Abstract
BACKGROUND
Mortality following total hip and knee replacement is lower than the general population, but it is unknown whether there are differences by surgery type, demographics and calendar year. Our objective was to evaluate trends and determinants of long-term mortality among patients with total hip and knee replacement.
METHODS
Using a historical cohort study design, we passively followed up population-based cohorts of total hip and total knee replacement patients with degenerative arthritis who underwent surgery between 1/1/1969 and 12/31/2008. Patients were followed up until death or 8/31/2014. Observed and expected survival was compared using standardized mortality ratios (SMR). Poisson regression models were used to examine relative mortality patterns by surgery type, age, sex, calendar year and time since surgery.
RESULTS
The overall age- and sex-adjusted mortality was significantly lower than the general population following both total hip (SMR: 0.82, 95% CI: 0.76, 0.88) and total knee (SMR = 0.80, 95% CI: 0.75, 0.86) replacement. Despite the low relative mortality within the first 8 years of surgery, we observed a worsening of relative mortality beyond 15 years after total knee replacement surgery. Both short and long term mortality improved over calendar time, and the improvement occurred about a decade earlier in total knee replacement than in total knee replacement.
CONCLUSION
Survival following total hip and total knee replacement is better than the general population for about 8 years following surgery. Secular trends are encouraging and suggest that survival following both procedures has been improving even further in recent years.
Introduction
Total hip and knee replacement are safe and effective procedures for management of morbidity attributable to end-stage osteoarthritis. Despite the high prevalence and significant public health burden[1], life expectancy among individuals with osteoarthritis and the modifying role of total hip and knee replacement are poorly understood [2–4]. Although individuals with osteoarthritis are at a higher risk of death compared to individuals of the same age and sex in the general population [4], mortality following total hip and knee replacement is better than the general population[5–12], in part due to selection of healthier individuals to undergo surgery and, potentially in part due to benefits of increased mobility and activity levels following surgery[3]. So far, studies with follow-up beyond 5-years are limited. Some studies, mainly from the Nordic countries, show a bi-modal mortality pattern [5–7]. For example, within the Medicare population, investigators observed a convergence of mortality after 5 years following total hip replacement [5]. In a nationwide study from Sweden [7], mortality was lower than the general population for 12 years following knee replacement, but after that, it increased and became significantly worse than the general population. Although these studies suggest disappearance of the mortality difference over time, it is unclear when this occurs, and whether it is true in both total hip and knee replacement.
Regarding demographics, there is strong evidence for an age effect with high standardized mortality ratios among younger patients [7, 8, 11, 12]. Recent studies from England and Wales also suggest that early postoperative mortality fell substantially in recent years[13, 14], but it is unclear whether this improvement in mortality extends beyond the postoperative period which is not influenced by surgery itself but general population mortality trends. Indeed, considering the dramatic improvements in overall mortality in the general population[15], it would be reasonable to expect that the long-term mortality among total hip and knee replacement patients has followed the same pattern, but this has never been investigated.
With this background, our objective was to evaluate the trends and determinants of long-term mortality among patients with total hip and knee replacement in the United States. We sought to describe mortality differences by surgery type, demographics, calendar year and time since surgery.
Methods
We performed a historical cohort study in a population-based setting in the United States[16, 17]. Population-based epidemiologic studies in Olmsted County, Minnesota are feasible because of its relative geographic isolation from other urban centers and because nearly all medical care is delivered to local residents by a small number of providers. Data from all healthcare providers are contained in a single comprehensive medical records linkage system. Consequently, the unique population-based data resources in Olmsted County ensure virtually complete ascertainment and follow-up of total hip and knee replacement patients in a geographically defined community.
The study population comprised Olmsted County residents who underwent primary total hip (n=1645) and total knee (n=1980) replacement surgery for degenerative arthritis between 1/1/1969 and 12/31/2008[18]. Patients who underwent surgery for other indications and those who denied research authorization for use of their medical records for research were excluded. All patients were followed up longitudinally until death or 8/31/2014.
Statistical analyses were performed separately for the total hip and knee replacement cohorts. Death rates following total hip or knee replacement were evaluated using a person-years approach, in which the observed number of deaths in each cohort was compared to the expected number of deaths over the follow-up period. Expected survival was generated using the annual life tables. The results were reported as standardized mortality ratios (SMRs) with corresponding 95% confidence intervals (CIs). The confidence intervals were calculated assuming that the expected rates are fixed and the observed deaths follow a Poisson distribution. The confidence intervals are shown as dashed lines in the figures. Poisson regression models were used to model relative mortality by surgery type, age, calendar year of surgery and time since surgery. Although the relative mortality was slightly lower in males, the relative mortality patterns were similar in males and females; therefore, analyses were performed by combining data for male and female patients. Additionally, separate analyses were performed to evaluate relative mortality within the first year following surgery, and in the period following one year after surgery. For the former, all patients were included, but only deaths observed in the first year were analyzed, and follow-up greater than 365 days was censored at one year. For the latter, only patients with at least one year of follow-up were included. All analyses were performed using R version 3.0 (http://www.R-project.org/).
Results
Over a mean follow-up of 11.9 years (19573.7 person-years) of 1645 total hip replacement patients, 814 patients died. Similarly, over a mean follow-up of 10.8 years (21465.4 person-years) of 1980 total knee replacement patients, 842 patients died. Survival in both the total hip replacement and the knee replacement cohorts was significantly better than that expected in the general population with an SMR of 0.82 (95% CI 0.76, 0.88) following total hip replacement and SMR of 0.80 (95% CI 0.75, 0.86) following total knee replacement (Table 1).
Table 1.
Observed and Expected Number of Deaths and Standardized Mortality Ratios (95% Confidence Intervals) in Total Hip and Knee Replacement
| Total Hip Replacement | Total Knee Replacement | |||||
|---|---|---|---|---|---|---|
| Observed | Expected | SMR (95% CI) | Observed | Expected | SMR (95% CI) | |
| Overall | 1091 | 1184 | 0.92 (0.87, 0.98) | 1010 | 1200 | 0.84 (0.79, 0.90) |
| Osteoarthritis | 814 | 995 | 0.82 (0.76, 0.88) | 842 | 1049 | 0.80 (0.75, 0.86) |
| Sex | ||||||
| Men | 412 | 472 | 0.87 (0.79, 0.96) | 401 | 504 | 0.80 (0.72, 0.88) |
| Women | 679 | 712 | 0.95 (0.88, 1.03) | 609 | 696 | 0.88 (0.81, 0.95) |
| Age groups, years | ||||||
| <60 | 147 | 108 | 1.36 (1.15, 1.60) | 86 | 69 | 1.25 (0.99, 1.54) |
| 61–70 | 297 | 338 | 0.88 (0.78, 0.98) | 260 | 293 | 0.89 (0.78, 1.00) |
| 71–80 | 439 | 473 | 0.93 (0.84, 1.02) | 482 | 589 | 0.82 (0.75, 0.90) |
| >80 | 208 | 265 | 0.79 (0.68, 0.90) | 182 | 250 | 0.73 (0.63, 0.84) |
Reduction in mortality was of similar magnitude in men and women for both procedures with an age-adjusted SMR of 0.82 (95% CI 0.75, 0.90) for women and 0.81 (95% CI 0.73, 0.90) for men in total hip replacement, and 0.82 (95% CI 0.75, 0.90) for women and 0.78 (95% CI 0.70, 0.86) for men in total knee replacement. Furthermore, the SMR decreased with increasing age at the time of surgery (Table 1).
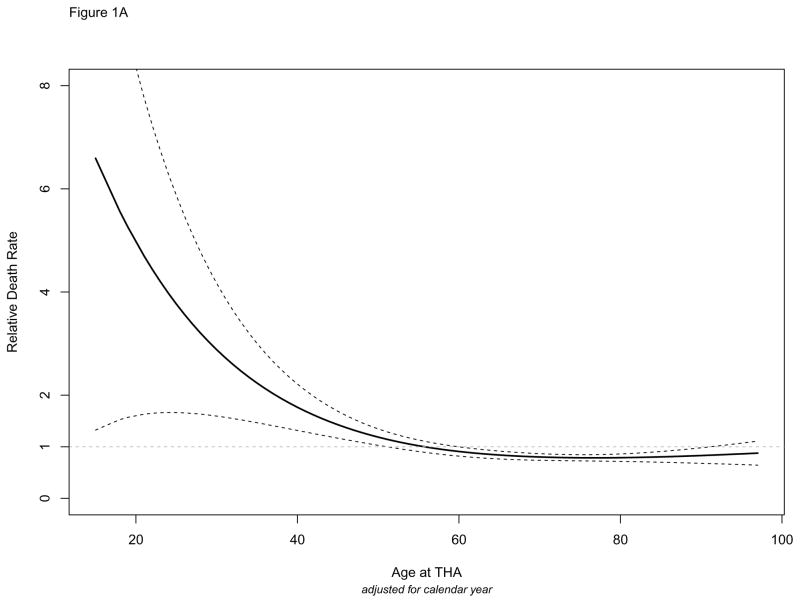
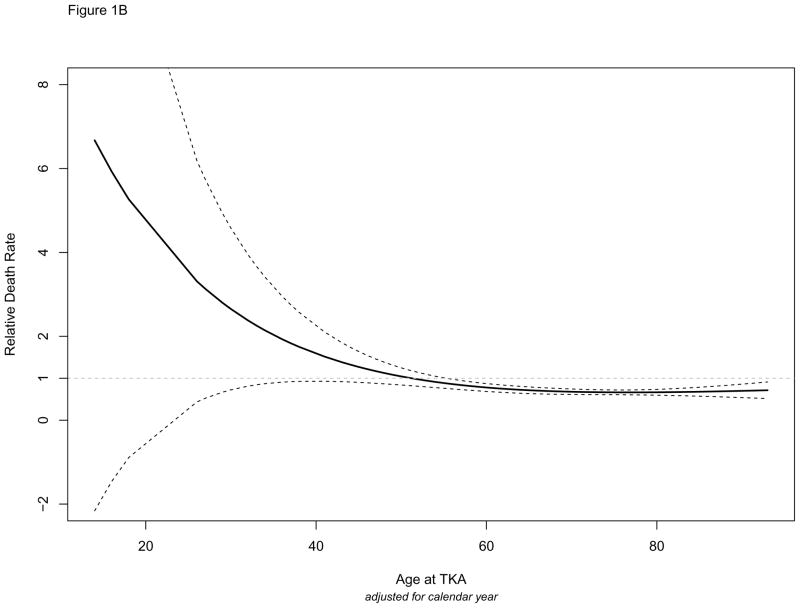
Figures 1A and 1B illustrate relative death rates according to age at surgery adjusting for calendar year of surgery. Dashed lines indicate the 95% confidence intervals. In both total hip (Figure 1A) and total knee replacement (Figure 1B), the relative death rate was highest in younger ages and declined as age at surgery increased. The wide confidence intervals at younger ages are due to the low number of patients less than 50 years of age. The confidence intervals for the relative death rate were below 1 after 60 years of age in total hip replacement and after 55 years of age in total knee replacement, indicating that their mortality was better than their peers of the same age in the general population. Moreover, consistent with the SMR estimates, the relative death rate curve for total knee replacement patients was lower than that for total hip replacement patients.
Figure 1.
Figure 1A. Relative Death Rates (observed/expected) by Age: Total Hip Replacement
Figure 1B. Relative Death Rates (observed/expected) by Age: Total Knee Replacement
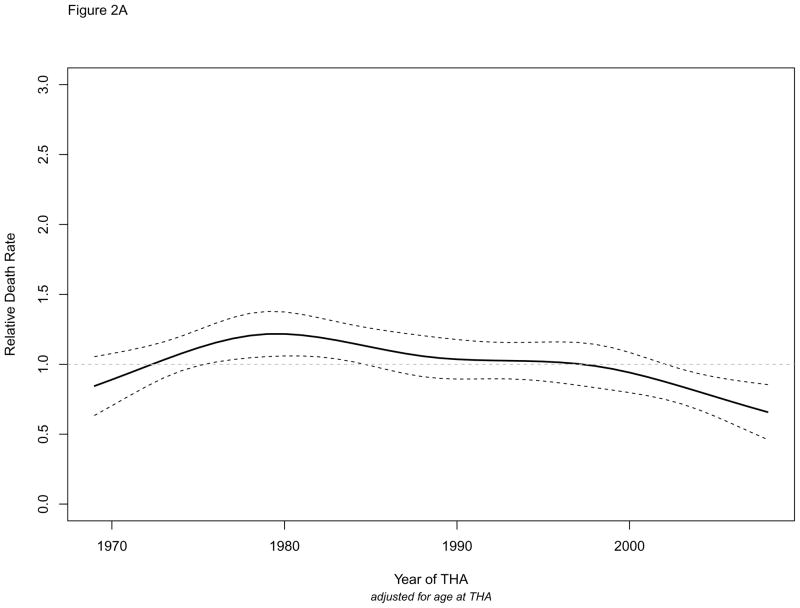
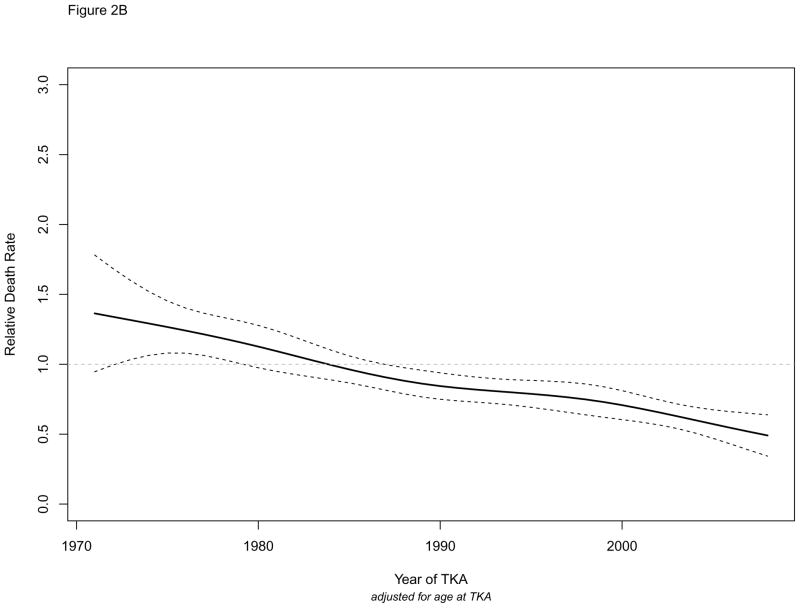
Figures 2A and 2B illustrate the relative death rates over time according to calendar year of surgery derived from age-adjusted Poisson regression models. We observed notable differences by surgery type. In total hip replacement (Figure 2A), the relative death rate was relatively flat around 1 (indicating mortality similar to the general population) until early 2000’s after which it declined and became significantly better than the general population. In total knee replacement (Figure 2B), the relative death rate showed almost a linear decline over time, indicating steady improvements in survival of total knee replacement patients over time. In fact, as early as late1980’s, the death rate following total knee replacement was significantly better than the general population (as indicated by the non-overlap of the confidence intervals with the unity line at 1) and continued to improve over time. These trends indicate that first, improvement in relative mortality occurred about a decade earlier in total knee replacement than in total hip replacement, and second, mortality rates following total knee replacement declined faster than the general population mortality.
Figure 2.
Figure 2 A. Relative Death Rates (observed/expected) by Calendar Year of Surgery: Total Hip Replacement
Figure 2 B. Relative Death Rates (observed/expected) by Calendar Year of Surgery: Total Knee Replacement
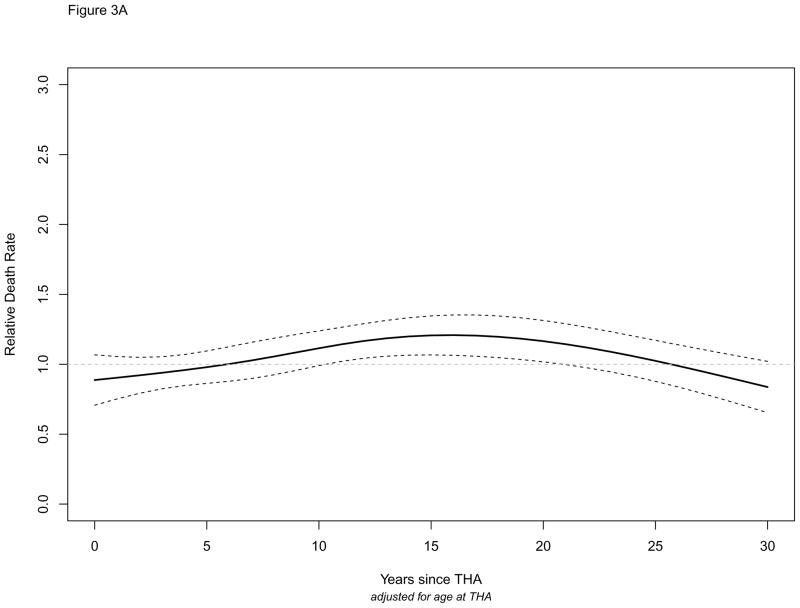
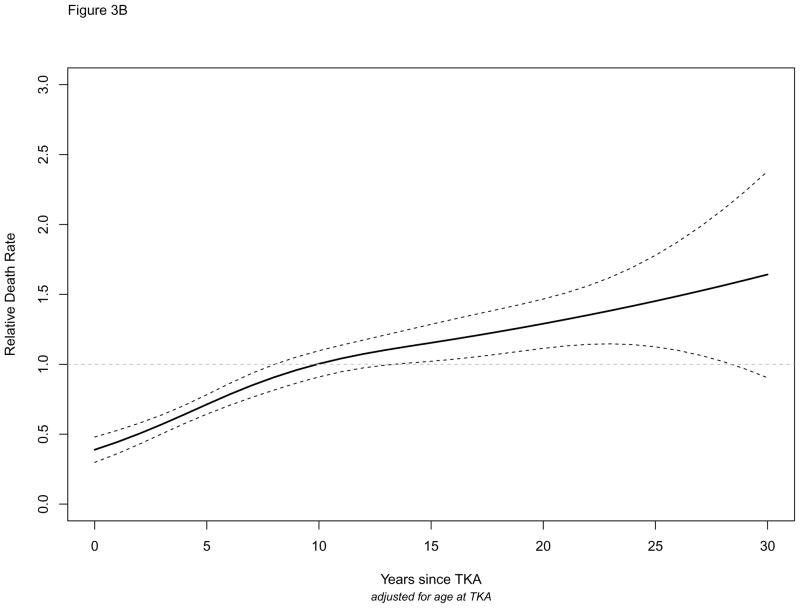
We then examined relative death rates according to time since surgery. The relative death rate was significantly lower than the general population for about 8 years following both procedures (Figures 3A and 3B). The relative death rate was as low as 50% within the first year of total knee replacement surgery but there was a shift in relative mortality beyond 15 years (Figure 3B). The relative death rate following total knee replacement increased steadily during follow-up and became significantly worse than the general population beyond 18 years after surgery. Indeed, the relative death rates at 5 and 18 years following total knee replacement were 0.67 (95 % CI, 0.61, 0.74) and 1.19 (95 % CI, 1.01, 1.36), respectively. We did not observe such a shift in mortality in total hip replacement (Figure 3A).
Figure 3.
Figure 3A. Relative Death Rates (observed/expected) by Time since Surgery: Total Hip Replacement
Figure 3B. Relative Death Rates (observed/expected) by Time since Surgery: Total Knee Replacement
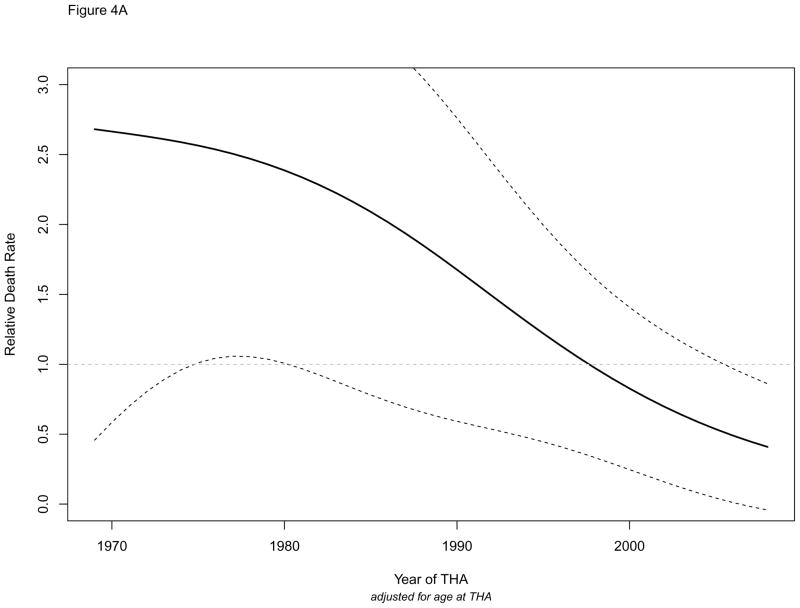
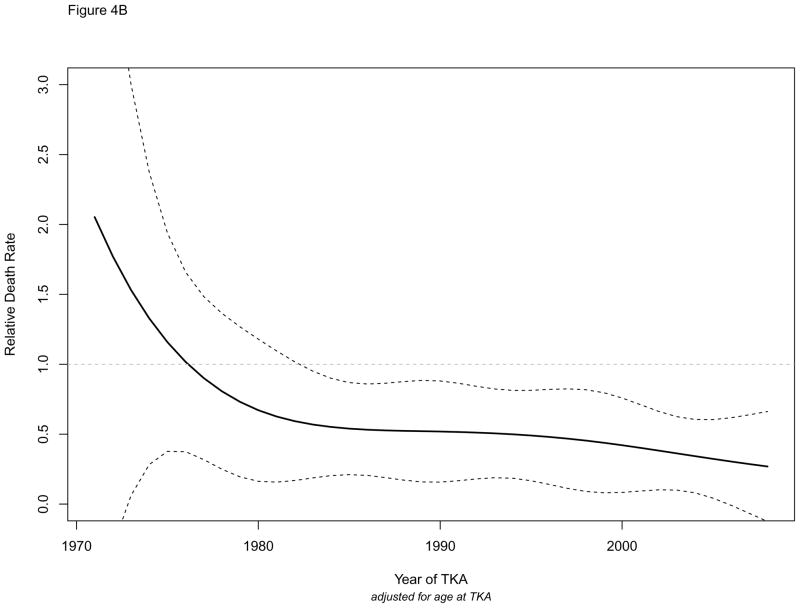
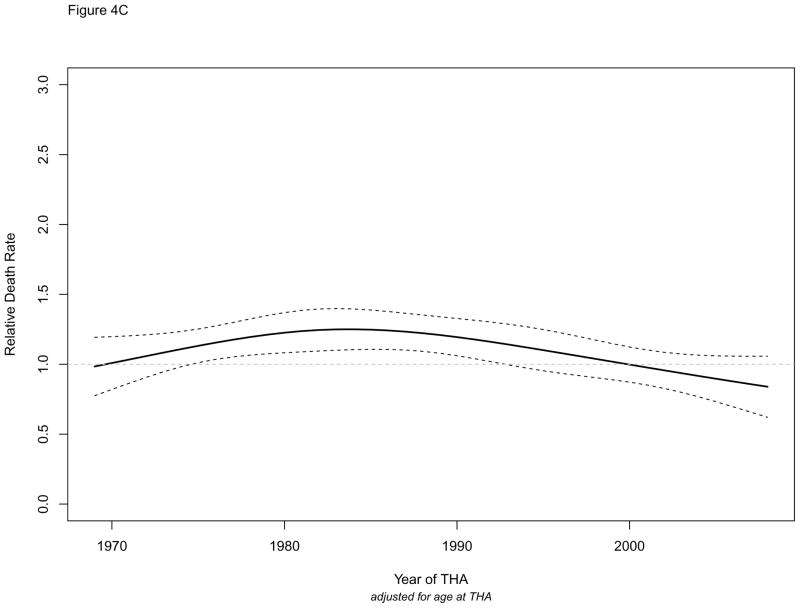
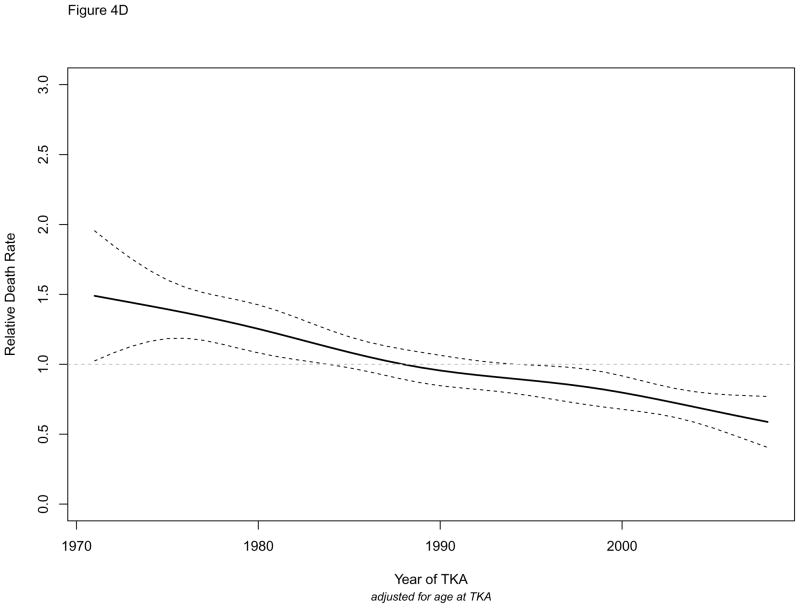
We further examined to what extent these secular trends were driven by improvements in short-term (1-year) mortality in recent years, as shown in recent studies (Figure 4). Figures 4A and 4B illustrate relative death rates within the first year of surgery, and Figures 4C and 4D illustrate relative death rates beyond the first year following surgery. Overall, the downward trends in these figures indicate that improvements in mortality occurred both for short- and long-term mortality. In total hip replacement, improvement in 1st year mortality seems to have started in early 1990’s but the pattern was not significant as indicated by the wide confidence intervals overlapping the unity line at 1 (Figure 4A). In total knee replacement, improvement in 1st year mortality started earlier and continued to improve thereafter (Figure 4B). Figures of relative death rates beyond the first year following surgery (Figure 4C and 4D) were similar to overall Figures 2A and 2B. Among total hip replacement patients who survived the first year (4C), improvement in mortality occurred only during the last decade. Among total knee replacement patients who survived the first year (Figure 4D), the relative death rate declined gradually and was significantly better than the general population by early 1990’s.
Figure 4.
Figure 4A. Relative Death Rates within the First Year of Surgery: Total Hip Replacement
Figure 4B. Relative Death Rates within the First Year of Surgery: Total Knee Replacement
Figure 4C. Relative Death Rates beyond the First Year: Total Hip Replacement
Figure 4D. Relative Death Rates beyond the First Year: Total Knee Replacement
Discussion
In this population-based study that spanned four decades, we evaluated mortality trends following total hip and knee replacement. Consistent with previous studies, mortality following both procedures is lower than the general population, and declines with increasing age at surgery. Despite the low relative mortality for about 8 years following surgery, mortality becomes worse than the general population beyond 15 years after total knee replacement surgery. Secular trends are encouraging and suggest that both short and long term mortality continues to improve in recent years. Finally, improvement in mortality seems to have occurred about a decade earlier in total knee replacement than in total hip replacement. Although the reasons for some trends, in particular the worsening of mortality beyond the first decade, remain to be determined with certainty, our encouraging findings reflect the success of the orthopedic community in improving the outcomes of their arthroplasty patients.
Our findings update and extend previous studies with findings broadly similar to those reported from population-based cohorts of similar age and sex distribution and length of follow-up [5–12]. For example, total hip replacement patients in Norway had 20% reduction in mortality (HR = 0.81) compared to the general population at eight years after surgery, despite having a higher risk of death within the first 2 months[8]. The reduced mortality following total hip and knee replacement is generally attributed to patient selection. The inverse relationship between age and mortality has been previously described [7, 8, 12], and similar to our findings, more pronounced in total hip replacement than in knee replacement.
In contrast to the overall and age-specific SMR estimates, there are only a handful of long-term mortality studies describing the bi-modal mortality pattern with the worsening of mortality beyond the first decade of surgery. Our findings are strikingly consistent with these studies [6, 7, 19]. Among almost 25,000 total hip replacement patients from Finland, Paavolainen et al [6] found that mortality was low during the first 5 years after surgery, but increased to unity (i.e., similar to general population) thereafter. In a cohort of more than 65,000 total knee replacement patients from Sweden[7], Robertsson et al. described reduced mortality during the first 12 postoperative years, but beyond 12 years, mortality increased and became significantly worse than the general population. Robertsson et al. attributed this finding to increased mortality in younger patients with longer follow-up, rather than an increased mortality in all patients. The reasons for the bimodal mortality pattern are unknown, and may potentially include underlying comorbidities and/or revision surgeries in these patients. Individuals who undergo surgery at a younger age may have more comorbidities and higher risk of death. With the ever growing number of individuals living with hip and knee replacement[20], there is a need to identify the drivers of the long-term morbidity and mortality in total hip and knee replacement.
Our analyses of secular trends indicate temporal improvements in mortality in both total hip and knee replacement patients. Although this was previously demonstrated for short-term mortality[13, 14, 21, 22], only one prior study from Norway reported declines in long-term mortality[8]. In a nationwide total hip replacement cohort, investigators observed a statistically significant difference in the SMR between 1987–90 and 1995–98 but a significance test for trend was not significant. This is not surprising because our observations suggest that the mortality decline following total hip replacement may have occurred after 2000, and possibly about a decade later than in total knee replacement. With a mean follow-up of 11 years, we were able to show that the temporal improvements in in mortality is not just confined to the first year of surgery, and, at least in the case of total knee replacement, may have occurred even faster than the general population. Combined with the results of the short-term mortality studies[13, 14, 21], we can conclude that total hip and knee replacement patients have much lower mortality today than their counterparts about a decade ago.
Our study has a number of potential limitations. First and foremost, findings may not be generalizable to all joint replacement patients in the United States, in part due to racial and ethnic composition of the population during the calendar years under investigation, and in part due to variation in patient selection for joint replacement [23]. The generalizability of our mortality findings to demographically more diverse populations is unknown. Second, although our follow-up extended to August 2014, the cohort of joint replacement patients was limited to those who underwent surgery prior to 2008. Therefore, we cannot extrapolate our findings to patients who underwent surgery after 2008, who may have a different underlying mortality risk[21]. Third, due to the small cohort size, we had limited power for some of the analyses, such as mortality patterns among younger arthroplasty patients. Fourth, the reasons for the observed relative mortality trends, i.e. comorbidities, revisions are not addressed in the study. Our population-based design and inclusion of successive joint replacement cohorts since these procedures first started are unique strengths of the present study. In addition, our long and complete follow-up of all hip and knee replacement patients and ready access to general population mortality (expected) rates throughout the entire time period are advantages that made the current study feasible. In conclusion, there are notable differences in relative mortality trends following total hip and total knee replacement. Both short-term and long-term mortality are improving in recent years. These encouraging findings underscore the safety and effectiveness of total hip and knee replacement.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Murray CJL, Vos T, Lozano R, AlMazroa MA, Memish ZA. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010 (vol 380, pg 2197, 2012) Lancet. 2013 Feb 23;381(9867):628. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 2.Liu R, Huizinga TW, Kloppenburg M. Mortality in Osteoarthritis: A Systematic Review. Osteoarthritis and Cartilage. 2013 Apr;21:S137-S. doi: 10.1016/j.joca.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 3.Ravi B, Croxford R, Austin PC, Lipscombe L, Bierman AS, Harvey PJ, Hawker GA. The relation between total joint arthroplasty and risk for serious cardiovascular events in patients with moderate-severe osteoarthritis: propensity score matched landmark analysis. BMJ-Brit Med J. 2013 Oct 30;347 doi: 10.1136/bmj.f6187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nuesch E, Dieppe P, Reichenbach S, Williams S, Iff S, Juni P. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ. 2011;342:d1165. doi: 10.1136/bmj.d1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barrett J, Losina E, Baron JA, Mahomed NN, Wright J, Katz JN. Survival following total hip replacement. J Bone Joint Surg Am. 2005 Sep;87(9):1965–71. doi: 10.2106/JBJS.D.02440. [DOI] [PubMed] [Google Scholar]
- 6.Paavolainen P, Pukkala E, Pulkkinen P, Visuri T. Causes of death after total hip arthroplasty - A nationwide cohort study with 24,638 patients. J Arthroplasty. 2002 Apr;17(3):274–81. doi: 10.1054/arth.2002.30774. [DOI] [PubMed] [Google Scholar]
- 7.Robertsson O, Stefansdottir A, Lidgren L, Ranstam J. Increased long-term mortality in patients less than 55 years old who have undergone knee replacement for osteoarthritis: results from the Swedish Knee Arthroplasty Register. The Journal of Bone and Joint Surgery British volume. 2007 May;89(5):599–603. doi: 10.1302/0301-620X.89B5.18355. [DOI] [PubMed] [Google Scholar]
- 8.Lie SA, Engesaeter LB, Havelin LI, Gjessing HK, Vollset SE. Mortality after total hip replacement: 0–10-year follow-up of 39,543 patients in the Norwegian Arthroplasty Register. Acta Orthopaedica Scandinavica. 2000 Feb;71(1):19–27. doi: 10.1080/00016470052943838. [DOI] [PubMed] [Google Scholar]
- 9.Ohzawa S, Takahara Y, Furumatsu T, Inoue H. Patient survival after total knee arthroplasty. Acta medica Okayama. 2001 Oct;55(5):295–9. doi: 10.18926/AMO/32013. [DOI] [PubMed] [Google Scholar]
- 10.Clement ND, Jenkins PJ, Brenkel IJ, Walmsley P. Predictors of mortality after total knee replacement: a ten-year survivorship analysis. The Journal of Bone and Joint Surgery British volume. 2012 Feb;94(2):200–4. doi: 10.1302/0301-620X.94B2.28114. [DOI] [PubMed] [Google Scholar]
- 11.Ramiah RD, Ashmore AM, Whitley E, Bannister GC. Ten-year life expectancy after primary total hip replacement. The Journal of Bone and Joint Surgery British volume. 2007 Oct;89(10):1299–302. doi: 10.1302/0301-620X.89B10.18735. [DOI] [PubMed] [Google Scholar]
- 12.Pedersen AB, Baron JA, Overgaard S, Johnsen SP. Short- and long-term mortality following primary total hip replacement for osteoarthritis: a Danish nationwide epidemiological study. The Journal of Bone and Joint Surgery British volume. 2011 Feb;93(2):172–7. doi: 10.1302/0301-620X.93B2.25629. [DOI] [PubMed] [Google Scholar]
- 13.Hunt LP, Ben-Shlomo Y, Clark EM, Dieppe P, Judge A, MacGregor AJ, Tobias JH, Vernon K, Blom AW. 90-day mortality after 409 096 total hip replacements for osteoarthritis, from the National Joint Registry for England and Wales: a retrospective analysis. Lancet. 2013 Sep 28;382(9898):1097–104. doi: 10.1016/S0140-6736(13)61749-3. [DOI] [PubMed] [Google Scholar]
- 14.Hunt LP, Ben-Shlomo Y, Clark EM, Dieppe P, Judge A, MacGregor AJ, Tobias JH, Vernon K, Blom AW. 45-day mortality after 467,779 knee replacements for osteoarthritis from the National Joint Registry for England and Wales: an observational study. Lancet. 2014 Oct 18;384(9952):1429–36. doi: 10.1016/S0140-6736(14)60540-7. [DOI] [PubMed] [Google Scholar]
- 15.Hoyert DL. NCHS data brief. 88. Hyattsville, MD: National Center for Health Statistics; 2012. 75 years of mortality in the United States, 1935–2010. [PubMed] [Google Scholar]
- 16.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, Pankratz JJ, Brue SM, et al. Data Resource Profile: The Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012 Dec;41(6):1614–24. doi: 10.1093/ije/dys195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, Rocca WA. Use of a Medical Records Linkage System to Enumerate a Dynamic Population Over Time: The Rochester Epidemiology Project. Am J Epidemiol. 2011 May 1;173(9):1059–68. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh JA, Vessely MB, Harmsen WS, Schleck CD, Melton LJ, Kurland RL, et al. A Population-Based Study of Trends in the Use of Total Hip and Total Knee Arthroplasty, 1969–2008. Mayo Clin Proc. 2010 Oct;85(10):898–904. doi: 10.4065/mcp.2010.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Visuri T, Borg H, Pulkkinen P, Paavolainen P, Pukkala E. A retrospective comparative comparative study of mortality and causes of death among patients with metal-on-metal and metal-on-polyethylene total hip prostheses in primary osteoarthritis after a long-term follow-up. Bmc Musculoskeletal Disorders. 2010 Apr 23;11 doi: 10.1186/1471-2474-11-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, et al. Prevalence of Total Hip and Knee Replacement in the United States. JBJS. doi: 10.2106/JBJS.N.01141. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lalmohamed A, Vestergaard P, Javaid MK, de Boer A, Leufkens HGM, van Staa TP, de Vries F. Changes in mortality patterns following total hip and knee replacement over the past two decades:a nationwide cohort study. Arthritis and Rheumatology. 2014 doi: 10.1002/art.38232. in press. [DOI] [PubMed] [Google Scholar]
- 22.Cram P, Lu X, Kaboli PJ, Vaughan-Sarrazin MS, Cai X, Wolf BR, Li Y. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991–2008. JAMA. 2011 Apr 20;305(15):1560–7. doi: 10.1001/jama.2011.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, Rocca WA. Generalizability of Epidemiological Findings and Public Health Decisions: An Illustration From the Rochester Epidemiology Project. Mayo Clin Proc. 2012 Feb;87(2):151–60. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.