available to students whenever beverages are offered or sold | 71% | ||||
| This school has a formal or informal policy or practice requiring or recommending junk foods be prohibited in school settings | 43.5% | ||||
| This school has a formal or informal policy or practice prohibiting advertising for candy, fast food, or soft drinks on school property | 21% | ||||
| Staff at this school prohibit or discourage use of food or food coupons as rewards for student behavior and/or performance | 38.7% | ||||
| This school provides information to students on the impact of health on school performance | 58.1% | ||||
| This school provides information in the cafeteria and other food service locations on nutrition education | 51.6% | ||||
| Restrictions on access to competitive foods (α = .70) | Restrictive policies and practices for unhealthy competitive foods (i.e., vending, fundraising, school store sales) | This school has a formal or informal policy or practice restricting times when certain beverages can be sold in school venues | 38.7% | 1.93 (1.19) | 0–4 |
| This school has a formal or informal policy or practice restricting times when junk foods can be sold in school venues | 41.9% | ||||
| This school has a formal or informal policy or practice restricting times when students can access vending machines | 35.5% | ||||
| This school offers healthy options in vending machines | 14.5% | ||||
| Recess policies (α = .70) | Regular access to recess | This school provides regularly scheduled recess after student lunch periods | 56.5% | 1.12 (0.77) | 0–2 |
| Teachers at this school sometimes exclude students from recess as punishment for bad behaviorb | 67.7% | ||||
| Student health services (α = .68) | Coordinated health services for students (i.e., body mass index screening, health counseling, school health centers) | This school provides nutrition and dietary behavior counseling | 16.1% | 0.85 (0.94) | 0–3 |
| This school provides physical activity and fitness counseling | 19.4% | ||||
| This school provides student services for health conditions related to nutrition or weight management | 37.1% | ||||
| Staff development practices (α = .84) | Initiatives targeted at improving staff health and nutrition | This school offers professional development for staff in nutrition and dietary behavior | 29% | 0.92 (1.16) | 0–3 |
| The school offers professional development for staff in physical activity and fitness | 29% | ||||
| The school offers professional development for staff in weight management | 22.6% |
This item was not included in the PE policy category sum due to lower resulting internal consistency when combined with the rest of the PE items.
These items were reverse coded in analyses.
Statistical analysis
Multiple regression and slope analyses were conducted to assess the probability of prevention strategy implementation as a function of the hypothesized implementation climate predictors and moderators (Hellevik, 2009, Holmbeck, 2002). Missing data were addressed using multiple imputation. Two sets of regression models were run: 1) predicting the probability of broad strategy category implementation (i.e., healthy food policies) by macro-level implementation factors, and 2) predicting implementation probability of individual strategies, rather than broad strategy categories, by macro-level implementation factors. Estimates from statistically significant models were interpreted. Slope analyses explored the role of school commitment to prevention as a moderator by testing its interaction with each macro-level implementation factor. Regression estimates were calculated at high (+ 1 standard deviation, SD, above mean) and low (− 1 SD) conditions for both commitment and each of the macro-level implementation factors combined with commitment. Bivariate correlations were conducted between micro-level implementation factors and strategy implementation rates.
Results
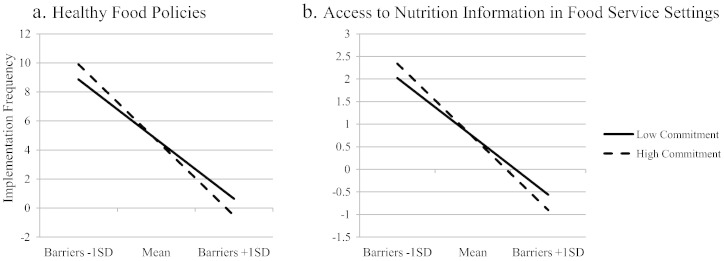
Table 1 indicates that implementation rates varied across strategy categories and specific policies. Regression estimates (see Table 2, Table 3 for strategy category estimates) suggested that when more barriers to implementation were in place, the likelihood of having healthy food policies decreased (β = − 2.95; p = .03; 95% CI [− 20.08, − 1.08]), particularly providing nutritional information in food service settings (F(7, 54) = 2.49, p = .03; β = − 3.76, p = .008; 95% CI [− 5.71, − 0.91]). The interaction of commitment and barriers was significant for both broad implementation of healthy food policies (p = .03; 95% CI [0.28, 4.39]) and specific access to nutritional information (β = 5.02, p = .008; 95% CI [0.19, 1.23]), suggesting that commitment to prevention serves as a moderator to implementation for these policy areas. According to the slope analyses (see Fig. 2), with fewer barriers (− 1 SD), higher commitment (+ 1 SD) correlated with greater implementation of these policies.
Table 2.
Regression estimates between macro-level implementation factors and broad school health, nutritional, and physical education prevention categories.
| M | SD | Physical Ed policies |
Healthy food policies |
Staff development practices |
Restricted access to competitive foods |
Student health services |
Food service practices |
Recess policies |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | CIa | β | CI | β | CI | β | CI | β | CI | β | CI | β | CI | |||
| Attitudes & Beliefs | 5.04 | 0.60 | − 0.74 | − 4.35, 2.74 | − 0.12 | − 7.62, 7.00 | − 0.10 | − 6.33, 5.96 | − 0.10 | − 6.51, 6.12 | 1.98 | − 1.23, 7.48 | 1.24 | − 0.61, 1.63 | 0.96 | − 2.82, 5.31 |
| Commitment to Prevention | 4.53 | 0.53 | − 0.65 | − 5.22, 3.64 | − 3.57⁎ | − 19.81, − 1.53 | − 1.82 | − 11.69, 3.68 | 1.33 | − 4.91, 10.88 | − 1.13 | − 7.56, 3.43 | 2.06 | − 0.44, 2.36 | − 2.05 | − 8.09, 2.07 |
| Stakeholder Collaboration | 5.37 | 0.78 | 0.67 | − 1.94, 3.06 | 0.19 | − 4.77, 5.55 | 0.38 | − 3.77, 4.91 | − 0.12 | − 4.64, 4.27 | − 1.04 | − 4.33, 1.82 | − 0.46 | − 0.94, 0.65 | − 0.82 | − 3.69, 2.05 |
| Barriers | 3.52 | 0.44 | − 0.33 | − 5.09, 4.11 | − 2.95⁎ | − 20.08, − 1.08 | − 1.30 | − 11.42, 4.54 | 1.37 | − 4.50, 11.91 | − 1.07 | − 7.95, 3.36 | 1.66 | − 0.53, 2.39 | − 1.67 | − 8.23, 2.33 |
| Attitudes & Beliefs X Commitment to Prevention | 23.08 | 4.39 | 1.28 | − 0.58, 0.96 | 1.03 | − 1.22, 1.96 | 0.64 | − 1.17, 1.51 | − 0.13 | − 1.41, 1.34 | − 2.63 | − 1.51, 0.38 | − 1.63 | − 0.34, 0.15 | − 1.12 | − 1.08, 0.69 |
| Stakeholder Collaboration X Commitment to Prevention | 24.60 | 4.87 | − 0.98 | − 0.69, 0.43 | 0.15 | − 1.11, 1.21 | − 0.21 | − 1.02, 0.92 | 0.37 | − 0.91, 1.09 | 2.35 | − 0.23, 1.15 | 0.70 | − 0.14, 0.21 | 1.30 | − 0.44, 0.85 |
| Barriers X Commitment to Prevention | 15.95 | 2.73 | 0.53 | − 0.87, 1.12 | 4.04⁎ | 0.28, 4.39 | 1.89 | − 0.92, 2.54 | − 1.81 | − 2.56, 0.99 | 0.88 | − 0.92, 1.53 | − 1.97 | − 0.49, 0.14 | 2.29 | − 0.49, 1.79 |
| Model Fit | F(7,54) = 0.10 | F(7,54) = 3.11⁎⁎ | F(7,54) = 0.65 | F(7,54) = 0.52 | F(7,54) = 3.21⁎⁎ | F(7, 54) = 3.48⁎⁎ | F(7,54) = 0.75 | |||||||||
Study conducted in Southwestern U.S. in Dec. 2011. Each macro-level implementation factor was included simultaneously in each regression model predicting policy categories. Each of the individual policy categories was used as a dependent variable in separate regression models.
p < .05.
p < .01.
CI = 95% confidence interval for non-standardized regression coefficients.
Table 3.
Pearson's correlation coefficients between micro-level implementation factors and broad school health, nutritional, and physical education prevention categories.
| M | SD | Physical Ed policies | Healthy food policies | Staff development practices | Restricted access to competitive foods | Student health services | Food service practices | Recess policies | |
|---|---|---|---|---|---|---|---|---|---|
| Attitudes & beliefs about prevention | |||||||||
| Satisfaction with strategies | 4.64 | 0.64 | 0.03 | 0.22 | 0.01 | − 0.09 | − 0.08 | 0.47⁎⁎ | − 0.04 |
| Beneficial outcomes expected | 4.71 | 0.82 | − 0.09 | 0.34⁎⁎ | 0.12 | 0.08 | 0.11 | 0.42⁎⁎ | 0.01 |
| Advantages to Implementation | 5.82 | 0.90 | − 0.11 | 0.21 | 0.04 | 0.07 | − 0.06 | 0.39⁎⁎ | − 0.10 |
| Organization's prevention knowledge | 5.50 | 0.80 | − 0.002 | 0.24⁎ | 0.16 | 0.08 | − 0.03 | 0.16 | − 0.07 |
| Commitment to prevention | |||||||||
| Internal organizational support | 4.59 | 0.80 | − 0.07 | 0.27⁎ | 0.14 | 0.04 | − 0.10 | 0.35⁎ | − 0.15 |
| External organizational support | 3.98 | 0.53 | 0.16 | 0.12 | 0.02 | 0.08 | 0.14 | 0.05 | − 0.16 |
| Sustainability of strategies | 4.95 | 0.86 | − 0.10 | 0.29⁎⁎ | 0.09 | 0.02 | − 0.06 | 0.35⁎⁎ | 0.02 |
| Intrinsic motivation for implementation | 5.04 | 0.61 | − 0.19 | 0.11 | − 0.05 | 0.07 | − 0.19 | 0.23⁎ | − 0.004 |
| Commitment of administration to prevention | 4.54 | 0.97 | − 0.04 | 0.32⁎⁎ | 0.10 | 0.12 | − 0.002 | 0.28⁎ | − 0.16 |
| Assimilation of prevention into regular school operations | 2.63 | 1.06 | 0.08 | 0.07 | − 0.07 | 0.08 | 0.03 | 0.01 | − .11 |
| Stakeholder collaboration | |||||||||
| Commitment of individual school health professionals to implementation | 5.88 | 0.85 | − 0.10 | 0.25⁎ | 0.04 | 0.14 | − 0.01 | 0.33⁎⁎ | − 0.12 |
| Staff participation in strategy decision-making | 3.84 | 1.12 | 0.01 | 0.15 | 0.22 | 0.10 | 0.22 | 0.15 | 0.03 |
| Barriers | |||||||||
| Lack of strategy clarity | 4.01 | 0.90 | − 0.05 | 0.06 | 0.20 | 0.08 | − 0.13 | − .001 | 0.05 |
| Outside resistance to prevention | 3.01 | 0.50 | 0.06 | 0.06 | 0.26⁎ | − 0.12 | − 0.15 | 0.16 | 0.03 |
| Organizational instability in staffing and operations | 3.41 | 0.70 | − 0.06 | 0.02 | 0.06 | 0.04 | − 0.14 | 0.06 | 0.07 |
| Need for external support | 4.15 | 0.97 | 0.12 | − 0.15 | − 0.20 | 0.24⁎ | − 0.19 | − 0.06 | 0.11 |
| Need for formal training | 5.70 | 1.30 | − 0.20 | − 0.20 | − 0.26 | 0.03 | − 0.65⁎⁎ | − 0.02 | − 0.16 |
Study conducted in Southwestern U.S. in Dec. 2011.
p < .05.
p < .01.
Fig. 2.
Slope analysis of the relationship between frequency of healthy food policy implementation and access to nutrition information and barriers at high and low levels of school commitment to prevention; Southwestern U.S. Dec. 2011.
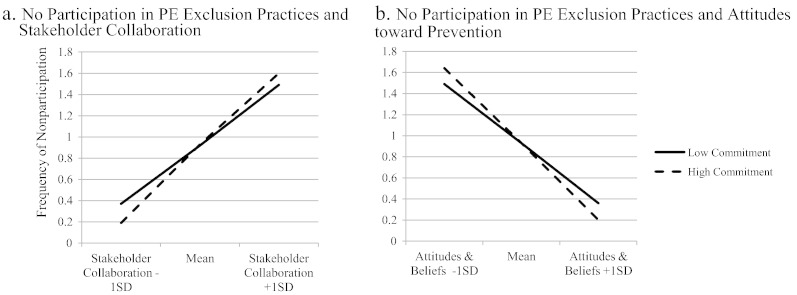
While none of the macro-level implementation factors predicted implementation of PE policies more broadly, school commitment to prevention did have a moderating effect on PE exclusion. Teachers were less likely to exclude students from PE for misbehavior with greater levels of staff collaboration (F(7, 54) = 2.81, p = .01; β = 2.93, p = .03; 95% CI [0.10, 1.57]), particularly when coupled with higher levels of commitment to prevention (β = − 4.79, p = .01; 95% CI [− 0.38, − 0.05]) as indicated by implementation variations at high and low levels of commitment and collaboration (Fig. 3). Surprisingly, school attitudes supportive of prevention were correlated with more PE exclusion (β = − 2.91, p = .04; 95% CI [− 2.12, − 0.04]), especially at higher levels of commitment to prevention (β = 4.90, p = .03; 95% CI [0.02, 0.47]).
Fig. 3.
Slope analysis of the relationship between nonparticipation in physical education (PE) exclusion practices and stakeholder collaboration and attitudes toward obesity prevention at high and low levels of school commitment to prevention; Southwestern U.S. Dec. 2011.
Both implementation of healthy food policies and food service practices were significantly and positively correlated with multiple micro-level implementation factors, particularly beneficial outcomes expected, advantages to implementation, internal organizational support for prevention, sustainability of strategies, commitment of administration to prevention, and commitment of individual school health professionals to implementation (see Table 3).
Discussion
This study found that organizational factors dictate implementation climate for school-based policies and environmental strategies to prevent childhood obesity. To the authors' knowledge, this is the first empirical study testing models of implementation for a comprehensive array of environmental obesity prevention strategies in schools. Common barriers, such as lack of a clear obesity prevention strategy, resistance from stakeholders, and need for significant training and external supports, decreased the likelihood that strategies would be in place, especially those related to increasing access to healthy foods and nutritional education information. Regardless of a school's commitment toward obesity prevention, this study finds that having institutional barriers in place is correlated with limited implementation of prevention strategies. However, commitment to prevention becomes more important as barriers are reduced.
Coupled with the support of individual champions and stakeholders within the school, commitment predicted nonparticipation in physical education exclusion as punishment for misbehavior, a practice at odds with recommended obesity prevention practices. On the contrary, when paired with supportive attitudes and beliefs about perceived advantages of obesity prevention for schools and students, commitment to prevention was associated with increased likelihood that exclusion from PE would be used as a consequence for student misbehavior. This may be evidence of a mismatch between teacher expectations around school-based obesity prevention and expectations for effectively managing student behavior in an academic environment, even in school contexts where there appear to be beliefs supportive of prevention in general. Previous research suggests that excluding students from PE may not be an uncommon practice even in schools that support physical activity; students may be excluded from physical activity in favor of other school activities up to 25% of the time (Young et al., 2007). This finding underscores the importance of agreement between policy planners and frontline implementers on the nature of student challenges and the relevancy of prevention strategies (Milio, 1988).
Several explanations may account for the findings in the present study. The implementation of healthy food policies and the availability of nutrition education information may be more sensitive to identified barriers in schools, particularly lack of coordination among implementers. When stakeholders, such as food service staff, health educators, and teachers, have limited opportunity to communicate about prevention strategies, they are less likely to coordinate efforts to promote school-wide nutrition programming and healthy food policies (Cho and Nadow, 2004). Recent research has confirmed the importance of understanding environmental factors on youth consumption behaviors, especially situational food norms among influential stakeholders in the school context (De la Hayne et al., 2013). Furthermore, schools committed to prevention and more knowledgeable about what it takes for prevention efforts to be successful may better identify legitimate barriers to effective implementation related to specific strategies, such as those guiding access to healthy food options or for developing comprehensive school-wide student health services. Therefore, regardless of commitment, identification of barriers perceived as difficult to overcome will impede implementation of certain strategies.
Study limitations and strengths
The present results should be considered in light of some potential limitations. Implementation climate was assessed as support for obesity prevention in general, while the frequency of prevention efforts was assessed by strategies that were not specifically labeled obesity prevention, but are nonetheless indicative of obesity prevention per recommendations by the Centers for Disease Control and Prevention (2011). Perhaps participants did not necessarily view the strategies they reported on as recommended childhood obesity prevention efforts, while having alternate perspectives for what constitutes effective and beneficial obesity-related prevention activities in schools, especially given current school priorities. That the sample of participants constituted primarily school nurses who might serve more than one school may have limited the available knowledge of strategy implementation. Consequently, associations between strategy implementation and beliefs about prevention may have been limited. Although school nurses are considered main champions of obesity prevention in schools (Kubik et al., 2007), this study was necessarily restricted to policy assessment via self-report of their knowledge rather than through a multi-method and multi-informant approach. Future studies of implementation climate should incorporate additional key informants and data collection methods to provide a more definitive assessment of the policy landscape. Information was also collected from a modestly sized sample which may have reduced the ability to find expected significant effects. Moreover, the number of statistical tests conducted may have resulted in spurious findings contributing to some of the counterintuitive relationships observed. These relationships necessitate further investigation.
Further, data collection did not include degree or timeline of implementation, so it is not certain which stage of implementation schools were in when each identified strategy was assessed. Implementation was defined by the number of policies or practices, with greater implementation indicated as simply having more strategies in place. This definition constricts the conceptualization of implementation “success” to the frequency of policies or practices without indicating the degree or stage of implementation for each policy. What cannot be determined is whether schools may have many superficially implemented strategies, or a few key strategies that are very well implemented. Without knowing which implementation stage each school is in for each obesity prevention strategy and the motivations behind adopting initiatives, it is hard to understand the exact implications of organizational commitment and stakeholder collaboration. Considering these limitations, this study design allowed for one of the first empirical assessments of implementation factors for a comprehensive range of evidence-based environmental strategies in a countywide school sample.
Conclusions
Organizations move through several stages of change in order to accept and execute a prevention strategy, namely development, implementation, and monitoring (Rohrbach et al., 2006). Previous research found perceived lags in organizational capacity depending on which stage of implementation is addressed (Agron et al., 2010). Additional work is needed to examine acceptance of obesity prevention across various implementation stages and levels of school capacity. Despite positive beliefs about the value of obesity prevention, capacity concerns may lead school staff to engage in practices contrary to evidence-based strategies. Teachers often have multiple, disparate demands and consequently classroom management and prevention practices may not always align well (Agron et al., 2010). For instance, recommended prevention policies such as restricting “junk” foods sold during meals and for fundraising, may run counter to the perceived financial risk among schools of restricting these sales. Interestingly, research indicates that this perceived risk is unfounded (Wharton et al., 2008). Further research is needed to thoroughly assess expectations surrounding obesity prevention among school personnel, students, and parents in order to align recommended policies with what is perceived as feasible in the school environment (Bradley and Greene, 2013, Centers for Disease Control and Prevention, 2011).
Findings from the present study suggest that while school commitment to obesity prevention is important, commitment level alone is not a reliable predictor of strategy implementation in schools. Many policies and practices are implemented by either state or federal regulation, leaving little room at the local level for input and meaningful collaboration on strategic planning or adaptability (Matland, 1995; USDA Food and Nutrition Service, 2004). While stakeholder collaboration is highly valued, having it does not automatically imply successful implementation (Brynard, 2009). The more complex or large in scope a strategy is, the more critical collaboration is. Additionally, leadership must endorse resource allocation and training of implementers in order to guarantee that a strategy can be adopted and sustained. Contrariwise, less complex efforts may not require a great degree of collaboration to have effective implementation (Lundin, 2007).
The parameters of individual obesity prevention policies and environmental strategies must be comprehensively evaluated in order to determine their alignment with the existing characteristics of school environments. Without considering organizational readiness and stage of implementation, strategies that stem from good intentions and awareness may stall once champions of the efforts leave or school priorities shift. Thorough assessment of school compliance with policies and practices will help to ascertain whether they will be effective, impactful, and sustainable. This is a place for future research and practice.
Conflict of interest statement
The authors have no conflicts of interest to declare. This research was supported by funding from the Maricopa County Department of Public Health (MCDPH), PH RFP 11-016. The sponsors were not involved in study design, data collection, data analysis and interpretation, manuscript preparation, or the decision to submit the manuscript for publication.
Acknowledgments
The authors would like to thank the Maricopa County Department of Public Health, the Arizona Department of Education, and participating school health professionals for making this study possible. Additionally, we are grateful to Wendy Wolfersteig, Ph.D. and the evaluation associates with the Southwest Interdisciplinary Research Center (SIRC) for their expert input on this study.
Footnotes
Among adults, obesity is defined as a body mass index (BMI) over 30.0 and overweight is a BMI between 25.0 and 29.9.
The listserv consisted of approximately 140 local professionals belonging to the National School Nurses Association, resulting in a response rate of 44.3%. Survey instructions requested the participation of only those professionals affiliated with schools in the target county.
Contributor Information
Christine M.W. Totura, Email: christine.totura@auburn.edu.
Holly Lewis Figueroa, Email: Holly.T.Lewis@asu.edu.
Christopher Wharton, Email: Christopher.Wharton@asu.edu.
Flavio F. Marsiglia, Email: Marsiglia@asu.edu.
References
- Aarons G.A. Collaboration, negotiation, and coalescence for interagency-collaborative teams to scale-up evidence-based practice. J. Clin. Child Adolesc. Psychol. 2014;43(6):915–928. doi: 10.1080/15374416.2013.876642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agron P., Berends V., Ellis K., Gonzalez M. School wellness policies: perceptions barriers, and needs among leaders and wellness advocates. J. Sch. Health. 2010;80:527–535. doi: 10.1111/j.1746-1561.2010.00538.x. [DOI] [PubMed] [Google Scholar]
- Bradley B.J., Greene A.C. Do health and education agencies in the United States share responsibility for academic achievement and health? A review of 25 years of evidence about the relationship of adolescents' academic achievement and health behaviors. J. Adolesc. Health. 2013;52:523–532. doi: 10.1016/j.jadohealth.2013.01.008. [DOI] [PubMed] [Google Scholar]
- Brown T., Sumerbell C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: a update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obes. Rev. 2009;10:110–141. doi: 10.1111/j.1467-789X.2008.00515.x. [DOI] [PubMed] [Google Scholar]
- Brownson R.C., Haire-Joshu D., Luke D.A. Shaping the context of health: a review of environmental and policy approaches in the prevention of chronic diseases. Annu. Rev. Public Health. 2006;27:341–370. doi: 10.1146/annurev.publhealth.27.021405.102137. [DOI] [PubMed] [Google Scholar]
- Brynard P.A. Mapping the factors that influence policy implementation. J. Public Adm. 2009;44:557–577. [Google Scholar]
- Centers for Disease Control and Prevention . U.S. Department of Health and Human Services; Atlanta, GA: 2010. The Association Between School-based Physical Activity, Including Physical Education, and Academic Performance. [Google Scholar]
- Centers for Disease Control and Prevention School health guidelines to promote healthy eating and physical activity. Morb. Mortal. Wkly Rep. 2011;60:1–76. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . Behavioral Risk Factor Surveillance System. 2012. Prevalence and trends data: nationwide (states and DC) — 2012 overweight and obesity (BMI) ([Online] Available at: http://apps.nccd.cdc.gov/brfss [Accessed 19 August 2013]) [Google Scholar]
- Centers for Disease Control and Prevention Vital signs: obesity among low-income, preschool-aged children — United States, 2008–2011. Morb. Mortal. Wkly Rep. 2013;62:629–634. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention National Center for Health Statistics . 2013. State and local area integrated telephone survey, National Survey of Children's Health 2011–2012. ([Online] Available at: http://www.cdc.gov/nchs/slaits/nsch.htm [Accessed 11 June 2013]) [Google Scholar]
- Cho H., Nadow M.Z. Understanding barriers to implementing quality lunch and nutrition education. J. Community Health. 2004;29:421–435. doi: 10.1023/b:johe.0000038656.32950.45. [DOI] [PubMed] [Google Scholar]
- De la Hayne K., Robins G., Mohr P., Wilson C. Adolescents' intake of junk food: processes and mechanisms driving consumption similarities among friends. J. Res. Adolesc. 2013;23:524–536. [Google Scholar]
- Fixsen D.L. University of South Florida, Louis de la Parte Florida Mental Health Institute, National Implementation Research Network; Tampa, FL: 2005. Implementation Research: A Synthesis of the Literature. [Google Scholar]
- Geier A.B. The relationship between relative weight and school attendance among elementary school children. Obes. 2007;15:2157–2161. doi: 10.1038/oby.2007.256. [DOI] [PubMed] [Google Scholar]
- Giacchino S., Kakabadse A. Successful policy implementation: the route to building self-confident government. Int. Rev. Adm. Sci. 2003;69:139–160. [Google Scholar]
- Griffiths L.J., Wolke D., Page A.S., Horwood J.P. Obesity and bullying: different effects for boys and girls. Arch. Dis. Child. 2006;91:121–125. doi: 10.1136/adc.2005.072314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellevik O. Linear versus logistic regression when the dependent variable is a dichotomy. Qual. Quant. 2009;43:59–74. [Google Scholar]
- Hillman C.H. Effects of the FITKids randomized controlled trial on executive control and brain function. Pediatrics. 2014 doi: 10.1542/peds.2013-3219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoelscher D.M. School-based health education programs can be maintained over time: results from the CATCH Institutionalization study. Prev. Med. 2004;38(5):594–606. doi: 10.1016/j.ypmed.2003.11.017. [DOI] [PubMed] [Google Scholar]
- Holmbeck G.N. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. J. Pediatr. Psychol. 2002;27(1):87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Jaime P.C., Lock K. Do school based food and nutrition policies improve diet and reduce obesity? Prev. Med. 2009;48:45–53. doi: 10.1016/j.ypmed.2008.10.018. [DOI] [PubMed] [Google Scholar]
- Kubik M.Y., Story M., Davey C. Obesity prevention in schools: current role and future practice of school nurses. Prev. Med. 2007;44:504–507. doi: 10.1016/j.ypmed.2007.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubik M.Y. The association of the school food environmet with dietary behaviors of young adolescents. Am. J. Public Health. 2003;93:1168–1173. doi: 10.2105/ajph.93.7.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundin M. When does cooperation improve public policy implementation? Policy Stud J. 2007;35:629–652. [Google Scholar]
- Matland R.E. Synthesizing the implementation literature: the ambiguity-conflict model of policy implementation. J. Public Adm. Res. Theory. 1995;5:145–174. [Google Scholar]
- Matthews C., Boon H., Flisher A.J., Schaalma H.P. Factors associated with teachers' implementation of HIV/AIDS education in secondary schools in Cape Town South Africa. AIDS Care. 2006;18:388–397. doi: 10.1080/09540120500498203. [DOI] [PubMed] [Google Scholar]
- McGraw S.A. Measuring implementation of school programs and policies to promote healthy eating and physical activity among youth. Prev. Med. 2000;31:S86–S97. [Google Scholar]
- Milio N. Making healthy public policy: developing the science by learning the art: an ecological framework for policy studies. Health Promot. 1988;2:263–274. doi: 10.1093/heapro/2.3.263. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D. School lunch and snacking patterns among high school students: associations with school food environment and policies. Int. J. Behav. Nutr. Phys. Act. 2005;2:1–7. doi: 10.1186/1479-5868-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Toole L. Recommendations for multi-factor implementation: an assessment of the field. J. Public Policy. 1986;6:181–210. [Google Scholar]
- Panzano P.C., Fixsen D., Naoom S. University of South Florida, Louis de la Parte Florida Mental Health Institute, National Implementation Research Network; Tampa, FL: 2007. Climate for Implementation Model. [Google Scholar]
- Rodriguez A., Southam-Gerow M.A., O'Connor M.K., Allin R.B. An analysis of stakeholder views on children's mental health services. J. Clin. Child Adolesc. Psychol. 2014;43:862–876. doi: 10.1080/15374416.2013.873982. [DOI] [PubMed] [Google Scholar]
- Rohrbach L.A., Grana R., Sussman S., Valente T.W. Type II translation: transporting prevention interventions from research to real-world settings. Eval. Health Prof. 2006;29:302–333. doi: 10.1177/0163278706290408. [DOI] [PubMed] [Google Scholar]
- Stang J.S., Story M., Kalina B. School-based weight management services: perceptions and practices of school nurses and administrators. Am. J. Health Promot. 1997;11:183–185. doi: 10.4278/0890-1171-11.3.183. [DOI] [PubMed] [Google Scholar]
- Story M. School-based approaches for preventing and treating obesity. Int. J. Obes. 1999;23:S43–S51. doi: 10.1038/sj.ijo.0800859. [DOI] [PubMed] [Google Scholar]
- Story M., Nanney M.S., Schwartz M.B. Schools and obesity prevention: creating school environments and policies to promote healthy eating and physical activity. Milbank Q. 2009;87:71–100. doi: 10.1111/j.1468-0009.2009.00548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taras H., Potts-Datema W. Obesity and student performance at school. J. Sch. Health. 2005;75:291–295. doi: 10.1111/j.1746-1561.2005.00040.x. [DOI] [PubMed] [Google Scholar]
- Totura C.M. Paper Presented at the 43rd Annual Conference for the American Association of Suicidology, Orlando, FL. 2010. Why some succeed and others fail: the effects of organizational climate, training engagement, and perceived attitudes and intentions on the implementation and effectiveness or gatekeeper suicide prevention training. [Google Scholar]
- Trasande L., Chatterjee S. The impact of obesity on health service utilization and costs in childhood. Obes. 2009;17:1749–1754. doi: 10.1038/oby.2009.67. [DOI] [PubMed] [Google Scholar]
- Trust for America's Health, Robert Wood Johnson Foundation F as in fat: how obesity threatens America's future. 2012. http://www.fasinfat.org/files/fasinfat2012.pdf [Online] Available at. ([Accessed 20 March 2013])
- Food U.S.D.A., Nutrition Service The Child Nutrition and Women Infants and Children (WIC) Reauthorization Act of 2004 (Sec. 204 of P.L. 108–205) 2004. http://www.fns.usda.gov/tn/healthy/108-265.pdf [Online] Available at. ([Accessed 12 July 2013])
- Veugelers P.J., Fitzgerald A.L. Effectiveness of school programs in preventing childhood obesity: a multilevel comparison. Am. J. Public Health. 2005;95:432–435. doi: 10.2105/AJPH.2004.045898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wharton C.M., Long M., Schwartz M.B. Changing nutrition standards in schools: the emerging impact on school revenue. J. Sch. Health. 2008;78:245–251. doi: 10.1111/j.1746-1561.2008.00296.x. [DOI] [PubMed] [Google Scholar]
- Whitaker R.C. Predicting obesity in young adulthood from childhood and parental obesity. N. Engl. J. Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- Woodard-Lopez G. Lessons learned from evaluations of California's state nutrition standards. Am. J. Public Health. 2010;100(11):2137–2145. doi: 10.2105/AJPH.2010.193490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young D.R. Policies and opportunities for physical activity in middle school environments. J. Sch. Health. 2007;77:41–47. doi: 10.1111/j.1746-1561.2007.00161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]