Abstract
PURPOSE
To compare the push-out bond strength of feldspar and zirconia-based ceramic inlays bonded to dentin with different resin cements following simulated aging.
MATERIALS AND METHODS
Occlusal cavities in 80 extracted molars were restored in 2 groups (n=40) with CAD/CAM feldspar (Vitablocs Trilux forte) (FP) and zirconia-based (Ceramill Zi) (ZR) ceramic inlays. The fabricated inlays were luted in 2 subgroups (n=20) with either etch-and-bond (RelyX Ultimate Clicker) (EB) or self-adhesive (RelyX Unicem Aplicap) (SA) resin cement. Ten inlays in each subgroup were subjected to 3,500 thermal cycles and 24,000 loading cycles, while the other 10 served as control. Horizontal 3 mm thick specimens were cut out of the restored teeth for push out bond strength testing. Bond strength data were statistically analyzed using 1-way ANOVA and Tukey's comparisons at α=.05. The mode of ceramic-cement-dentin bond failure for each specimen was also assessed.
RESULTS
No statistically significant differences were noticed between FP and ZR bond strength to dentin in all subgroups (ANOVA, P=.05113). No differences were noticed between EB and SA (Tukey's, P>.05) bonded to either type of ceramics. Both adhesive and mixed modes of bond failure were dominant for non-aged inlays. Simulated aging had no significant effect on bond strength values (Tukey's, P>.05) of all ceramic-cement combinations although the adhesive mode of bond failure became more common (60-80%) in aged inlays.
CONCLUSION
The suggested cement-ceramic combinations offer comparable bonding performance to dentin substrate either before or after simulated aging that seems to have no adverse effect on the achieved bond.
Keywords: Inlays, Bonding, Ceramics, Resin cement, Dentin
INTRODUCTION
Current popularity of tooth-colored restorations is a normal response to increased esthetic demands of dental patients.1 Ceramic inlays were introduced to dentistry many decades back, however problems were encountered with the early types that have limited their application.1,2 Several laboratory studies3,4,5,6,7 assessed factors responsible for early ceramic inlay failures. Brittle fracture, loss of retention, marginal inaccuracy and unsatisfactory esthetics of the air fired porcelain were reported to be common. However, the evolution of many strengthened ceramic systems with sensible levels of success refreshed the attention to using ceramic restorations.8
Both glass-infiltrated and pressable glass ceramics were generally able to produce inlays with acceptable strength and fit.2 Lithium disilicate-based ceramics also showed similar ability to provide successful restorations.9 In order to save operators' and patients' time, machinable techniques became popular and many types of ceramic blocks/disks are currently available for either chair-side or laboratory inlay fabrication.9,10,11
Some studies12,13 reported similar clinical survival rates of current ceramic inlays to other materials in posterior region of the mouth. However, the clinical longevity of these restorations is usually governed by the strong and durable bonding to both ceramic and tooth.2 Achieving that goal can be feasible using contemporary resin-based luting cements and the new generation of bonding systems.14,15 Current ceramic bonding usually depends on chemomechanical conditioning of ceramic surfaces. Hydrofluoric acid etching and the application of silane primer are reported to help achieve successful adhesion of resin cement to glass ceramic surfaces.16 On the other hand, sandblasting is mandatory to mechanically retain cementing agents to the surfaces of zirconia-based ceramic surfaces.17
Despite the wide diversity in luting cements, none of the currently available materials is ideal for all situations. Etch-and-bond, dual-cured resin cements were known to achieve the desired bonding quality of different ceramic inlay restorations to tooth substrates.18,19 Some researchers20,21,22 reported years of acceptable clinical performance and declared fewer bulk fractures of ceramic inlays luted with those cements. However, their multi-step application possibly led to crucial errors and, in some instances, failure of cemented restoration.23 Accordingly, one-step self-adhesive resin cements were developed aiming to offset the drawbacks of etch-and-bond, dual-cured ones. Moreover, some researchers nominated the self-adhesive resin cement to be the best choice to lute zirconia-based ceramics.17,23
In spite of the revealed clinical success of ceramic inlays luted with different resin cements over respected periods in service19,20 a debate is there based on the common thought that the performance of ceramic-resin cement bond is adversely affected following aging simulation.24,25 Both cyclic fatigue and thermocycling were believed to lead to weakened bond and a predominance of adhesive failure at the interface between dual-cured resin cement and glass ceramic substrates.23 A weakened bond of self-adhesive resin cements to both glass and zirconia ceramics was also reported following laboratory-conducted thermocycling.25 The aforementioned findings may necessitate further studies to confirm the effect of simulating aging on the performance of contemporary ceramic-cement systems. The compatibility of inlay-cement system materials and the durability of their bonding could additionally influence such restorations' performance.2 Therefore, the present study aimed to compare the push-out bond strength of CAD/CAM feldspar and zirconia-based ceramic inlays luted to dentin using either etch-and bond, dual-cured or one-step, self-adhesive resin cements before and after artificial aging with cyclic fatigue loading and thermocycling. The suggested null hypothesis was that there is no difference between bond strength values of different ceramic-cement combinations following simulated aging.
MATERIALS AND METHODS
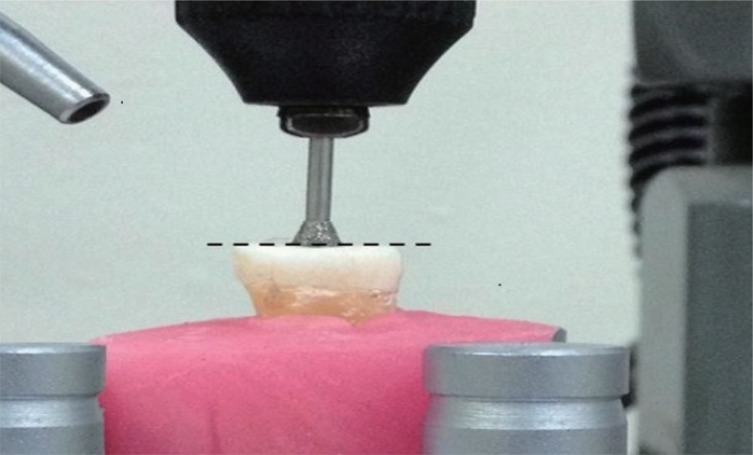
Eighty caries-free human molars extracted for periodontal reasons were collected at King Khalid University, College of Dentistry clinics. All teeth were ultrasonically cleaned to get rid of both soft and hard deposits and then stored in water at 4℃ (FLOCCHETTI, Frigoriferi Scientifici, Luzzara, Italy) for less than one month before coating their roots with a single layer of low viscosity rubber impression material (Imprint, 3M ESPE, St. paul, MN, USA) representing tooth periodontal ligament. In order to facilitate further handling, the rubber-coated roots were then embedded into acrylic blocks 3 cm in diameter and height (Hygenic, Coltene/Whaledent AG. Alstatten, Switzerland). The occlusal surfaces of all teeth were cut flat to expose dentin using Isomet precision saw machine (Isomet, Lake Bluff, IL, USA). Round diamond points (#001-018 DIA-BURS BR31, Mani Inc., Tochigi, Japan) were used in presence of copious water cooling to drill 2 mm deep through the center of occlusal dentine. The drilling procedure was subsequently continued with the same cooling protocol using double truncated cone diamond tips (#039/032 DIA-BURS EX11, Mani Inc., Tochigi, Japan) parallel to the long axis of each tooth till having occlusally diverged cavities with standard dimensions (3 and 1.5 mm in occlusal and pulpal diameters and 3 mm deep) (Fig. 1).
Fig. 1. Preparation of occlusal cavities (The dotted line indicates the standardized leveling of cavity depth).
Tooth cavities were optically scanned using Ceramil Map400 (Amann Girrbach, Kolbach, Austeria). Standardized inlay restorations were first designed with Ceramil Mind software 15 µm smaller than their respective cavities to allow uniform standardized space for the cementing material. The inlays were then milled on Ceramil Motion2 (Amann Girrbach, Kolbach, Austeria) out of 2 machinable ceramic materials; feldspar (FP) (Vitablocs Trilux forte, VITA Zahnfabrik, Bad Sackingen, Germany) (Group I, n = 40) and zirconia-based ceramic blocks (ZR) (Ceramill Zi, Amann Girrbach, Kolbach, Austria) (Group II, n = 40). Details of materials used are shown in Table 1.
Table 1. Materials used.
| Material | Description | Composition | Manufacturer |
|---|---|---|---|
| Vitablocs Trilux forte | Feldspar-based CAD/CAM ceramic blocks | Silicon oxide (SiO2), Aluminum oxide (Al2O3), Sodium oxide (Na2O), Potassium oxide (K2O), Calcium oxide (CaO), Titanium oxide (TiO2). | VITA Zahnfabrik, Bad Sackingen, Germany |
| Ceramill Zi | Zirconia-based CAD/CAM ceramic blocks | Zirconium oxide (ZrO2), Hafnium oxide (HfO2), Yttrium oxide(Y2O), Aluminum oxide (Al2O3) and other oxides | Amann Girrbach, Kolbach, Austria |
| Porcelain etchant | 9.5% Hydrofluoric acid gel | Hydrofluoric acid, sulphoric acid and ethanol | Bisco Inc., Schaumburg, IL, USA |
| ESPE Sil | Silane coupling agent | Ethyl alcohol, Methacryloxypropyltrimethoxysilane, methyl ethyl ketone | 3M ESPE, St. Paul, MN, USA |
| Scotchbond Universal Etchant | Acid etch | 35% phosphoric acid gel | 3M ESPE, St. Paul, MN, USA |
| RelyX Ultimate Clicker | Etch-and-Bond, dual-cured resin cement | Base paste: methacrylate monomers, Radiopaque, silanated fillers, initiator, stabilizers, rheological additives | 3M ESPE, St. Paul, MN, USA |
| Catalyst paste: Methacrylate monomers, radiopaque alkaline fillers, initiators, stabilizers, pigments, rheological additives, fluorescence dye, dual-cure activator for single bond universal adhesive | |||
| RelyX Unicem Aplicap | Self-Adhesive resin luting cement | Powder: Alkaline fillers, silanated fillers, initiator components, pigments | 3M ESPE, St. Paul, MN, USA |
| Liquid: methacrylate monomers containing phosphoric acid groups, methacrylate monomers, initiator components, stabilizers | |||
| Single Bond Universal Adhesive | Total etch, 2-step resin adhesive | MDP phosphate-monomer dimethacrylate resins, HEMA, vitrbond Copolymer, filler, ethanol, water, initiators and silane | 3M ESPE, St. Paul, MN, USA |
Before cementing the fabricated inlays to their respective cavities, their fitting surfaces were first treated according to the manufacturers' recommendation of the used cements. FP inlays were first etched with 9.5% hydrofluoric acid gel (HF) (Porcelain etchant, Bisco Inc., Schaumburg, IL, USA) for 90 seconds, rinsed and air dried. Using custom-made nozzle holder adjusted 40 mm away and 45° on the surfaces; ZR inlays were bombarded with a mixture of 50 and 110 µm alumina (Al2O3) particles for 10 seconds using a pressure of 250 KPa21 following their dense sintering in Ceramil Therm high temperature furnace (Amann Girrbach, Kolbach, Austeria) at 1400℃ for 120 minutes.26 Sandblasted inlays were then subjected to thorough cleaning with alcohol and air dried. Inlays in each group were then luted to their respective cavities in 2 subgroups (n=20 each) using etch-and-bond dual-cured resin cement (EB) (RelyX Ultimate Clicker, 3M ESPE, St. Paul, MN, USA) and self-adhesive luting cement (SA) (RelyX Unicem Aplicap, 3M ESPE) following their manufacturer's instructions.
In subgroup 1, cavity surfaces were acid etched with 35% phosphoric acid gel (Scotchbond Universal Etchant, 3M ESPE) for 15 seconds, washed with air-water spray and blot dried. Two successive coats of single component adhesive (Single Bond Universal Adhesive, 3M ESPE), each was agitated against etched dentin surfaces for 15 seconds, air thinned for 5 seconds followed by 10 seconds of light curing (Elipar S10, 3M ESPE AG, Seefeld, Germany). Roughened surfaces of FP and ZR inlay surfaces were then received a uniform coat of Single Bond Universal resin adhesive (3M ESPE) and light curing for 10 seconds before their cementation. Equal amounts of cement pastes were dispensed and mixed for 45 seconds to a uniform consistency on a paper pad. The mixed cement was first applied into the prepared cavities, after then inlays were seated in using firm hand pressure followed with a constant loading of 5 N.27 The excess cement was immediately removed with sponge pellet and the exposed margins were covered with glycerin gel to ensure complete polymerization in contact with air. In subgroup 2, tooth cavities were only rinsed with water and lightly dried. Further silanization with ESPE Sil (3M ESPE) was only considered before cementation of HF acid-etched FP inlays. RelyX Unicem Aplicaps were then activated for 4 seconds and automatically mixed for 15 seconds on CapMix mixing unit (3M ESPE). An Aplicap applicator was then used to dispense the mixed cement into the prepared cavities. The inlay restorations were then seated into their respective cavities, following the previously mentioned protocol, and the cement excess was allowed to reach its gel state before its removal with sharp scaler. Half the number of cemented inlays in each subgroup (Class A, n=10) were only stored in water at 37 ± 1℃ for 24 hours (FUNCTION Line, Thermo Electronic Inc., Lagenselbold, Germany) to serve as control. The remaining teeth in each subgroup (Class B, n=10) were subjected to cyclic fatigue on a universal testing machine (Model 5965, Instron, Grove City, PA, USA) using a vertical constant loading of 50 N for 240,000 cycles.28 Same specimens were then subjected to 5-55℃ thermocycling (MSCT-1, São Carlos, SP, Brazil) following ISO-TR 11405 Standard for 3,500 cycles with a dwell time of 30 seconds.10,29
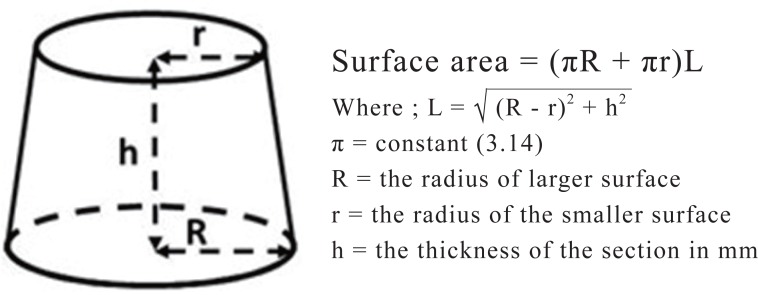
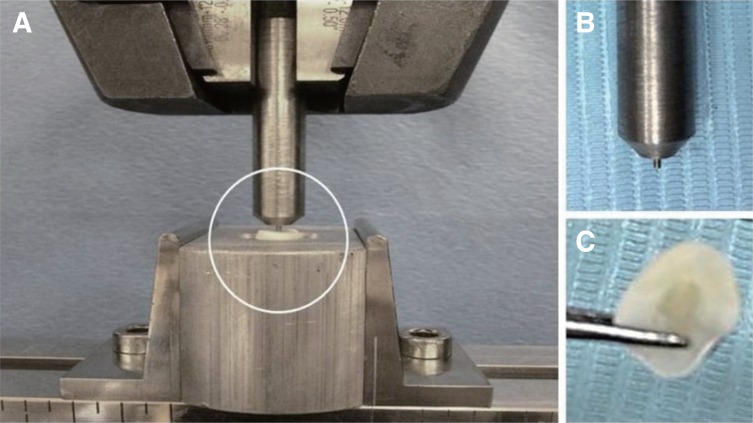
All restored teeth were cut horizontally 3 mm away from their flat occlusal surfaces, using low speed precision saw, to separate one disk specimen out of each. All specimens were then finished to the exact inlay's thickness (approximately 3 mm) on a serial grit polishing machine (Arotec APL 4; Arotec Ind. Com., São Paulo, SP, Brazil) exposing pulpal and occlusal inlay surfaces with no remains of cementing material. Following finishing, all sectioned specimens were inspected under low angle illumination at X10 original magnification to ensure complete removal of cement remains and absence of cracks within ceramic or tooth substrate. The exact thickness of each specimen was then measured using electronic caliper (Mitutoyo, Kawasaki, Japan) and recorded for further calculation of the bonded surface area using the formula shown in Figure 2.30 Using specially designed holder, all specimens were fixed onto the lower member of universal testing machine with their pulpal surface facing up. A flat-ended metal rod with a tip diameter of 1mm moving at a crosshead speed of 1.0 mm/min was used to stress the cemented inlays on compression (Fig. 3). The maximum load at failure was recorded for each specimen and the push-out bond strength value was then calculated in respect to its bonded surface area. Fractured specimens were then inspected at ×10 using a stereomicroscope (MSM 400, Mitutoyo, Kawasaki, Japan) to determine the mode of bond failure. The detected failure modes were then classified as cohesive, for fractures within the body of dentin, cement or ceramic substrate; adhesive, for total separation at dentin-cement or ceramic-cement interface; or mixed, for combined adhesive and cohesive failure criteria. The collected data for both control and test specimens' classes were statistically analyzed using 1-way ANOVA at α=0.05 to determine the existence of differences between their push-out bond strength values. Tukey's comparisons (α=0.05) were then considered to identify the significance of the detected differences.
Fig. 2. Calculation of the bonded surface area.
Fig. 3. Testing push-out bond strength (A) Stressing test specimens on compression, (B) Flat-ended indenter and (C) test specimen.
RESULTS
The mean bond strength values and standard deviations in different test subgroups before (Control) and after simulated aging were presented in Table 2, while the reported incidences of different bond failure modes were presented in Table 3. Initial statistical analysis of the collected results using 1-ANOVA showed no differences between the bond strength values of different classes (P = .05113). Further Tukey's comparisons also indicated no significant differences (P = .9856, .7985, .9674 and .8835) between the bond strength of both types of ceramic materials to dentin in different classes of test specimens. At the same time, no preference was noticed between the used types of cements (Tukey's comparisons, P = .909, .5685, .9908 and .9486). Simulated aging using cyclic fatigue loading and thermocycling had no significant effect (Tukey's comparisons, P = .9795, .9996, .9566 and 1.0) on the recorded bond strength values of different ceramic-cement combinations in comparison to their control counterparts.
Table 2. Push-out bond strength values (MPa) of different ceramic inlay materials to dentin.
| Ceramic material | Mean bond strength | |||
|---|---|---|---|---|
| Etch-and-Bond cement (EB) | Self-adhesive cement (SA) | |||
| Non-aged | Aged | Non-aged | Aged | |
| Feldspar-based ceramic (FP) | 6.33 ± 1.80a | 5.74 ± 1.71a | 5.55 ± 1.46a | 5.23 ± 1.09a |
| Zirconia-based ceramic (ZR) | 5.77 ± 0.96a | 5.10 ± 0.97a | 4.62 ± 1.59a | 4.41 ± 1.12a |
FP = Feldspar-based ceramic, ZR = Zirconia-based ceramic, EB = Etch-and-Bond cement, SA = Self-adhesive cement
Same superscript letters indicate no significant difference between classes of test specimens (Tukey's comparisons, P > .05).
Table 3. Incidence of bond failure modes.
| Mode of bond failure | Incidence (%) of bond failures | |||||||
|---|---|---|---|---|---|---|---|---|
| Feldspar-based ceramic (FP) | Zirconia-based ceramic (ZR) | |||||||
| Etch-and Bond cement (EB) | Self-adhesive cement (SA) | Etch-and-Bond cement (EB) | Self-adhesive cement (SA) | |||||
| Non-aged | Aged | Non-aged | Aged | Non-aged | Aged | Non-aged | Aged | |
| Adhesive (D) | 40 | 10 | 20 | 40 | 10 | 40 | 40 | 30 |
| Adhesive (C) | 40 | 70 | 20 | 20 | 30 | 40 | 40 | 40 |
| Mixed | 20 | 20 | 60 | 40 | 60 | 20 | 20 | 30 |
| Cohesive (D) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cohesive (C) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
D = Dentin interface, C = Ceramic interface, FP = feldspar-based ceramic, ZR = Zirconia-based ceramic, EB = Etch-and-Bond cement, SA = Self-adhesive cement
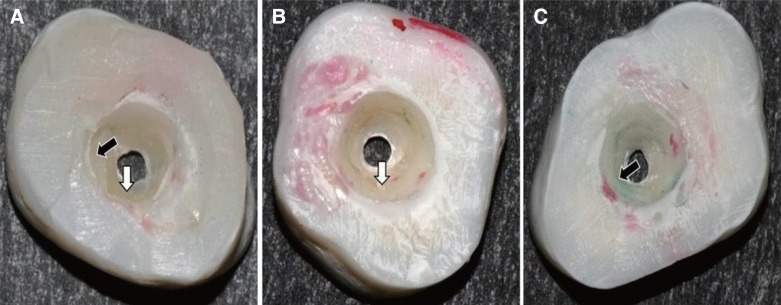
For the non-aged inlays (Control), the mixed mode of bond failure (Fig. 4A) was dominant (60%) with FP and ZR specimens luted with SA and EB respectively. The total incidences of adhesive failures were, in contrary, dominant (80%) with FB and ZR inlays luted to dentin with EB and SA respectively, However, the recorded incidence of adhesive failures were evenly distributed between both dentin-cement and ceramic-cement interfaces (40% of tested inlays for each interface) (Fig. 4B and Fig. 4C). Simulated aging using cyclic fatigue loading and thermocycling was reflected negatively on the mode of bond failures, where most of the tested inlays showed adhesive type of bond failure (60-80%), however the recorded incidences were unevenly distributed between dentin-cement and ceramic-cement interfaces (Table 3). At the same time, the highest incidence of the mixed mode of bond failures (40%) was recorded for FP specimens luted with SA, while the lowest mixed incidences were noticed with FP and ZR specimens luted with EB. None of the aged and non-aged inlays showed cohesive type of bond failure in the body of either dentin or ceramic substrate.
Fig. 4. Recorded modes of bond failure. (A) Mixed failure (white arrow indicates dentin substrate and the black arrow indicates cement material), (B) Adhesive bond failure at dentin-cement interface (white arrow indicates dentin substrate), (C) Adhesive failure at ceramic-cement interface (black arrow indicates cement material).
DISCUSSION
Both feldspar and zirconia-based ceramics are known materials for chair-side and laboratory CAD/CAM inlays.2,31 However, the clinical longevity of these restorations normally relies on their durable bonding to tooth substrates.14,32 Since the achievement of the desired bond is dependent on the participating materials, it is necessary to compare the bonding performance of different ceramic-resin cement combinations in respect to the wide range of materials available in dental market.2,17 The present study, accordingly, aimed to compare the bonding values of both feldspar and zirconia-based ceramics to tooth structure using either etch-and-bond, dual-cured or self-adhesive resin cement. The selected cements have proved acceptable laboratory and clinical bonding of different ceramic inlay materials to tooth structures.14,15,19,20,21,22,23 However, that bond is believed to be adversely affected on aging.24,25 Therefore, the influence of 240,000 loading cycles and 3,500 of thermal cycles were also considered in this study to simulate the effect of one year of aging on the efficiency of ceramic-cement-dentin adhesive bond.10,28,29
The push-out bond strength test was selected to assess the efficiency of bonding of different ceramic-cement combinations to tooth dentin due to its ability to demonstrate more homogenous stress distribution at the bonding interfaces.33 Moreover, this test was preferably selected to evaluate the adhesive junction when brittle materials are included.34 The null hypothesis of this in vitro study was that there is no difference between bond strength values of different ceramics-cement combinations following simulated aging. This hypothesis should be accepted in response to the recorded results that revealed no difference in bond strength values of both types of ceramic materials to dentin within each of the tested subgroups. This finding could be attributed to the ability of ceramic surface preparation protocols used to achieve reasonable means of ceramic-cement bonding. Etching of FP surfaces using hydrofluoric acid provided valuable means of cement micromechanical attachment. In addition, the application of the less viscous silane coupling agent into the created micro-irregularities helped achieving chemo-mechanical bonding to the etched ceramic surfaces.17 On the other hand, sandblasting of ZR surfaces provided the same opportunity for the cementing materials to have micromechanical attachment to the roughened ceramic surfaces.17 This postulation was supported with the results of both Queiroz et al.35 and Souza et al.,36 that necessitated the roughening process before the application of priming agents. Other researchers37 additionally recommended the application of resin primers with the ability to bond chemically to the properly roughened ceramic surfaces seeking for higher bond strength.
At the same time, no differences in bond strength values were noticed between the two types of cements (EB and SA) used to lute either type of ceramic inlays. This finding came in disagreement with the results of Viotti et al.,38 and Souza et al.,36 who indicated lower bond strength of self-adhesive cements to dentin and ceramics than conventional (etch-and-bond) resin cements. On contrary, Abdelaziz et al.,17 reported higher bond strength of self-adhesive cement to zirconia substrates following their sandblasting. Results of Feitosa et al.,39 also indicated higher bond strength of self-adhesive cements to roughened feldspar-based ceramic substrates. The comparable performance of both cement systems in this study probably related to the efficient penetration into surface irregularities of the roughened ceramic surfaces. The self-adhesive cement probably got this advantage based on its thixotropic property that allowed its significant flow and subsequent micromechanical attachment into ceramics' surface irregularities.40
Aging of test samples was carried out to simulate the inservice conditions. Using 3,500 cycles of thermal changes together with 240,000 cycles of fatigue loading were selected to resemble one year of clinical service.10,28,29 Regardless the type of resin cement used, many studies25,36,41,42,43 revealed an adverse effect of thermocycling on their bond strength to zirconia and feldspar-based ceramics. Another study24 also showed a significant reduction in bond strength values of resin cement to ceramic following simulated aging applying cyclic fatigue loading. Those findings disagreed with the results of the current study that showed no statistically significant effect of both thermocycling and cyclic fatigue loading on ceramic-cement-dentin bond strength. The recorded results were probably related to the ability of current resin cement formulations to offer durable bonding under simulated aging conditions.22,44 The proved micromechanical attachment of the cements used to roughened ceramic surfaces may also contribute to the achieved results.17 Several researchers supported the outcomes of the current study as they reported no significant effect of different aging conditions on resin cements-ceramic bonding.45,46,47
Regardless the type of luting cement, the majority of the noticed modes of bond failure, in all test groups before and after simulated aging, were belonging to the adhesive type either at dentine-cement or ceramic-cement interface. These findings were in agreement with that of Flury et al.,48 who studied the push-out bond strength of CAD/CAM ceramic inlays luted to dentin with resin cements and reported predominance of adhesive mode of failure at the cement-dentin interface. Another study by Aleisa et al.,49 also supported the predominance of adhesive failure at zirconia-resin cement interface. They referred this observation to the difficulty to establish strong bond to zirconia surfaces, in addition to lower stability of the created bond on aging. The incidence of the mixed type combining both adhesive failure at cement-dentin interface and cohesive failure within cement body was decreased in most of the test groups following simulated aging of the tested samples. This observation possibly was the result of the bonding fatigue in response to difference in coefficient of thermal expansion and water sorption during thermocycling in addition to the mechanical stresses expressed at the time of cyclic fatigue loading. These factors may increase the incidence of adhesive failures at the expense of the mixed type.47,50 Findings and limitations of this in vitro study, accordingly, necessitate further evaluation of ceramic-cement-dentin bonding performance following prolonged aging.
CONCLUSION
The suggested cement-ceramic combinations offer comparable bonding performance to dentin substrate either before or after simulated aging that seems to have no adverse effect on the achieved bond.
References
- 1.Banks RG. Conservative posterior ceramic restorations: a literature review. J Prosthet Dent. 1990;63:619–626. doi: 10.1016/0022-3913(90)90316-5. [DOI] [PubMed] [Google Scholar]
- 2.Hopp CD, Land MF. Considerations for ceramic inlays in posterior teeth: a review. Clin Cosmet Investig Dent. 2013;5:21–32. doi: 10.2147/CCIDE.S42016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kawai K, Hayashi M, Torii M, Tsuchitani Y. Marginal adaptability and fit of ceramic milled inlays. J Am Dent Assoc. 1995;126:1414–1419. doi: 10.14219/jada.archive.1995.0053. [DOI] [PubMed] [Google Scholar]
- 4.Krejci I, Lutz F, Reimer M. Marginal adaptation and fit of adhesive ceramic inlays. J Dent. 1993;21:39–46. doi: 10.1016/0300-5712(93)90048-u. [DOI] [PubMed] [Google Scholar]
- 5.Thordrup M, Isidor F, Hörsted-Bindslev P. Comparison of marginal fit and microleakage of ceramic and composite inlays: an in vitro study. J Dent. 1994;22:147–153. doi: 10.1016/0300-5712(94)90198-8. [DOI] [PubMed] [Google Scholar]
- 6.Dietschi D, Maeder M, Meyer JM, Holz J. In vitro resistance to fracture of porcelain inlays bonded to tooth. Quintessence Int. 1990;21:823–831. [PubMed] [Google Scholar]
- 7.Leinfelder KF. Porcelain esthetics for the 21st century. J Am Dent Assoc. 2000;131:47S–51S. doi: 10.14219/jada.archive.2000.0402. [DOI] [PubMed] [Google Scholar]
- 8.Tyas MJ. Dental amalgam-what are the alternatives? Int Dent J. 1994;44:303–308. [PubMed] [Google Scholar]
- 9.Beier US, Kapferer I, Dumfahrt H. Clinical long-term evaluation and failure characteristics of 1,335 all-ceramic restorations. Int J Prosthodont. 2012;25:70–78. [PubMed] [Google Scholar]
- 10.Critchlow S. Ceramic materials have similar short term survival rates to other materials on posterior teeth. Evid Based Dent. 2012;13:49. doi: 10.1038/sj.ebd.6400860. [DOI] [PubMed] [Google Scholar]
- 11.Molin M, Karlsson S. The fit of gold inlays and three ceramic inlay systems. A clinical and in vitro study. Acta Odontol Scand. 1993;51:201–206. doi: 10.3109/00016359309040568. [DOI] [PubMed] [Google Scholar]
- 12.Martin N, Jedynakiewicz NM. Interface dimensions of CEREC-2 MOD inlays. Dent Mater. 2000;16:68–74. doi: 10.1016/s0109-5641(99)00089-5. [DOI] [PubMed] [Google Scholar]
- 13.Nathanson D. Etched porcelain restorations for improved esthetics, part II: Onlays. Compendium. 1987;8:105–110. [PubMed] [Google Scholar]
- 14.Jensen ME, Sheth JJ, Tolliver D. Etched-porcelain resinbonded full-veneer crowns: in vitro fracture resistance. Compendium. 1989;10:336–338. 340–341, 344–347. [PubMed] [Google Scholar]
- 15.Dietschi D, Maeder M, Meyer JM, Holz J. In vitro resistance to fracture of porcelain inlays bonded to tooth. Quintessence Int. 1990;21:823–831. [PubMed] [Google Scholar]
- 16.Llobell A, Nicholls JI, Kois JC, Daly CH. Fatigue life of porcelain repair systems. Int J Prosthodont. 1992;5:205–213. [PubMed] [Google Scholar]
- 17.Abdelaziz KM, Al-Qahtani NM, Al-Shehri AS, Abdelmoneam AM. Bonding quality of contemporary dental cements to sandblasted esthetic crown copings. J Investig Clin Dent. 2012;3:142–147. doi: 10.1111/j.2041-1626.2011.00106.x. [DOI] [PubMed] [Google Scholar]
- 18.Frankenberger R, Lohbauer U, Schaible RB, Nikolaenko SA, Naumann M. Luting of ceramic inlays in vitro: marginal quality of self-etch and etch-and-rinse adhesives versus self-etch cements. Dent Mater. 2008;24:185–191. doi: 10.1016/j.dental.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 19.Taschner M, Krämer N, Lohbauer U, Pelka M, Breschi L, Petschelt A, Frankenberger R. Leucite-reinforced glass ceramic inlays luted with self-adhesive resin cement: a 2-year in vivo study. Dent Mater. 2012;28:535–540. doi: 10.1016/j.dental.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Santos MJ, Mondelli RF, Navarro MF, Francischone CE, Rubo JH, Santos GC., Jr Clinical evaluation of ceramic inlays and onlays fabricated with two systems: five-year follow-up. Oper Dent. 2013;38:3–11. doi: 10.2341/12-039-C. [DOI] [PubMed] [Google Scholar]
- 21.Frankenberger R, Taschner M, Garcia-Godoy F, Petschelt A, Krämer N. Leucite-reinforced glass ceramic inlays and onlays after 12 years. J Adhes Dent. 2008;10:393–398. [PubMed] [Google Scholar]
- 22.Sjgren G, Molin M, van Dijken JW. A 10-year prospective evaluation of CAD/CAM-manufactured (Cerec) ceramic inlays cemented with a chemically cured or dual-cured resin composite. Int J Prosthodont. 2004;17:241–246. [PubMed] [Google Scholar]
- 23.Krämer N, Frankenberger R. Clinical performance of bonded leucite-reinforced glass ceramic inlays and onlays after eight years. Dent Mater. 2005;21:262–271. doi: 10.1016/j.dental.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 24.Guarda GB, Correr AB, Gonçalves LS, Costa AR, Borges GA, Sinhoreti MA, Correr-Sobrinho L. Effects of surface treatments, thermocycling, and cyclic loading on the bond strength of a resin cement bonded to a lithium disilicate glass ceramic. Oper Dent. 2013;38:208–217. doi: 10.2341/11-076-L. [DOI] [PubMed] [Google Scholar]
- 25.Zorzin J, Belli R, Wagner A, Petschelt A, Lohbauer U. Self-adhesive resin cements: adhesive performance to indirect restorative ceramics. J Adhes Dent. 2014;16:541–546. doi: 10.3290/j.jad.a33201. [DOI] [PubMed] [Google Scholar]
- 26.Stawarczyk B, Ozcan M, Hallmann L, Ender A, Mehl A, Hämmerlet CH. The effect of zirconia sintering temperature on flexural strength, grain size, and contrast ratio. Clin Oral Investig. 2013;17:269–274. doi: 10.1007/s00784-012-0692-6. [DOI] [PubMed] [Google Scholar]
- 27.Flury S, Lussi A, Peutzfeldt A, Zimmerli B. Push-out bond strength of CAD/CAM-ceramic luted to dentin with self-adhesive resin cements. Dent Mater. 2010;26:855–863. doi: 10.1016/j.dental.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 28.Heintze SD, Faouzi M, Rousson V, Ozcan M. Correlation of wear in vivo and six laboratory wear methods. Dent Mater. 2012;28:961–973. doi: 10.1016/j.dental.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 29.Subramanian D, Sivagami G, Sendhilnathan D, Rajmohan C. Effect of thermocycling on the flexural strength of porcelain laminate veneers. J Conserv Dent. 2008;11:144–149. doi: 10.4103/0972-0707.48835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hashem AA, Ghoneim AG, Lutfy RA, Fouda MY. The effect of different irrigating solutions on bond strength of two root canal-filling systems. J Endod. 2009;35:537–540. doi: 10.1016/j.joen.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 31.Martin N, Jedynakiewicz NM. Clinical performance of CEREC ceramic inlays: a systematic review. Dent Mater. 1999;15:54–61. doi: 10.1016/s0109-5641(99)00014-7. [DOI] [PubMed] [Google Scholar]
- 32.Dietschi D, Maeder M, Meyer JM, Holz J. In vitro resistance to fracture of porcelain inlays bonded to tooth. Quintessence Int. 1990;21:823–831. [PubMed] [Google Scholar]
- 33.Soares CJ, Santana FR, Castro CG, Santos-Filho PC, Soares PV, Qian F, Armstrong SR. Finite element analysis and bond strength of a glass post to intraradicular dentin: comparison between microtensile and push-out tests. Dent Mater. 2008;24:1405–1411. doi: 10.1016/j.dental.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 34.Cheylan JM, Gonthier S, Degrange M. In vitro push-out strength of seven luting agents to dentin. Int J Prosthodont. 2002;15:365–370. [PubMed] [Google Scholar]
- 35.Queiroz JR, Souza RO, Nogueira Junior L, Jr, Ozcan M, Bottino MA. Influence of acid-etching and ceramic primers on the repair of a glass ceramic. Gen Dent. 2012;60:e79–e85. [PubMed] [Google Scholar]
- 36.Souza RO, Castilho AA, Fernandes VV, Bottino MA, Valandro LF. Durability of microtensile bond to nonetched and etched feldspar ceramic: self-adhesive resin cements vs conventional resin. J Adhes Dent. 2011;13:155–162. doi: 10.3290/j.jad.a18784. [DOI] [PubMed] [Google Scholar]
- 37.Valandro LF, Ozcan M, Bottino MC, Bottino MA, Scotti R, Bona AD. Bond strength of a resin cement to high-alumina and zirconia-reinforced ceramics: the effect of surface conditioning. J Adhes Dent. 2006;8:175–181. [PubMed] [Google Scholar]
- 38.Viotti RG, Kasaz A, Pena CE, Alexandre RS, Arrais CA, Reis AF. Microtensile bond strength of new self-adhesive luting agents and conventional multistep systems. J Prosthet Dent. 2009;102:306–312. doi: 10.1016/S0022-3913(09)60180-3. [DOI] [PubMed] [Google Scholar]
- 39.Feitosa SA, Corazza PH, Cesar PF, Bottino MA, Valandro LF. Pressable feldspathic inlays in premolars: effect of cementation strategy and mechanical cycling on the adhesive bond between dentin and restoration. J Adhes Dent. 2014;16:147–154. doi: 10.3290/j.jad.a30555. [DOI] [PubMed] [Google Scholar]
- 40.Kious AR, Roberts HW, Brackett WW. Film thicknesses of recently introduced luting cements. J Prosthet Dent. 2009;101:189–192. doi: 10.1016/S0022-3913(09)60026-3. [DOI] [PubMed] [Google Scholar]
- 41.Amaral R, Ozcan M, Valandro LF, Balducci I, Bottino MA. Effect of conditioning methods on the microtensile bond strength of phosphate monomer-based cement on zirconia ceramic in dry and aged conditions. J Biomed Mater Res B Appl Biomater. 2008;85:1–9. doi: 10.1002/jbm.b.30908. [DOI] [PubMed] [Google Scholar]
- 42.Wegner SM, Gerdes W, Kern M. Effect of different artificial aging conditions on ceramic-composite bond strength. Int J Prosthodont. 2002;15:267–272. [PubMed] [Google Scholar]
- 43.Vanderlei A, Passos SP, Özcan M, Bottino MA, Valandro LF. Durability of adhesion between feldspathic ceramic and resin cements: effect of adhesive resin, polymerization mode of resin cement, and aging. J Prosthodont. 2013;22:196–202. doi: 10.1111/j.1532-849X.2012.00934.x. [DOI] [PubMed] [Google Scholar]
- 44.Osorio R, Castillo-de Oyagüe R, Monticelli F, Osorio E, Toledano M. Resistance to bond degradation between dualcure resin cements and pre-treated sintered CAD-CAM dental ceramics. Med Oral Patol Oral Cir Bucal. 2012;17:e669–e677. doi: 10.4317/medoral.17828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kumbuloglu O, Lassila LV, User A, Vallittu PK. Bonding of resin composite luting cements to zirconium oxide by two air-particle abrasion methods. Oper Dent. 2006;31:248–255. doi: 10.2341/05-22. [DOI] [PubMed] [Google Scholar]
- 46.Tanaka R, Fujishima A, Shibata Y, Manabe A, Miyazaki T. Cooperation of phosphate monomer and silica modification on zirconia. J Dent Res. 2008;87:666–670. doi: 10.1177/154405910808700705. [DOI] [PubMed] [Google Scholar]
- 47.Gomes AL, Ramos JC, Santos-del Riego S, Montero J, Albaladejo A. Thermocycling effect on microshear bond strength to zirconia ceramic using Er:YAG and tribochemical silica coating as surface conditioning. Lasers Med Sci. 2015;30:787–795. doi: 10.1007/s10103-013-1433-z. [DOI] [PubMed] [Google Scholar]
- 48.Flury S, Lussi A, Peutzfeldt A, Zimmerli B. Push-out bond strength of CAD/CAM-ceramic luted to dentin with self-adhesive resin cements. Dent Mater. 2010;26:855–863. doi: 10.1016/j.dental.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 49.Aleisa KI, Almufleh BS, Morgano SM, Lynch CD. Effect of types of luting agent on push-out bond strength of zirconium oxide posts. J Dent. 2013;41:377–383. doi: 10.1016/j.jdent.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 50.Saavedra G, Ariki EK, Federico CD, Galhano G, Zamboni S, Baldissara P, Valandro LF. Effect of acid neutralization and mechanical cycling on the microtensile bond strength of glass-ceramic inlays. Oper Dent. 2009;34:211–216. doi: 10.2341/08-68. [DOI] [PubMed] [Google Scholar]