Abstract
Introduction:
Infected nonunion of radius and ulna are rare but difficult problems to deal. We report a case of successfully managed infected non-unonion of forearm bones and the reasoning behind strategy of approach to the case.
Case Report:
42 year old female presented with history of closed forearm fracture three months back for which she was operated with open reduction and internal fixation using dynamic compression plate. There was pain and fever post-surgery and discharge and wound gape. This was treated with resuturing of the wound and oral antibiotics. She continued to have pain fever and discharge and consulted another surgeon who removed first the radius plate and then the ulna plate sequentially with stabilisation by external fixation. She presented to us at three months post injury with infected nonunion of radius and ulna with loosening of fixators, sequestrum on radiograph and wristdrop. A staged treatment was planned for her. As first stage debridement, antibiotic Calcium Sulphate cement bead insertion and intramedullary flexible nail fixation. She was given iv antibiotics as per culture report. At 3 months post surgery the infection had settled and pellets were resorbed. Double barrel vascularized fibula graft was used to fill the gap and fixation using long locked plates was done. At one year follow up radiographs showed good healing and clinically patient had a good elbow movements and was able to carry out her daily activities.
Conclusions:
Proper planning and staged management of such cases helps to achieve goals with good functional outcome.
Keywords: Infected nonunion, radius, ulna, vascular fibula graft
What to Learn from this Article?
Clinical Decision Making (CDM), Planning and Managing cases of Infected Non union of Radius & Ulna? Technical Tips and Pearls of Surgical management in such cases. How to prevent such case?
Theoretical Background
Infected nonunions are complications that are rare but have tremendous impact both on the patient and on the surgeon’s skills. Infected nonunions of forearm bones are rarely encountered with very few reports in literature [1-5]. These are seen especially after treatment of neglected cases or cases with history of smoking, alcoholism or other co- morbidities [5]. Management options include staged debridements and internal fixation after control of infection or single staged debridement and external fixator [5]. Although cases are reported individually, and as part of larger series, a definite guideline is difficult to establish. A recent case series of 15 such cases reported a protocol of aggressive debridement, early definitive fixation within 7-14 days with good results [5]. All cases of infected nonunion have unique and different presentation and require a customized approach. This case study recounts our strategy to treat one such case.
Case Introduction Forty two year old house wife had a fall and sustained a closed radius ulna fracture. Open reduction and internal fixation was done at a different surgical center. She developed infection for which repeated debridement and implant removal was done. Bones were stabilized with external fixator however the infection was still not controlled. She came to us with infected non unions of both bones of forearm and external fixator in place.
Case History
Patient complained of fall and sustained a closed fracture on February 2011. She went to a surgical center close to her house and was operated on the same day with open reduction and internal fixation using dynamic compression plates (Fig 1). On the second day after surgery, she developed a high fever. Blood counts were asked and a WBC count of 13500 was noted. The antibiotic was changed and presumably, a higher antibiotic was administered. This settled the fever, however wound gape was noted and there was discharge from the radial wound. This was secondarily sutured on the 5th day and she was sent home. However, the patient continued to be ‘ill’ and had pain and swelling in the operated limb, and decided to take a second opinion. The second surgeon debrided the radial wound, removed the radial plate and applied an external fixator on the radius (Fig. 2). The ulnar incision was not opened and ulnar plate was retained. She was administered oral antibiotics. She continued to be troubled by discharge from the radial incision and after 3 weeks the ulnar incision began discharging seropurulent fluid. The ulnar wound was debrided and plate was removed. An external fixator was applied to ulna in addition to the radial fixator (Fig. 3). Patient continued to have discharge from the wound and radiographic picture worsened (Fig. 4). Patient was advised to get a CT- bone scan done. At this point the patient presented to us with discharging wounds and pain with external fixators in situ.
Figure 1.

Immediate Postoperative radiograph showing radius ulna fractures stablised by DCP plate.
Figure 2.

Radial plate removed and Fixator applied at 3 weeks post primary surgery. Note the short fixator length well within the DCP plate length. Also long fixator pins traversing the interosseous space
Figure 3.
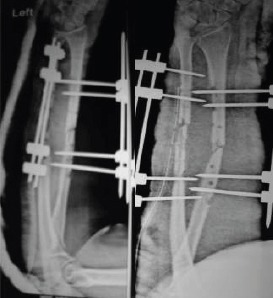
Ulnar plate removed and fixator application. Again note the small length of fixator and long fixator pins.
Figure 4.

Intermediate radiograph showing worsening of pin sites with Radius sequestrating
Case Assessment
The general condition of the patient was fair, she had been having fever on and off with pain and discharge from both the radial and ulnar wounds (Fig. 5). Wounds were dressed daily and oral medication [antibiotics and anti- inflammatory] were being administered. Surgical scars over radius and ulna showed sinuses with granulation tissue [as seen in Fig. 5] and had discharge on pressing the edges. There was no wide gape and no fulminant signs of infection. There was loosening and discharge from the radius pin tracts. Sequential radiographs were available with first radiograph showing fixation of the radius and ulna done using DCP plates. The second radiograph with radius plate removed by the second surgeon and external fixator applied. The third radiograph showed removal of ulna plate and application of external fixation. Radiograph at presentation showed that the middle of the radius had sequestered out, with similar changes in ulna (Fig. 6).
Figure 5.

Clinical Appearance and pin sites at presentation. Note the ‘wrist drop’
Figure 6.

Radiograph at presentation showing infected nonunion of radius and ulna and possible sequestration os large radius and ulna fragments
Case Conceptualization & Management Options
Problems of the Case: On presentation the patient had already undergone four surgeries [primary surgery, wound gape resuturing, radial plate removal and ulna plate removal]. Since these surgeries were not done at our center we were not sure about the extent of debridement. The reason for continued infection may be inadequate debridement or a resistant organism. Culture done at the previous center had grown Kleibsiella Pneumoniae and appropriate antibiotics were administered so possibly the debridement was an issue.
Problems to the patient: The patient was really anxious. She was an earning member of her family and since last three months she had been incapacitated. Her expectations were not met and she was very unsure of the future. We explained her the positive and negative aspects of the current situation and the further treatment plan. She was difficult to convince and seemed to have lost a lot of faith.
Problems to surgeon: We were looking at a case with active infection, secondary to inadequate debridement with radiological sequestrum in both radius and ulna. In current scenario there were three goals to achieve; clearance of infection, bony union, and facilitate maximum possible functional restoration.
Plan was laid down according to our goals above 1. Clearance of infection: The radiograph showed sequestrated fragments in radius and ulna. A PET-CT was done to delineate the extent of sequestrum which showed involvement along the entire length between the pin tracts of the fixator. A large abscess was also noted. A preoperative culture was send which grew staphylococcus aureus sensitive to vancomycin. Plan was to debride the wound, remove the fixator, sequestrectomy and antibiotic cement beads insertion was made. The second issue to be considered at this time was mode of bone gap stabilization after excision of sequestrum. Patient was averse to external fixator and we considered internal fixation as our primary option. All options of internal and external fixator were made available during surgery. We had personally planned for internal fixation using a flexible nail with added stabilization with external fixator (if required).
2. Achieving union: After infection has settled achieving union was the next step. There are two main options here bone transport or bone graft. Bone transport in radius ulna is technically difficult and very less work is available on this. Bone transport can have following disadvantages (a) in forearm fixation of radius will lead to transfixation of the muscles. The patient already has a wrist drop which is due to muscle fibrosis and transfixation and bone transport will worsen it (b) bone transport will lead to movement of origin of the muscles leading to clawing and other complications (c) application of fixator can functionally limit the patient for long time in cases with long gaps [as in this case]. Vascular or non vascular bone grafting can be used successfully and we had experience in using vascularized fibula graft for tibial gap nonunion and thus this modality was chosen by us. In this case the soft tissues is scarred and are less vascular, addition of new vascular graft will be more favorable in attaining successful graft incorporation.
Treatment Given
In May 2011, debridement, cement bead insertion and intramedullary flexible nailing were done. The debridement and excision of all dead bone was done till bleeding bone was found. How to stabilize a large defect was a decision to be finalized intraoperatively, however both intramedullary, extramedullary and external fixation options were kept ready. Once the necrotic bone, granulation etc was removed (Fig. 7), we decided to use Titanium elastic nails (TENS nail), along with external support by a plaster slab. We wished to use a Vacuum assisted Closure (VAC) in the postoperative period and a fixator would have made it difficult to apply the VAC (although VAC was not used, it is a point to be considered in decision making). TENS nails can provide surprisingly good rotational fixation and can maintain the gap in forearms. Technical tips are to use a ‘single pass method’ which means to avoid repeated insertion and multiple tract formation which makes the implant loose later. If the curved end is anchored to the subchondral bone, good stability can be achieved. This gives rotational stability and also resistance against collapse. We filled in the empty space with 20 Gms of Stimulan (Calcium sulphate) loaded with 2 Gms vancomycin and 3 million units Colistin (based on the earlier culture reports) (Fig 8). Multiple tissue samples were taken, from multiple areas in the wound, for culture (which would guide the post operative IV antibiotics). The deep culture grew paesudomonas aerugenosa sensitive to colistin and Carbapenams. Since colistin was already put into cement, IV Imepenum was given for 3weeks. Postoperatively, the forearm quite clearly ‘calmed down’ with decrease pain, redness, swelling and discharge (Fig 9a). Regular dressings showed consistent improvements, and blood parameters improved gradually (Fig 9b). Deep culture grew Pseudomonas aerugenosa, which was sensitive only to Carbapenams and Colistin. Since Colistin was already added to the cement pellets, antibiotic depot IV Imipenam was given for 3 weeks. Use of IV antibiotics can be regulated based on a combination of clinical appearance and response, and blood parameters - notably CRP. Based on these, we stopped IV antibiotics after 3 weeks, despite the CRP not being normal, but it was showing a clear downward trend and the patient was comfortable. No further antibiotics were administered to her after this.
Figure 7.
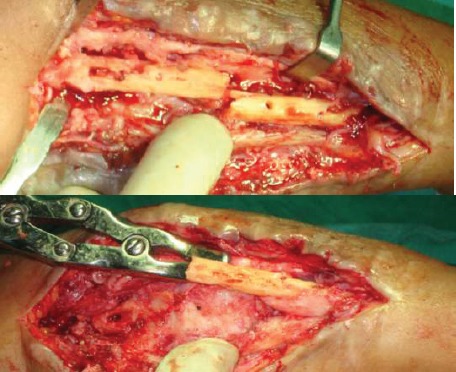
Central diaphysis of the Radius and Ulna sequestrated
Figure 8.

Bone gap stabiised by TENS nail. Stimulan Pellets for local Antibiotic Delivery Wound closure
Figure 9.

Healing of the wound
Intermittent period and second surgery: Over the next few months, a regular watch was kept on her, clinically as well as by radiographs. The TENS nails did their job of stabilization well, and radiographs showed gradual disappearance of the pellets (as expected) (Fig. 10). We had discussed with the patient, and suggested that a vascular fibula was a good option for her to shorten the recovery and maintain function (in contrast to bone transport, which would have been the other option). With help of plastic surgeons a double barreled vascular fibula was harvested and grafted in the gap of both radius and ulna (Fig. 11). Fixation was done using a long titanium plates that covered the bones almost completely (Fig. 11b,c). For about 6 weeks she was protected in a slab, with intermittent mobilization out of the slab, and gradual weaning off of the external support after that. Rehabilitation protocol was aimed at restoring maximal elbow and wrist movements at first stage and prono- supination at second stage.
Figure 10.

Biodegradable CaSo4 Pellets disappear over time 2 to three months post surgery. TENS nail held the position well
Fig 11a.

Vascularized Fibula with Pedicle converted to double barrel was used to fill the gap. Plate fixation through single incision to stablise both radius and ulna. b: Vascularized Fibula with Skin paddle and final closure
Fig 11c.
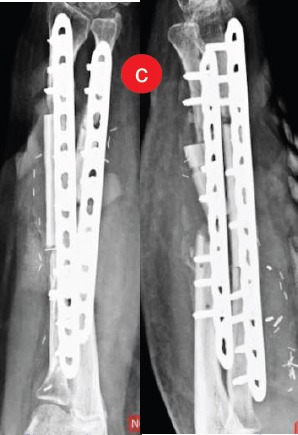
Immediate post-operative radiograph
Follow up: At 1 year after that surgery, she is back to an active life, happy, fairly good function from a medical standpoint, but “able to do everything that she needs to do” and the radiographs show a solid union at all the four sites, without any additional procedures being required (Fig 12a,b). [Watch for the patients smile at follow up, such untold outcome measures are one that are most relevant in clinical practice]
Figure 12a.

Excellent Function, except for pronation beyond midprone at one year follow up
Fig 12b.

Radiograph showing good healing at one year follow up
Implications of the case
How to prevent such cases?
Theater asepsis is a must and continuous review of the sterilization process in your operation theaters is most essential. Cases of infected nonunion in forearm are rare due to good vasculature, however even if one case is infected it is 100% disaster for that case. Be vigilant about the asepsis during surgery and of course handling the soft tissue, achieving stable fixations are other basic principles that need to be kept in mind.
How should the patient have been treated?
Stage 1: Post-operative fever and discharge
There is no role for antibiotics only and no role for wait and watch. Do not wait for infection to settle, take it head on. Also if there are two incisions in the same limb as in this case and one incision is showing signs of infection the others incision should also be considered to be infected and treated like wise. If the wound is showing all signs of infection it has to be opened up and debrided and washed. I personally use dilute betadine solution for lavage and use about 3 to 4 liters of this solution [6]. The decision on implant removal has to be taken intraoperatively after debridement and wash. Early in the course of infection the implant can be retained if the soft tissues look healthy after debridement. If there is lot of granulation tissue which is covering the plates [underside or screw holes] the plate needs to be removed.
Stage 2: With radius plate removed and fixator applied and continued infection
At this stage there were two errors made, first debridement of only one incision and unstable external fixation. As mentioned above, unless obvious the second incision has to be taken as infected and at least warrants opening and lavage. Secondly the fixator length chosen was short. The fixators should have at least extended beyond the screw holes and should be of more stable construct [like a delta frame]. Instability combined with inadequate debridement would have led to continued infection. One of the other mistakes that one can see is the incision size. The debridement incision was not extending beyond the original incision. The debridements should always be through extended incision on both sides and thorough exploration. For a successful debridement the ‘Enough’ rule can be followed with enough time, enough incision, enough exposure for thorough and complete debridement. For debridements always err towards excess. With infection in mind local antibiotic pellets are to be considered with very low threshold. One of the issues with antibiotic cement (PMMA) beads is that they require second surgery for removal. For this reason we use calcium sulphate pellets. These are self-absorbing and do not require a second surgery. The other advantage of calcium sulphatepellets over PMMA beads is the ability to use any antibiotic according to culture instead of only thermo-stable antibiotic for beads. We always use the antibiotic pellets in all our cases of debridement for infected bony injuries. We recommend antibiotic beads as there is a limit to soft tissue excision and residual infected material can flare the infection and also these pellets fill up the dead space, not allowing for large collections post-surgery.
This particular patient really underlines the importance of recognition of the destructiveness of infection, need for experience to deal with it aggressively, the requirement of the surgeon to deal with the surgery, the pharmacology and the psychology of infection and need to use the best knowledge, techniques, and tools/implants available to achieve an optimal result.
Recommendations to Surgeons and Students
1. Stage the surgeries: Plan and stage your surgeries in such cases. Go for stage wise goals and keep the patient informed
2. Assess your infrastructure: Primarily the OT complex, need for specialized care like vascularized bone graft and plastic surgeons. If need be do not hesitate to refer the patient
3. If war cannot be won at one time, look to win the battles individually. Eradicate the infection first which is one battle won and then plan for reconstruction and later plan for functional improvement. Stage your treatment
4. Send for Opinions: one of the most important points is to seek as many opinions possible on such cases. Approach seniors and discuss cases.
5. Use such cases to audit your techniques of debridement. For example, after debridement the wound should start settling by the end of one week, it should reduce in redness, discharge and swelling. If there is no change for 4 to 5 weeks that means the debridement has failed and you should review your debridement process and introspect on what was inadequate
6. Use local antibiotic delivery: have a low threshold to use beads. Calcium sulphate is most advantageous without problem of conventional beads
7. Believe the worse radiograph, follow the enough rule and err towards excess in such cases.
Acknowledgment
Authors will like to acknowledge Dr Sameer Kumta for performing the double barrel fibula graft in this case and also for providing the related photographs
Biography

Footnotes
Conflict of Interest: Nil
Source of Support: None
References
- 1.Hurst LC, Mirz MA, Spellman W. Vascular fibular graft for infected loss of the ulna: case report. J Hand Surg. 1982;7:498–501. doi: 10.1016/s0363-5023(82)80047-6. [DOI] [PubMed] [Google Scholar]
- 2.Meals RA. The use of flexor carpi ulnaris muscle flap in the treatment of an infected nonunion of the proximal ulna:a case report. Clin Orthop. 1989;240:68–72. [PubMed] [Google Scholar]
- 3.Malki A, Wong-Chung J, Hariharan V. Centralization of ulna for infected nonunion of the radius with extensive bone loss. A modified Hey-Groves procedure. Injury. 2000;31:345–349. doi: 10.1016/s0020-1383(99)00307-1. [DOI] [PubMed] [Google Scholar]
- 4.Dell PC, Sheppard JE. Vascularized bone grafts in the treatment of infected forearm nonunions. J Hand Surg. 1984;9:653–658. doi: 10.1016/s0363-5023(84)80006-4. [DOI] [PubMed] [Google Scholar]
- 5.Prasarn ML, Ouellette EA, Miller DR. Infected nonunions of diaphyseal fractures of the forearm. Arch Orthop Trauma Surg. 2010 Jul;130(7):867–73. doi: 10.1007/s00402-009-1016-4. [DOI] [PubMed] [Google Scholar]
- 6.Brown NM, Cipriano CA, Moric M, Della Valle CJ. Presented at the 2011 Annual Meeting of the American Academy of Orthopaedic Surgeons. San Diego: Feb 15-19, Dilute betadine lavage prior to closure for preventing acute deep periprosthetic joint infection Paper #128. [Google Scholar]


