Abstract
PURPOSE
The objective of this study was to evaluate the influence of various cement types on the stress distribution in monolithic zirconia crowns under maximum bite force using the finite element analysis.
MATERIALS AND METHODS
The models of the prepared #46 crown (deep chamfer margin) were scanned and solid models composed of the monolithic zirconia crown, cement layer, and prepared tooth were produced using the computer-aided design technology and were subsequently translated into 3-dimensional finite element models. Four models were prepared according to different cement types (zinc phosphate, polycarboxylate, glass ionomer, and resin). A load of 700 N was applied vertically on the crowns (8 loading points). Maximum principal stress was determined.
RESULTS
Zinc phosphate cement had a greater stress concentration in the cement layer, while polycarboxylate cement had a greater stress concentration on the distal surface of the monolithic zirconia crown and abutment tooth. Resin cement and glass ionomer cement showed similar patterns, but resin cement showed a lower stress distribution on the lingual and mesial surface of the cement layer.
CONCLUSION
The test results indicate that the use of different luting agents that have various elastic moduli has an impact on the stress distribution of the monolithic zirconia crowns, cement layers, and abutment tooth. Resin cement is recommended for the luting agent of the monolithic zirconia crowns.
Keywords: Crowns, Dental cement, Dental stress analysis, Finite element analysis, Zirconium
INTRODUCTION
The strength aspect of the posterior restoration material is more important than the esthetic aspect because posterior restorations are subject to higher stresses during mastication than anterior restorations. To overcome fracture of all ceramic restorations, many core materials have been developed to support the weaker-veneering porcelains. These include lithium disilicate, glass-infiltrated alumina, high-purity alumina, and zirconia.1 Among many dental ceramics, yttria-stabilized tetragonal zirconia polycrystal (Y-TZP) was proven to be satisfactory and was widely used for its remarkable fracture resistance and flexural strength compared to other dental ceramic materials.2
Zirconia exists in three different crystal phases at three different temperatures; monoclinic, tetragonal, and cubic. Zirconia is in the monoclinic phase at room temperature. The monoclinic phase changes into the tetragonal phase at temperatures from above 1,070℃. Then zirconia becomes stable in the tetragonal phase at temperatures between 1,170℃ and 2,370℃. At temperatures above 2,370℃, zirconia exists in the cubic phase. Zirconia can maintain the tetragonal phase at room temperature when stabilizers such as ceria, magnesia, or yttria are added. The transformation of martensitic tetragonal to monoclinic phase may be initiated by stress, such as machining, wear, or water. The transformation from the tetragonal to monoclinic phase causes a volume expansion by 3-4%. Crack propagation is blocked by the volume expansion at the crack tip. This transformation-toughening phenomenon results in the fracture resistibility and higher strength of zirconia. Zirconia has flexural strength ranging between 800-1200 MPa and a fracture toughness ranging between 6-8 MPa, and it meets the mechanical requirements for high stress-bearing posterior restorations.3,4,5
Guess et al.6 reported that monolithic lithium disilicate ceramic which were fabricated by the application of computer-aided design/computer-aided manufacturing (CAD/CAM) resulted in fatigue-resistant crowns, whereas veneered zirconia crowns showed a higher susceptibility to cyclic loading with early veneer failures based on fatigue findings. Advances in dental ceramic materials and the development of CAD/CAM along with milling technologies have improved the materials and made them easier to use which was impossible with conventional dental processing techniques.7,8,9 The monolithic zirconia crowns have been used more widely because of the recent developments in zirconia stain and glaze techniques. Moreover, they have been used more to avoid chipping of veneering porcelain. Even with their rapid development and increased uses, distinct criteria have not been established for the application of monolithic zirconia crowns. Little information is currently available on the cementation of the monolithic zirconia crowns. Finite element analysis (FEA) is an appropriate method for stress analysis. Since FEA was developed in the engineering field, it has been a popular option to analyze stress. In dentistry, FEA has been used to study stress distributions in the teeth and restorative materials.10,11 The purpose of this study was to evaluate the influence of different cement materials on the stress distribution in monolithic zirconia crowns by three dimensional FEA.
MATERIALS AND METHODS
FEA has been used as a method to analyze the magnitude and distribution of stresses in complex geometries. The geometric solid model was divided into elements, which were used as mathematical functions.12,13
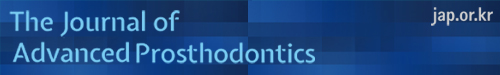
A standard crown preparation with a 8° convergence angle between tooth axis and axial wall, the chamfer depth of 1.2 mm, was prepared on a mandibular first molar of the Nissin study model (D85DP-500B.1, Nissin Dental, Kyoto, Japan) by using a surveyor (F1, Degu Dent GmbH, Kanau, Germany). The prepared model and unprepared mandibular right first molar resin model were scanned using an optical scanner (Optical 3D Scanner Activity 101, Smart Optics Sensor technik GmbH, Bochum, Germany). They were imported into the CAD software for modeling (Free Form modeling systems, Sensable-Geomagic, Woburn, MA, USA). Subsequently, a monolithic zirconia crown was designed based on an unprepared tooth resin model by using CAD. The solid models of a monolithic zirconia crown (1.5-mm thickness), a cement layer, and a prepared tooth were generated by using the scanned images with CAD software (Hyper Works 10.0, Altair Engineering, Ontario, Canada). Even though the recommended cement thickness is 50 µm, the cement thickness in this study was defined to be 200 µm to approximate the reported mean occlusal gap values of 219-369 µm.14 Moreover, Reich et al. studied the cement thickness of crown fabricated by 3 commercially available CAD/CAM systems and reported the mean occlusal gaps were 215 µm, 371 µm and 383 µm.15 In this process, 4 different models were fabricated for the different cement types (zinc phosphate cement (ZPC), polycarboxylate cement (PC), glass ionomer cement (GIC), and resin cement). The monolithic zirconia crown layer, the cement layer, and the prepared tooth were assembled in the final model (Fig. 1. A-C).
Fig. 1. Three components of the finite element analysis model. (A) Monolithic zirconia crown, (B) cement layer, (C) prepared tooth. Eight loading points and directions of load applying. (D), (E) three points on the outer inclines of each buccal cusp, three points on the inner inclines of each buccal cusp, and two points on the inner inclines of each lingual cusp.
Model I: vertical load 700 N, zinc phosphate cement
Model II: vertical load 700 N, polycarboxylate cement
Model III: vertical load 700 N, glass ionomer cement
Model IV: vertical load 700 N, resin cement
The finite element model was developed by using ABAQUS/CAE 6.9 software (Dassault Systèmes, Vèlizy-Villacoublay, France). The solid model was then meshed with parabolic tetrahedron solid elements. The material properties used in this study are listed in Table 1.16
Table 1. Material properties used in finite element analysis16.
| Component | Material | Elastic modulus (GPa) | Poisson's ratio | Density (g/cm3) |
|---|---|---|---|---|
| Crown | Zirconia | 205 | 0.19 | 2.40 |
| Cement layer | Zinc Phosphate Cement | 13.7 | 0.33 | 3.25 |
| Polycarboxylate Cement | 5.11 | 0.35 | 2.57 | |
| Glass Ionomer Cement | 7.56 | 0.35 | 1.88 | |
| Resin Cement | 8 | 0.33 | 2.19 | |
| Tooth | Dentin | 16 | 0.31 | 2.14 |
The following assumptions were included in the finite element models: (1) all components (monolithic zirconia crown, cement layer, and prepared tooth) were assumed to be homogeneous, linearly elastic, and isotropic in properties; (2) no slip happened between components (perfect bonding); (3) the cement layer had a 200-µm uniform thickness except at the margins; (4) the monolithic zirconia crown had a 1.5-mm uniform thickness except at the margins; (5) no components were flawed; and (6) all degrees of freedom were constrained at the root component surface.
Occlusal loads must be resisted by the prostheses as well as the cement. In the majority of previous research, maximum bite force has been reported as 700 N.17,18 Therefore, the magnitude of the values of load used in the present study was 700 N to simulate maximum bite force depending on the published data.10,17,18 The load of 700 N was distributed uniformly on the following 8 points of the crown in a vertical direction: 3 points on the outer inclines of each buccal cusp, 3 points on the inner inclines of each buccal cusp, and 2 points on the inner inclines of each lingual cusp (Fig. 1. D-E).10 The maximum principal stresses were recorded for the monolithic zirconia crown, each cement layer, and prepared tooth.
RESULTS
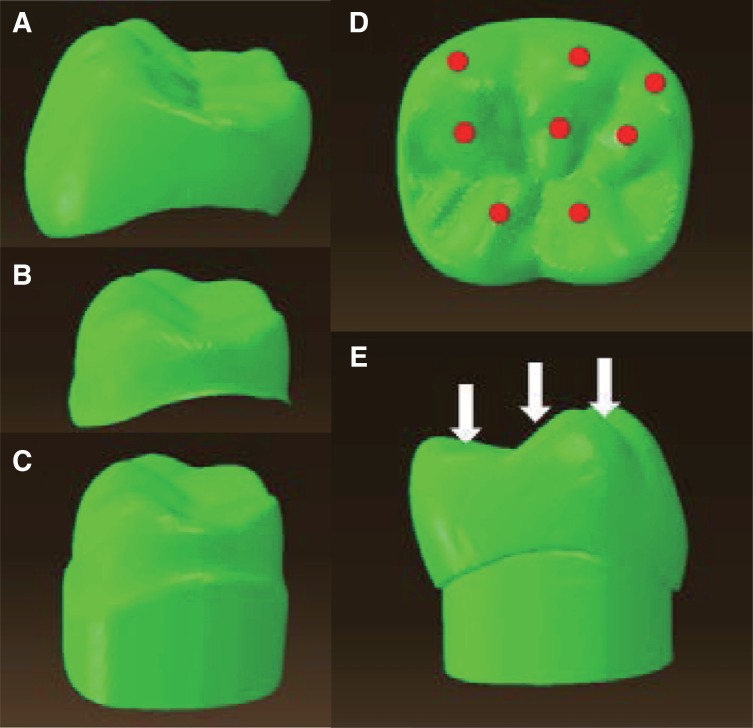
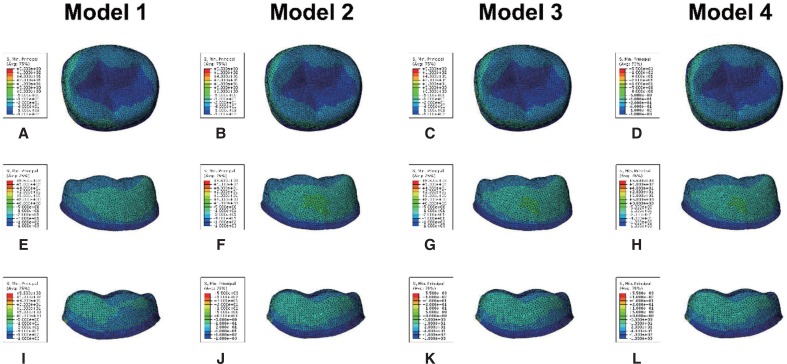
The stress patterns of each model are presented in Fig. 2, Fig. 3, Fig. 4, and Fig. 5. The same color indicates a similar range of the distributed stress level. The maximum principal stress distributions of the monolithic zirconia crown are shown in Fig. 2. The stress distributions changed with the different cement types. Concentrations of maximum principal stress were observed on 8 loading points on the occlusal surface, the buccal cusp on the buccal surface, the lingual pit on the lingual surface, and the cervical area on the mesial and distal surfaces. Difference in the stress distribution of the monolithic zirconia crown was observed in each model for the mesial, distal, and intaglio surfaces. Model I showed the highest maximum principal stress on the occlusal, cervical areas of the mesial, and intaglio surfaces, while Model II showed the highest maximum principal stress on the cervical areas of the distal surface. Model III and Model IV showed similar stress distribution pattern each other.
Fig. 2. Maximum principal stress distribution of the monolithic zirconia crown. (A) - (D) Buccal, (E) - (H) lingual, (I) - (L) mesial, (M) - (P) distal view.
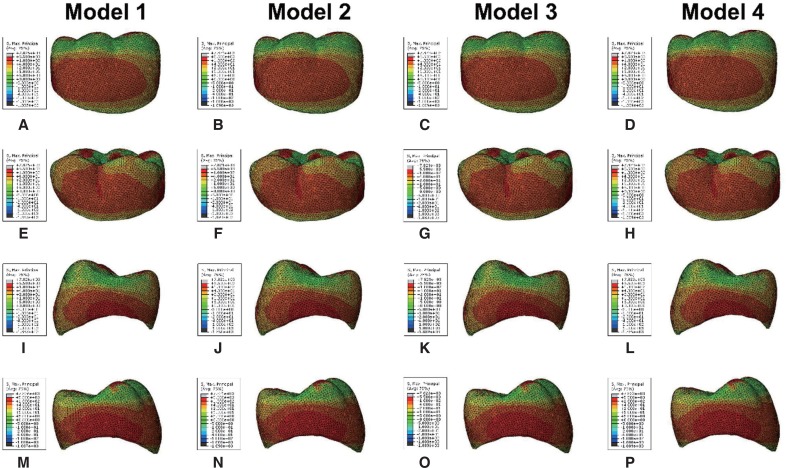
Fig. 3. Maximum principal stress distribution of the cement layer. (A) - (D) Occlusal, (E) - (H) buccal, (I) - (L) lingual view.
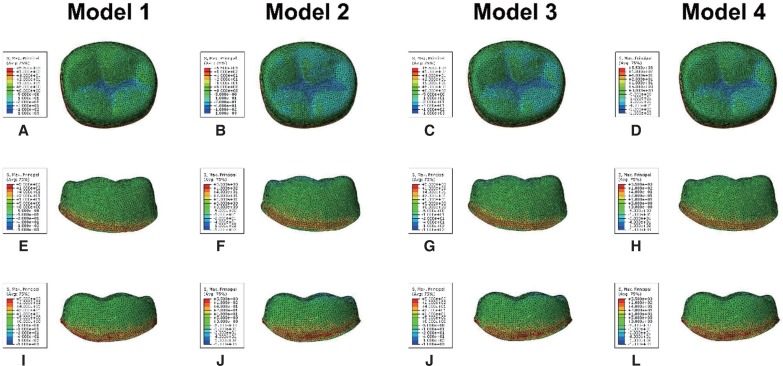
Fig. 4. Minimum principal stress distribution of the cement layer. (A) - (D) Occlusal, (E) - (H) buccal, (I) - (L) lingual view.
Fig. 5. von Mises stress distribution of the cement layer. (A) - (D) Occlusal, (E) - (H) buccal, (I) - (L) lingual view.
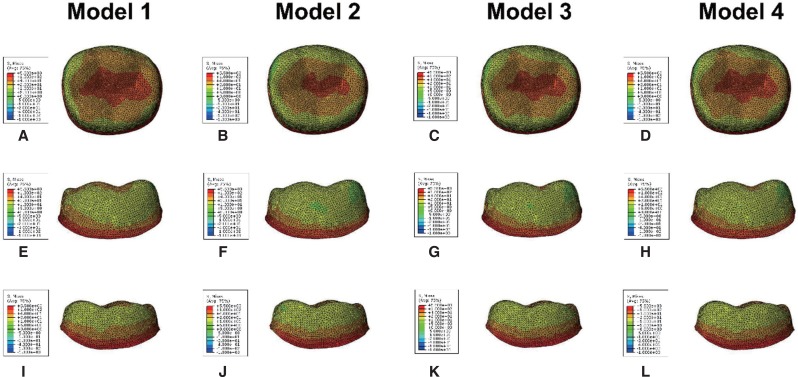
The maximum principal stress distributions of the cement layers are shown in Fig. 3; concentrations of maximum principal stress were observed on the occlusal surface, intaglio surface, and cervical area of the cement layers. The stress distribution changed with the different cement types. Model I showed the highest maximum principal stress on the mesial and distal surfaces, while Model II showed the lowest maximum principal stress on the mesial and distal surfaces of the cement layer. Model III and Model IV showed similar stress distribution pattern each other except for the lingual surface. Model IV showed the lowest maximum principal stress concentration on the lingual surface of the cement layer.
The minimum principal stress distributions of the cement layer are shown in Fig. 4; concentrations of minimum principal stress were observed on the occlusal surface, intaglio surface, and cervical areas of the cement layer. The stress distributions changed with the different cement types. Model I showed the highest stress concentrations on the buccal, mesial, and distal surfaces, whereas Model II showed the lowest stress concentrations on the buccal, mesial, and distal surfaces. However, Model II showed the highest minimum principal stress on the lingual surface. Model III and Model IV showed similar stress distribution pattern each other.
The von Mises stress distributions of the cement layer are shown in Fig. 5; concentrations of von Mises stresses were observed on the occlusal surface and cervical areas of the cement layer. The stress distributions changed with the different cement types. Model I showed the highest stress concentrations on the occlusal, buccal, lingual, cervical areas of the mesial, and intaglio surfaces, while Model II showed a lower stress concentrations on the lingual and mesial surfaces than the other models. Model III showed the lowest stress concentration on the buccal surface, while Model IV showed a lower stress concentration on the distal surface than the other models.
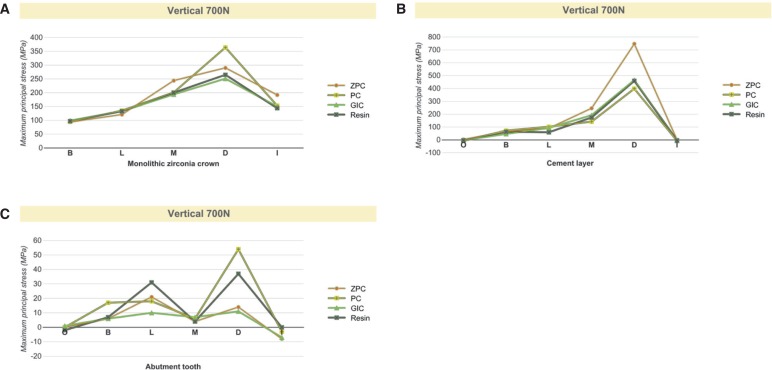
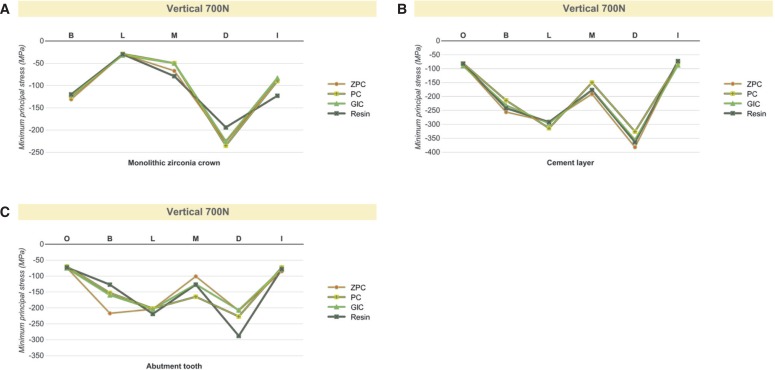
The highest levels of the maximum principal stress, minimum principal stress, and von Mises stress in each component are shown in Fig. 6, Fig. 7, and Fig. 8.
Fig. 6. The peak maximum principal stress value in each model. (A) Monolithic zirconia crown, (B) cement layer, (C) abutment tooth.
Fig. 7. The peak minimum principal stress value in each model. (A) Monolithic zirconia crown, (B) cement layer, (C) abutment tooth.
Fig. 8. The peak von Mises stress value in each model. (A) Monolithic zirconia crown, (B) cement layer, (C) abutment tooth.
DISCUSSION
The use of the monolithic zirconia crowns has become popular in the restorative dentistry. While there are a vast variety of dental cements presently available in the market including ZPC, PC, GIC, and resin cements, there are no well-established guidelines for the selection of dental cements for the monolithic zirconia restorations.
Dental cements are designed to provide stability and retention to the restorations in the harsh oral environment. Retention mechanisms are divided as chemical, mechanical, and micromechanical elements. Usually, 2 or 3 mechanisms work together in combination, depending on the nature of the cement and material.19 Dental cements are subdivided as resin-based and non-resin-based cements. They should have properties such as resistance to dissolution, a strong bond, high strength under tension, good manipulation properties, and biocompatibility. ZPC has been traditionally regarded as the most popular material, despite its lack of adhesion, solubility, and low hardness properties. Although the final marginal accuracy of all-ceramic systems produced from CAD/CAM has significantly improved, these products still result in larger internal gaps than those of cast crowns, possibly resulting in thicker cement layers and less frictional retention to the abutments.14,15 These would be drawbacks for ZPC because of its solubility and lack of adhesiveness. ZPC has been used in some all-ceramic systems, but long-term clinical data have not yet been published. PC was the first cement exhibiting adhesive properties to the tooth. However, PC exhibited low compressive strength, tensile strength, and it may undergo significant plastic deformation under functional force after set. GIC are also of great interest to clinicians. These cements exhibit several clinical advantages, including physicochemical bonding to tooth structures, low coefficients of thermal expansion, and long-term release of fluoride. However, low mechanical strength compromises the use of GIC in high-stress-bearing areas. Moreover, GIC would not be suitable for ceramics that require support from the cement. Therefore, resin-based cements are widely used as the choice of cements for ceramic restorations due to the disadvantages of other cements such as lack of solubility, support, and adhesion. Resin cements are based on bisphenol-A-glycidyl metharcrylate and other metharcrylates. It has the advantages such as high bonding strength, high compressive strength and low solubility.
Restorative dentistry constantly undergoes changes and no currently available cement is ideal for all situations. The advent of adhesive cements has considerably expanded the scope of fixed prosthodontics. Resin-based cements are used in all-ceramic systems because of the important role that those cements play in the final clinical success of this treatment modality.20,21,22,23,24
Several authors have studied the role of dental cement by using FEA. Proos et al.16 investigated the influence of adhesive resin and ZPC on In-Ceram coping and gold coping, and their results suggested that the type of dental cement has a minor effect on the resultant stress distribution. Kamposiora et al.,25 who studied the stress level and distribution of the cement layer with 4 types of cement under an all-ceramic crown and gold crown, found that ZPC shows a greater stress value than other cement materials. Shahrbaf et al.26 studied the influence of the tooth preparation design and the elastic moduli of cement which include 4 kinds of commercially available resin cements and extremely high value hypothetical cement. Their results suggested that both the preparation design and the elastic modulus of cement affect the stress distribution of the restored crown-root complex. Rekow et al.27 studied the influence of 7 variables, including crown material and thickness, cement material and thickness, position of load, cusp inclination, and the supporting core, on the maximum principal stress distribution. They found that the crown material and thickness are major contributive factors. In their study, all cements were assumed to be in the rigid bonding condition, which means that the interface of each component cannot slip. Additionally, these bonding conditions can create internal tensile stress on the bonded crown. May et al.,28 who studied the influence of the cement thickness and bonding condition on the feldspathic porcelain crown by means of 2-dimensional multiphysics FEA and a physical test, found that the well-fitted, bonded feldspathic crown can withstand a greater load than the non-bonded crown, but the bonding effect disappears under a large cement layer.
The present study used 4 types of dental cements and showed that these types of cements have similar stress distributions except for ZPC and PC, which had a wider distribution of a high stress level on the monolithic zirconia crown and cement layer. These findings suggest that low-elastic materials result in a lower stress distribution in the cement layer and transfer less stress to the prepared tooth. Resin cements have the advantage of high tensile strength, high compressive strength, high bonding strength, and low solubility. Resin cements are relatively insoluble compared to the other dental cements. Moreover, resin cements have shown better retention than ZPC or GI.29 However, conventional resin cements require multiple steps for bonding procedure.30 In addition, it is difficult to establish chemical bonding between resin cements and the zirconia inner surfaces without functional monomer or other surface treatments. Therefore, self-adhesive resin cement containing functional monomer is recommended for luting agent of the monolithic zirconia crowns.
The results of in vitro simulation testing cannot be postulated to the clinical situation, because this simulation study design did not contemplate typical factors of the oral cavity, such as dynamic forces of mastication or fatigue loading. Obviously, direction of occlusal loading is relevant to the teeth anatomy during mastication. This, however, was not taken into consideration in the current study. In the present study, the maximum bite force was simulated. Further studies are necessary on the effect of the cement type under conditions of dynamic occlusion, various cement thicknesses, and cement polymerization. In clinical practice, the restored crown-root complex is always located in conditions that are moist and prone to temperature changes. Therefore, further studies are necessary on the influence of the cement under conditions of bonding, water storage, cyclic loading, and thermo-cycling.
CONCLUSION
Within the limitations of this study, it can be concluded that the use of different dental cements that have different elastic moduli has an impact on the stress distribution of the monolithic zirconia crown, cement layer, and prepared tooth. Dental cement with higher elastic modulus creates a wider distribution of a higher stress concentration area within the cement layer. Resin cement is recommended for luting agent of the monolithic zirconia crown, because it showed low stress concentration in the cement layer and it has an advantage of low solubility.
ACKNOWLEDGEMENTS
The author would like to express gratitude to Sky dental laboratory research institute for designing and digitizing the crowns. The author is grateful to prof. Seung-Hyun Yoo (Department of Mechanical Engineering, College of Engineering, Ajou University) for his assistance with FEA.
References
- 1.De Jager N, Pallav P, Feilzer AJ. The influence of design parameters on the FEA-determined stress distribution in CADCAM produced all-ceramic dental crowns. Dent Mater. 2005;21:242–251. doi: 10.1016/j.dental.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 2.Piconi C, Maccauro G. Zirconia as a ceramic biomaterial. Biomaterials. 1999;20:1–25. doi: 10.1016/s0142-9612(98)00010-6. [DOI] [PubMed] [Google Scholar]
- 3.Shimizu K, Oka M, Kumar P, Kotoura Y, Yamamuro T, Makinouchi K, Nakamura T. Time-dependent changes in the mechanical properties of zirconia ceramic. J Biomed Mater Res. 1993;27:729–734. doi: 10.1002/jbm.820270605. [DOI] [PubMed] [Google Scholar]
- 4.Luthardt RG, Holzhüter M, Sandkuhl O, Herold V, Schnapp JD, Kuhlisch E, Walter M. Reliability and properties of ground Y-TZP-zirconia ceramics. J Dent Res. 2002;81:487–491. doi: 10.1177/154405910208100711. [DOI] [PubMed] [Google Scholar]
- 5.Blatz MB, Sadan A, Martin J, Lang B. In vitro evaluation of shear bond strengths of resin to densely-sintered high-purity zirconium-oxide ceramic after long-term storage and thermal cycling. J Prosthet Dent. 2004;91:356–362. doi: 10.1016/j.prosdent.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Guess PC, Zavanelli RA, Silva NR, Bonfante EA, Coelho PG, Thompson VP. Monolithic CAD/CAM lithium disilicate versus veneered Y-TZP crowns: comparison of failure modes and reliability after fatigue. Int J Prosthodont. 2010;23:434–442. [PubMed] [Google Scholar]
- 7.McLaren EA, Terry DA. CAD/CAM systems, materials, and clinical guidelines for all-ceramic crowns and fixed partial dentures. Compend Contin Educ Dent. 2002;23:637–641. 644, 646 passim. quiz 654. [PubMed] [Google Scholar]
- 8.Luthardt RG, Sandkuhl O, Herold V, Walter MH. Accuracy of mechanical digitizing with a CAD/CAM system for fixed restorations. Int J Prosthodont. 2001;14:146–151. [PubMed] [Google Scholar]
- 9.Preis V, Behr M, Hahnel S, Handel G, Rosentritt M. In vitro failure and fracture resistance of veneered and full-contour zirconia restorations. J Dent. 2012;40:921–928. doi: 10.1016/j.jdent.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 10.Ha SR, Kim SH, Han JS, Yoo SH, Jeong SC, Lee JB, Yeo IS. The influence of various core designs on stress distribution in the veneered zirconia crown: a finite element analysis study. J Adv Prosthodont. 2013;5:187–197. doi: 10.4047/jap.2013.5.2.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li X, Cao Z, Qiu X, Tang Z, Gong L, Wang D. Does matching relation exist between the length and the tilting angle of terminal implants in the all-on-four protocol? stress distributions by 3D finite element analysis. J Adv Prosthodont. 2015;7:240–248. doi: 10.4047/jap.2015.7.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spazzin AO, Galafassi D, de Meira-Júnior AD, Braz R, Garbin CA. Influence of post and resin cement on stress distribution of maxillary central incisors restored with direct resin composite. Oper Dent. 2009;34:223–229. doi: 10.2341/08-73. [DOI] [PubMed] [Google Scholar]
- 13.Soares CJ, Raposo LH, Soares PV, Santos-Filho PC, Menezes MS, Soares PB, Magalhães D. Effect of different cements onthe biomechanical behavior of teeth restored with cast dowel- and-cores-in vitro and FEA analysis. J Prosthodont. 2010;19:130–137. doi: 10.1111/j.1532-849X.2009.00527.x. [DOI] [PubMed] [Google Scholar]
- 14.Pilo R, Cardash HS. In vivo retrospective study of cement thickness under crowns. J Prosthet Dent. 1998;79:621–625. doi: 10.1016/s0022-3913(98)70067-8. [DOI] [PubMed] [Google Scholar]
- 15.Reich S, Wichmann M, Nkenke E, Proeschel P. Clinical fit of all-ceramic three-unit fixed partial dentures, generated with three different CAD/CAM systems. Eur J Oral Sci. 2005;113:174–179. doi: 10.1111/j.1600-0722.2004.00197.x. [DOI] [PubMed] [Google Scholar]
- 16.Proos KA, Swain MV, Ironside J, Steven GP. Influence of cement on a restored crown of a first premolar using finite element analysis. Int J Prosthodont. 2003;16:82–90. [PubMed] [Google Scholar]
- 17.Ferrario VF, Sforza C, Zanotti G, Tartaglia GM. Maximal bite forces in healthy young adults as predicted by surface electromyography. J Dent. 2004;32:451–457. doi: 10.1016/j.jdent.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 18.Nishigawa K, Bando E, Nakano M. Quantitative study of bite force during sleep associated bruxism. J Oral Rehabil. 2001;28:485–491. doi: 10.1046/j.1365-2842.2001.00692.x. [DOI] [PubMed] [Google Scholar]
- 19.Manso AP, Silva NR, Bonfante EA, Pegoraro TA, Dias RA, Carvalho RM. Cements and adhesives for all-ceramic restorations. Dent Clin North Am. 2011;55:311–332, ix. doi: 10.1016/j.cden.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 20.Palacios RP, Johnson GH, Phillips KM, Raigrodski AJ. Retention of zirconium oxide ceramic crowns with three types of cement. J Prosthet Dent. 2006;96:104–114. doi: 10.1016/j.prosdent.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 21.Blatz MB, Sadan A, Kern M. Resin-ceramic bonding: a review of the literature. J Prosthet Dent. 2003;89:268–274. doi: 10.1067/mpr.2003.50. [DOI] [PubMed] [Google Scholar]
- 22.Ernst CP, Cohnen U, Stender E, Willershausen B. In vitro retentive strength of zirconium oxide ceramic crowns using different luting agents. J Prosthet Dent. 2005;93:551–558. doi: 10.1016/j.prosdent.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 23.Pospiech P. All-ceramic crowns: bonding or cementing? Clin Oral Investig. 2002;6:189–197. doi: 10.1007/s00784-002-0183-2. [DOI] [PubMed] [Google Scholar]
- 24.Thompson JY, Stoner BR, Piascik JR, Smith R. Adhesion/cementation to zirconia and other non-silicate ceramics: where are we now? Dent Mater. 2011;27:71–82. doi: 10.1016/j.dental.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kamposiora P, Papavasilious G, Bayne SC, Felton DA. Finite element analysis estimates of cement microfracture under complete veneer crowns. J Prosthet Dent. 1994;71:435–441. doi: 10.1016/0022-3913(94)90179-1. [DOI] [PubMed] [Google Scholar]
- 26.Shahrbaf S, vanNoort R, Mirzakouchaki B, Ghassemieh E, Martin N. Effect of the crown design and interface lute parameters on the stress-state of a machined crown-tooth system: a finite element analysis. Dent Mater. 2013;29:e123–e131. doi: 10.1016/j.dental.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 27.Rekow ED, Harsono M, Janal M, Thompson VP, Zhang G. Factorial analysis of variables influencing stress in all-ceramic crowns. Dent Mater. 2006;22:125–132. doi: 10.1016/j.dental.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 28.May LG, Kelly JR, Bottino MA, Hill T. Effects of cement thickness and bonding on the failure loads of CAD/CAM ceramic crowns: multi-physics FEA modeling and monotonic testing. Dent Mater. 2012;28:e99–109. doi: 10.1016/j.dental.2012.04.033. [DOI] [PubMed] [Google Scholar]
- 29.Ayad MF, Rosenstiel SF, Salama M. Influence of tooth surface roughness and type of cement on retention of complete cast crowns. J Prosthet Dent. 1997;77:116–121. doi: 10.1016/s0022-3913(97)70223-3. [DOI] [PubMed] [Google Scholar]
- 30.Pameijer CH. A review of luting agents. Int J Dent. 2012;2012:752861. doi: 10.1155/2012/752861. [DOI] [PMC free article] [PubMed] [Google Scholar]