Abstract
Ankle instability is a condition that often requires surgery to stabilize the ankle joint that will improve pain and function if nonoperative treatments fail. Ankle stabilization surgery may be performed as a repair in which the native existing anterior talofibular ligament or calcaneofibular ligament (or both) is imbricated or reattached. Alternatively, when native ankle ligaments are insufficient for repair, a reconstruction of the ligaments may be performed in which an autologous or allograft tendon is used to reconstruct the anterior talofibular ligament or calcaneofibular ligament (or both). Currently, ankle stabilization surgery is most commonly performed through an open incision, but arthroscopic ankle stabilization using repair techniques has been described and is being used more often. We present our technique for anatomic ankle arthroscopic reconstruction of the lateral ligaments (anti-ROLL) performed in an all–inside-out manner that is likely safe for patients and minimally invasive.
Ankle instability is a problem that requires surgical treatment to improve pain and function if nonoperative treatments fail.1, 2 Many open surgical techniques have been described to repair or reconstruct the lateral ligaments of the ankle, specifically the anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL). Open surgical repair techniques are designed to reattach or imbricate the ATFL and CFL,3, 4, 5, 6 whereas open surgical reconstruction techniques are designed to replace an absent or incompetent ATFL and CFL in an anatomic or nonanatomic fashion.7, 8, 9, 10, 11, 12, 13, 14 This article describes our surgical technique for ankle arthroscopic reconstruction of the lateral ligaments (anti-ROLL) performed in an all–inside-out manner that is likely safe for patients and minimally invasive.
Surgical Technique
Step 1: Landmark Drawing, Portal Placement, and Patient Positioning
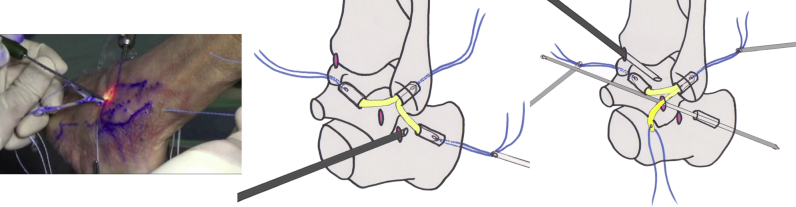
The anatomic landmarks should always be drawn on the patient's skin before anesthesia administration, when the patient is awake and able to voluntarily contract the muscular landmarks (Fig 1, Video 1). First, the bony landmarks are drawn, including the distal edge of the tibial plafond, as well as the medial and lateral malleolus; then, the extensor digitorum longus and tibialis posterior tendon are traced. Next, 3 portals are drawn, including the medial midline (MML) portal located just lateral to the tibialis anterior tendon and just below the tibial plafond. The accessory anterolateral (AAL) portal is positioned just lateral to the extensor digitorum longus tendon and 1.5 cm below the tibial plafond (or level with the distal fibula). The subtalar (ST) portal is positioned with the ankle in extension at the tip of the lateral malleolus near the superior border of the peroneal tendon. An optional fourth portal may be used to access any additional pathology in the lateral tibiotalar region (an anterolateral portal located just lateral to the extensor digitorum longus tendon and just below the tibial plafond).
Fig 1.
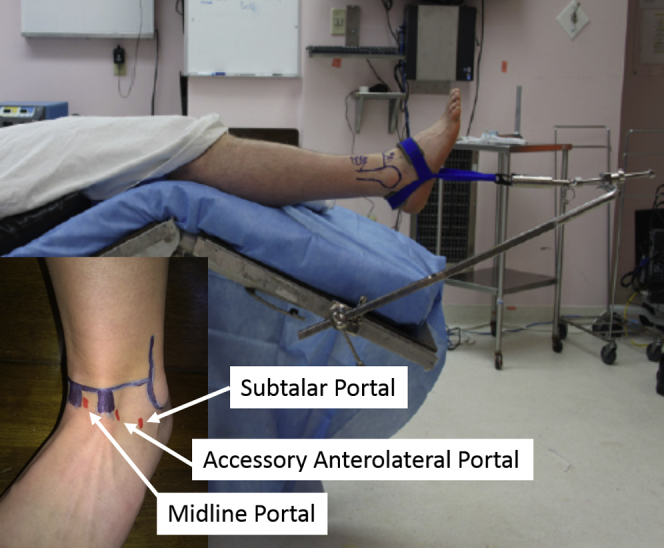
The patient is positioned in a semi–beach-chair manner with the hips and knees flexed and noninvasive distraction applied. The inset shows anatomic landmarks drawn on the patient's skin before anesthesia administration, including the subtalar, accessory anterolateral, and midline portals.
The patient is positioned supine with a sandbag under the ipsilateral hip to allow the foot to be pointing vertical. The hips and knees are flexed, and a disposable ankle harness is attached to the foot and ankle (Fig 1). A sterile noninvasive ankle Guhl distractor (Smith & Nephew, Memphis, TN) with a strain gauge monitor is then attached to the ankle harness. This will allow the scrubbed surgeon total control over the magnitude of traction applied to the patient's ankle during arthroscopy to assist in avoiding neurologic injury associated with excessive and prolonged traction and compression of the foot and ankle.15 It is important to note that distraction is not necessary for anti-ROLL but may be necessary for addressing any associated tibiotalar intra-articular pathology. Further it is also important to be sure that no traction is used while tensioning the ligament graft since this may counteract stabilization.
Step 2: Ankle Joint Access Through Arthroscopic Portals
The ankle joint is accessed by first infiltrating approximately 15 to 30 mL of sterile saline solution through the previously drawn MML portal site. The needle on the syringe is directed perpendicular to the leg in the sagittal plane and aimed at the anterior border of the fibula (approximately 30° in the coronal plane). The skin is then safely incised to protect the neural structures using the tip of a No. 10 scalpel blade with subsequent blunt dissection using a hemostat spreading technique. The joint is entered bluntly with the hemostat, followed by cannula insertion on the same line as the needle insertion. Once the arthroscope is inserted through the MML portal, the appropriate placement of the AAL portal is confirmed using a center of light from the arthroscope. The AAL portal is made using the same neural protection technique. Finally, a systematic inspection of the intra-articular structures can be made to identify any additional pathology and to determine whether there are sufficient ATFL and CFL fiber remnants to warrant an ankle stabilization repair technique rather than an ankle stabilization reconstruction technique. If there are insufficient ATFL and CFL fiber remnants to warrant a ligament repair, then one may proceed with ankle anti-ROLL.
Step 3: Constructing Anatomic Y-Graft for Ankle Anti-ROLL
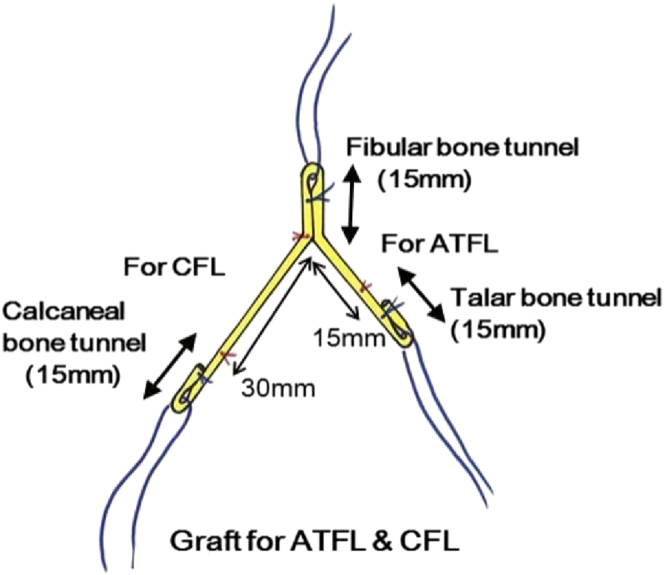
The surgeon and patient may choose an autograft (e.g., gracilis tendon) harvested from the patient's ipsilateral knee using a tendon harvester or an allograft of sufficient size (approximately 135 mm in length) and strength16 for the reconstruction of the ATFL and CFL. The graft is prepared in an anatomic Y configuration with graft loops at all 3 ends of the anatomic Y-graft to facilitate attachment of a suture for graft delivery (Fig 2). The base or fibular anchor site of the Y-graft is constructed by doubling the graft to a length of 15 mm. The calcaneal limb of the Y-graft is constructed to a total length of 55 mm, with the most distal 15 mm doubled to form the calcaneal bone tunnel anchor site. The talar limb of the Y-graft is constructed to a total length of 30 mm, with the most distal 15 mm doubled to form the talar bone tunnel anchor site.
Fig 2.
Construction of the anatomic Y-graft with graft loops at all 3 ends to facilitate attachment of a suture for graft delivery. The base or fibular anchor site of the Y-graft is constructed by doubling the graft to a length of 15 mm. The calcaneal limb of the Y-graft is constructed to a total length of 55 mm, with the most distal 15 mm doubled to form the calcaneal bone tunnel anchor site. The talar limb of the Y-graft is constructed to a total length of 30 mm, with the most distal 15 mm doubled to form the talar bone tunnel anchor site. (ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament.)
Step 4: Construction of Anti-ROLL Bone Tunnels
The interference screw technique used to secure the anatomic Y-graft described in this report is not technically challenging. However, constructing the 3 bone tunnels required to accept the Y-graft and interference screw is based on the passage of a guidewire through the recipient bone. It is essential to protect the local neurovascular structures when using these techniques to avoid the complications of a neurovascular injury. Although not described in this report, surgical techniques for surgeons to consider for fixation of the Y-graft to avoid neurovascular damage include the use of a custom drill guide system to more precisely pass the guidewire through the recipient bone. Alternately, there exist a number of devices that are adequate for fixation of the Y-graft that should be considered and may be safer than the passage of a guidewire through the recipient bone. Some of these devices include the Bioraptor (Smith & Nephew), JuggerKnot (Biomet, Warsaw, IN), and Bio-Tenodesis (Arthrex, Naples, FL).
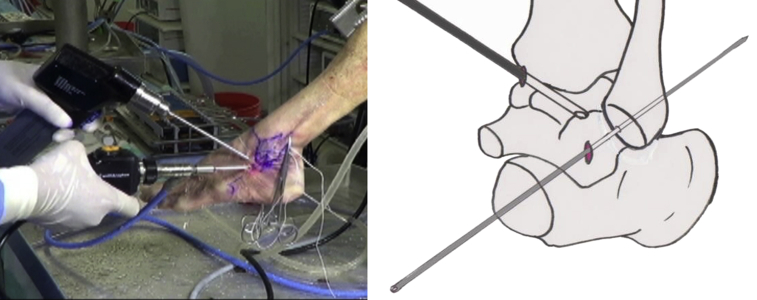
Fibular Bone Tunnel
The fibular bone tunnel is constructed to serve as the docking site for the fibular stem of the anatomic Y-graft (Fig 3). The arthroscope is inserted through the MML portal, which is used as the viewing portal, whereas the AAL is used as the working portal. A guidewire is inserted through the AAL portal to penetrate the fibula 8 mm distal to the fibular attachment of the ATFL and directed toward the proximal and posterior edge of the fibula at an angle of approximately 20° with respect to the long axis of the fibula. Care is taken to pass the guidewire through the central portion of the fibula in the coronal axis to prevent fracture with over-drilling. The guide pin is passed through the posterior cortex of the fibula and through the skin posterior to the fibula, with care taken not to damage the sural nerve. Over-drilling is then performed to a diameter of 6 mm and a depth of 20 mm.
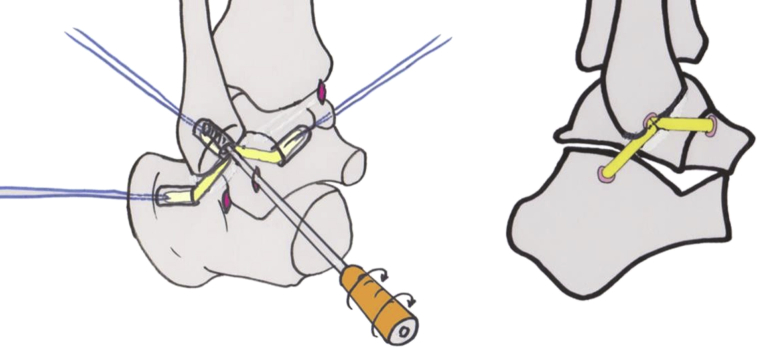
Fig 3.
Construction of the fibular bone tunnel to serve as the docking site for the fibular stem of the anatomic Y-graft. The arthroscope is inserted through the medial midline portal, which is used as the viewing portal, whereas the accessory anterolateral portal is used as the working portal. A guidewire is inserted through the accessory anterolateral portal to penetrate the fibula 8 mm distal to the fibular attachment of the anterior talofibular ligament and directed toward the proximal and posterior edge of the fibula at an angle of approximately 20° with respect to the long axis of the fibula. Care is taken to pass the guidewire through the central portion of the fibula in the coronal axis to prevent fracture with over-drilling.
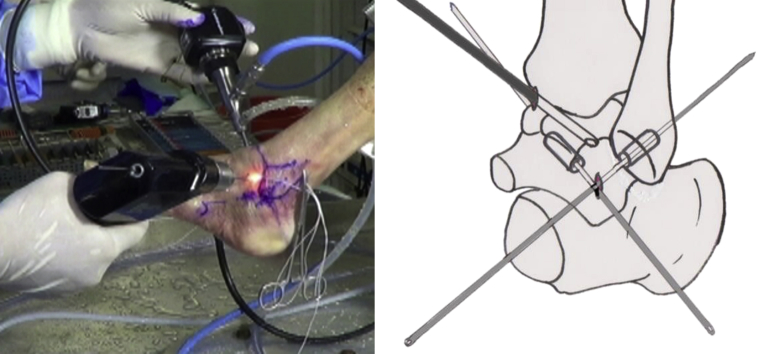
Talar Bone Tunnel
The talar bone tunnel is constructed to serve as the docking site for the talar stem of the anatomic Y-graft (Fig 4). The MML portal and anterolateral portal are again used as the viewing portal and working portal, respectively. A guidewire is inserted through the AAL portal to penetrate the talus through the talar insertion site of the ATFL and directed toward the distal end of the medial malleolus. Care is taken to pass the guide through the anterior-central body of the talus to prevent fracture or penetration of the anterior and superior surfaces of the talus. The guide pin is passed through the medial wall of the talus and then through the skin just anterior and slightly distal to the tip of the medial malleolus, with great care taken not to damage the tibial neurovascular bundle. Over-drilling is performed to a diameter of 6 mm and a depth of 20 mm.
Fig 4.
Construction of the talar bone tunnel to serve as the docking site for the talar stem of the anatomic Y-graft. The medial midline portal and anterolateral portal are used as the viewing portal and working portal, respectively. A guidewire is inserted through the accessory anterolateral portal to penetrate the talus through the talar insertion site of the anterior talofibular ligament and directed toward the distal end of the medial malleolus. Care is taken to pass the guide through the anterior-central body of the talus to prevent fracture or penetration of the anterior and superior surfaces of the talus.
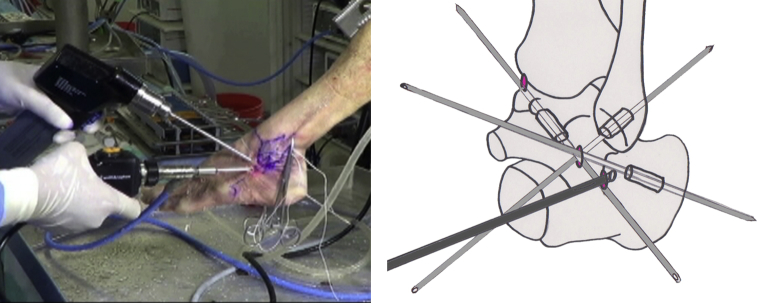
Calcaneal Bone Tunnel
The calcaneal bone tunnel is constructed to serve as the docking site for the calcaneal stem of the anatomic Y-graft (Fig 5). The arthroscope is inserted through the AAL portal, which is used as the viewing portal, whereas the ST portal is used as the working portal. A shaver is inserted through the ST portal to allow minimum debridement and allow visualization of the anterolateral border of the posterior facet of the ST joint. The anterior edge of the posterior facet is observed, and the tip of the arthroscope is moved posteriorly to find the CFL insertion site on the calcaneus, approximately 15 mm posterior to the anterior edge of the posterior facet and about 10 mm inferior to the joint line. A guidewire is used to penetrate the calcaneal insertion site of the CFL and directed toward the central posteromedial cortex of the calcaneus, with great care taken not to damage the tibial neurovascular bundle posterior to the medial malleolus. The guide pin is then over-drilled to a diameter of 6 mm and a depth of 30 mm.
Fig 5.
Construction of the calcaneal bone tunnel to serve as the docking site for the calcaneal stem of the anatomic Y-graft. The arthroscope is inserted through the accessory anterolateral portal, which is used as the viewing portal, whereas the subtalar (ST) portal is used as the working portal. A shaver is inserted through the ST portal to allow minimum debridement and allow visualization of the anterolateral border of the posterior facet of the ST joint. The anterior edge of the posterior facet is observed, and the tip of the arthroscope is moved posteriorly to find the calcaneofibular ligament insertion site on the calcaneus, approximately 15 mm posterior to the anterior edge of the posterior facet and about 10 mm inferior to the joint line.
Step 5: Delivery and Fixation of Anatomic Y-Graft to Bone Tunnels
All 3 stems of the anatomic Y-graft are delivered through the AAL portal using an inside-out technique (Fig 6). First, the sutures passing through the talar stem loop of the graft are attached to a guidewire, which is then passed through the talar tunnel. Similarly, the sutures passing through the fibular and calcaneal stem loops are attached to a guidewire and passed through their respective tunnels in sequence to pull the grafts through the ALL portal and into position. Each graft end is tensioned using the threads exiting the skin on the opposite side of each bone tunnel.
Fig 6.
All 3 stems of the anatomic Y-graft are delivered through the accessory anterolateral portal using an inside-out technique. First, the sutures passing through the talar stem loop of the graft are attached to a guidewire, which is then passed through the talar tunnel. Similarly, the sutures passing through the fibular and calcaneal stem loops are attached to a guidewire and passed through their respective tunnels in sequence to pull the grafts through the accessory anterolateral portal and into position.
The 3 anatomic Y-graft stems are inserted into their respective tunnels to a depth of at least 15 mm and fixed with interference screws (Fig 7). Each bony attachment of the tendon graft is fixed with a 6-mm-diameter interference screw (Smith & Nephew) while a 30-N tension force is applied. First, the fibular stem is fixed; then, the talar attachment is fixed while the ankle is in a neutral position with 0° of flexion. Finally, the calcaneal attachment is fixed in the same manner as the talar attachment. Once all 3 stems of the anatomic Y-graft are fixed, the sutures are removed, the portal sites are closed using nylon sutures, and the lower extremity is dressed and immobilized with a below-knee plaster of Paris cast.
Fig 7.
The 3 anatomic Y-graft stems are inserted into their respective tunnels to a depth of at least 15 mm and fixed with interference screws. Each bony attachment of the tendon graft is fixed with a 5-mm-diameter interference screw while a 30-N tension force is applied. First, the fibular stem is fixed; then, the talar attachment is fixed while the ankle is in a neutral position with 0° of flexion. Finally, the calcaneal attachment is fixed in the same manner as the talar attachment.
Step 6: Postoperative Care
The patient's operative limb is immobilized in a below-knee cast for a total of 6 weeks with weight bearing as tolerated.17 Wound inspection and portal suture removal occurs between 7 and 14 days postoperatively.
Discussion
Recently, there have been published descriptions of ankle arthroscopic stabilization procedures using repair techniques that have been shown to be safe and effective in the short-term.18 Guillo demonstrated a similar arthroscopic reconstruction stabilization procedure for lateral ankle instability at the 2014 annual meeting of the European Society of Sports Traumatology, Knee Surgery and Arthroscopy. Guillo et al.19, 20 described a novel arthroscopic reconstruction technique that uses lateral ankle endoscopy to provide a better view of the internal anatomy of the ankle. The aim of this technique is to use ankle endoscopy and arthroscopy to attain a more physiological reconstruction of the lateral complex of ligaments.
In this report we present our technique for anatomic ankle arthroscopic reconstruction of the lateral ligaments (anti-ROLL) performed in an all–inside-out manner that is likely safe for patients and minimally invasive. Recommended indications are shown in Table 1 and advantages and risks in Table 2.
Table 1.
Indications and Contraindications for Anatomic Ankle Arthroscopic Reconstruction of Lateral Ligaments
| Indications |
| Ankle instability with failed nonoperative treatment |
| Insufficient remnant ligament to allow repair technique |
| Previous failed arthroscopic ankle repair stabilization |
| Contraindications |
| Previous failed ankle reconstruction stabilization |
| Previous failed open repair or reconstruction technique |
| Active infection |
Table 2.
Advantages and Risks of Anatomic Ankle Arthroscopic Reconstruction of Lateral Ligaments
| Advantages |
| Minimally invasive |
| Decreased morbidity |
| Faster recovery |
| Decreased scarring |
| Risks |
| Nerve injury |
| Blood vessel injury |
| Tunnel fracture |
Footnotes
The European Society of Sports Traumatolgy, Knee Surgery and Arthroscopy Ankle and Foot ASsociates Ankle Instability Group (ESSKA AFAS AIG) comprises Thomas Bauer, James Calder, Nuno Corte-Real, Ali Ghorbani, Mark Glazebrook, Stéphane Guillo, Jon Karlsson, John G. Kennedy, Gino M.M.J. Kerkhoffs, Siu Wah Kong, Peter G. Mangone, Frederick Michels, Andy Molloy, Caio Nery, Christopher Pearce, Anthony Perera, Hélder Pereira, Bas Pinenburg, Fernando Raduan, James W. Stone, Masato Takao, Yves Tourné, Niek C. N. van Dijk, Jordi Vega, and Jin Woo Lee.
The authors report the following potential conflict of interest or source of funding: J.S. receives support from Smith & Nephew.
Supplementary Data
Anatomic ankle arthroscopic reconstruction of lateral ligaments (anti-ROLL) using all–inside-out technique for treatment of ankle instability in a cadaver. The patient is positioned in the supine position.
References
- 1.Karlsson J., Lansinger O. Chronic lateral instability of the ankle in athletes. Sports Med. 1993;16:355–365. doi: 10.2165/00007256-199316050-00006. [DOI] [PubMed] [Google Scholar]
- 2.Kerkhoffs G.M., Handoll H.H., de Bie R., Rowe B.H., Struijs P.A. Surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults. Cochrane Database Syst Rev. 2007:CD000380. doi: 10.1002/14651858.CD000380.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Bell S.J., Mologne T.S., Sitler D.F., Cox J.S. Twenty-six-year results after Broström procedure for chronic lateral ankle instability. Am J Sports Med. 2006;34:975–978. doi: 10.1177/0363546505282616. [DOI] [PubMed] [Google Scholar]
- 4.Broström L. Sprained ankles. VI. Surgical treatment of “chronic” ligament ruptures. Acta Chir Scand. 1966;132:551–565. [PubMed] [Google Scholar]
- 5.Krips R., van Dijk C.N., Halasi T. Anatomical reconstruction versus tenodesis for the treatment of chronic anterolateral instability of the ankle joint: A 2- to 10-year follow-up, multicenter study. Knee Surg Sports Traumatol Arthrosc. 2000;8:173–179. doi: 10.1007/s001670050210. [DOI] [PubMed] [Google Scholar]
- 6.Liu S.H., Baker C.L. Comparison of lateral ankle ligamentous reconstruction procedures. Am J Sports Med. 1994;22:313–317. doi: 10.1177/036354659402200303. [DOI] [PubMed] [Google Scholar]
- 7.Chrisman O.D., Snook G.A. Reconstruction of lateral ligament tears of the ankle. An experimental study and clinical evaluation of seven patients treated by a new modification of the Elmslie procedure. J Bone Joint Surg Am. 1969;51:904–912. [PubMed] [Google Scholar]
- 8.Coughlin M.J., Schenck R.C., Jr., Grebing B.R., Treme G. Comprehensive reconstruction of the lateral ankle for chronic instability using a free gracilis graft. Foot Ankle Int. 2004;25:231–241. doi: 10.1177/107110070402500407. [DOI] [PubMed] [Google Scholar]
- 9.Younes C., Fowles J.V., Fallaha M., Antoun R. Long-term results of surgical reconstruction for chronic lateral instability of the ankle: Comparison of Watson-Jones and Evans techniques. J Trauma. 1988;28:1330–1334. doi: 10.1097/00005373-198809000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Noyez J.F., Martens M.A. Secondary reconstruction of the lateral ligaments of the ankle by the Chrisman-Snook technique. Arch Orthop Trauma Surg. 1986;106:52–56. doi: 10.1007/BF00435653. [DOI] [PubMed] [Google Scholar]
- 11.Cass J.R., Morrey B.F., Katoh Y., Chao E.Y. Ankle instability: Comparison of primary repair and delayed reconstruction after long-term follow-up study. Clin Orthop Relat Res. 1985:110–117. [PubMed] [Google Scholar]
- 12.Snook G.A., Chrisman O.D., Wilson T.C. Long-term results of the Chrisman-Snook operation for reconstruction of the lateral ligaments of the ankle. J Bone Joint Surg Am. 1985;67:1–7. [PubMed] [Google Scholar]
- 13.Zenni E.J., Jr., Grefer M., Krieg J.K., Lambert M.B., Florez R. Lateral ligamentous instability of the ankle: A method of surgical reconstruction by a modified Watson-Jones technique. Am J Sports Med. 1977;5:78–83. doi: 10.1177/036354657700500205. [DOI] [PubMed] [Google Scholar]
- 14.Takao M., Oae K., Uchio Y., Ochi M., Yamamoto H. Anatomical reconstruction of the lateral ligaments of the ankle with a gracilis autograft: A new technique using an interference fit anchoring system. Am J Sports Med. 2005;33:814–823. doi: 10.1177/0363546504272688. [DOI] [PubMed] [Google Scholar]
- 15.Dowdy P.A., Watson B.V., Amendola A., Brown J.D. Noninvasive ankle distraction: Relationship between force, magnitude of distraction, and nerve conduction abnormalities. Arthroscopy. 1996;12:64–69. doi: 10.1016/s0749-8063(96)90221-2. [DOI] [PubMed] [Google Scholar]
- 16.Penn D., Willet T.L., Glazebrook M., Snow M., Stanish W.D. Is there significant variation in the material properties of four different allografts implanted for ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17:260–265. doi: 10.1007/s00167-008-0678-8. [DOI] [PubMed] [Google Scholar]
- 17.Haraguchi N., Armiger R.S., Myerson M.S., Campbell J.T., Chao E.Y. Prediction of three-dimensional contact stress and ligament tension in the ankle during stance determined from computational modeling. Foot Ankle Int. 2009;30:177–185. doi: 10.3113/FAI-2009-0177. [DOI] [PubMed] [Google Scholar]
- 18.Wang J., Hua Y., Chen S., Li H., Zhang J., Li Y. Arthroscopic repair of lateral ankle ligament complex by suture anchor. Arthroscopy. 2014;30:766–773. doi: 10.1016/j.arthro.2014.02.023. [DOI] [PubMed] [Google Scholar]
- 19.Guillo S., Archbold P., Perera A., Bauer T., Sonnery-Cottet B. Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc Tech. 2014;3:e593–e598. doi: 10.1016/j.eats.2014.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guillo S., Cordier G., Sonnery-Cottet B., Bauer T. Anatomical reconstruction of the anterior talofibular and calcaneofibular ligaments with an all-arthroscopic surgical technique. Orthop Traumatol Surg Res. 2014;100(suppl):S413–S417. doi: 10.1016/j.otsr.2014.09.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Anatomic ankle arthroscopic reconstruction of lateral ligaments (anti-ROLL) using all–inside-out technique for treatment of ankle instability in a cadaver. The patient is positioned in the supine position.