Abstract
Objective
To identify the barriers and facilitators for sustainability of tele‐homecare programs implemented by home health nursing agencies for chronic disease management.
Data Sources
English‐language articles on home telehealth in the CINAHL, PubMed/MEDLINE, PsychInfo, Web of Science, and Cochrane Reviews databases published from January 1996 to December 2013.
Study Design
We performed a systematic literature review. Data extraction using PRISMA guidelines and quality appraisal using the Mixed Methods Appraisal Tool (MMAT) were conducted on relevant empirical studies. Thematic analysis across the studies and narrative summaries were used to synthesize the findings from the included studies.
Principal Findings
Of the initial 3,920 citations, we identified 16 articles of moderate quality meeting our inclusion criteria. Perceptions on effectiveness of tele‐homecare programs for achieving intended outcomes; tailoring of tele‐homecare programs to patient characteristics and needs; relationship and communication between patient, nurse, and other health care professional users of tele‐homecare; home health organizational process and culture; and technology quality, capability, and usability impacted the sustainability of tele‐homecare programs.
Conclusions
The findings of this systematic review provide implications for sustained usage of tele‐homecare programs by home health nursing agencies and can help such programs realize their potential for chronic disease management.
Keywords: Telehealth, tele‐homecare, home health nursing, chronic disease management, sustainability
In the United States, chronic diseases account for 7 in 10 deaths each year and more than 75 percent of health care costs (Centers for Disease Control and Prevention 2013). In 2003–2004, for example, 67 percent of Medicare beneficiaries who were discharged from hospitals with a chronic disease were rehospitalized or died within the first year of discharge (Jencks, Williams, and Coleman 2009). To reduce preventable hospitalizations due to chronic diseases, home health has begun to play a valuable role (National Association for Home Care and Hospice 2010): Home health is one of the nation's fastest growing health care sectors (Henderson 2012), and home health agencies, defined as agencies or organizations primarily engaged in providing skilled nursing services and other therapeutic services to patients in their homes (Centers for Medicare & Medicaid Services [CMS] 2013b), are becoming instrumental in the attempt to reduce hospitalizations due to chronic diseases.
In 2010, the National Association for Home Care & Hospice reported that 12,000 home health agencies in the United States were admitting 12 million patients, and in 2012, the CMS reported that these agencies were serving approximately 4.5 million Medicare and Medicaid patients annually. However, home health agencies are facing challenges: With decreasing payments for home health services (Centers for Medicare & Medicaid Services [CMS] 2013a) and increases in home health accountability for patient outcomes, there is an urgent need for innovations to assist home health nurses in providing effective and efficient care to home health patients with chronic diseases. Remote monitoring technologies such as telehealth have therefore emerged as a potential solution to help home health agencies increase accountability in managing chronic diseases of patients in their homes (Bowles and Baugh 2007).
Tele‐homecare, a form of home telehealth, is defined as a communication and clinical information system that enables the interaction of voice, video, and health‐related data using ordinary telephone lines from the patients' homes to their home health agencies in conjunction with skilled nurses' home visits (Dansky, Bowles, and Palmer 2003). Daily monitoring of patients via tele‐homecare can enable home health care nurses to detect early warning signs, prevent expensive emergency department visits, and reduce the frequency of hospitalizations, allowing patients to feel secure at home and improving their quality of life.
Tele‐homecare information can also empower homebound patients with chronic diseases to make informed decisions about their disease management. Such empowerment can remove or at least delay their transition to high‐cost care settings, as well as reduce the burden currently experienced by their formal and informal caregivers. This is especially important within the context of today's home health care provider shortage. To date, however, the evidence on the cost and clinical effectiveness of home telehealth has been mixed and difficult to interpret (Clark et al. 2007; Polisena et al. 2009; Paré et al. 2010; Klersy et al. 2011; Pandor et al. 2013; Udsen, Hejlesen, and Ehlers 2014). Moreover, despite a modest 11 percent increase in tele‐homecare adoption by home health agencies from 2007 to 2013 (Fazzi, Ashe, and Doak 2008; Fazzi Associates 2014), the utilization of tele‐homecare devices by home health agencies remains low, with at least 27 percent of home health agencies reporting that they used less than 25 percent of their tele‐homecare devices on a given day (Fazzi Associates 2014). In addition, researchers are also reporting poor utilization and discontinued use of tele‐homecare adopted by home health agencies for chronic disease‐related care delivery (May et al. 2011; Juretic et al. 2012; Sanders et al. 2012). The sustainability of tele‐homecare programs intended as an innovation to home health care delivery thus remains a major challenge, and our understanding of the factors contributing to both discontinued and sustained tele‐homecare use is unclear.
Earlier systematic reviews have focused on the effectiveness of home telehealth programs for health care utilization, physiological, or behavioral outcomes (Klersy et al. 2009; Paré et al. 2010; Radhakrishnan and Jacelon 2012; Udsen, Hejlesen, and Ehlers 2014), but they have not addressed these programs' sustainability. This study is significant as we address the knowledge gap regarding the sustainability of tele‐homecare programs and related implications for chronic disease management by home health agencies. We present a systematic review of articles published from 1996 to 2013 in which we identify barriers to and facilitators for sustained tele‐homecare use by home health agencies for chronic disease management. For this review, we have adapted Cradduck's (2002) definition of sustainability for telehealth services which defined sustainability as the use of tele‐homecare services that hold the promise of being absorbed into routine health care delivery. Indicators of tele‐homecare's sustainability include continued use of tele‐homecare systems with an increasing demand for those services, and acceptance of such services among home health care providers with a commitment to invest in them.
Methods
For this study, we reviewed articles indexed in databases of peer‐reviewed literature, following best practice guidelines developed by the Cochrane Collaboration to search, retrieve, and synthesize the findings of studies on health services research (Higgins and Green 2011).
Search Strategy
We performed a systematic search of the CINAHL, PubMed/MEDLINE, PsychInfo, Web of Science, and Cochrane Reviews databases for English‐language articles on tele‐homecare. The keywords telehealth, telemonitoring, telecare, telemedicine, and telehomecare were used to retrieve articles published from January 1996 to December 2013, because pilot projects and literature on tele‐homecare began to expand during that period. From the retrieved articles, we then identified studies conducted in home health agencies. All studies that matched the key words were included in the review. We chose to examine articles that addressed the management of the chronic diseases of heart failure (HF), hypertension (HTN), diabetes, and chronic obstructive pulmonary disease (COPD) in older adults age 65 years or above, because those diagnoses and that population are common for tele‐homecare services (Polisena et al. 2009). Studies that were not based in home health agencies or that did not explore tele‐homecare usage were excluded. Table 1 provides the inclusion and exclusion criteria for the studies in this review.
Table 1.
Inclusion and Exclusion Criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Types of studies | |
|
|
| Types of participants | |
|
|
| Types of interventions | |
|
|
| Types of outcome measures | |
|
|
To examine the sustainability of tele‐homecare, which involves both contextual and organizational factors, clinical trials may not adequately capture the complexity of implementing a tele‐homecare program and sustaining its implementation, or replicate the conditions on the ground. We therefore included other studies as well, such as longitudinal observational or qualitative studies.
Data Abstraction
PRISMA guidelines were followed up for data abstraction and assessment (Moher et al. 2009). After consensus was obtained among the three reviewers regarding the abstraction tool, one reviewer (A. B.) extracted data from all the studies included for data abstraction. Data were also extracted from a random sample (10 percent) by a second reviewer (K. R.) to assess reliability. One reviewer (K. R.), who has extensive research experience and clinical expertise in home tele‐homecare, independently reviewed the tele‐homecare studies. Then a second reviewer (A. B.) and a third (B. X.) joined the first to test reviewer agreement (kappa = 1) on a small sample of randomly selected studies (20 and 4 articles, respectively). For each article, eligibility was first identified according to the following criteria: (1) Was the study based in a home health agency? (2) Did the study employ an empirical methodology? (3) Did the study explore determinants of sustainability or long‐term usage of tele‐homecare programs? These criteria led to the inclusion of the final articles for further extraction. For example, a study on sustainability of telehealth services in Australia by Wade and Eliott (2012) was excluded, because it was unclear whether home health agencies were included as study sites. Similarly, a study by Shea and Chamoff (2012) that examined the communication and integration of telehealth information by patients was excluded, because the study did not explore the determinants of tele‐homecare usage (see Appendix SA3). From the final included articles, the following data were extracted: (1) study design; (2) study quality; (3) characteristics of the participants, including demographics, diagnoses, and role in the tele‐homecare program; (4) data collection methods; (5) description of the tele‐homecare program; and (6) determinants of the sustainability of tele‐homecare programs. These data were entered into Microsoft Excel tables to facilitate analyses of the included studies.
Data Analysis
Thematic analysis was used to identify themes representing the determinants of sustained tele‐homecare usage in home health agencies. This involved systematic identification of recurring themes in the key findings of the included studies. The studies were too heterogeneous to perform a meta‐analysis, but aggregate frequencies, means, and proportions of data from the included studies were identified whenever appropriate. Narrative summaries were then used for synthesis of findings from the included studies.
Quality Appraisal
To evaluate the studies, we used the Mixed Methods Appraisal Tool (MMAT) developed by Pace et al. (2012) for the critical appraisal of the quality of qualitative, quantitative, and mixed methods research studies. This tool has been used in previous systematic reviews (Humphries et al. 2014) to judge the trustworthiness, value, and relevance of the methodological quality of studies with varied designs. With the MMAT, we examined the data sources, data analysis, research contexts, and researchers' influences in the qualitative studies; the study design, sampling strategies, selection biases, comparisons of groups, measurements, and response rates in the quantitative studies; and the relevance of mixed‐method design, integration of methods, and limitations in mixed‐method studies. Quality assessment was conducted by author K. R., who scored the quality of studies as “Yes” if they clearly met the criteria, “No” if they clearly did not meet the criteria, “Unclear” if it could not be determined from the reporting whether they met the criteria or not, or “Not Applicable” if the specific quality question did not apply to the study design. Based on their quality scores, the studies were ranked as having low, moderate, or high quality, but they were not excluded on the basis of low quality.
Results
Search Outcome
Our initial search of the databases identified 3,920 abstracts, which we reduced to 943 after applying initial search criteria to include articles in the English language focusing on the chronic diseases of HF, HTN, diabetes, and COPD and to exclude duplicates. After title and abstract search, we eliminated articles on studies that investigated effectiveness of tele‐homecare for reducing health care utilization, or improving physiological or behavioral outcomes, as well as studies that were not based in home health agencies, and systematic reviews. This left 142 articles for data abstraction. The final number of original empirical studies based in home health agencies that investigated usage of tele‐homecare programs as an outcome was 16, after in‐depth analysis of the articles according to the inclusion criteria. The contents regarding barriers to and facilitators for sustained usage of tele‐homecare were obtained from the findings and discussion sections of the studies. Figure 1 provides a PRISMA diagram illustrating details of the search strategy.
Figure 1.
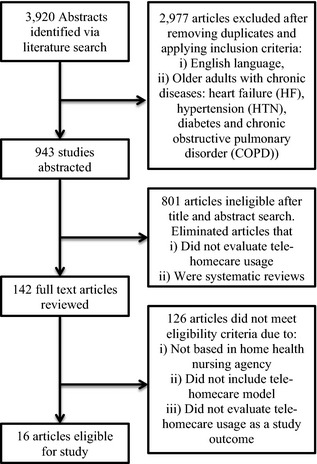
Literature Search Flow Diagram
Quality Appraisal
Table 2 summarizes the quality assessment of the included studies. The studies are organized by design (qualitative, quantitative, mixed methods), and the relevant quality questions are reported for each study. Based on responses to questions reflecting the critical appraisal criteria for mixed methods study designs (Pace et al. 2012), the overall quality of the one included study was moderate. Ten of the 16 studies had qualitative designs; these included case study, phenomenological, and ethnographic approaches, as well as two process evaluations of randomized controlled trials. As summarized in Table 2, the quality of analysis was moderate among the qualitative studies: almost all of the 10 qualitative studies (9 of 10) reported triangulation of findings through the use of multiple methods for addressing the same question; only three of the 10 qualitative studies mentioned sampling until saturation was reached or assessed the credibility of study findings through member checks or independent analysis by researchers. The majority of the qualitative studies provided background contextual information either through description within the articles (5 of 10) or through description in other articles on the same study (3 of 10) to enable potential transferability of findings to other settings. However, only two of the 10 qualitative studies reported on the researchers' influence on the findings—for example, on use of reflexivity, use of audit trails, or background information about the researchers' preparation for performing the research.
Table 2.
Quality Assessment of Included Studies
| Type of Study | Study | Screening Questions | Methodological Quality Criteria | ||||
|---|---|---|---|---|---|---|---|
| 1. Qualitative | Are there clear qualitative and quantitative research questions (or objectives*), or a clear mixed methods question (or objective*)? | Do the collected data allow the research question (objective) to be appropriately addressed? | 1.1. Are the sources of qualitative data (archives, documents, informants, observations) relevant to address the research question (objective)? | 1.2. Is the process for analyzing qualitative data relevant to address the research question (objective)? | 1.3. Is appropriate consideration given to how findings relate to the context, e.g., the setting, in which the data were collected? | 1.4. Is appropriate consideration given to how findings relate to researchers' influence, e.g., through their interactions with participants? | |
| Hardisty et al. (2011) | Yes | Yes | Yes | Yes | Unclear | No | |
| Fairbrother et al. (2012) | Yes | Yes | Yes | Yes | Yes | Yes | |
| Fairbrother et al. (2013) | Yes | Yes | Yes | Yes | Yes | Yes | |
| Gale and Sultan (2013) | Yes | Yes | Yes | Unclear | Unclear | No | |
| Hibbert et al. (2004) | Yes | Yes | Yes | Unclear | Unclear (described elsewhere) | No | |
| Lamothe et al. (2006) | Yes | Yes | Yes | Unclear | Yes | Yes | |
| Mair, Hiscock, and Beaton (2008) | Yes | Yes | Yes | Unclear | Unclear (described elsewhere) | No | |
| Rogers et al. (2011) | Yes | Yes | Yes | Unclear | Yes | No | |
| Sanders et al. (2012) | Yes | Yes | Yes | Yes | Unclear (described elsewhere) | No | |
| West and Milio (2004) | Yes | Yes | Yes | Unclear | Yes | No | |
| 5. Mixed methods | Radhakrishnan, Jacelon, and Roche (2012) | Yes | Yes | Yes | Yes | Yes | No |
| 4. Quantitative descriptive | Are there clear qualitative and quantitative research questions (or objectives*), or a clear mixed methods question (or objective*)? | Do the collected data allow the research question (objective) to be appropriately addressed? | 4.1. Is the sampling strategy relevant to address the quantitative research question (quantitative aspect of the mixed methods question)? | 4.2. Is the sample representative of the population understudy? | 4.3. Are measurements appropriate (clear origin, or validity known, or standard instrument)? | 4.4. Is there an acceptable response rate (60% or above)? | |
| Guzman‐Clark et al. (2013) | Yes | Yes | Yes | Yes | Unclear (validity unknown) | Yes | |
| Juretic et al. (2012) | Yes | Yes | Yes | Yes | Yes | Yes | |
| Kaufman et al. (2006) | Yes | Yes | Yes | Yes | Yes | Not applicable | |
| Peeters et al. (2012) | Yes | Yes | Yes | Unclear | Yes | No | |
| Radhakrishnan, Bowles et al. (2013) | Yes | Yes | Yes | Yes | Yes | Yes | |
| 5. Mixed methods | Radhakrishnan, Jacelon, and Roche (2012) | Yes | Yes | Yes | Unclear | Yes | Yes |
| 5. Mixed methods | Are there clear qualitative and quantitative research questions (or objectives*), or a clear mixed methods question (or objective*)? | Do the collected data allow the research question (objective) to be appropriately addressed? | 5.1. Is the mixed methods research design relevant to address the qualitative and quantitative research questions (or objectives), or the qualitative and quantitative aspects of the mixed methods question (or objective)? | 5.2. Is the integration of qualitative and quantitative data (or results*) relevant to address the research question (objective)? | 5.3. Is appropriate consideration given to the limitations associated with this integration, e.g., the divergence of qualitative and quantitative data (or results*) in a triangulation design? | ||
| Radhakrishnan, Jacelon, and Roche (2012) | Yes | Yes | Yes | Yes | Yes | ||
The five quantitative studies included one descriptive usability study, one survey, and three secondary analyses of retrospective data. Among the five quantitative studies, response rates were acceptable in three studies, and the majority of the studies (four out of five) adequately addressed the validity of instruments and representativeness of the sample population.
Article Characteristics
Table 3 provides a descriptive summary of the studies included in this review. The majority of the studies were conducted in the United Kingdom (eight) and United States (six), with two conducted in Canada and the Netherlands. The articles are recent; 11 of the 16 studies were published after 2010. Sample sizes ranged from 12 to 82 for the qualitative studies and from 132 to 403 for the survey and secondary analysis studies. Participants included only patients (eight), only clinicians (two), or mixed samples of both patients and clinicians (six). Patient diagnoses targeted by the tele‐homecare programs included only HF (four), only COPD (four), only diabetes (one), or a combination of the four chronic diseases of HF, HTN, COPD, and diabetes (seven). The total duration of tele‐homecare use at the study setting before the study was conducted was unknown in most studies, so this could not be abstracted for the present review.
Table 3.
Description of Included Studies
| Study | Study Design/Study Location | Study Methods | Study Participants/Patient Diagnosis | Study Purpose/Objectives |
|---|---|---|---|---|
| Fairbrother et al. (2012) | Qualitative/UK | Semistructured interviews and framework approach for qualitative data analysis | 38 patients (mean age—67.5) and 32 health care professionals/COPD and HF | To explore the views of patients and professionals on telemonitoring and its impact on continuity of care |
| Fairbrother et al. (2013) | Qualitative/UK | Semistructured interviews and framework approach for qualitative data analysis | 18 patients (mean age—75) and 5 health care professionals (1 GP, 3 nurses, 1 IT professional)/HF | To understand the views of patients and professionals on the acceptability and perceived usefulness of day‐to‐day provision of telemonitoring for HF |
| Gale and Sultan (2013) | Qualitative/UK | Situational interviews and framework approach for qualitative data analysis | 18 patients (mean age—69)/COPD | To understand how people with COPD negotiated incorporating telehealth technologies into their everyday life and home space and understand WHY they valued it |
| Guzman‐Clark et al. (2013) | Quantitative correlation/USA | Secondary analysis of data from the Department of Veterans Affairs | 248 patients (mean age—76)/HF | To examine home telehealth adherence and its potential predictors and outcomes |
| Hardisty et al. (2011) | Qualitative/UK | Multipath mapping using literature review, interviews with key informants, and focus group interviews with patients and caregivers | 16 patients and 7 caregivers (mean age—not available); 26 key informants of academic researchers, nonacademic clinicians, and policy makers/COPD and HF | To propose a research agenda that addresses technological and other knowledge gaps in developing telemonitoring solutions for patient with chronic diseases, with particular focus on detecting deterioration early enough to intervene effectively |
| Hibbert et al. (2004) | Qualitative ethnographic/UK | Participant observation within a randomized controlled trial | 12 nurses/COPD | To study the socio‐technical processes involved in the implementation of a home telehealth nursing service for patients with COPD, within a RCT |
| Juretic et al. (2012) | Quantitative correlation/USA | Secondary analysis of data from the Department of Veterans Affairs | 132 patients (mean age—73)/COPD | To evaluate predictors of attrition of veterans with chronic medical conditions who were enrolled in a Veterans Administration Care Coordination Home Telehealth program |
| Kaufman et al. (2006) | Quantitative descriptive/USA | Usability evaluation | 16 patients (mean age—unknown)/Diabetes | To present a framework for understanding and reducing barriers for older adults to effectively use health information systems designed for disease management |
| Lamothe et al. (2006) | Qualitative/Canada | Participant observations, document review, interviews focus groups | 82 participants including managers, home care staff, and patients from three sites/HTN, COPD, and HF | To explore the dynamics taking place with the introduction of tele‐homecare for the treatment of elderly people suffering from severe chronic conditions |
| Mair, Hiscock, and Beaton (2008) | Qualitative/UK | Process evaluation of a randomized controlled trial | 9 patients (mean age—unknown) and 11 nurses/COPD | To perform a process evaluation of a RCT of home telecare for the management of acute exacerbations of COPD |
| Peeters et al. (2012) | Quantitative descriptive/Netherlands | Questionnaire/survey and multiple regression | 254 patients (mean age—77)/Arthritis, HF, and Diabetes | To provide insight into client characteristics and characteristics of home telecare contacts, which may influence the adoption of home telecare. Also to examine the applicability of four perceived attributes in Rogers' diffusion of innovations theory, which may influence adoption: relative advantage, compatibility, complexity, and observability |
| Rogers et al. (2011) | Qualitative/UK | Semistructured interviews | 31 patients (mean age unknown) and spouses/Diabetes, COPD, HF | To illuminate how people experience, understand, and negotiate the transfer of technologies into their homes; to examine the extent to which telecare systems are incorporated into the life world of patients and carers and the factors that promote or inhibit their integration |
| Radhakrishnan, Jacelon, and Roche (2012) | Mixed‐method design combining descriptive correlation of data and qualitative analysis/USA | Quantitative—Demiris' patients impressions of home telecare instrument Qualitative—Focus group interviews of nurses and interviews with patients | 31 home care nurses and 4 patients (mean age 75)/HF | To explore perceptions on effectiveness of telehealth for HF management beyond the initial acceptance phase in a home care setting |
| Radhakrishnan et al. (2013) | Quantitative correlation/USA | Retrospective chart review of home health electronic health records | 403 patients (mean age = 75)/HF | To examine the association of the comorbidity characteristics of HF patients with nursing utilization along with withdrawal from telehealth service during an episode of tele‐home care |
| Sanders et al. (2012) | Qualitative/UK | Semistructured interviews of participants within a large randomized controlled trial Whole System Demonstrator (WSD) project | 22 patients (mean age—71) who declined to participate in the RCT or who withdrew from the intervention arm/COPD, HF, Diabetes | To explore barriers to participation and adoption of telehealth and telecare from the perspective of people who declined to participate or withdrew from a RCT |
| West and Milio (2004) | Qualitative case study/USA | Semistructured interviews, administrative document review, patient chart review, and field observations | 16 interviews: 5 with homecare staff and 9 with affiliated organizations/HF, Diabetes, COPD, HTN | To provide an in‐depth, descriptive analysis of the implementation and use of HCO's telemedicine program and the implications for future utilization of telemedicine by homecare organizations |
RCT, randomized controlled trial; COPD, chronic obstructive pulmonary disorder; HTN, hypertension.
The tele‐homecare program model in all the studies typically involved the daily transmission of health‐related data via tele‐homecare devices by patients in their homes in conjunction with home nursing visits. A tele‐homecare coordinator reviewed patients' transmitted tele‐homecare data daily at the home health agency sites; the data were prioritized according to preset alerts for specific signs and symptoms. Home health nurses followed up abnormal alerts by contacting the referring physician or the patient for further information through phone or home visits.
Key Findings
The determinants of sustainability of tele‐homecare programs are presented in this section (see Appendix SA2). Barriers to and facilitators for sustainability of home tele‐homecare programs were categorized into six themes: (1) perceptions of effectiveness, comprising clinicians' and patients' perceptions of the effectiveness of tele‐homecare programs for achieving intended clinical or behavioral outcomes; (2) tailoring to patients, comprising the tailoring of tele‐homecare programs to patient‐centered factors and needs; (3) nurse–patient communication and collaboration, reflecting aspects of the nurse–patient relationship; (4) interprofessional communication and collaboration, comprising negotiation of patient care among health care professionals from different disciplines; (5) organization of process and culture, indicating the impact of existing home health agency organizational culture and process; and (6) quality of tele‐homecare technology, presenting the impact of usability and innovation of tele‐homecare technology. We discuss these six themes in detail below.
Perceptions of Effectiveness
Home health clinicians debated the clinical or cost‐effectiveness of tele‐homecare programs in achieving patient outcomes such as reducing hospitalizations or improving self‐management behaviors (Hibbert et al. 2004; West and Milio 2004; Mair, Hiscock, and Beaton 2008; Hardisty et al. 2011; Radhakrishnan, Jacelon, and Roche 2012). Home health nurses reported a lack of training in or orientation to tele‐homecare programs and, as a result, a lack of understanding on how tele‐homecare might be utilized to improve or achieve intended clinical or behavioral outcomes in their patients (West and Milio 2004; Radhakrishnan, Jacelon, and Roche 2012). In addition, clinicians perceived that tele‐homecare can be ineffective in identifying disease exacerbation, due to recent evidence suggesting that current tele‐homecare alert thresholds based on simple individual parameters such as weight data instead of a complex alert management system that includes other patient data might not be a sufficiently early indicator of a patient's impending disease crisis (Hardisty et al. 2011).
Patients typically reported a more positive experience with tele‐homecare than did clinicians. Patients felt that tele‐homecare promoted daily self‐monitoring activities, and they were satisfied that the clinicians were monitoring their tele‐homecare readings daily (Lamothe et al. 2006; Gale and Sultan 2013). However, clinicians perceived that patients' reliance on clinicians' daily tele‐homecare monitoring introduced a paradoxical threat to patients' independence and self‐reliance (Rogers et al. 2011; Fairbrother et al. 2012; Radhakrishnan, Jacelon, and Roche 2012; Sanders et al. 2012). Clinicians debated whether the focus of current tele‐homecare programs on patient compliance with transmission of vital signs increased patients' confidence in managing their conditions or promoted patients' dependence on clinicians by preempting patients from independently interpreting their disease status or making decisions about self‐management (Rogers et al. 2011; Fairbrother et al. 2012; Radhakrishnan, Jacelon, and Roche 2012; Sanders et al. 2012). This continuing uncertainty about the clinical effectiveness of tele‐homecare programs was an adverse predictor of the sustainability of tele‐homecare programs.
Tailoring to Patients
Tele‐homecare programs were perceived as being suitable for certain individuals or medical circumstances as opposed to all of them (Hardisty et al. 2011). Knowing the patient allowed for contextualizing the tele‐homecare data relative to the individual patient's current health status, capability, and situation as well as for targeting nursing interventions to the patient's specific needs (Fairbrother et al. 2012, 2013; Peeters et al. 2012; Sanders et al. 2012). Criteria for appropriate selection of patients for tele‐homecare programs would allow maximizing the benefits of tele‐homecare to achieve intended patient outcomes (West and Milio 2004; Kaufman et al. 2006; Lamothe et al. 2006; Juretic et al. 2012; Radhakrishnan, Jacelon, et al. 2013; Radhakrishnan, Jacelon, and Roche 2012; Guzman‐Clark et al. 2013). Implementation of tele‐homecare programs and collection of tele‐homecare data without a clear aim or relevance to a patient's situation adversely impacted the sustainability of tele‐homecare programs.
Nurse–Patient Communication and Collaboration
In general, patients perceived an increased sense of security and reassurance along with improved access to clinicians as benefits of tele‐homecare programs (Hardisty et al. 2011; Rogers et al. 2011; Radhakrishnan, Jacelon, and Roche 2012; Fairbrother et al. 2013; Gale and Sultan 2013). Patients and providers perceived that tele‐homecare facilitated continuity in home health nursing care through daily remote monitoring, surveillance, and support, which otherwise would not have been possible (Hibbert et al. 2004; Mair, Hiscock, and Beaton 2008; Fairbrother et al. 2012, 2013). After all, daily in‐home visits are not feasible, especially when patients live in remote or rural areas. Continuity of care not only improved relationships between patients and providers but also enhanced providers' understanding of patients' unique situations and patients' levels of knowledge about their conditions. Home health nurses' timely feedback in response to tele‐homecare data or alerts significantly influenced sustained adherence of patients in tele‐homecare interventions (Hardisty et al. 2011; Fairbrother et al. 2012, 2013; Juretic et al. 2012; Peeters et al. 2012). Patients felt cared for or watched over when home health providers responded in a timely manner to tele‐homecare data, and they had better self‐management outcomes because the nurses helped them connect the dots between data, behavior, and consequences. However, technical difficulties impacted the quality of tele‐homecare communication, so that tele‐homecare was sometimes perceived as unhelpful in establishing effective relationships with patients (Hibbert et al. 2004; Mair, Hiscock, and Beaton 2008).
Interprofessional Communication and Collaboration
Interactions between health care professionals involved in tele‐homecare delivery were problematic at times, because clinical roles and responsibilities as well as responses to abnormal tele‐homecare data and expectations about patient outcomes were not delineated (Lamothe et al. 2006; Mair, Hiscock, and Beaton 2008; Hardisty et al. 2011; Fairbrother et al. 2012). On the other hand, collaborative and trustworthy relationships developed between nurses and doctors in a tele‐homecare program that included standardized teaching about shared goals for patient outcomes (Lamothe et al. 2006). Medico‐legal issues related to patient safety were a concern among clinicians who delivered care through tele‐homecare programs, because clinicians might be held accountable for missing signs and symptoms in tele‐homecare data that were indicative of a patient in crisis (Mair, Hiscock, and Beaton 2008). Lack of interoperability between home health agencies providing tele‐homecare services and existing patient information systems in primary care frustrated health care professionals (Hardisty et al. 2011; Fairbrother et al. 2012, 2013; Radhakrishnan, Jacelon, and Roche 2012) because this “compartmentalized data” (Fairbrother et al. 2012), further hindering the sharing of information on care delivery to patients among health care professionals.
Organization of Process and Culture
Top‐down decision making by managers and high‐level executives was commonly associated with the adoption of tele‐homecare in the home health care system (Hibbert et al. 2004; Fairbrother et al. 2012; Radhakrishnan, Jacelon, and Roche 2012). Potential economic benefits of using tele‐homecare as a means of driving down service costs or diminishing budgets was perceived as the main impulse behind the adoption of tele‐homecare programs by executives in the home health agencies (Fairbrother et al. 2012). The input of stakeholders, especially those of end users of tele‐homecare such as home health nurses and patients, was rarely sought either in the design of tele‐homecare devices or in the implementation of tele‐homecare programs (West and Milio 2004). As a result, professional resistance to tele‐homecare programs was sometimes reported among nurses, who perceived tele‐homecare programs as a “threat to nurses' identity” (Mair, Hiscock, and Beaton 2008) that undermined their credibility and professional security (Hibbert et al. 2004). In addition, tele‐homecare programs changed traditional home health nursing work arrangements because of work involved in monitoring and responding to tele‐homecare data, installing devices and training patients, and resolving technical difficulties, as well as owing to increased communication and interaction with patients (Hibbert et al. 2004; West and Milio 2004; Mair, Hiscock, and Beaton 2008; Radhakrishnan, Jacelon, and Roche 2012; Fairbrother et al. 2013). Poor home health workflow adaptability to tele‐homecare programs often resulted in the perception of increased workload by home health nurses, which adversely impacted the sustainability of tele‐homecare programs.
Quality of Tele‐Homecare Technology
Device usability was a problem cited more often in studies conducted in the early 2000s rather than later. Participants (mainly patients) reported ease of use and in‐home convenience of tele‐homecare device use (Peeters et al. 2012; Radhakrishnan, Jacelon, and Roche 2012), but devices were also found to be cumbersome, with poor speech and picture quality (Hardisty et al. 2011) and numerous connectivity and transmission issues (West and Milio 2004; Radhakrishnan, Jacelon, and Roche 2012). Tele‐homecare devices must be tailored for use by older people and must be sensitive to their cognitive and motor skills as well as their health and computer literacy level (Kaufman et al. 2006). Also, some tele‐homecare programs continued to use primitive, simple thresholds for vital sign parameters as a basis for triggering alerts, as opposed to automated and sophisticated analysis of longitudinal data (Hardisty et al. 2011; Fairbrother et al. 2012). Use of tele‐homecare technology that did not incorporate innovative technological advances was an adverse predictor of sustainability of tele‐homecare programs.
Discussion and Implications
In this review, we have synthesized recent evidence on barriers to and facilitators for the sustainability of tele‐homecare programs at home health agencies. While the literature has focused extensively on the clinical and behavioral effectiveness of home telehealth programs (Polisena et al. 2009; Paré et al. 2010; Radhakrishnan and Jacelon 2012), to our knowledge this is the first review to systematically assess the sustainability of tele‐homecare programs in home health agencies, which represent one of the fastest growing health care sectors and an important care setting for the management of chronic diseases for older adults living in the community.
The review's findings revealed that patients' levels of satisfaction with tele‐homecare programs were far more positive than those of clinicians. This finding was echoed in another review on patients' sustained adoption of telehealth (Gorst et al. 2014). Several of the factors affecting patients' use of home telehealth identified in that review—perceptions of increased access to health care providers, improved knowledge, peace of mind, technical problems, and preference for in‐person care—have been identified in the present review as well.
Home health nurses, on the other hand, expressed concern about the utility of tele‐homecare programs to foster self‐management behaviors in patients and consequently about their health outcomes. Lack of home health nurses' training and orientation to make tele‐homecare effective for their patients can be alleviated by providing clear guidelines and protocols for the application of tele‐homecare to foster patient self‐management behaviors, effective mechanism for feedback and response to patient self‐monitoring actions, and renegotiation of the patient–clinician relationship to empower the patients themselves (Horton 2008). Perceptions on the effectiveness of tele‐homecare to identify patients in crisis and/or in need of suitable interventions can be improved through use of intelligent tele‐homecare alert management systems based on qualitative parameters of symptoms, patients' contexts including their self‐care behaviors and disease status, and psychosocial factors such as presence of anxiety or depression in addition to vital signs (Hardisty et al. 2011; Radhakrishnan, Bowles, et al. 2013). Additionally, to increase the relevance of tele‐homecare programs to a patient's situation, criteria for patient characteristics can be identified to tailor tele‐homecare service delivery to individual patients' capabilities and context. However, there is a need for future research to identify such criteria, because many studies tend to exclude patients with the characteristic limitations of those who are older (e.g., cognitive and visual impairment, communication barriers, hearing problems) (van den Berg et al. 2012).
To facilitate interprofessional collaboration, future tele‐homecare programs must recognize a formal reorganization of work between the staffs of home health agencies and clinics that will include partnership and accountability negotiation, system interoperability, and shared vision of patient care management (Horton 2008; Mair, Hiscock, and Beaton 2008; Hardisty et al. 2011). In addition, the benefits of implementing tele‐homecare programs, especially improvements in overall patient outcomes and economic benefits as defined by cost–benefit analyses, need to be advertised to all stakeholders periodically to sustain their engagement. The need for role negotiation among various clinicians involved in tele‐homecare delivery and training to recognize and achieve a shared vision in care management has also been observed in a review on telemedicine programs for COPD (Bartoli et al. 2009). While financial reimbursements for tele‐homecare services by private or government health insurance agencies alone will not sustain tele‐homecare programs, they can certainly support tele‐homecare programs' economic feasibility (Wade et al. 2010).
It is important that the development and deployment of future tele‐homecare programs retain the active involvement and engagement of stakeholders, especially nurses and patients, during all stages of deployment from planning to actual implementation. For tele‐homecare programs to become fully incorporated into routine home health service delivery, it is essential to address home health nurses' concerns regarding increased workload, communication, safety, and effectiveness. This will provide feedback for the implementation of tele‐homecare programs that are minimally disruptive to workflows and routines. Clinicians' acceptance of tele‐homecare services was identified as a key factor of sustainability in a study on Australian tele‐homecare services (Wade, Eliott, and Hiller 2014). Home health nurses should be periodically oriented not only in the actual use of tele‐homecare technology but also in the effective deployment of tele‐homecare to achieve intended patient outcomes.
Finally, the sustainability of tele‐homecare programs can be enhanced by improving the quality of tele‐homecare technology including technical quality of communication. Because the target population of tele‐homecare programs typically consists of older adults with chronic diseases, device usability must be specifically tailored to the cognitive and physical capabilities of older adults. In addition to intelligent alert management, the use of innovative visual displays can have a profound influence on patients' and clinicians' decision making and communication, influencing not only how quickly one can interpret information but also how the information is interpreted (Le et al. 2013). Future research can incorporate advances in computer science to enhance the collection, processing, and visualization of tele‐homecare data for more meaningful presentations that are sensitive to patients' and clinicians' needs.
Limitations
The lack of any standardized definition of tele‐homecare in the literature led us to employ a broad range of search terms and exclusion of a large number of identified studies because they did not address our immediate topic of interest. Also, by considering only English‐language articles, we may have excluded other relevant studies. There remains a possibility as well that research on many of the tele‐homecare programs implemented by home health agencies has not yet been submitted or completed the peer‐review process. These limitations aside, this review suggests several implications for home health agencies regarding the implementation of an innovative care delivery program such as tele‐homecare in a sustainable manner.
Conclusion
This review presents findings and implications based on a critical examination of evidence from 16 studies in which home health agencies used tele‐homecare programs for chronic disease management. In summary, the sustainability of tele‐homecare programs was found to be influenced by home health nurses' and patients' perceptions on effectiveness of tele‐homecare programs to achieve clinical and behavioral outcomes; the degree to which tele‐homecare programs are tailored to patient‐centered factors and needs; the role played by tele‐homecare programs in nurse–patient or interprofessional communication and relationships; the organizational culture and process within home health agencies; and quality of the tele‐homecare technology.
Supporting information
Appendix SA1: Author Matrix.
Appendix SA2: Determinants of Sustainability of Tele‐Homecare Programs.
Appendix SA3: Excluded Articles.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors gratefully acknowledge the editorial services of John Bellquist, Editor, CAIN Center and the NINR funded Center for Transdisciplinary Collaborative Research in Self‐management Science (TCRSS), School of Nursing, University of Texas at Austin. Dr. Bo Xie's start‐up funds at the University of Texas–Austin and Ed and Molly Smith Centennial Fellowship in Nursing.
Disclosures: None of the authors associated with this work report any conflict of interest in conducting this review.
Disclaimers: None.
References
- Bartoli, L. , Zanaboni P., Masella C., and Ursini N.. 2009. “Systematic Review of Telemedicine Services for Patients Affected by Chronic Obstructive Pulmonary Disease (COPD).” Telemedicine and e‐Health 15 (9): 877–83. [DOI] [PubMed] [Google Scholar]
- van den Berg, N. , Schumann M., Kraft K., and Hoffmann W.. 2012. “Telemedicine and Telecare for Older Patients—A Systematic Review.” Maturitas 73 (2): 94–114. [DOI] [PubMed] [Google Scholar]
- Bowles, K. H. , and Baugh A. C.. 2007. “Applying Research Evidence to Optimize Telehomecare.” Journal of Cardiovascular Nursing 22 (1): 5–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2013. “Deaths and Mortality” [accessed on October 20, 2014]. Available at http://www.cdc.gov/nchs/fastats/deaths.htm
- Centers for Medicare & Medicaid Services . 2013a. “CY 2014 Home Health Prospective Payment System Rate Update, Conversion to ICD‐10‐CM, Home Health Quality Reporting Requirements, and Cost Allocation of Home Health Survey Expenses” [accessed on September 27, 2014]. Available at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HomeHealthPPS/Home-Health-Prospective-Payment-System-Regulations-and-Notices-Items/CMS-1450-P.html
- Centers for Medicare & Medicaid Services . 2013b. “Home Health Providers” [accessed on February 5, 2014]. Available at http://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/HHAs.html
- Clark, R. A. , Inglis S. C., McAlister F. A., Cleland J. G. F., and Stewart S.. 2007. “Telemonitoring or Structured Telephone Support Programmes for Patients with Chronic Heart Failure: Systematic Review and Meta‐Analysis.” British Medical Journal 334: 942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cradduck, T. D. 2002. “Sustainability—The Holy Grail of Telehealth?” Journal of Telemedicine and Telecare 8 (Suppl 2): 7–8. [DOI] [PubMed] [Google Scholar]
- Dansky, K. H. , Bowles K. H., and Palmer L.. 2003. “Clinical Outcomes of Telehomecare for Diabetic Patients Receiving Homecare.” The Journal on Information Technology in Healthcare 1 (1): 61–74. [Google Scholar]
- Fairbrother, P. , Pinnock H., Hanley J., McCloughan L., Sheikh A., Pagliari C., and McKinstry B.. 2012. “Continuity, But at What Cost? The Impact of Telemonitoring COPD on Continuities of Care: A Qualitative Study.” Primary Care Respiratory Journal 21 (3): 322–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbrother, P. , Ure J., Hanley J., McCloughan L., Denvir M., Sheikh A., McKinstry B., and the Telescot Programme Team . 2013. “Telemonitoring for Chronic Heart Failure: The Views of Patients and Healthcare Professionals—A Qualitative Study.” Journal of Clinical Nursing 23 (1–2): 132–44. [DOI] [PubMed] [Google Scholar]
- Fazzi, R. , Ashe T., and Doak L.. 2008. “Telehealth, Disease Management, Home Care and the Future—Part 2.” Caring 27 (1): 36–8, 40–1, 3. [PubMed] [Google Scholar]
- Fazzi Associates . 2014. National State of the Industry Report for Home Health and Hospice 2013‐2014 [accessed on January 10, 2014]. Available at http://www.fazzi.com/id-2013-state-of-the-home-care-industry-study.html [Google Scholar]
- Gale, N. , and Sultan H.. 2013. “Telehealth as ‘Peace of Mind’: Embodiment, Emotions and the Home as the Primary Health Space for People with Chronic Obstructive Pulmonary Disorder.” Health & Place 21: 140–7. [DOI] [PubMed] [Google Scholar]
- Gorst, S. L. , Armitage C. J., Brownsell S., and Hawley M. S.. 2014. “Home Telehealth Uptake and Continued Use among Heart Failure and Chronic Obstructive Pulmonary Disease Patients: A Systematic Review.” Annals of Behavioral Medicine. doi:10.1007/s12160‐014‐9607‐x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzman‐Clark, J. R. S. , van Servellen G., Chang B., Mentes J., and Hahn T. J.. 2013. “Predictors and Outcomes of Early Adherence to the Use of a Home Telehealth Device by Older Veterans with Heart Failure.” Telemed and e‐Health 19 (3): 217–23. [DOI] [PubMed] [Google Scholar]
- Hardisty, A. R. , Peirce S. C., Preece A., Bolton C. E., Conley E. C., Gray W. A., Rana O. F., Yousef Z., and Elwyn G.. 2011. “Bridging Two Translation Gaps: A New Informatics Research Agenda for Telemonitoring of Chronic Disease.” International Journal of Medical Informatics 80 (10): 734–44. [DOI] [PubMed] [Google Scholar]
- Henderson, R. 2012. “Employment Outlook: 2010‐2020. Industry Employment and Output Projections to 2020.” Monthly Labor Review, January, 2012 [accessed on October 7, 2014]. Available at http://www.bls.gov/opub/mlr/2012/01/art4full.pdf [Google Scholar]
- Hibbert, D. , Mair F. S., May C. R., Boland A., O'Connor J., Capewell S., and Angus R. M.. 2004. “Health Professionals' Responses to the Introduction of a Home Telehealth Service.” Journal of Telemedicine and Telecare 10 (4): 226–30. [DOI] [PubMed] [Google Scholar]
- Higgins J. P. T., and Green S. (Eds). 2011. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; [accessed on July 15, 2013]. Available at http://www.cochrane-handbook.org [Google Scholar]
- Horton, K. 2008. “The Use of Telecare for People with Chronic Obstructive Pulmonary Disease: Implications for Management.” Journal of Nursing Management 16 (2): 173–80. [DOI] [PubMed] [Google Scholar]
- Humphries, S. , Stafinski T., Mumtaz Z., and Menon D.. 2014. “Barriers and Facilitators to Evidence‐Use in Program Management: A Systematic Review of the Literature.” BMC Health Services Research 14: 171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jencks, S. F. , Williams M. V., and Coleman E. A.. 2009. “Rehospitalizations among Patients in the Medicare Fee‐for‐Service Program.” New England Journal of Medicine 360 (14): 1418–28. [DOI] [PubMed] [Google Scholar]
- Juretic, M. , Hill R., Hicken B., Luptak M., Rupper R., and Bair B.. 2012. “Predictors of Attrition in Older Users of a Home‐Based Monitoring and Health Information Delivery System.” Telemedicine and e‐Health 18 (9): 709–12. [DOI] [PubMed] [Google Scholar]
- Kaufman, D. R. , Pevzner J., Hilliman C., Weinstock R. S., Teresi J., Shea S., and Starren J.. 2006. “Redesigning a Telehealth Diabetes Management Program for a Digital Divide Seniors Population.” Home Health Care Management & Practice 18: 223–34. [Google Scholar]
- Klersy, C. , De Silvestri A., Gabutti G., Regoli F., and Auricchio A.. 2009. “A Meta‐Analysis of Remote Monitoring of Heart Failure Patients.” Journal of the American College of Cardiology 54 (18): 1683–94. [DOI] [PubMed] [Google Scholar]
- Klersy, C. , De Silvestri A., Gabutti G., Raisaro A., Curti M., Regoli F., and Auricchio A.. 2011. “Economic Impact of Remote Patient Monitoring: An Integrated Economic Model Derived from a Meta‐Analysis of Randomized Controlled Trials in Heart Failure.” European Journal of Heart Failure 13 (4): 450–9. [DOI] [PubMed] [Google Scholar]
- Lamothe, L. , Fortin J.‐P., Labbé F., Gagnon M.‐P., and Messikh D.. 2006. “Impacts of Telehomecare on Patients, Providers, and Organizations.” Telemedicine and e‐Health 12 (3): 363–9. [DOI] [PubMed] [Google Scholar]
- Le, T. , Reeder B., Thompson H., and Demiris G.. 2013. “Health Providers' Perceptions of Novel Approaches to Visualizing Integrated Health Information.” Methods of Information in Medicine 52 (3): 250–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair, F. S. , Hiscock J., and Beaton S. C.. 2008. “Understanding Factors That Inhibit or Promote the Utilization of Telecare in Chronic Lung Disease.” Chronic Illness 4 (2): 110–7. [DOI] [PubMed] [Google Scholar]
- May, C. R. , Finch T. L., Cornford J., Exley C., Gately C., Kirk S., Jenkings K. N., Osbourne J., Robinson A. L., Rogers A., Wilson R., and Mair F. S.. 2011. “Integrating Telecare for Chronic Disease Management in the Community: What Needs to Be Done?” BMC Health Services Research 11: 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher, D. , Liberati A., Tetzlaff J., Altman D. G., and the PRISMA Group . 2009. “Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: The PRISMA Statement.” PLoS Medicine 6 (7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association for Home Care & Hospice . 2010. Basic Statistics about Homecare. Washington, DC: NAHCH. [Google Scholar]
- Pace, R. , Pluye P., Bartlett G., Macaulay A. C., Salsberg J., Jagosh J., and Seller R.. 2012. “Testing the Reliability and Efficiency of the Pilot Mixed Methods Appraisal Tool (MMAT) for Systematic Mixed Studies Review.” International Journal of Nursing Studies 49 (1): 47–53. [DOI] [PubMed] [Google Scholar]
- Pandor, A. , Thokala P., Gomersall T., Baalbaki H., Stevens J., Wang J., Wong R., Brennan A., and Fitzgerald P.. 2013. “Home Telemonitoring or Structured Telephone Support Programmes after Recent Discharge in Patients with Heart Failure: Systematic Review and Economic Evaluation.” Health Technology Assessment 17 (32): 1–207, v–vi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paré, G. , Moqadem K., Pineau G., and St‐Hilaire C.. 2010. “Clinical Effects of Home Telemonitoring in the Context of Diabetes, Asthma, Heart Failure and Hypertension: A Systematic Review.” Journal of Medical Internet Research 12 (2): e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters, J. M. , de Veer A. J. E., van der Hoek L., and Francke A. L.. 2012. “Factors Influencing the Adoption of Home Telecare by Elderly or Chronically Ill People: A National Survey.” Journal of Clinical Nursing 21 (21–22): 3183–93. [DOI] [PubMed] [Google Scholar]
- Polisena, J. , Coyle D., Coyle K., and McGill S.. 2009. “Home Telehealth for Chronic Disease Management: A Systematic Review and an Analysis of Economic Evaluations.” International Journal of Technology Assessment in Health Care 25 (3): 339–49. [DOI] [PubMed] [Google Scholar]
- Radhakrishnan, K. , and Jacelon C.. 2012. “Impact of Telehealth on Patient Self‐Management of Heart Failure: A Review of Literature.” Journal of Cardiovascular Nursing 27 (1): 33–43. [DOI] [PubMed] [Google Scholar]
- Radhakrishnan, K. , Jacelon C., and Roche J.. 2012. “Perceptions on the Use of Telehealth by Homecare Nurses and Patients with Heart Failure: A Mixed Method Study.” Home Health Care Management & Practice 24 (4): 175–81. [Google Scholar]
- Radhakrishnan, K. , Bowles K. H., Hanlon A., Topaz M., and Chittams J.. 2013. “A Retrospective Study on Patient Characteristics and Telehealth Alerts Indicative of Key Medical Events for Heart Failure (HF) Patients at a Home Health Agency.” Telemedicine Journal and E‐health 19 (9): 664: 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radhakrishnan, K. , Jacelon C. S., Bigelow C., Roche J. P., Marquard J. L., and Bowles K. H.. 2013. “Association of Comorbidities with Home Care Service Utilization of Patients with Heart Failure While Receiving Telehealth.” Journal of Cardiovascular Nursing 28 (3): 216–27. [DOI] [PubMed] [Google Scholar]
- Rogers, A. , Kirk S., Gately C., May C. R., and Finch T.. 2011. “Established Users and the Making of Telecare Work in Long Term Condition Management: Implications for Health Policy.” Social Science & Medicine 72 (7): 1077–84. [DOI] [PubMed] [Google Scholar]
- Sanders, C. , Rogers A., Bowen R., Bower P., Hirani S., Cartwright M., Fitzpatrick R., Knapp M., Barlow J., Hendy J., Chrysanthaki T., Bardsley M., and Newman S. P.. 2012. “Exploring Barriers to Participation and Adoption of Telehealth and Telecare within the Whole System Demonstrator Trial: A Qualitative Study.” BMC Services Research 12: 220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea, K. , and Chamoff B.. 2012. “Telehomecare Communication and Self‐Care in Chronic Conditions: Moving toward a Shared Understanding.” Worldviews Evidence‐Based Nursing 9 (2): 109–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udsen, F. W. , Hejlesen O., and Ehlers L. H.. 2014. “A Systematic Review of the Cost and Cost‐Effectiveness of Telehealth for Patients Suffering from Chronic Obstructive Pulmonary Disease.” Journal of Telemedicine and Telecare. doi:10.1177/1357633X14533896. [DOI] [PubMed] [Google Scholar]
- Wade, V. , and Eliott J.. 2012. “The Role of the Champion in Telehealth Service Development: A Qualitative Analysis.” Journal of Telemedicine and Telecare 18 (8): 490–2. [DOI] [PubMed] [Google Scholar]
- Wade, V. A. , Eliott J. A., and Hiller J. E.. 2014. “Clinician Acceptance Is the Key Factor for Sustainable Telehealth Services.” Qualitative Health Research 24 (5): 682–94. [DOI] [PubMed] [Google Scholar]
- Wade, V. , Eliott J., Karnon J., and Elshaug A. G.. 2010. “A Qualitative Study of Sustainability and Vulnerability in Australian Telehealth Services.” Studies in Health Technology and Informatics 161: 190–201. [PubMed] [Google Scholar]
- West, V. , and Milio N.. 2004. “Organizational and Environmental Factors Affecting the Utilization of Telemedicine in Rural Home Healthcare.” Home Health Care Services Quarterly 23 (4): 49–67. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Determinants of Sustainability of Tele‐Homecare Programs.
Appendix SA3: Excluded Articles.


