Abstract
Introduction:
Neglected cases of osteomyelitis are not uncommon. We present a case of humerus osteomyelitis neglected for 10 years and presented with a sequestrum protruding out of the arm in the shape of a flowerpot. Such a long duration of neglect and a startling presentation are rare and have implications not only on healthcare but also reflect the socio-economic and cultural fabric of the society.
Case Report:
22 year old lady presented with history of bone jutting out of right arm since last 10 years. She had a trivial injury to the arm 10 years back followed by pain and fever. She was treated by local osteopath and ‘registered’ doctors but developed wound over the arm with purulent discharge. On and off treatment with dressing was continued with symptomatic relief but in few weeks bone fragment started protruding out of the wound. The size of bone protruding from the wound increased gradually with on and off history of discharge since 10 years. Clinically a flowerpot shaped sequestrum was seen protruding from the arm. Radiographs showed a defined diaphyseal sequestrum of the humerus with continuity of the bone maintained by new bone formation. Sequestrectomy was done and at one year follow up patient was fine with no recurrence of infection
Conclusions:
Lack of health infrastructure, ignorance, and other social and cultural factors lead to such bad wounds. Even with such long history a single surgery for debridement and sequestrectomy was all that was needed for healing the patient.
Keywords: flowerpot sequestrum, osteomyelitis, sequestrectomy
What to Learn from this Article?
Neglected Chronic osteomyelitis - Medical and social perspective Surgical Management of such complicated cases - Clinical decision making
Introduction
Extensive diaphyseal sequestrations are not unknown. They generally follow hematogeneous osteomyelitis and are mostly seen in children [1,2]. We present a startling case of 10 year long neglect of such extensive diaphyseal osteomyelitis leading to formation of a ‘Flowerpot’ sequestrum.
Case History
A 22 year old lady presented to our OPD with complains of ‘bone jutting out of arm’. The complaint was such that a preliminary clinical examination was done before further history taking. A flowerpot shaped dead bone (sequestrum) was seen protruding from the middle of the right arm (Fig. 1a,b). Large irregular scars of old sinuses, healed with secondary intension marked the entire lateral side of the arm above and below the sequestrum. The elbow was fused in almost 80° of flexion and in midprone position. Shoulder movements were restricted. There was no active discharge from the wound. There was no neurovascular problem in the affected limb. On inquiry she gave history of trivial injury to right arm at age of 12 years. This was followed by pain swelling and fever. She was given ‘massage’ by local osteopath and was also given medications by local medical practitioner. There was some symptomatic relief, but within a week a wound appeared over the lateral aspect of the arm with purulent discharge with pain and swelling at the elbow. Dressing was done and oral medications were given, however wound continued to discharge. Gradually bony fragments started to protrude from the wound and increased stiffness at the elbow. There was neglect from patient’s family due to financial and (possibly cultural) reasons and treatment was taken on and off. The protruding bone increased in size over period of years and the girl used to continuously cover it with her ‘dupatta’ (scarf). The wound had intermittent discharge alternating with dry period and the elbow was completely stiff. She was now of marrying age and probably for this reason treatment was suggested by relatives. Radiographs revealed a large diaphyseal sequestrum extending from outside protrusion till distal humerus (Fig 2a,b). The humerus shaft was deformed but had no discontinuity due to the formation of extensive involucrum. Bony ankylosis of the elbow was noted. On blood examination she was anaemic while rest parameters like ESR and CRP and blood counts were normal. She was given blood transfusion before surgery. Since there was no active discharge in last 6 months and wound was dry, preoperative microbial culture was not done. Sequestrectomy through lateral approach taking the wound area into the incision was performed. Total diaphyseal sequestrectomy was done by curetting the margins of sequestrum and gentle rotatory movements. 21 cms long sequestrum was removed in totality [8 cms was out of the skin] (Fig. 3). The margins of the marrow cavity and involucrum were thoroughly curetted and all dead bone was removed. Debridement of the surrounding unhealthy soft tissue was also done. Thorough wash of the wound was done with primary closure of the wound. Sample taken from the deep wound grew Staphylococcus Aureus and appropriate antibiotics were given for 3 months, parentral for 1st 10 days and then oral. Oral antibiotics were changed every15 days. Wound check was done on day 5 and then every 15 days for three months, though the wound healed completely in 2 months. At one year follow up, the wound is healthy with no recurrence of infection. Radiologically there are no signs of infective activity (Fig 4a). Functionally the elbow is in 80° of flexion and in midprone position [good functional position] (Fig 4b) and she is able to carry out most of her daily activities independently.
Figure 1a,b.

Clinical appearance of ‘Flowerpot’ sequestrum from the humerus. Elbow is fixed in 80 degree of flexion
Figure 2a,b.

Radiographs showing huge diaphyseal sequestration with good new bone formed. Note the bony ankylosis of the elbow
Figure 3.
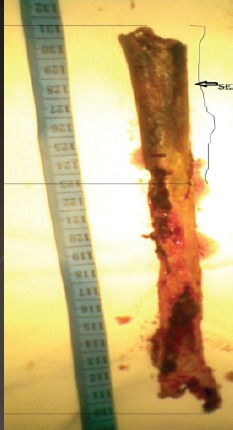
21 cms of sequestrum excised in totality
Figure 4.

a- One year post surgery radiograph showing good continuity of the bone with no signs of active infection. b-clinical picture showing good wound healing
Discussion
Extensive diaphyseal osteomyelitis can lead to sequestration of large segments of bones [3,4]. Most of these cases are of delayed presentation but still present to proper healthcare system within 1 or 2 months. Our case presented 10 years after the primary episode. This is not only a failure of healthcare system but also stands testimony to social and cultural aspects of our society in general. Females in Punjab are still looked down upon as compared to their male counterparts and this could be one of the main reasons for not taking the girl child to some qualified doctor for the treatment.
Since the patient was from a small village, a proper healthcare system was not available. Again financial situation of the parents was a factor for delay in treatment. Treatment by local osteopath and quacks is another factor that can contribute to mismanagement of such cases. Anemia, malnutrition, frequent bacteremia due to poor hygiene, also contributes to such lesions. [5] However, a delay of 10 years cannot be explained by any one of these factors. The very fact, that the girl was living with a dead bone protruding out of her arm for 10 years, raises lot of unanswered questions.
As far as management of such cases is concerned, it is pretty straightforward based on principles of treatment of chronic osteomyelitis [6]. Since the infection was quiescent for more than 6 months prior to presentation, we planned a single stage surgery [7]. Thorough debridement and complete removal of sequestrum are necessary. Intraoperative, there was no active infection so extensive bony debridement was not needed. The continuity of humerus was maintained and strong new bone was already present so no bone grafting was done. The treatment as such was quite simple and should have been available at any primary health care centre [or at least a referral can be arranged]. Bony ankylosis of elbow was not disturbed as it was in good functional position.
Conclusion
In conclusion we report a case of delayed management of humerus osteomyelitis which raises a question on the social, and healthcare system of the country. The treatment was simple with good results even after the infection had ‘coexisted’ in the arm for about 10 years.
Clinical Message.
A lot is left to be desired in terms of delivery of healthcare in our country and to improve the psyche of the society in favor of the female children. Such chronic osteomyelitis cases come along rarely, but can be treated by simply following the principles of sequestrectomy, thorough debridement and antibiotic treatment.
Biography

Footnotes
Conflict of Interest: Nil
Source of Support: None
References
- 1.Agus H, Kalenderer O, Ozcalabi IT, Arslantas M. Treatment of infected defect pseudoarthrosis of the tibia by in situ fibular transfer in children. Injury. 2005 Dec;36(12):1476–9. doi: 10.1016/j.injury.2005.06.040. [DOI] [PubMed] [Google Scholar]
- 2.Daoud A, Saighi-Bouaouina A. Treatment of sequestra, pseudoarthroses, and defects in the long bones of children who have chronic hematogenous osteomyelitis. J Bone Joint Surg. 1989;71A:1448–68. [PubMed] [Google Scholar]
- 3.Agiza AR. Treatment of tibial osteomyelitic defects and infected pseudarthroses by the Huntington fibular transference operation. J Bone Joint Surg Am. 1981 Jun;63(5):814–9. [PubMed] [Google Scholar]
- 4.Jain AK, Sharma DK, Kumar S, Sethi A, Arora A, Tuli SM. Incorporation of diaphyseal sequestra in chronic haematogenous osteomyelitis. Int Orthop. 1995;19(4):238–41. doi: 10.1007/BF00185230. [DOI] [PubMed] [Google Scholar]
- 5.Jones HW, Beckles VL, Akinola B, Stevenson AJ, Harrison WJ. Chronic haematogenous osteomyelitis in children:an unsolved problem. J Bone Joint Surg Br. 2011 Aug;93(8):1005–10. doi: 10.1302/0301-620X.93B8.25951. [DOI] [PubMed] [Google Scholar]
- 6.Spiegel DA, Penny JN. Chronic osteomyelitis in children. Techniques in Orthopaedics. 2005;20:142–152. [Google Scholar]
- 7.Beckles VL, Jones HW, Harrison WJ. Chronic haematogenous osteomyelitis in children:a retrospective review of 167patients in Malawi. J Bone Joint Surg Br. 2010 Aug;92(8):1138–43. doi: 10.1302/0301-620X.92B8.23413. [DOI] [PubMed] [Google Scholar]


