Abstract
Objective
Health literacy measurement can help inform healthcare service delivery. The objective of this study is to identify validated tools to measure health literacy among Spanish speakers and to summarize characteristics that are relevant when selecting tools for use in clinical or research settings.
Methods
An English and Spanish search of 9 databases was conducted between October 2014 and May 2015. Inclusion criteria were peer-reviewed articles presenting initial validation and psychometric properties of a tool to measure health literacy among Spanish speaking patients. Characteristics relevant to tool selection were reviewed and presented.
Results
Twenty articles validating19 instruments met inclusion criteria. Instruments were designed for use with Spanish speakers in numerous contexts and measured different health literacy skills such as reading comprehension or numeracy. Methods used to validate tools were inconsistent across instruments.
Conclusion
Although tools have inconsistencies and inefficiencies, many can be used for assessment of health literacy among Spanish speakers.
Practice implications
Healthcare providers, organizations, and researchers can use this review to select effective health literacy tools to indicate patient’s ability to understand and use health information so that services and materials can be more appropriately tailored to Spanish speaking patients.
Keywords: Health literacy, Tool, Instrument, Assessment, Spanish, Measurement, Integrative review
1. Introduction
Health literacy can be defined as, “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” [1]. This term was first used in 1974 [2], though many definitions of health literacy have since been used in practice and research [3–5]. The concept of health literacy is distinct from general literacy and includes skills such as problem solving, decision-making, information seeking, and other actions pertinent to health management [4,6].
Low health literacy levels among patients can increase health care costs, hinder informed consent, prevent timely screenings, and is a risk factor for numerous adverse health outcomes [6–13]. Negative health outcomes may be exacerbated in vulnerable populations and can contribute to health disparities, particularly among minority groups such as the elderly, immigrants and some cultural subgroups, especially when language barriers are present [12,14,15]. Improving health literacy among the medically under-served has the potential to lower healthcare costs, enhance access to healthcare, improve social conditions, and reduce health disparities [16–18]. The importance of health literacy has been acknowledged in reports by the Department of Health and Human Services, the Institute of Medicine, and the World Health Organization, which have all issued reports in the last decade that highlight health literacy as a priority and indicate the need for further research on the topic [4,19,20].
1.1. Measuring health literacy among Spanish speakers
The Latino population is the largest and fastest growing subgroup in the United States and now comprises more than 17% of the U.S. population [21–23]. For the purpose of this review “Latino” refers to individuals whose origins are in Spanish speaking countries of Latin America [24,25]. Latinos as a group often have lower educational, general and health literacy levels than the general U.S. population [26,27]. Many Latinos speak Spanish as their primary language, which affects both their ability to access services as well as their interactions with providers in healthcare settings [28]. Lower health literacy combined with language differences can lead to additional problems such as hindered ability to navigate the healthcare system and difficulty accessing health insurance coverage [26,28,29]. Additionally, Latinos are disproportionately affected by many different health conditions such as higher rates of obesity, type 2 diabetes, and human immunodeficiency virus in comparison to their white counterparts because of numerous social and genetic factors [25,30]. Therefore, understanding the health literacy levels of Latino patients is necessary to reduce health disparities and requires tools to measure health literacy that are valid for use among Spanish speakers.
Although health literacy is considered a critical area of research, and about one in every six people in the U.S. are Spanish speakers, most health literacy measures have been developed in English [31,32]. This is a limitation to health literacy measurement because some of the methods that have been used to measure health literacy in English are less effective amongst Spanish speakers. One example is the cloze procedure which asks participants to read a list of words out loud. Scoring is then based on the ability to correctly pronounce the word, as literacy has been closely associated with this ability in English [33,34]. This method is less effective among Spanish speakers because the Spanish language has a more phoneme–grapheme correspondence than English, meaning that each letter has one corresponding phonetic sound so Spanish speakers are more likely to pronounce words correctly even if they do not know or understand the word that they are reading [35]. In addition, English tools must either be translated or newly developed in Spanish so that they are understandable among the populations in which they are intended for use. Verbatim translation of an English tool into any foreign language, and specifically Spanish, may not account for linguistic and cultural differences of different patient populations [36,37]. As a result, tools that have been directly translated from English to Spanish, without cultural and contextual considerations, may be asking patients about words or terms that have no meaning or significance to them based on their country of origin or specific cultural subgroup. In order to effectively measure a person’s understanding of medical terms and information, tools that measure health literacy must be linguistically, culturally, and contextually relevant to the population in which they are administered [32,38]. Tools that have been developed to target a specific subpopulation of interest may be the most informative of patient's actual understanding of health materials [39].
Numeracy is a critical health literacy skill that refers to an individual’s ability to use and understand numbers to achieve tasks such medication dosing, nutrition labels, physiological measures such as blood sugar, and may also directly influences an individual's ability to rate their health status [40,41]. Tools that assess skills such as reading comprehension and numeracy may be the most informative to providers as they represent a patient’s ability to comprehend and use the health information provided to them. Potential limitations, including preferred language, of patients must be considered when testing health literacy in a clinical setting. If a patient has poor eyesight or diminished hearing capacity, as is frequently the case in the elderly, they may score poorly on a reading or listening comprehension test respectively regardless of the language of administration [42].
Because the U.S. has such a large Latino population, it is important to provide healthcare services and health information to patients in Spanish. To do that effectively, health literacy measurement in Spanish is warranted. Although tools to measure health literacy are available in Spanish, they have not yet been comprehensively identified and reviewed. The purpose of this review is to identify validated tools to measure health literacy among Spanish speakers and to summarize characteristics that are relevant when selecting tools for use in clinical or research settings.
2. Methods
Using Whittemore and Knafl’s updated integrative review methodology [43], a comprehensive literature search was conducted, then pertinent article information was reviewed and summarized. The search was conducted in October and November 2014 and was confirmed in May 2015 in both English and in Spanish. Searched databases included: MEDLINE, PubMed, Embase, PsycINFO, CINAHL, Scopus, Cochrane Library, HAPI, and ERIC. No beginning date parameter was specified for articles for the search and the review included papers published and available online through May 10th, 2015. The English search consisted of the combined terms run as both MeSH headings and keywords, “health literacy”, “Spanish”, “tool,” “instrument,” “assessment,” “measurement,” and “questionnaire.” For the Spanish search, the term “health literacy” was applied while using the Spanish language filters for each of the above listed databases. Additionally, the phrase health literacy was translated as “alfabetismo de salud,” confirmed in the literature as an applicable translation of the concept [44,45] and other possible translations such as, “con-ocimiento sobre salud,” “educación para la salud,” “formación sanitaria,” and “conocimiento de la salud” were combined with the following translations of keywords: “herramienta,” “instrumento,” “medir,” “la medida,” “la medición,” “cuestionario,” and “validación”. Citations located in the search were uploaded into Eppi Reviewer 4 and considered for inclusion and exclusion criteria. Duplicates were removed and remaining articles were screened by title and abstract. Inclusion criteria were peer-reviewed articles that presented the initial validation and psychometric properties of a tool to measure health literacy among Spanish speaking patients. Articles were excluded if not published in English or Spanish; were not peer reviewed; did not measure the health literacy of patients; if the purpose of the paper was to use a previously validated tool rather than to assess the tool and if the measure of health literacy was not in Spanish.
2.1. Data extraction
To our knowledge, a validated tool for the quality appraisal of instruments that measure health literacy does not exist. Measurements of health literacy vary greatly based on the reason for conducting health literacy measurement (e.g., screening for low health literacy vs. measuring level of health literacy), the amount of time available for administration, health literacy skills assessed, and health topic addressed. These differences make the consistent assessment of psychometric properties between instruments difficult and the comparison of tools complex [1,4,46,47]. Therefore, in this review we did not appraise the quality of each study but extracted and presented the tool characteristics from each article that are relevant to a healthcare provider or other professional selecting a tool to assess health literacy among Spanish speaking populations. The tool characteristics considered were purpose and context, translation and cultural considerations, item number, health literacy skills assessed, feasibility and method of administration, scoring method, and validity and reliability. Data pertaining to these characteristics were extracted from each article by one researcher (SS) and then confirmed by the other authors and displayed in Table 1 as is specified in the Whittemore and Knafl’s methodology [43,48]. Each tool’s properties were then examined and compared so that a more comprehensive understanding of existent tools to measure health literacy in Spanish could be reached.
Table 1.
Characteristics of Tools to Measure Health Literacy in Spanish.
| Author (date) |
Tool title | Purpose and context | Translation and cultural considerations |
Item number and skill(s) assessed |
Method of administration and feasibility |
Scoring | Validity | Reliability |
|---|---|---|---|---|---|---|---|---|
| Aguirre et al. (2005) | Article presents the validation of the Spanish Test of Functional Health Literacy Assessment (Spanish S- TOFHLA) |
|
|
|
|
|
|
|
| Coffman et al. (2012) | Spanish Nutrition Literacy Scale (NLS) |
|
|
|
|
|
|
|
| Cordasco et al. (2012), Sarkar et al. (2011) | Single Item Literacy Screener (SILS) |
|
|
|
|
|
|
|
| García et al. (2009) | No title specified |
|
|
|
|
|
|
|
| Lee et al. (2006) | Short Assessment of Health Literacy for Spanish- speaking Adults (SAHLSA) |
|
|
|
|
|
|
|
| Lee et al. (2010) | Short Assessment of Health Literacy —Spanish and English (SAHL- S&E) |
|
|
|
|
|
|
|
| Lee et al. (2013) | Oral Health Literacy Assessment in Spanish (OHLA-S) |
|
|
|
|
|
|
|
| Ownby et al. (2013) | Fostering Literacy for Good Health Today (FLIGHT)/Vive Desarollando Amplia Salud (VIDAS) |
|
|
|
|
|
|
|
| Parker et al. (1995) | Test of Functional Health Literacy in Adults— Spanish version (TOFHLA-S) |
|
|
|
|
|
|
|
| Rodriguez et al. (2015) | The Spanish language Rapid Estimate of Adult Literacy in Genetics (REAL-G-Sp) |
|
|
|
|
|
|
|
| Sauceda et al. (2012) | Medication Literacy Assessment in Spanish and English (MedLitRx SE) |
|
|
|
|
|
|
|
| Sorensen et al. (2013) | European Health Literacy Survey Questionnaire (HLS-EU-Q) |
|
|
|
|
|
|
|
| Villanueva Vilchis et al. (2015) | Spanish Oral Health Literacy Scale (SOHLS) |
|
|
|
|
|
|
|
| Weiss et al. (2005) | Newest Vital Sign (NVS) |
|
|
|
|
|
|
|
| White et al. (2011) | Diabetes Numeracy Test (DNT- 15 Latino) |
|
|
|
|
|
|
|
| Williams et al. (2013) | Breast Cancer Literacy Assessment Tool (Breast- CLAT) |
|
|
|
|
|
|
|
| Williams et al. (2013) | Cervical Cancer Literacy Assessment Tool (C-CLAT) |
|
|
|
|
|
|
|
| Yin et al. (2012) | Spanish Parental Health Literacy Activities Test (PHLAT Spanish) |
|
|
|
|
|
|
|
| Yost et al. (2009) | The Talking Touchscreen/ La Pantalla Parlanchina |
|
|
|
|
|
|
|
3. Results
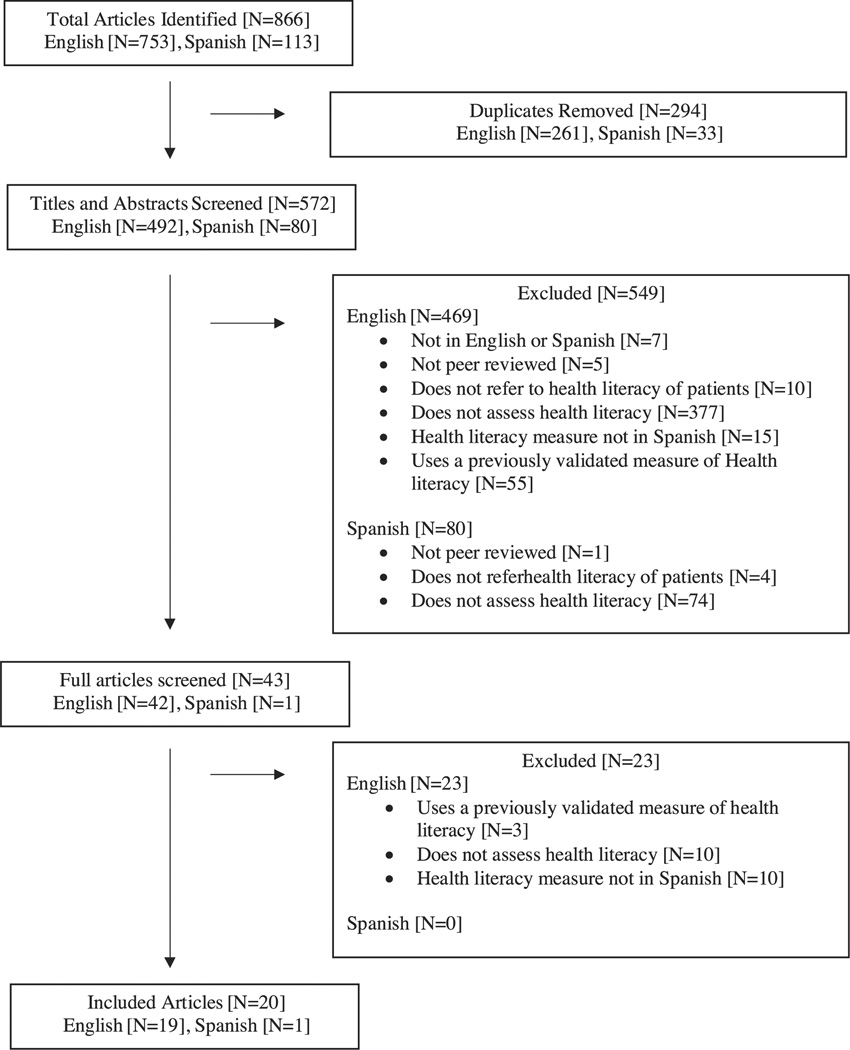
The search yielded 866 articles, 753 in the English search and 113 in the Spanish (Fig. 1). A total of 261 duplicates were excluded from the English and 33 from the Spanish articles. During the title and abstract screening, an additional 469 English and 80 Spanish articles were removed because they did not meet inclusion criteria. The full text of the remaining 43 English and one Spanish articles were reviewed by SS who is fluent in Spanish. Following the full text review, an additional 23 English articles were excluded.
Fig. 1.
Flow diagram of articles included and excluded in search.
Despite extensive search, the initial development of the Spanish version of the Shortened Test of Functional Health Literacy in Adults (S-TOFHLA), the most commonly used tool to assess health literacy in Spanish speakers, was not located. Only the development of the English, shortened version is available as are the directions for administration of the Spanish S-TOFHLA [29,49]. We, therefore, included the article, “Performance of the English and Spanish S-TOFHLA among publicly insured Medicaid and Medicare patients”, to demonstrate the psychometric testing of the instrument [34]. The Spanish article retained in the study did not specifically mention health literacy, but because the article met all other inclusion criteria and measured medication literacy in a similar way to one of the English language articles [50], it was included. Thus, the final sample consisted of 20 articles published between 1995 and 2015 (Fig. 1). The psychometric properties of the Spanish version of the three-question tool rapid screening tool, the Single Item Literacy Screener (SILS), were independently assessed in two separate studies that are included together in Table 1 [51,52]. The tool characteristics presented in Table 1 therefore include 20 articles [22,26,31,34,50–65] that describe the initial development and/or validation of 19 different tools.
3.1. Purpose and context
Tools were designed to measure either general health literacy or health literacy related to a specific condition such as nutrition or type of cancer, and their purpose was clearly stated in all 20 articles. The contexts in which tools were intended for administration were primary care or health promotion settings, in “any setting”, or among specific populations. All were developed for use with Spanish speaking adults with the exception of one [52], which tested the validity of the single item literacy screener (SILS) questions among bilingual speakers (Spanish and English) [52].
3.2. Translation and cultural considerations
Because most tools 15/19 (78.9%) [22,26,31,34,51,56–63,65] that measure health literacy in Spanish were created from a previously validated English tool, the method of translation and who conducted the translation for each tool were reviewed (Table 1). Professional translators, interdisciplinary teams of experts and bilingual or bicultural researchers or a Delphi process were used to develop or confirm 16 of the tools [22,26,31,50,51,53,54,56,57, 59–61,63–65], while the remaining three [34,55,58] did not report their translation process. The extent to which cultural meaning and word usage were maintained was also assessed for each tool; of the 15 tools that were translated into Spanish, 11 specified their intent to safeguard the meaning and usage of the words, phrases or concepts being translated [22,26,31,54,57–63]. The remaining four articles [34,51,56,65] did not refer to cultural considerations during their translation processes. The linguistic and cultural translation method of the two cancer literacy assessment tools [60,61] was further confirmed in an additional article by Rivera-Vasquez et al. [66]. Three tools were developed for specific subgroups, one among populations on the U.S.–Mexican border [50], the second among Spanish speaking parents of young children [62] and the third, for the adult Mexican population [64].
3.3. Health literacy skills assessed
Specific health literacy skills assessed in each of the 19 tools were identified based on a previously established health literacy skills taxonomy [3,4]. They included: reading comprehension, listening comprehension, confidence, responsibility, application/ function, conceptual knowledge, and numeracy. Reading comprehension was addressed by 14/19 (73.7%) of the articles [22,26,31,34,50,53–58,62–64]. After reading comprehension, numeracy was the second most assessed skill in 10/19 (52.3%) of tools [50,53,55,56,58,59,62–65]. Listening comprehension was assessed by two of the tools, the Vive Desarrollando Amplia Salud (VIDAS) [55], a computer administered instrument and the Rapid Estimate of Adult Literacy in Genetics (REAL-G-Sp) [65]. Confidence and responsibility were both assessed in the articles by Cordasco et. al. [51] and Sarkar et. al. [52] which aimed to identify individuals with limited health literacy based on their responses to three short questions previously validated in English [9,51,52,67]. Application/ function, the ability for an individual to use the information that they have just been presented, was assessed in 6/19 (31.6%) of the included tools [22,53,57,62–64].
3.4. Feasibility and method of administration
Feasibility was assessed by the estimated time required for a participant to complete the tool as well as the method of administration. Time estimates ranged from a matter of seconds in the case of the rapid screening instruments to upwards of 30 min. Administration time was not addressed in five of the articles [50,55,60,62,63]. Health literacy assessments were administered via computer, read allowed to participants, or required a patient or participant to complete a written questionnaire.
3.5. Scoring method
The scoring method for each tool depended on the type of question used, the health literacy skills assessed and how tools were administered. For example, computerized assessments detailed a computer-scored method and pronunciation tests are scored on a participant's ability to correctly pronounce a word whereas comprehension tests are based on correct association of two words. Most categorized the final scores generated from their assessment by the level of health literacy (e.g., inadequate, adequate and functional) depending on how participants scored. The specific method of scoring for four tools was not reported.
3.6. Validity and reliability
Most studies thoroughly described how the content for their tool was selected and reviewed and by whom. In 7/19 (36.8%) of tools, validity was assessed by comparing results of the newly developed tool to the S-TOFHLA [22,26,31,50,54,58,59], the accepted gold standard for health literacy measurement [9,68] and in 4/19 (21.1%), validity was established through comparisons to other tests of health literacy such as the Newest Vital Sign (NVS) or the Short Assessment of Health Literacy for Spanish-speaking Adults (SAHLSA) [22,54,55,65]. Other indicators associated with health literacy such as level of education or age, or self-assessment of health literacy were used to validate six (31.6%) tools [31,34,59,60,62,64]. Remaining tools confirmed validity through the use of differential item functioning, principal component analyses, factor analyses or by calculating sensitivity and specificity of the tool, comparison to other measures such as self-identified literacy or a combination of methods. Depending on the scoring method of each tool, dichotomous or ordinal, the reliability of instruments was assessed using the Kuder–Richardson or Cronbach’s alpha, respectively [69–71]. Cronbach’s alpha was reported in 13/19 (68.4%) of tools [26,31,34,53–58,60,61,64,65] and the Kuder–Richardson coefficient of reliability was used in 4/ 19 (21.1%) [22,50,59,62]. Two of the 19 tools (10.5%) did not report reliability (Table 1) [51,52,63].
4. Discussion and conclusion
4.1. Discussion
This integrative review identified 20 articles that described the development and psychometric testing of 19 tools to measure health literacy among Spanish speakers. Our findings indicate that tools vary widely in what they measure, the contexts in which they should be used, as well as the methods through which they were verified. These findings mirror results from other reviews of health literacy instruments [1,2,47], which present health literacy as a broad concept without well-defined constructs. Lack of consensus about the concept of health literacy limits comprehensive agreement on what components are necessary for tools to measure health literacy should entail. Nonetheless, the 19 tools that are available to measure health literacy in Spanish form a foundation that can further inform researchers and providers about how to more effectively address the healthcare needs of Spanish speaking populations.
Some have suggested that it is not necessary to screen for health literacy [72] and that patients completing a health literacy assessment may be embarrassed [2,61,73]; however, understanding patient’s strengths and limitations in acquiring and using health information is a necessary consideration for healthcare providers who are communicating health information to patients. Beyond the utility of health literacy measurement for providers, organizations can use health literacy measurement to inform patient-centered services such as enhancing patient involvement in service design, providing navigation assistance, creating education materials that are intelligible and verifying understanding at multiple points in a clinical visit [74,75]. Materials designed for low health literacy populations can include visuals as part of educational materials or content can be tailored to lower reading levels to maximize understandability [76,77]. Beyond organizational structure, interventions developed to address low health literacy have been associated with improvement in patient outcomes such as decreased levels of depression and increased ability to access and use preventive services [78,79]. Using the results presented in Table 1, professionals can select a tool that will improve understanding of patient’s ability to receive and use information in healthcare settings will help inform how these interventions and patient education materials are designed to more effectively meet the needs of Spanish speaking patients.
Native Spanish speakers living in the U.S. have to navigate a healthcare system and acquire and use information often presented to them in a language other than their own. It is the responsibility of organizations and providers to take note of discordant language concerns and take steps to appropriately provide care among these populations. As previously mentioned, health literacy assessments that are validated in Spanish only assess patients' ability to comprehend and use information that is presented to them in Spanish, not in English. However, the assessment of health literacy in either language can facilitate this understanding and inform the ability to tailor healthcare services and interventions to Spanish speakers. Tools to measure health literacy that are validated in Spanish are critical to inform the provision of language-appropriate care by illuminating the extent of language and educational differences. In this review, we found that health literacy instruments are not generally translated for specific cultural subgroups so caution must be used when selecting tools. Studies have shown that even if a country’s official language is Spanish, there may be different usages for specific words, and measurement instruments must be translated accordingly [80]. Further research is therefore needed to develop tools to measure health literacy in Spanish that are tailored to specific populations, contextually relevant, and psychometrically sound.
This study has several limitations. First, the Spanish literature search only included articles that have been indexed in large international databases. As a result, articles published in smaller, country-specific or less well-known journals may not have been identified. Second, the quality of the psychometrics was not assessed in a standardized way, as a tool does not exist to compare health literacy measurement tools. Further research should be conducted to define the concept of health literacy as well as the domains and skills that it contains to enable more effective comparisons across tools. Regardless of limitations, these findings will enable readers to identify the available and valid tools that measure health literacy in Spanish speaking populations as well as enhance their ability to select the most appropriate tool for the context in which they will use it.
4.2. Conclusion
Nineteen tools to measure health literacy that are validated in Spanish were identified through this review, but the extent of psychometric testing, health literacy skills measured, administration, scoring methods, and contexts in which they are intended for use varied between the instruments. Nevertheless, the use of any of these tools to assess health literacy can lead researchers, organizations, and individual clinicians to an enhanced understanding of Spanish speaking patient's health information needs. This study contributes to the literature by identifying and presenting the tools that have been validated to measure health literacy among Spanish speaking populations. This will aid individuals looking for tools to measure health literacy among Spanish speakers as well as form a foundation from which further research of health literacy instruments in Spanish can take place.
4.3. Practice implications
The effective measurement of health literacy can inform researchers, organizations and providers about how to mitigate challenges to providing high quality, cross-cultural healthcare [42,79,81]. This review is useful for any member of the healthcare community working with Spanish speaking adults to identify an appropriate tool to measure health literacy to inform healthcare services. Researchers will be able to use these results to both inform more effective health literacy instrument design as well as more effective tool selection relevant to specific study methods and settings. Similarly, healthcare organizations will be able to select a tool that lends itself to effective use among their context and patient population so that services may be more appropriately tailored to the specific needs of their patients, particularly those generated from language differences. Providers can use the shorter health literacy measurements in the clinical setting to quickly identify patients who may need information communicated at a more granular level. The use of health literacy measurement tools by all of these different healthcare professionals can inform better and more linguistically appropriate healthcare services for Spanish speaking patients. This can contribute to better healthcare services, improved healthcare outcomes [38] and lessen the healthcare disparities that are evident among Spanish speaking populations.
Acknowledgements
The authors would like to thank Lindsay Greenawalt, one of the informationists at Columbia University Medical Center, for her expert guidance during both the English and Spanish searches involved in this review.
Funding
The author, S. Stonbraker, is funded as a pre-doctoral fellow on the Training in Interdisciplinary Research to Prevent Infections (TIRI) grant, T32NR013454, funded by National Institute for Nursing Research, National Institutes of Health.
Contributor Information
Rebecca Schnall, Email: Rb897@Cumc.Columbia.edu.
Elaine Larson, Email: Ell23@Cumc.Columbia.edu.
References
- 1.Jordan J, Osborne R, Buchbinder R. Critical appraisal of health literacy indices revealed variable underlying constructs, narrow content and psychometric weaknesses. J. Clin. Epidemiol. 2011;64:366–379. doi: 10.1016/j.jclinepi.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 2.Mancuso J. Assessment and measurement of health literacy: an integrative review of the literature. Nurs. Health Sci. 2009;11:77–89. doi: 10.1111/j.1442-2018.2008.00408.x. [DOI] [PubMed] [Google Scholar]
- 3.Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12:1471–2458. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haun J, Valerio M, McCormack L, Sørensen K, Paasche-Orlow M. Health literacy measurement: an inventory and descriptive summary of 51 instruments. J. Health Commun. 2014;19:302–333. doi: 10.1080/10810730.2014.936571. [DOI] [PubMed] [Google Scholar]
- 5.Squiers L, Peinado S, Berkman N, Boudewyns V, McCormack L. The health literacy skills framework. J. Health Commun. 2012;17:30–54. doi: 10.1080/10810730.2012.713442. [DOI] [PubMed] [Google Scholar]
- 6.DeWalt D, Berkman N, Sheridan S, Lohr K, Pignone M. Literacy and health outcomes. J. Gen. Intern. Med. 2004;19:1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams M, Davis T, Parker R, Weiss B. The role of health literacy in patient–physician communication. Fam. Med. 2002;34:383–389. [PubMed] [Google Scholar]
- 8.Berkman N, Sheridan S, Donahue K, Halpern D, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann. Intern. Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 9.Chew L, Griffin J, Partin M, Noorbaloochi S, Grill J, Snyder A, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J. Gen. Intern. Med. 2008;23:5. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cortés D, Drainoni M, Henault L, Paasche-Orlow M. How to achieve informed consent for research from Spanish-speaking individuals with low literacy: a qualitative report. J. Health Commun. 2010;15:172–182. doi: 10.1080/10810730.2010.499990. [DOI] [PubMed] [Google Scholar]
- 11.Sorlie V, Lopez R. When language, health literacy, and miscommunication collide: tremors versus seizures. Fam. Med. 2011;43:48–50. [PubMed] [Google Scholar]
- 12.Scott T, Gazmararian J, Williams M, Baker D. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med. Care. 2002;40:395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Shieh C, Mays R, McDaniel A, Yu J. Health literacy and its association with the use of information sources and with barriers to information seeking in clinic-based pregnant women. Health Care Women Int. 2009;30:971–988. doi: 10.1080/07399330903052152. [DOI] [PubMed] [Google Scholar]
- 14.Parker R, Ratzan S, Lurie N. Health literacy: a policy challenge for advancing high-quality health care. Health Aff. 2003;22:147–153. doi: 10.1377/hlthaff.22.4.147. [DOI] [PubMed] [Google Scholar]
- 15.Coffman M, Norton C. Demands of immigration, health literacy, and depression in recent Latino immigrants. Home Health Care Manag. Pract. 2010:116–122. [Google Scholar]
- 16.Kickbusch I. Health literacy: addressing the health and education divide. Health Promot. Int. 2001;16:289–297. doi: 10.1093/heapro/16.3.289. [DOI] [PubMed] [Google Scholar]
- 17.Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000;15:259–267. [Google Scholar]
- 18.Andrus M, Roth M. Health literacy: a review. Pharmacotherapy. 2002;22:282–302. doi: 10.1592/phco.22.5.282.33191. [DOI] [PubMed] [Google Scholar]
- 19.Parker R, Kindig D. Beyond the Institute of Medicine health literacy report: are the recommendations being taken seriously? J. Gen. Intern. Med. 2006;21:891–892. doi: 10.1111/j.1525-1497.2006.00541.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peerson A, Saunders M. Health literacy revisited: what do we mean and why does it matter. Health Promot. Int. 2009;24:285–296. doi: 10.1093/heapro/dap014. [DOI] [PubMed] [Google Scholar]
- 21.Passel J, Cohn D, Lopez M. Hispanics Account for More Than Half of Nation’s Growth in Past Decade. Washington, D.C.: 2011. [Google Scholar]
- 22.Coffman M, La-Rocque S. Development and testing of the Spanish nutrition literacy scale. Hisp. Health Care Int. 2012;10:168–174. [Google Scholar]
- 23.U.S. Census Bureau, State and County QuickFacts. 2013 Retrieved April 2015 from http://quickfacts.census.gov/qfd/states/00000.html.
- 24.Jaimes N, Londono V, Halpern A. The term Hispanic/Latino: a note of caution. JAMA Dermatol. 2013;149:274–275. doi: 10.1001/jamadermatol.2013.1304. [DOI] [PubMed] [Google Scholar]
- 25.Pérez-Escamilla R. Acculturation, nutrition, and health disparities in Latinos. Am. J. Clin. Nutr. 2011;93:1163S–1167S. doi: 10.3945/ajcn.110.003467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee S, Bender D, Ruiz R, Cho Y. Development of an easy-to-use Spanish health literacy test. Health Serv. Res. 2006;41:1392–1412. doi: 10.1111/j.1475-6773.2006.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hemphill F, Vanneman A. Achievement Gaps: How Hispanic and White Students in Public Schools Perform in Mathematics and Reading on the National Assessment of Educational Progress. Washington, D.C.: 2011. [Google Scholar]
- 28.Perez-Escamilla R. Health care access among Latinos: implications for social and health care reforms. J. Hisp. High. Educ. 2010;9:43–60. [Google Scholar]
- 29.Baker D, Williams M, Parker R, Gazmararian J, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ. Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 30.Sutton M, Parks C. HIV/AIDS prevention, faith, and spirituality among black/ African American and Latino communities in the United States: strengthening scientific faith-based efforts to shift the course of the epidemic and reduce HIV-related health disparities. J. Relig. Health. 2013;52:514–530. doi: 10.1007/s10943-011-9499-z. [DOI] [PubMed] [Google Scholar]
- 31.Lee J, Stucky B, Rozier G, Lee S, Zeldin L. Oral health literacy assessment: development of an oral health literacy instrument for Spanish speakers. J. Public Health Dent. 2013;73:1–8. doi: 10.1111/jphd.12000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Koskan A, Friedman D, Messias D. Health literacy among Hispanics: a systematic research review (1992–2008) Hisp. Health Care Int. 2010;8:65–76. [Google Scholar]
- 33.Taylor W. “Cloze Procedure”: a new tool for measuring readability. J. Q. 1953;30:415–433. [Google Scholar]
- 34.Aguirre A, Ebrahim N, Shea J. Performance of the English and Spanish S-TOFHLA among publicly insured Medicaid and Medicare patients. Patient Educ. Couns. 2005;56:332–339. doi: 10.1016/j.pec.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 35.Nurss J, Baker D, Davis T, Parker R, Williams M. Difficulties in functional health literacy screening in Spanish-speaking adults. J. Read. 1995;63:2–7. [Google Scholar]
- 36.Hilton A, Skrutkowski M. Translating instruments into other languages: development and testing processes. Cancer Nurs. 2002;25:1–7. doi: 10.1097/00002820-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Sartorius N, Kuyken W. Translation of health status instruments, Quality of Life Assessment: International Perspective. Heidelberg, Germany: Springer-Verlag; pp. 19943–20018. [Google Scholar]
- 38.Paasche-Orlow M, Wolf M. The causal pathways linking health literacy to health outcomes. Am. J. Health Behav. 2007;31:S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 39.Motel S, Patten E. The 10 Largest Hispanic Origin Groups: Characteristics, Rankings, Top Counties. Washington, D.C.: 2012. [Google Scholar]
- 40.Reyna V, Nelson W, Han P, Dieckmann N. How numeracy influences risk comprehension and medical decision making. Psychol. Bull. 2009;135:943. doi: 10.1037/a0017327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rothman R, Housam R, Weiss H, Davis D, Gregory R, Gebretsadik T, et al. Patient understanding of food labels: the role of literacy and numeracy. Am. J. Prev. Med. 2006;31:391–398. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 42.Safeer R, Keenan J. Health literacy: the gap between physicians and patients. Am. Fam. Physician. 2005;72:463–468. [PubMed] [Google Scholar]
- 43.Whittemore R, Knafl K. The integrative review: updated methodology. J. Adv. Nurs. 2005;52:546–553. doi: 10.1111/j.1365-2648.2005.03621.x. [DOI] [PubMed] [Google Scholar]
- 44.Konfino J, Mejía R, Majdalani M, Pérez-Stable E. Alfabetización en salud en pacientes que asisten a un hospital universitario. Medicina (B Aires) 2009;69:631–634. [PMC free article] [PubMed] [Google Scholar]
- 45.Bonal R, Marzán D, Castillo F, Rubán Alfaro M. Alfabetización en salud en medicina general integral: perspectivas en Santiago de Cuba [Health literacy in comprehensive general medicine] Medisan. 2013;17:126–140. [Google Scholar]
- 46.Griffin J, Partin M, Noorbaloochi S, Grill J, Saha S, Snyder A, et al. Variation in estimates of limited health literacy by assessment instruments and non-response bias. J. Gen. Intern. Med. 2010;25:675–681. doi: 10.1007/s11606-010-1304-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Haun J, Luther S, Dodd V, Donaldson P. Measurement variation across health literacy assessments: implications for assessment selection in research and practice. J. Health Commun. 2012;17:141–159. doi: 10.1080/10810730.2012.712615. [DOI] [PubMed] [Google Scholar]
- 48.Miles M, Huberman A. Qualitative Data Analysis: An Expanded Sourcebook. Thousand Oaks: Sage Publications; 1994. [Google Scholar]
- 49.Nurss J, Parker R, Williams M, Baker D. Directions for administration and scoring and technical data, Short Test of Functional Health Literacy in Adults (STOFHLA-English and STOFHLA-Spanish) Center for the Study of Adult Literacy. 1998 [Google Scholar]
- 50.Sauceda J, Loya A, Sias J, Taylor T, Wiebe J, Rivera J. Medication literacy in Spanish and English: psychometric evaluation of a new assessment tool. J. Am. Pharm. Assoc. 2012;52:e231–e240. doi: 10.1331/JAPhA.2012.11264. [DOI] [PubMed] [Google Scholar]
- 51.Cordasco K, Homeier D, Franco I, Wang P, Sarkisian C. Health literacy screening of geriatric monolingual Spanish-speaking patients using single-item literacy screening questions and education. Health Educ. J. 2012;71:597–605. doi: 10.1177/0017896911411764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sarkar U, Schillinger D, Lopez A, Sudore R. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. J. Gen. Intern. Med. 2011;26:265–271. doi: 10.1007/s11606-010-1552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.García D, Gastelurrutia G, Baena P, Fisac L, Martínez M. Validation of a questionnaire to assess patient knowledge of their medicines. Aten. Primaria. 2009;41:661–668. doi: 10.1016/j.aprim.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee S, Stucky B, Lee J, Rozier R, Bender D. Short assessment of health literacy-spanish and english: a comparable test of health literacy for Spanish and English speakers. Health Serv. Res. 2010;45:1105–1120. doi: 10.1111/j.1475-6773.2010.01119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ownby R, Acevedo A, Waldrop-Valverde D, Jacobs R, Caballero J, Davenport R, et al. Development and initial validation of a computer-administered health literacy assessment in Spanish and English: FLIGHT/ VIDAS. Patient Relat. Outcome Meas. 2013;4:21–35. doi: 10.2147/PROM.S48384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Parker R, Baker D, Williams M, Nurss J. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J. Gen. Intern. Med. 1995;10:537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 57.Sorensen K, Van den Broucke S, Pelikan J, Fullam J, Doyle G, Slonska Z, et al. Measuring health literacy in populations: illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q) BMC Public Health. 2013;13:948. doi: 10.1186/1471-2458-13-948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Weiss B, Mays M, Martz W, Castro K, DeWalt D, Pignone M, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann. Fam. Med. 2005;3:514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.White R, Osborn C, Gebretsadik T, Kripalani S, Rothman R. Development and validation of a Spanish diabetes-specific numeracy measure: DNT-15 Latino. Diabetes Technol. Ther. 2011;13:893–898. doi: 10.1089/dia.2011.0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Williams K, Templin T, Hines R. Answering the call: a tool that measures functional breast cancer literacy. J. Health Commun. 2013;18:1310–1325. doi: 10.1080/10810730.2013.778367. [DOI] [PubMed] [Google Scholar]
- 61.Williams K, Templin T. Bringing the real world to psychometric evaluation of cervical cancer literacy assessments with Black, Latina, and Arab women in real-world settings. J. Cancer Educ. 2013;28:738–743. doi: 10.1007/s13187-013-0549-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yin H, Sanders L, Rothman R, Mendelsohn A, Dreyer B, White R, et al. Assessment of health literacy and numeracy among Spanish-speaking parents of young children: validation of the Spanish parental health literacy activities test (PHLAT Spanish) Acad. Pediatr. 2012;12:68–74. doi: 10.1016/j.acap.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yost K, Webster K, Baker D, Choi S, Bode R, Hahn E. Bilingual health literacy assessment using the Talking Touchscreen/la Pantalla Parlanchina: development and pilot testing. Patient Educ. Couns. 2009;75:295–301. doi: 10.1016/j.pec.2009.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Villanueva Vilchis M, Wintergerst A, Borges Yáñez S. Toward a comprehensive instrument of oral health literacy in Spanish. J. Health Commun. 2015:1–8. doi: 10.1080/10810730.2015.1018568. [DOI] [PubMed] [Google Scholar]
- 65.Rodríguez S, Roter D, Castillo-Salgado C, Hooker G, Erby L. Translation and validation of a Spanish-language genetic health literacy screening tool. Health Psychol. 2015;34:120. doi: 10.1037/hea0000162. [DOI] [PubMed] [Google Scholar]
- 66.Rivera-Vásquez O, Mabiso A, Hammad A, Williams K. A community-based approach to translating and testing cancer literacy assessment tools. J. Cancer Educ. 2009;24:319–325. doi: 10.1080/08858190902997373. [DOI] [PubMed] [Google Scholar]
- 67.Chew L, Bradley K, Boyko E. Brief questions to identify patients with inadequate health literacy. Fam. Med. 2004;11:588–594. [PubMed] [Google Scholar]
- 68.Morris N, MacLean C, Chew L, Littenberg B. The single item literacy screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam. Pract. 2006;7:21. doi: 10.1186/1471-2296-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mokkink L, Terwee C, Patrick D, Alonso J, Stratford P, Knol D, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual. Life Res. 2010;19:539–549. doi: 10.1007/s11136-010-9606-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Santos J. Cronbach’s alpha: a tool for assessing the reliability of scales. J. Ext. 1999;37:1–5. [Google Scholar]
- 71.Cureton E. The definition and estimation of test reliability. Educ. Psychol. Meas. 1958;18:715–738. [Google Scholar]
- 72.Paasche-Orlow M, Wolf M. Evidence does not support clinical screening of literacy. J. Gen. Intern. Med. 2008;23:100–102. doi: 10.1007/s11606-007-0447-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Parikh N, Parker R, Nurss J, Baker D, Williams M. Shame and health literacy: the unspoken connection. Patient Educ. Couns. 1996;27:33–39. doi: 10.1016/0738-3991(95)00787-3. [DOI] [PubMed] [Google Scholar]
- 74.Brach C, Keller D, Hernandez L, Baur C, Parker R, Dreyer B, et al. Ten Attributes of Health Literate Health Care Organizations. Washington, D.C.: National Academy of Sciences; pp. 20121–20130. [Google Scholar]
- 75.Pleasant A, Kuruvilla S. A tale of two health literacies: public health and clinical approaches to health literacy. Health Promot. Int. 2008;23:152–159. doi: 10.1093/heapro/dan001. [DOI] [PubMed] [Google Scholar]
- 76.Houts P, Doak C, Doak L, Loscalzo M. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ. Couns. 2006;61:173–190. doi: 10.1016/j.pec.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 77.Hansberry D, Agarwal N, Shah R, Schmitt P, Baredes S, Setzen M, et al. Analysis of the readability of patient education materials from surgical subspecialties. Laryngoscope. 2014;124:405–412. doi: 10.1002/lary.24261. [DOI] [PubMed] [Google Scholar]
- 78.Pignone M, DeWalt D, Sheridan S, Berkman N, Lohr K. Interventions to improve health outcomes for patients with low literacy. J. Gen. Intern. Med. 2005;20:185–192. doi: 10.1111/j.1525-1497.2005.40208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Stableford S, Mettger W. Plain language: a strategic response to the health literacy challenge. J. Public Health Policy. 2007;28:71–93. doi: 10.1057/palgrave.jphp.3200102. [DOI] [PubMed] [Google Scholar]
- 80.Casas F, Sarriera J, Abs D, Coenders G, Alfaro J, Saforcada E, et al. Subjective indicators of personal well-being among adolescents: Performance and results for different scales in Latin-language speaking countries: a contribution to the international debate. Child Indic. Res. 2012;5:1–28. [Google Scholar]
- 81.Parker R. Health literacy: a challenge for American patients and their health care providers. Health Promot. Int. 2000;15:277–283. [Google Scholar]