Abstract
In older adults the relationships between health, fall-related risk factors, perceived neighborhood walkability, walking behavior and intervention impacts are poorly understood.
To determine whether: i) health and fall-related risk factors were associated with perceptions of neighborhood walkability; ii) perceived environmental attributes, and fall-related risk factors predicted change in walking behavior at 12 months; and iii) perceived environmental attributes and fall-related risk factors moderated the effect of a self-paced walking program on walking behavior.
Randomized trial on walking and falls conducted between 2009 and 2012 involving 315 community-dwelling inactive adults ≥ 65 years living in Sydney, Australia. Measures were: mobility status, fall history, injurious fall and fear of falling (i.e., fall-related risk factors), health status, walking self-efficacy and 11 items from the neighborhood walkability scale and planned walking ≥ 150 min/week at 12 months.
Participants with poorer mobility, fear of falling, and poor health perceived their surroundings as less walkable. Walking at 12 months was significantly greater in “less greenery” (AOR = 3.3, 95% CI: 1.11–9.98) and “high traffic” (AOR = 1.98, 95% CI: 1.00–3.91) neighborhoods. The intervention had greater effects in neighborhoods perceived to have poorer pedestrian infrastructure (p for interaction = 0.036).
Low perceived walkability was shaped by health status and did not appear to be a barrier to walking behavior. There appears to be a greater impact of, and thus, need for, interventions to encourage walking in environments perceived not to have supportive walking infrastructure. Future studies on built environments and walking should gather information on fall-related risk factors to better understand how these characteristics interact.
Keywords: Walking, Fall, Neighborhood, Walkability, Older adults, Randomized controlled trial
Highlights
-
•
In older adults the associations between walkability attributes and walking are inconsistent.
-
•
We examined if perceived walkability, fear and risk of falling predicted walking at 12-months.
-
•
Seniors at risk and fear of falling perceived their neighborhoods as less walkable.
-
•
Risk and fear of falling did not appear to be a barrier to increase walking.
-
•
The intervention had greater effects in neighborhoods perceived to have poorer pedestrian infrastructure.
Introduction
Over the past decade extensive research has been dedicated to the relationship between the built environment and walking (Sallis et al., 2012, Harris et al., 2013). Relatively consistent associations between certain perceived and objectively measured neighborhood attributes (e.g., residential density, mixed land use, and perceived esthetics, and distance to destinations) and walking have been reported for children, adolescents and young and middle-aged adults (Ding et al., 2011, Saelens and Handy, 2008).
However, according to systematic reviews (van Cauwenberg et al., 2011, Hanson et al., 2012), in older populations (> 60 years) the relationships between the same environmental attributes and walking have been inconsistent. A major limitation of the evidence accumulated to date is the preponderance of cross-sectional designs (van Cauwenberg et al., 2011), which cannot investigate causality. Only three out of the 31 publications reviewed by van Cauwenberg et al. (2011) were longitudinal observational studies and their findings were inconsistent (Li et al., 2005, Lee et al., 2009, Michael et al., 2010).
Randomized controlled trials (RCTs) that aim to increase physical activity among individuals can potentially afford new insights on the role of neighborhood attributes for several reasons. First, RCTs are longitudinal in nature and can identify neighborhood attributes at baseline which predict a change in walking duration, after accounting for the intervention effect. Second, the randomization process ensures a balanced distribution of walkability features between groups. Third, data from RCTs can be analyzed to determine whether the response to the intervention is moderated by attributes of participants' neighborhoods. To date, three RCTs involving older adults have examined environmental influences on physical activity. In a walking group intervention, perceived neighborhood problems (e.g., safety) attenuated the 6 months decline in walking observed in non-intervention communities (Michael et al., 2010). On the other hand, contrary to expectations, one RCT reported that older women (50–75 years) who lived in neighborhoods with high mixed land use were the least active at the end of a 6-month intervention (Sallis et al., 2007). Another RCT found that the effects of a lifestyle intervention for overweight men were apparent only for those in low walkable environments (Kerr et al., 2010). None of these studies considered the participants' mobility status or their fear or risk of falling, factors that could affect their perceptions of their environment and thus may have confounded associations. Furthermore, given that objectively measured mixed land use was found to moderate functional disabilities in old age (Clarke and George, 2005), it is possible that other features of the perceived environment would impact differentially on older adults' walking levels according to falls-related risk factors.
The present study is therefore aimed to determine whether: 1) health status and fall-related risk factors, specifically mobility status, fall history and fear of falling, were associated with perceptions of walkability; 2) perceived environmental attributes and fall-related risk factors predicted change in walking behavior at 12 months; and 3) environmental perceptions, fall history and fear of falling moderated the intervention effect on walking behavior.
Methods
Participants were community dwelling older adults (≥ 65 years) who enrolled in the “Easy Steps to Health” RCT that evaluated the effect of a home-based self-paced walking program on falls (primary outcome), walking and physical activity (secondary outcomes). The study protocol (Voukelatos et al., 2011) and main outcomes (Voukelatos et al., 2015) have been published elsewhere. The walking program did not significantly reduce falls (IRR = 0.88, 95% CI: 0.60–1.29) in the intervention group compared to the control group, but significantly increased walking and physical activity (median change 1.69 vs. 0.75 h/week, Cohen's D = 0.52) (Voukelatos et al., 2015). The study was registered prior to commencement (ACTRN12610000380099), approved by the Research Ethics Review Committee of the Sydney South West Area Health Service, Eastern Zone (X08-0279 & HREC/08/RPAH/477) and all participants gave informed consent.
Participants were recruited through community advertisements and letters to those on the electoral roll of the state of New South Wales. Potential participants had a short telephone screening interview to determine eligibility. To be eligible, participants needed to be ≥ 65 years of age, physically inactive (< 120 min/week), able to walk 50 m unaided, without medical issues that precluded regular physical activity, and without cognitive impairment (< 7 on the Short Portable Mental Status Questionnaire) (Pfeiffer, 1975) and be able to read and speak English. Randomization to intervention and control arms (n = 386) took place after the baseline interviews.
Intervention
Participants in the intervention group received a sequential mailing of three manuals adapted from the Step-by-Step 3-month program (Merom et al., 2009) (sent at weeks 0, 12 and 24), a pedometer, and seven telephone coaching sessions, at weeks 1, 3, 6, 12, 16, 24, and 36. The first manual (1–12 weeks) focused on accumulating walking time through a gradual increase of frequent short walks and the duration of walking according to the participant's ability. The second manual (weeks 13–24) focused on increasing walking intensity to a brisk pace. The third manual (weeks 25–48) was the maintenance phase and focused on strategies to maintain the level of health-enhancing walking (2.5 h/week) and strategies to manage setbacks and relapses. All guides included several environment-related tips such as safe conditions for walking, how to plan longer walking routes, and more. Participants were asked to record all walks and any falls experienced on a calendar that was mailed, monthly, to the research center in pre-paid envelopes.
Control group participants were requested not to change their physical activity habits during the study. They received health information on mental wellbeing, healthy eating and developing good sleeping habits, at the same time the intervention group participants received their walking manuals. They also received seven telephone calls in parallel to the intervention group, asking whether they received the education information. Control group participants were also required to record any falls they had on a calendar.
Perceived neighborhood walkability and walking outcomes
Perceived environmental attributes were measured with 11 items from the Australian version of the Neighborhood Environment Walkability Scale (NEWS-AU) (Cerin et al., 2008) (see Table 1 for item details). Responses to each item were measured with 4-point scales (strongly disagree = 1, somewhat disagree = 2, somewhat agree = 3, and strongly agree = 4). The NEWS-AU items were used as categorical variables computed in three ways. The 11 items were first summed (possible range 11–44) and dichotomized at the lowest quartile indicating “low walkability” (items 5, 9, and 11 were reversed to match a phrasing of high walkability). Second, the effect of each attribute on walking levels was examined by collapsing the responses “strongly disagree” and “somewhat disagree” to form a single attribute to denote an unsupportive/supportive condition for walking. Last, we summed four walkability items into a previously identified ‘pedestrian-oriented designs’ subscale (Cervero and Kockelman, 1997). Items included many places to go within easy walking distance, easy to walk to public transport, sidewalks on most streets, and existence of crosswalks and pedestrian crossing signals. This gave a score between 4–16, which was dichotomized at the bottom quartile. These items had high internal consistency (Cronbach's alpha = 0.71).
Table 1.
Participants' demographic, health, and psychological attributes and neighborhood walkability, Sydney, Australia.
| All participants (n = 315) |
Control group (n = 170) |
Walking group (n = 145) |
p-Value | |
|---|---|---|---|---|
| Male (%) | 26.9 | 26.5 | 27.6 | 0.824 |
| Age ≥ 75 yearsa | 35.4 | 33.7 | 37.2 | 0.521 |
| Non-English speaking background (%) | 5.1 | 5.9 | 4.1 | 0.482 |
| Still employed (%)b | 14.4 | 16.5 | 12.0 | 0.260 |
| Post high-school education (%)b | 36.9 | 37.0 | 36.6 | 0.991 |
| Living alone (%) | 42.0 | 41.8 | 42.2 | 0.952 |
| Mobility status (walking before needing a rest) < 30 min (%) | 37.1 | 37.6 | 63.4 | 0.841 |
| Self-rated health (%) | ||||
| – Excellent or very good | 48.0 | 44.1 | 52.4 | |
| – Good | 40.6 | 44.7 | 35.9 | 0.068 |
| – Fair or poor | 11.4 | 11.2 | 11.7 | |
| Falls history (past 12 months)c | ||||
| – At least one fall (%) | 23.1 | 23.0 | 23.2 | 0.978 |
| – Recurrent fallers (%) | 11.3 | 13.2 | 9.0 | 0.241 |
| – Had injurious fall | 7.0 | 5.9 | 8.3 | 0.414 |
| Self-rating of risk of falling | ||||
| Moderate or high (%) | 29.4 | 33.5 | 25.1 | 0.071 |
| Fear of falling, score (16 items)c | ||||
| – Mean (SD) score out of 64d | 20.4 (4.7) | 21.1 (5.0) | 20.4 (4.2) | 0.257 |
| Fear of fallingc | ||||
| – High concern (% upper quartile) | 25.7 | 26.5 | 24.8 | 0.520 |
| Efficacy for duration of brisk walk | ||||
| Confident/very confident walking 30 min briskly | 32.0 | 28.2 | 36.5 | 0.115 |
| Neighborhood walkability e | ||||
| – Low (% lower tertile < 36 points) | 31.9 | 33.7 | 29.7 | 0.440 |
| Pedestrian-oriented neighborhoode | ||||
| – Low (% lower quartile < 13 points) | 27.6 | 27.6 | 27.6 | 0.990 |
| % strongly disagree or disagreed to statement e | ||||
| 1. Many places to go within easy walking distance | 26.4 | 28.8 | 23.4 | 0.280 |
| 2. It is easy to walk to a public transport stop | 10.5 | 10.6 | 10.3 | 0.944 |
| 3. There are footpaths on most of the streets | 18.4 | 17.6 | 19.3 | 0.704 |
| 4. There are crosswalks and pedestrian signals | 23.5 | 22.3 | 24.8 | 0.606 |
| 5. The streets in my neighborhood are not hilly | 13.0 | 15.3 | 10.3 | 0.193 |
| 6. Walkers in my neighborhood can be easily seen | 18.7 | 19.4 | 17.9 | 0.737 |
| 7. There is lots of greenery around my local area | 7.3 | 9.4 | 4.8 | 0.119 |
| 8. There are many interesting things to look at | 11.7 | 12.9 | 10.3 | 0.476 |
| 9. There is not much traffic along nearby streets | 22.5 | 26.5 | 17.9 | 0.071 |
| 10. My local areas has … parks, walking trails | 14.0 | 13.5 | 14.5 | 0.808 |
| 11. Crime rate in my neighborhood is not a problem | 8.0 | 8.2 | 7.6 | 0.832 |
Due to 7 missing date of birth % from n = 308.
Due to 3 missing % of n = 312.
Due to 5 missing on number of falls and FOF n = 310.
The lower the score the better.
Due to one missing neighborhood score and % were calculated from n = 314.
Planned walking (i.e., for exercise and recreation) and incidental walking (to get to places) in the past 7 days were measured with two separate questions from the Incidental and Planned Exercise Questionnaire (IPEQ), specifically developed for older adults (Delbaere et al., 2010). Participants were asked about the number of days and total time spent per day on these walks. Answers were close-coded in defined intervals of frequency (i.e., 0 days, 1–2 days a week) and duration (i.e. < 15 min/day, 15–29 min). Time spent on planned walking (hours/week) was calculated by multiplying the median values of the frequency and duration categories. The criterion validity of these questions combined was fair (Spearman's rho = 0.35) (Merom et al., 2014). A categorical measure of ‘regular walking’ was defined as meeting the physical activity guidelines for older adults (i.e., ≥ 2.5 h/ week) (Nelson et al., 2007).
Health and fall-related measures
Perceived health status was measured by the question “how would you rate your current level of health for someone your age (excellent/very good/good/fair/poor?)” (Richardson et al., 2004). Responses were dichotomized to fair/poor, or above. Low mobility was defined as less than 15 min before a rest is needed, based on the question “On an average day, how long can you walk before you need a rest?” Walking self-efficacy was measured by participants' rating of “how confident are you that you can walk on at least three days per week continuously at a brisk pace for 10, 20, 30, 40, 50, and 60 min” (Nagel et al., 2008).
Fall history was assessed by questions of “How many times did you fall in the past 12 months?”, and “Did you have any injuries as a result of any of these falls?” The confidence in one's ability to not fall, defined here as fear of falling (FOF), was assessed using the short form of the Falls Efficacy Scale-International (FES-I), which is a 16-item questionnaire that has acceptable reliability and construct validity (Kempen et al., 2007). The degree of concern was measured on a scale from 1 to 4 with 1 being “not at all concerned” and 4 being “very concerned”. We calculated the overall score by summing responses over the 16 items and dichotomized the score at the highest quartile, indicating concern. We also calculated separate scores for concern of falling in indoor (i.e., 7 items such as cleaning the house, getting in or out of a chair) and outdoor activities (i.e., 9 items, such as going up or downs stairs, walking in a place with crowds, walking on an uneven surface) The indoor and outdoor scores were dichotomized at the highest quartile, indicating concern.
Demographic information (age, gender, main language spoken at home, employment status, and living arrangement) was also collected at the baseline interview.
Statistical analysis
The associations between low perceived walkability (i.e., lowest tertile on the walkability scale) and self-rated health, mobility, walking self-efficacy, fall history and FOF were examined in bivariate analyses using baseline data. Generalized linear models (GLM) with binomial distribution were performed to identify significant predictors (longitudinal analysis) of ‘regular walking’ at follow-up (main effect models). The likelihood ratio statistics was used to eliminate non-significant variables, with a p-value set < 0.250 to allow for confounding. Finally, the modifying influence of FOF, recurrent falling (≥ 2 falls), unsupportive environments (i.e., lower tertile), and the subscale pedestrian-oriented design on the intervention outcome were tested using interaction terms in negative binomial regression models with the rate of falls as the outcome (main and interaction effects model). All models (including unadjusted) used 301 participants due to missing data on any covariates (see legend Table 1). Analyses were conducted with SAS version 9.3.
Results
The average age of study participants was 73.2 years (range: 65–90 years). Few participants were concerned about falling (Table 1) as indicated by the low mean score on the FES-I of 20.4 (maximum score was 64). As well, most study participants reported living in walkable neighborhoods with a mean score of 37 out of 44 (most walkable), the median was 38 and the lowest quartile value was 34. There were no significant differences in walkability measures between the control and intervention groups (Table 1) although there were marginal differences in the proportions who “strongly disagreed” or “disagreed” that the traffic in their neighborhoods makes it difficult to walk (26.0% vs. 17.9%, p = 0.085).
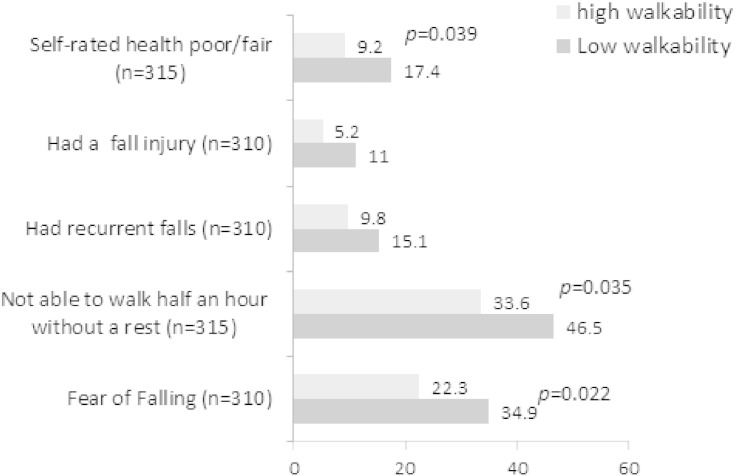
At baseline, there were significant positive associations between perceived low walkability and participants' poor health status, mobility status, falls and injury history and FOF (Fig. 1). For example, higher proportions of participants who perceived their health as poor, who were not able to walk 30 min without stopping, who fell or injured themselves before the intervention started, or who had low efficacy for brisk walking, were in the category of low walkability. FOF was negatively associated with neighborhood walkability; participants who had greater FOF perceived their neighborhoods to have lower walkability (Fig. 1). When examining the relationship between specific walkability attributes and sub-categories of FOF (data not shown), those having a greater concern of FOF indoors and FOF outdoors were more likely to have lower perceptions of destinations within short walking distance or ease of walking to public transport (p < 0.01) and the highest quartile of FOF outdoors was associated with a greater proportion perceiving “too much traffic that makes it difficult to walk” (p = 0.02).
Fig. 1.
Health status and fall-related risk factors by neighborhood walkability.
Predictors of regular walking: at 12 months, intervention participants were more than twice as likely to be regular walkers as the control participants (OR = 2.29, p < 0.01) (Table 2, 1st column). The lowest quartile of walkability at baseline (data not shown) had no significant effect on the proportion of ‘regular walking’ (OR = 0.88, p = 0.627) compared to the other quartiles for all participants. Examining each walkability attribute as a predictor of regular walking revealed that not having many places to go within easy walking distance nearly halved the likelihood of being a regular walker (OR = 0.55, p = 0.04), and, against expectations, low perceived greenery in the local area was associated with more than doubling the odds of regular walking (OR = 2.45, p = 0.04). Fair or poor self-rated health at baseline was significantly associated with decreased likelihood of regular walking (OR = 0.37, p < 0.01) and baseline self-efficacy for walking briskly at least 30 min was associated with a higher likelihood for regular walking.
Table 2.
Predictors of ‘regular walking’ at 12-month in the ‘Easy Step to Health’ randomized controlled trial: generalized linear models (n = 301).
| Regular walking |
Regular walking |
|
|---|---|---|
| Unadjusted modela |
Adjusted model b |
|
| OR (95% CI)c | OR (95% CI)c | |
| Main Effects models | ||
| Intervention (ref = control) | 2.29 (1.38; 3.81) | 2.57 (1.46; 4.54) |
| Recurrent fallers (ref = No) | 1.29 (0.61; 2.76) | 2.71 (1.10; 6.63) |
| Self-rated health fair& poor (ref = No) | 0.37 (0.14; 1.00)⁎ | 0.33 (0.11; 0.97) |
| Self-efficacy brisk walk 30 min score d | 1.07 (1.03; 1.12) | 1.06 (1.01; 1.11) |
| Fear of falling (ref = no) | 0.85 (0.48; 1.57) | 0.69 (0.30; 1.40) |
| Not able to walk 30 min without rest (ref = no) | 1.01 (0.61; 1.69) | – |
| Environmental attributes: reference category is "agree" in all statements | ||
| Many places to go within easy walking distance | 0.55 (0.30; 0.99)⁎ | 0.65 (0.30; 1.40) |
| It is easy to walk to a public transport stop | 0.79 (0.35; 1.81) | 1.90 (0.63; 5.72) |
| There are footpaths on most of the streets | 1.06 (0.56; 1.99) | 1.65 (0.74; 3.65) |
| There are crosswalks and pedestrian signals | 0.87 (0.52; 1.48) | 0.93 (0.43; 2.04) |
| The streets in my neighborhood are not hilly | 0.64 (0.30; 1.40) | 0.94 (0.38; 2.33) |
| Walkers in my neighborhood can be easily seen | 0.78 (0.41; 1.49) | 1.03 (0.45; 2.31) |
| There is lots of greenery around my local area | 2.45 (1.01; 5.92)⁎ | 3.33 (1.11; 9.98)⁎ |
| There are many interesting things to look at | 0.61 (0.26; 1.42) | 0.55 (0.21; 1.45) |
| There is not much traffic along nearby streets | 1.36 (0.76; 2.41) | 1.98 (1.00; 3.91)⁎ |
| My local areas has … parks, walking trails | 0.57 (0.26; 1.24) | 0.55 (0.22; 1.39) |
| Crime rate in my neighborhood is not a problem | 0.42 (0.13; 1.31) | 0.30 (0.09; 1.05)⁎ |
| Main effects and interaction model e | ||
| Pedestrian-oriented neighborhood (items 1–4) × intervention | 4.79 (1.28; 17.92) | |
Model predicting regular walking at 12 months adjusted for baseline regular walking and one predictor only.
Model further adjusted for age, gender, and education, and all the listed predictors and confounders.
OR = odds ratio.
Increment of 1 point in self-efficacy score which ranged from 1 to 5 (highest).
Interaction term model and all covariates in main effect model (pedestrian-oriented; items 1–4 collapsed).
p-value < 0.05
In multivariable analysis (Table 2, 2nd column), after adjusting for intervention group, baseline walking, significant predictors of walking (self-efficacy, perceived health status), and confounders (recurrent falling, FOF, gender, age and education), the significant (p < 0.05) perceived walkability predictors for regular walking at follow-up were not reporting “lots of greenery around my local area” (AOR = 3.28, 95% CI: 1.09–9.88), feeling unsafe from crime (AOR = 0.31, 95% CI: 0.09–1.09) and reporting “so much traffic along nearby streets that it makes it difficult or unpleasant to walk” (AOR = 1.98, 95% CI: 1.00–3.91). Interestingly, recurrent fallers were twice as likely to be regular walkers at follow-up as those who did not experience multiple falls.
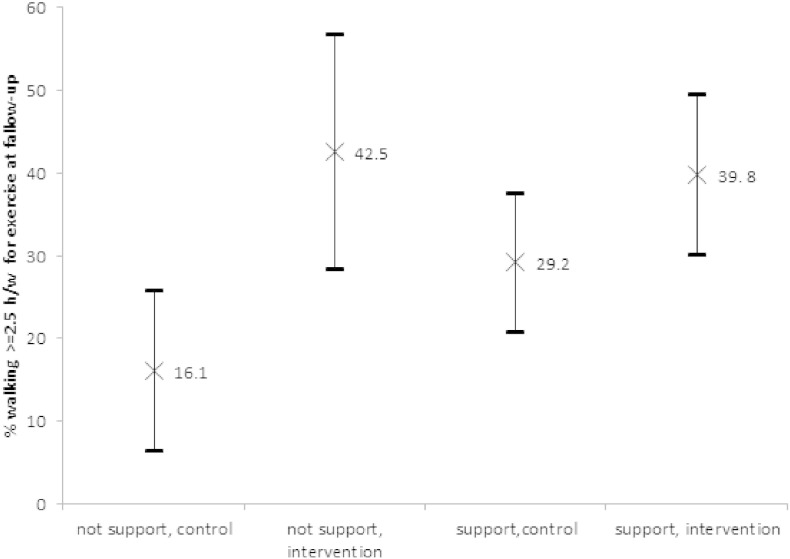
Neither FOF nor health status moderated the intervention effect (data not shown). There was also no significant interaction between the intervention group and any of the significant environmental predictors for ‘regular walking’ at follow-up, although the between-group differences in the proportion of regular walking at follow-up were greater in the lowest walkability quartile (25.3%) than in the higher combined (12.0%, p = 0.218 for interaction, data not shown). The ‘pedestrian-oriented’ subscale was a significant effect modifier (p < 0.036 for interaction). The intervention effect on regular walking at follow-up (Table 2 last row, Fig. 2) was significant only in low pedestrian-oriented environments. The between-group difference in regular walking in the lowest quartile of pedestrian-oriented environments was 30.9% (p < .002), but not significant in the higher pedestrian-oriented environments (9.8%, p = 0.131).
Fig. 2.
The effect of unsupportive infrastructure for walking for intervention and control group.
Discussion
This study joins the few investigations that can support a temporal association between perceived walkability measured at baseline with a subsequent change in walking for exercise and recreation, and, to the best of our knowledge, this is the first study to examine the relationship between FOF and perceived walkability. We found that participants' health status, fall history and concern about falling were associated with perceptions of the environment, in particular in the rating of “easy walking distance” to destinations. While participants' perceptions of low safety from crime was the single environmental predictor that reduced the likelihood for regular walking, unexpectedly, perceived low greenery around the neighborhood and heavy traffic were associated with significantly higher levels of walking for exercise. The greater intervention effect in participants who perceived local walking infrastructure to be poorer points to the usefulness of the intervention. Participants in the control group significantly increased their walking for exercise, yet appeared only able to do so in pedestrian-oriented neighborhoods, defined here as perceived close-by destinations and public transport, existence of sidewalks, crosswalks and pedestrian signals. By contrast, the intervention group participants increased regular walking in both low and high pedestrian-oriented neighborhoods, which highlights the particular benefit of the Easy Steps to Health Intervention in situations of poor walkability.
FOF is recognized as a debilitating condition which is associated with reduced mobility and increased risk of admission to a nursing home (Cumming et al., 2000). In the present study, FOF was strongly associated with perceptions of low walkability, which in turn can accelerate the process of reduced mobility. This is in line with previous studies which have shown that the neighborhood and home environment can speed up or slow down the disablement process (Clarke et al., 2008, Clarke et al., 2011). For example, land-use diversity was linked to greater independence of older adults despite declining physical functioning (Clarke et al., 2011). However, in the present study FOF was neither a predictor of walking at follow-up nor a moderator of intervention effectiveness. This can be explained by the very low proportion of participants who were concerned with falling. It is possible that had the sample been less homogeneous with a wider range on this measure we would have been able to clarify whether FOF is an intervening or moderating factor between neighborhood walkability and change in exercise walking. A previous study from Australia found that overweight and less physically active adults (≤ 65 years) were more likely to misperceive their objectively measured high walkable neighborhood as low walkable (Gebel et al., 2009). Along these lines, it is possible that older adults who had fallen and suffer from FOF are more likely to misperceive their environment as less walkable than those who did not have such experiences. Unfortunately, the present study did not include objective measures of walkability to clarify the extent to which low walkability is a misperception or real. Regardless, it highlights the need to include FOF and past history of falls in further population-based investigations on the role of the environment in influencing walking.
Some of the findings here are corroborated by qualitative research with older adults. In a recent review of 34 qualitative studies on built environments and physical activity in older adults, pedestrian infrastructure, safety (from traffic and crime), access to facilities, esthetics, and weather and air quality were identified as important factors influencing older adults' physical activity (Moran et al., 2014). Similarly, in focus groups with US older adults, local shopping and services close-by, access to public transport, inadequate pedestrian infrastructure, and neighborhood attractiveness were mentioned as key attributes that influence active aging (Michael et al., 2006). In a review of quantitative studies (van Cauwenberg et al., 2011) these attributes showed inconsistent associations in the six studies that specifically examined recreational and exercise walking, and of these only one employed a longitudinal design (Li et al., 2005). That study in Portland, USA, tracked changes in walking following a community-based leader-led walking intervention and found that the perceived safety of the walking environment, and access to physical activity facilities were associated with the prevention of decline in recreational walking (Li et al., 2005).
Control participants reported an increase in regular walking over the 12-month trial period. This has been observed previously, and can be attributed either to the Hawthorne effect (van Sluijs et al., 2006, Fernald et al., 2012), or to self-motivation. The greater impact of the intervention in neighborhoods perceived as having low pedestrian-oriented design suggests that walking interventions with telephone support can attenuate the effect of some environmental attributes that act as barriers for daily walking in the “real world”. Previously it was shown that in adults aged 30–64 recruited from all parts of New South Wales a pedometer-based walking intervention was effective only in less esthetically pleasing environments (Merom et al., 2009). Taken together, both trials suggest that some unfavorable aspects of an environment can be overcome by effective interventions.
In line with the literature, low perceived health was shown to be the most important barrier to walking (Dawson et al., 2007). However, against expectations, “recurrent fallers” were 2.6 times more likely to be classified as regular walkers at follow-up than those with one or no falls. This may be explained by the belief held in the older population that walking is an activity that can reduce risk of falls, reported by 82% of the participants in the New South Wales Older Adults Fall Prevention Survey (Centre for Health Advancement and Centre for Epidemiology and Research, 2010). It may also reflect the increased exposure to fall hazards among regular walkers.
While the present study provides stronger quality of evidence to the many inconsistent cross-sectional investigations on environment and physical activity relationships among older adults, it is subject to some limitations. First, we used a selective sample recruited based on eligibility criteria which is not representative of the general older adult population. Further, the study area was limited to an urban region with low variability in perceived environmental attributes, as most of the participants lived in suburbs that are close to the center of Sydney, neighborhoods which are mostly high walkable (Mayne et al., 2013). The homogeneity of the overall walkability score may have limited our ability to establish associations. Further, it may also explain unexpected results in relation to greenery; only 7% disagreed with the statement “there is lots of greenery in my neighborhood”. Sydney metro has coastal areas and bays which may be less green, but attractive for exercise walking. In some studies using self-reported measures of the environment has been called a limitation. However, in line with social-cognitive theory (Bandura, 1986, Baranowski et al., 2002), it has been argued that the association between neighborhood attributes and health behavior is mediated by environmental perceptions (Brug et al., 2006), and some studies found stronger associations with physical activity for perceived than for objective measures of the environment (Gebel et al., 2009, Kirtland et al., 2003, Gebel et al., 2011). Further, the narrow assessment of environmental attributes relative to the Australian NEWS (Cerin et al., 2008) limited our ability to better assess each construct. Last, our analysis may be subjected to spurious findings due to multiple testing and multiple interaction terms.
Conclusions
Although perceived neighborhood walkability can be shaped by health and fall-related risk factors, it may not pose a barrier for regular walking in a context of intervention. The intervention effect was significantly greater in low pedestrian-oriented environments. Future population-based studies on environments and walking should include information on fall-related risk factors to better understand how these person-level characteristics interact.
Funding
This work was supported by the NSW Ministry of Health (previously NSW Department of Health) (Ref No. HP08/08) Health Promotion Research Demonstration Grants Scheme (HP08/08). Dafna Merom was supported by a postdoc fellowship from the Australian National Health and Medical Research Council project #571150.
Neither body had any role in the design, execution, analysis and interpretation of data, or writing of the study.
Conflict of interests
None declared.
Acknowledgments
The authors wish to acknowledge the contribution of Joanna Jaques, Cameron Hicks, and Mayna Ratanapongleka, from the Health Promotion Service, in coordinating aspects of the study. The authors would also like to acknowledge the editorial support of Angela Balafas, Senior Health Promotion Officer, and Mandy Williams, Acting Director, Health Promotion Service.
Contributor Information
D. Merom, Email: d.merom@uws.edu.au.
K. Gebel, Email: klaus.gebel@jcu.edu.au.
A. Voukelatos, Email: alexander_voukelatos@hotmail.com.
C. Rissel, Email: chris.rissel@sydney.edu.au.
C. Sherrington, Email: csherrington@georgeinstitute.org.au.
References
- Bandura A. Prentice Hall; Englewood Cliffs, NJ: 1986. Social Foundations of Thought and Action. A Social Cognitive Theory. [Google Scholar]
- Baranowski T., Perry C., Parcel G. How individuals, environments, and health behavior interact: social cognitive theory. In: Glanz K., editor. Health Behavior and Health Education: Theory, Research, and Practice. Jossey-Bass, Wiley; San Francisco: 2002. pp. 165–178. [Google Scholar]
- Brug J., van Lenthe F.J., Kremers S.P. Revisiting Kurt Lewin: how to gain insight into environmental correlates of obesogenic behaviors. Am. J. Prev. Med. 2006;31:525–529. doi: 10.1016/j.amepre.2006.08.016. [DOI] [PubMed] [Google Scholar]
- Centre for Health Advancement and Centre for Epidemiology and Research . NSW Department of Health; Sydney: 2010. New South Wales Falls Prevention Baseline Survey: 2009 Report. [Google Scholar]
- Cerin E., Leslie E., Owen N., Bauman A.E. An Australian version of the Neighborhood Environment Walkability Scale: validity evidence. Meas. Phys. Educ. Exerc. Sci. 2008;12:31–51. [Google Scholar]
- Cervero R., Kockelman K.M. Travel demand and the 3Ds: density, diversity, and design. Transp. Res. D. 1997;2:199–219. [Google Scholar]
- Clarke P., George L.K. The role of the built environment in the disablement process. Am. J. Public Health. 2005;95:1933–1939. doi: 10.2105/AJPH.2004.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P., Ailshire J.A., Bader M., Morenoff J.D., House J.S. Mobility disability and the urban built environment. Am. J. Epidemiol. 2008;168:506–513. doi: 10.1093/aje/kwn185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P.J., Ailshire J.A., Nieuwenhuijsen E.R., de Kleijn-de Vrankrijker M.W. Participation among adults with disability: the role of the urban environment. Soc. Sci. Med. 2011;72:1674–1684. doi: 10.1016/j.socscimed.2011.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cumming R.G., Salkeld G., Thomas M., Szonyi G. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J. Gerontol. A Biol. Sci. Med. Sci. 2000;55:M299–M305. doi: 10.1093/gerona/55.5.m299. [DOI] [PubMed] [Google Scholar]
- Dawson J., Hillsdon M., Boller I., Foster C. Perceived barriers to walking in the neighborhood environment: a survey of middle-aged and older adults. J. Aging Phys. Act. 2007;15:318–335. doi: 10.1123/japa.15.3.318. [DOI] [PubMed] [Google Scholar]
- Delbaere K., Hauer K., Lord S.R. Evaluation of the incidental and planned activity questionnaire (IPEQ) for older people. Br. J. Sports Med. 2010;44:1029–1034. doi: 10.1136/bjsm.2009.060350. [DOI] [PubMed] [Google Scholar]
- Ding D., Sallis J.F., Kerr J., Lee S., Rosenberg D.E. Neighborhood environment and physical activity among youth a review. Am. J. Prev. Med. 2011;41:442–455. doi: 10.1016/j.amepre.2011.06.036. [DOI] [PubMed] [Google Scholar]
- Fernald D.H., Coombs L., DeAlleaume L., West D., Parnes B. An assessment of the Hawthorne effect in practice-based research. J. Am. Board Fam. Med. 2012;25:83–86. doi: 10.3122/jabfm.2012.01.110019. [DOI] [PubMed] [Google Scholar]
- Gebel K., Bauman A., Owen N. Correlates of non-concordance between perceived and objective measures of walkability. Ann. Behav. Med. 2009;37:228–238. doi: 10.1007/s12160-009-9098-3. [DOI] [PubMed] [Google Scholar]
- Gebel K., Bauman A.E., Sugiyama T., Owen N. Mismatch between perceived and objectively assessed neighborhood walkability attributes: prospective relationships with walking and weight gain. Health Place. 2011;17:519–524. doi: 10.1016/j.healthplace.2010.12.008. [DOI] [PubMed] [Google Scholar]
- Hanson H.M., Ashe M.C., McKay H.A., Winters M. National Collaborating Centre for Environmental Health; Vancouver: 2012. Intersection Between the Built and Social Environments and Older Adults' Mobility: An Evidence Review. [Google Scholar]
- Harris J.K., Lecy J., Hipp J.A., Brownson R.C., Parra D.C. Mapping the development of research on physical activity and the built environment. Prev. Med. 2013;57:533–540. doi: 10.1016/j.ypmed.2013.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempen G.I., Todd C.J., van Haastregt J.C. Cross-cultural validation of the Falls Efficacy Scale International (FES-I) in older people: results from Germany, the Netherlands and the UK were satisfactory. Disabil. Rehabil. 2007;29:155–162. doi: 10.1080/09638280600747637. [DOI] [PubMed] [Google Scholar]
- Kerr J., Norman G.J., Adams M.A. Do neighborhood environments moderate the effect of physical activity lifestyle interventions in adults? Health Place. 2010;16:903–908. doi: 10.1016/j.healthplace.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirtland K.A., Porter D.E., Addy C.L. Environmental measures of physical activity supports: perception versus reality. Am. J. Prev. Med. 2003;24:323–331. doi: 10.1016/s0749-3797(03)00021-7. [DOI] [PubMed] [Google Scholar]
- Lee I.M., Ewing R., Sesso H.D. The built environment and physical activity levels: the Harvard Alumni Health Study. Am. J. Prev. Med. 2009;37:293–298. doi: 10.1016/j.amepre.2009.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F., Fisher J., Brownson R.C. A multilevel analysis of change in neighborhood walking activity in older adults. J. Aging Phys. Act. 2005;13:145–159. doi: 10.1123/japa.13.2.145. [DOI] [PubMed] [Google Scholar]
- Mayne D.J., Morgan G.G., Willmore A. An objective index of walkability for research and planning in the Sydney Metropolitan Region of New South Wales, Australia: an ecological study. Int. J. Health Geogr. 2013:12. doi: 10.1186/1476-072X-12-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merom D., Bauman A., Phongsavan P. Can a motivational intervention overcome an unsupportive environment for walking—findings from the Step-by-Step Study. Ann. Behav. Med. 2009;38:137–146. doi: 10.1007/s12160-009-9138-z. [DOI] [PubMed] [Google Scholar]
- Merom D., Delbaere K., Cumming R. Incidental and planned exercise questionnaire for seniors: validity and responsiveness. Med. Sci. Sports Exerc. 2014;46:947–954. doi: 10.1249/MSS.0000000000000196. [DOI] [PubMed] [Google Scholar]
- Michael Y.L., Green M.K., Farquhar S.A. Neighborhood design and active aging. Health Place. 2006;12:734–740. doi: 10.1016/j.healthplace.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael Y.L., Perdue L.A., Orwoll E.S. Physical activity resources and changes in walking in a cohort of older men. Am. J. Public Health. 2010;100:654–660. doi: 10.2105/AJPH.2009.172031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran M., van Cauwenberg J., Hercky-Linnewiel R. Understanding the relationships between the physical environment and physical activity in older adults: a systematic review of qualitative studies. Int. J. Behav. Nutr. Phys. Act. 2014;11 doi: 10.1186/1479-5868-11-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagel C.L., Carlson N.E., Bosworth M., Michael Y.L. The relation between neighborhood built environment and walking activity among older adults. Am. J. Epidemiol. 2008;168:461–468. doi: 10.1093/aje/kwn158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson M.E., Rejeski W.J., Blair S.N. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007;39:1435–1445. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J. Am. Geriatr. Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Richardson J.K., Thies S.B., DeMott T.K., Ashton-Miller J.A. A comparison of gait characteristics between older women with and without peripheral neuropathy in standard and challenging environments. J. Am. Geriatr. Soc. 2004;52:1532–1537. doi: 10.1111/j.1532-5415.2004.52418.x. [DOI] [PubMed] [Google Scholar]
- Saelens B.E., Handy S.L. Built environment correlates of walking: a review. Med. Sci. Sports Exerc. 2008;40:S550–S566. doi: 10.1249/MSS.0b013e31817c67a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis J.F., King A.C., Sirard J.R., Albright C.L. Perceived environmental predictors of physical activity over 6 months in adults: activity counseling trial. Health Psychol. 2007;26:701–709. doi: 10.1037/0278-6133.26.6.701. [DOI] [PubMed] [Google Scholar]
- Sallis J.F., Floyd M.F., Rodriguez D.A., Saelens B.E. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125:729–737. doi: 10.1161/CIRCULATIONAHA.110.969022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Cauwenberg J., de Bourdeaudhuij I., de Meester F. Relationship between the physical environment and physical activity in older adults: a systematic review. Health Place. 2011;17:458–469. doi: 10.1016/j.healthplace.2010.11.010. [DOI] [PubMed] [Google Scholar]
- van Sluijs E.M., van Poppel M.N., Twisk J.W., van Mechelen W. Physical activity measurements affected participants' behavior in a randomized controlled trial. J. Clin. Epidemiol. 2006;59:404–411. doi: 10.1016/j.jclinepi.2005.08.016. [DOI] [PubMed] [Google Scholar]
- Voukelatos A., Merom D., Rissel C. The effect of walking on falls in older people: the ‘Easy Steps to Health’ randomized controlled trial study protocol. BMC Public Health. 2011;11:888. doi: 10.1186/1471-2458-11-888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voukelatos A., Merom D., Sherirngton C. The impact of a home-based walking program on falls in older people: the Easy Steps randomised controlled trial. Age Ageing. 2015;44:377–383. doi: 10.1093/ageing/afu186. [DOI] [PubMed] [Google Scholar]