Abstract
A 60‐year‐old woman without a history of liver diseases, but with a history of regular alcohol consumption, presented with a right‐sided transudative pleural effusion. Neither parenchymal lung lesion nor pleural thickening was seen on a chest computed tomography. On abdominal ultrasonography, the liver size and contour were normal, and ascites was not noted. Despite performing imaging and laboratory studies, we could not find a cause of the pleural effusion. Thus, due to her history of regular alcohol consumption, we decided to measure liver stiffness using a transient elastography (Fibroscan®, EchosensTM, Paris, France), which showed a value of 35.3 kPa suggestive of liver cirrhosis. An intraperitoneal injection of a radioisotope demonstrated the transdiaphragmatic flow of fluid from peritoneal cavity to pleural cavity. The diagnosis was confirmed as hepatic hydrothorax. Management consisting of restricted salt and water intake with diuretics resulted in resolution of the hepatic hydrothorax.
Keywords: Ascites, hepatic hydrothorax, liver cirrhosis, transient elastography
Introduction
Hepatic hydrothorax is a pleural effusion caused by portal hypertension. Patients with hepatic hydrothorax usually have ascites, but a few cases without ascites have been reported. The most likely explanation of hepatic hydrothorax is ascites passing through a diaphragmatic defect. Pressure gradient‐directed, unidirectional flow of ascites occurs through a diaphragmatic defect into the pleural cavity [1]. The presence of a diaphragmatic defect can be established with the intraperitoneal injection of a technetium 99 m‐sulfur colloid [2].
Here we report a case of hepatic hydrothorax without ascites, which was the first sign of liver cirrhosis that was diagnosed with a transient elastography.
Case Report
A 60‐year‐old woman was hospitalized for a week‐long history of progressive dyspnea and general weakness. She had a medical history of diabetes mellitus and hypertension. She had ingested approximate 14 g/day of alcohol for 20 years. She was acutely ill‐looking and had an alert mental status. Upon admission, her vital signs included a blood pressure of 132/80 mmHg, pulse of 76/min, respiratory rate of 20/min, and body temperature of 36.8°C. Decreased breathing sounds and dullness to percussion were evident over the lower one‐third of the right hemithorax. No friction rub was auscultated. Heart sounds were regular and there was no murmur. The liver and spleen were not palpated. Palmar erythema, vascular spider, and peripheral edema were absent.
Initial laboratory data revealed albumin 3.2 g/dL, total protein 6.4 g/dL, lactate dehydrogenase (LDH) of 229 IU/L, aspartate transaminase/alanine aminotransferase of 33/24 IU/L, alkaline phosphatase of 801 IU/L, total bilirubin of 0.6 mg/dL, blood urea nitrogen/creatinine of 12.5/0.89 mg/dL, white blood cell (WBC) count of 3430/mm3, hematocrit of 38.4%, platelet count of 150,000/mm3, prothrombin time (international normalized ratio) of 1.08, C‐reactive protein of 0.07 mg/dL, and blood analysis of N‐terminal‐pro‐brain natriuretic peptide of 257 ng/mL. Urinalysis revealed no proteinuria. Hepatitis B surface antigen and hepatitis C antibody were not detected.
Chest X‐ray showed a significant right‐sided pleural effusion. A thoracentesis was performed and 1500 mL of the pleural effusion was drained. The pleural fluid was yellowish, and an analysis revealed a pH of 7.3, glucose of 212 mg/dL, LDH of 105 IU/L, protein of 3.0 g/dL, red blood cell count of 330/mm3, WBC count of 1/mm3, adenosine deaminase of 11.9 IU/L, and carcinoembryonic antigen of 2.5 mg/mL. Pleural fluid was transudate. Culture for bacteria as well as an acid‐fast bacillus smear and culture were negative. No malignant cells were observed.
A chest computed tomography scan revealed no parenchymal lung disease or pleural thickening. On abdominal ultrasonography, the liver size and contour were within the normal range without evidence of ascites, but the liver parenchymal echogenicity was slightly increased, which was suggestive of fatty liver. We also performed an esophagogastroduodenoscopy, which revealed gastric erosion but no esophageal varices. Echocardiography revealed no evidence of cardiac disease.
We repeated the thoracentesis every 3 days for 2 weeks and empirically prescribed diuretics. The collected fluids were also transudate, but the right‐sided pleural effusion was not improved.
Although laboratory findings and abdominal ultrasonography did not show the evidence of liver cirrhosis, due to her alcoholic history, we performed an examination using a transient elastography, which can measure liver stiffness. The transient elastography result was 35.3 Kpa, which was suggestive of liver cirrhosis. Accordingly, we suspected a hepatic hydrothorax in the absence of ascites. A radioisotope 99mTc‐sulfur colloid injected in peritoneal cavity resulted in a positive uptake of radioactivity within the right pleural cavity (Fig. 1 ). This finding suggested that the pleural effusion originated in the peritoneal cavity and that there was a diaphragmatic defect.
Figure 1.
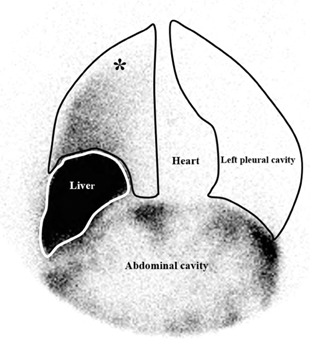
After the intraperitoneal injection of a 99mTc‐sulfur colloid, a positive uptake of radioactivity within right pleural cavity was found. *Right pleural cavity.
We diagnosed the patient as having hepatic hydrothorax without ascites, which was the first sign of alcoholic liver cirrhosis. Once the patient was started on a strict low salt diet and a water restriction with diuretics, the pleural effusion slowly regressed. After 2 months of treatment, the hydrothorax was resolved.
Discussion
Liver biopsy is the gold standard for the assessment of cirrhosis, but the risk of severe complications like bleeding and sampling error often occurs. Therefore, the assessment of liver fibrosis using a noninvasive technique is considered first [3]. In this case, since there was no definite evidence of liver cirrhosis on the abdominal ultrasonography or laboratory findings, it was difficult to suspect liver cirrhosis or proceed with a liver biopsy. Thus, we decided to measure liver stiffness using a transient elastography. The transient elastography has been demonstrated to be a reliable tool for assessing hepatic fibrosis and cirrhosis [4]. Using a threshold of 14.6 kPa on the transient elastography for liver cirrhosis, the positive predictive value was 74% and the negative predictive value was 94% in a study of 1007 patients with chronic liver disease by Ganne‐Carrie et al. [5].
The flow of ascites towards the pleural cavity is determined by the sum of negative pleural cavity pressure and positive abdominal pressure. When the pleural filling pressure equilibrates with negative pleural cavity pressure and positive abdominal pressure, the flow of ascites toward pleural cavity is stopped and ascites will be accumulated on abdominal cavity. But, if the pleural re‐absorption rate of ascites equilibrates with the production of ascites in abdominal cavity, hepatic hydrothorax without ascites will persist [6].
If pleural fluid is found in a patient with liver cirrhosis that does not have hypoalbuminemia and ascites, an alternative diagnosis should be considered. Despite this, we diagnosed liver cirrhosis using a transient elastography in a patient without evidence of liver cirrhosis and demonstrated that the pleural effusion originated from ascites using the intraperitoneal injection of a radioisotope. Moreover, the presentation of a significant pleural effusion without ascites as the first sign of liver cirrhosis is rare.
In conclusion, if a patient without a history of liver disease has the unclear cause of transudative pleural effusion, we might consider adding hepatic hydrothorax without ascites as a differential diagnosis.
Disclosure Statements
No conflict of interest declared.
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
References
- 1. Alberts WM, Salem AJ, Solomon DA, et al. 1991. Hepatic hydrothorax. Cause and management. Arch. Intern. Med. 151:2383–2388. [PubMed] [Google Scholar]
- 2. Daly JJ, Potts JM, Gordon L, et al. 1994. Scintigraphic diagnosis of peritoneo‐pleural communication in the absence of ascites. Clin. Nucl. Med. 19:892–894. [DOI] [PubMed] [Google Scholar]
- 3. Tovo CV, de Mattos AZ, Coral GP, et al. 2015. Noninvasive imaging assessment of non‐alcoholic fatty liver disease: Focus on liver scintigraphy. World J. Gastroenterol. 21:4432–4439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ziol M, Handra‐Luca A, Kettaneh A, et al. 2005. Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with chronic hepatitis C. Hepatology 41:48–54. [DOI] [PubMed] [Google Scholar]
- 5. Ganne‐Carrie N, Ziol M, de Ledinghen V, et al. 2006. Accuracy of liver stiffness measurement for the diagnosis of cirrhosis in patients with chronic liver diseases. Hepatology 44:1511–1517. [DOI] [PubMed] [Google Scholar]
- 6. Jimenez‐Saenz M, Venero J, Castro J, et al. 1990. Hepatic hydrothorax without ascites: A rare form of a common complication. J. R. Soc. Med. 83:747–748. [DOI] [PMC free article] [PubMed] [Google Scholar]


