Abstract
Introduction:
Mucormycosis is life threatening infection rarely affecting musculoskeletal system and spinal involvement is extremely rare with only two cases reported in English literature.
Case Report:
We present this rare case of spondylodiscitis with lumbar vertebral osteomyelitis due to mucormycosis in a patient with chronic kidney disease on haemodialysis diagnosed by CT guided biopsy and highlight its clinico –radiological presentation and management principles.
Conclusion:
Thus, as the incidence of Mucorales infection increase due to increase in patients with predisposing factors, the unusual sites of affection increase. Treating clinician should have a high vigilance in patients with predisposing factors. Although there is dramatic improvement in the treatment modalities of mucormycosis, still the mortality is high. Early diagnosis is important to prevent dissemination and timely intervention in order to reduce morbidity and mortality. A well equipped multidisciplinary approach for clinico-radiological assessment and management is necessary.
Keywords: Isolated, spine, Mucor my costs
Introduction
Mucormycosis is a rare life –threatening opportunistic infection belonging to phylum zygomycosis. The name mucormycosis was used by R.D. Baker to designate mycosis caused by members of order mucorales [1].
Anatomically the site of invasive mucormycosis has been classified in six categories including rhinocerebral (most common), pulmonary, cutaneous, gastrointestinal, disseminated and uncommon rare forms such as osteomyelitis, peritonitis, endocarditis and renal infection [2]. Osteomyelitis due to mucormycosis have been described in tibia, femur, humerus, scapula, metacarpals, phalanges, sternum, cuboid, calcaneum, following tibial pin placement and anterior cruciate ligament repair[3]. Spinal involvement in mucormycosis is rare and only two cases have been reported till now in English literature[4,5].
Mucormycosis infection is most commonly seen in immuno compromised state with risk factors being uncontrolled diabetes mellitus in ketoacidosis, corticosteroids, trauma, burns, malignant hematologic disorder, organ transplantation, neonatal prematurity and malnourishment, illicit intravenous drug abuse, patients on hemodialysis and deferoxamine therapy(6).
We present this rare case of spondylodiscitis with lumbar vertebral osteomyelitis due to mucormycosis in a patient with chronic kidney disease on haemodialysis diagnosed by CT guided biopsy and highlight its clinico –radiological presentation and management principles.
Case report
A 64 year old man presented with chronic low back pain which was continuous and dull aching without any radicular symptoms or diurnal variations accompanied with low grade fever and weight loss (about 14 kg) since 3 months. Patient was a known case of diabetes mellitus, hypertension and chronic kidney disease on maintenance haemodialysis twice a week.
On examination, Patient was febrile and pale. Systemic examination was normal. On local examination, there was tenderness over lower lumbar vertebrae and the movements of lumbar spine were terminally restricted due to pain. Patient’s sensory and motor examinations were normal.
Patient already had recent radiological investigations done by previous treating surgeon, so we didn’t perform fresh investigations. Radiograph of lumbo- sacral spine (figure 1) showed slightly decreased density at L4-5 level and spondylolisthesis L5-S1 level with normal disc space appearance. Magnetic resonance imaging of lower lumbar spine (non contrast) showed hypointense signal involving L4 and L5 vertebrae with anterolisthesis of L5 over S1 vertebrae (Figure 2a, 2b).
Figure 1.
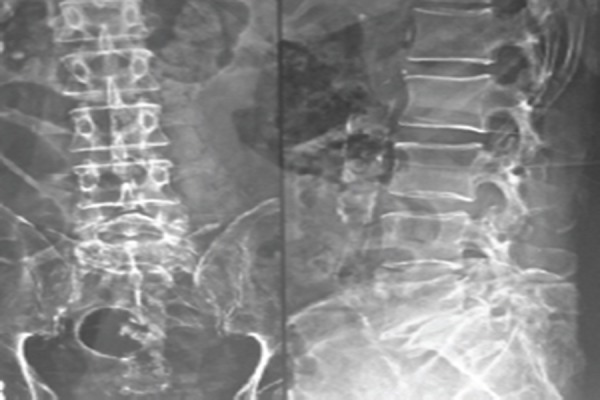
anteroposterior and lateral view of lumbo sacral spine
Figure 2a.
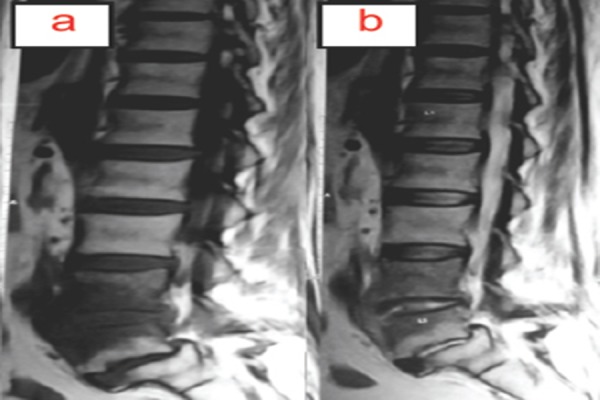
T1w Images showing hypointense signal involving L4 and L5 verteebae with anterolisthesis of L5 over S1 vertebrae. 2b precontrast T2w Images showing hypointense signal involving L4 and L5 vertebrae
Contrast MRI showed images demonstrating abnormal enhancement of L4 and L5 vertebrae without significant discal enhancement. Also enhancing soft tissue is noted anterior to L4-L5 disc. (Figure 3a, 3b, 4a, 4b)
Figure 3a & b.
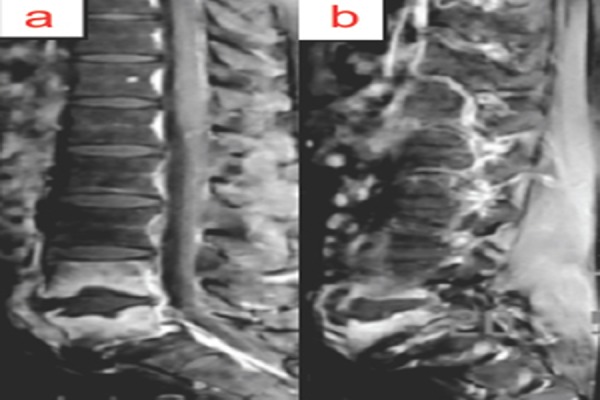
sagittal T1w images demonstrating abnormal enhancement of L4 and L5 vertebrae without significant discal enhancement. Also enhancing soft tissue is noted anterior to L4-L5 disc.
Figure 4a & b.
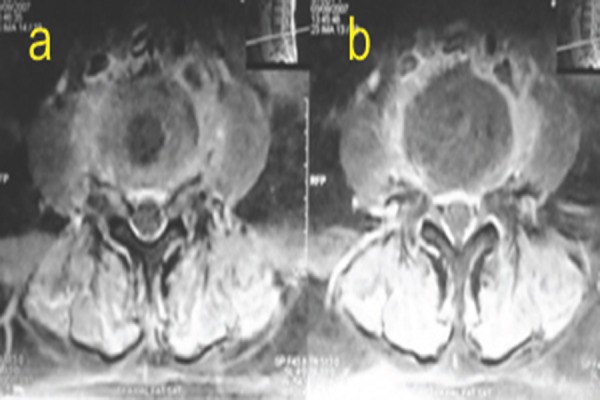
axial T1w images demonstrating abnormal enhancement of L4 and L5 vertebrae without significant discal enhancement. Also enhancing soft tissue is noted anterior to L4-L5 discand in epidural region
Imaging features were more in favour of infective pathology. We then performed laboratory investigations which revealed infectious etiology with deranged renal function. Haemoglobin- 8g/dl, Erythrocyte sedimentation rate -120mm/h, C-reactive protein- 10, Total leucocyte count -15,000 with lymphocytosis, Random blood sugar -/dl, Serum Creatinine- 5g/dl and Blood urea nitrogen-120 mg/dl.
With keeping infectious etiology in mind CT guided biopsy was performed under sedation.
Post biopsy patient was advised bed rest, mild analgesics and supportive medical line of treatment. Histopathology of the biopsy material showed classical phylle of mucor in haematoxylin and eosin stain. Infiltration by acute inflammatory cells like polymorphs and eosinophils were also seen. This confirmed fungus mucor on microscopy. (Figure 5a and 5b). No other procedure was performed on the patient.
Figure 5a & b.
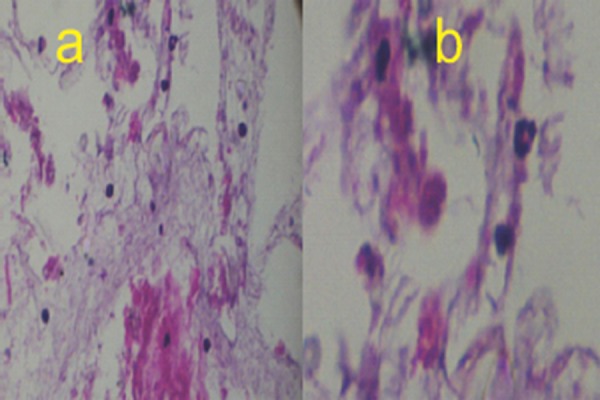
haemotoxylinand eosin stain showing mucor organism
5Amagnification 100x
5B magnification 400x
The prognosis of disease was explained in details to the patient and relatives. In view of the multiple comorbidities of the patient, conservative line of management was chosen. He was initated on Lipid formulation amphotericin B (LFAB). Renal function tests and leucocyte counts were monitored.
Symptomatically the patient initially improved and the leucocyte counts decreased. Maintenance dialysis was carried out twice a week. But in the third week the general condition started deteriorating requiring vasopressors due to septicemic shock. He progressed into septicemia and multiorgan failure and eventually succumbed after one week of aggressive medical management.
Discussion
The most common portal of entry of mucor organism is by inhalation of spores in air. Also it can enter the body via breach in mucosa of the skin or ingestion (7). Musculoskeletal mucormycosis is caused by breach in the skin due to trauma or direct inoculation. Hematogenous spread causing osteomyelitis is extremely rare (7). Spinal involvement has been described in only two cases in English literature. The case described by Buruma et al had cervical spine involvement with tetraplegia and previous medical history of laryngectomy with partial hypopharyngectomy and radiotherapy, eventually patient died because of pulmonary embolus and diagnosis was made on post-mortem specimen(5). In case described by Chen et al, lumbar puncture was proposed to be the mechanism of introduction of fungi (4). In our case, the patient was immuno compromised but there was no history suggestive of inoculation of organism or systemic involvement of mucormycosis.
Clinical features of mucormycosis depend on the site of involvement. The hallmark of condition is angioinvasion and localized destruction of tissues (7). Musculoskeletal symptoms are often neglected due to other co morbidities. Spinal involvement as seen in case of Buruma et al and Chen et al presented as localized pain and constitutional symptoms with associated numbness and weakness (4, 5). Our case also had similar clinical presentation. Majority of cases of mucormycosis presents in disseminated form because of angioinvasive nature of disease. Isolated lesions are rarely described with few cases reported in kidney, bone, heart, lung, brain, and gastro-intestinal tract (8, 9, 10). Our case presented as isolated lesion with no other organs involved except spine.
On plain radiograph, spinal mucormycosis presents as hypodensity in involved vertebra (4). MRI scanning (non contrast)reveals a low intensity on Tl-weighted and patches of high intensity on T2-weighted images (4). Our case showed hypodensity in plain radiograph and hypointense signal in T1 and T2 images in noncontrast MRI. We also present findings of contrast MRI, which shows hyperintense signal in vertebral body without abnormal signal in disc space.
Clinical features and radiographic manifestations are non specific and histopathology gives the definitive diagnosis (4). It is important to distinguish between mucorales and other fungi like fusarium, pseudallescheria and aspergillous species. The hyphae of mucorales organism typically are non septate, branching nondichotomously at right angles (4).
The success of treatment of mucormycosis depends on early diagnosis, reversal of predisposing factors, surgical debridement and prompt antifungal therapy (6). The mainstay of medical management mainly is Amphotericin B, but it is nephrotoxic(11). Majority of patients have chronic kidney disease like in our patient, so cautious use is required. Lipid formation of Amphotericin B has significantly less nephrotoxicity and can be used in higher doses. Hence it has become cornerstone of treatment of mucormycosis.
Recommended starting dose of LFAB is 5-7.5 mg/kg/day(11). Other drugs like Deferasirox (Iron chelator) or posaconazole are used as salvage options in cases of resistant disease or intolerance to Amphotericin B (12). Combination therapies of LFAB with deferasirox and LFAB-echinocandin have shown promising results in preclinical studies, but definitive trials are required to prove their efficacy(11).
Mucorales organism is angioinvasive causing thrombosis of vessels leading to poor penetration of antifungal agents. Hence debridement of the necrotic part is very important for complete eradication of mucormycosis (12). Chen et al showed successful treatment of spinal mucormycosis with repeated debridements(4). In our case because of medical comorbidities, we could not perform debridement.
Thus, as the incidence of Mucorales infection increase due to increase in patients with predisposing factors, the unusual sites of affection increase. Treating clinician should have a high vigilance in patients with predisposing factors. Although there is dramatic improvement in the treatment modalities of mucormycosis, still the mortality is high. Early diagnosis is important to prevent dissemination and timely intervention in order to reduce morbidity and mortality. A well equipped multidisciplinary approach for clinico-radiological assessment and management is necessary.
Conclusion
Mucormycosis of spine is a rare condition. Treating clinician should be aware of its predisposing factors and clinic oradio logical appearance. Early and prompt diagnosis decreases morbidity and mortality. Aggressive multi departmental approach is required for treatment of this lifethreatening condition.
Clinical Messege
Mucormycosis should be considered as an differential of atypical infection of spine. Proper clinicoradiological assessment is required for diagnosis. Aggressive multidepartmental approach is required for treatment of this lifethreatening condition.
Biography




Footnotes
Conflict of Interest: Nil
Source of Support: None
Reference
- 1.Baker RD. Pulmonary mucormycosis. Am J Pathol. 1956;32:287–313. [PMC free article] [PubMed] [Google Scholar]
- 2.Goodman NL, Rinaldi MG. Agents of mucormycosis. In: Balows A, Hausler WJ, Herrmann KL, Isenberg HD, Shadoomy HJ, editors. Manualof clinical microbiology. 5th ed. Washington, DC: ASM Press; 1991. pp. 674–92. [Google Scholar]
- 3.Manifestations of Mucormycosis d CID 2012. 2012 Feb;54(Suppl 1):23–341. doi: 10.1093/cid/cir866. [DOI] [PubMed] [Google Scholar]
- 4.Chen F, Lü G, Kang Y, Ma Z, Lu C, Wang B, Li J, Liu J, Li H. Mucormycosis spondylodiscitis after lumbar disc puncture. Eur Spine J. 2006 Mar;15(3):370–6. doi: 10.1007/s00586-005-1025-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buruma OJ, Craane H, Kunst MW. (1979) Vertebral osteomyelitis and epidural abscess due to mucormycosis, a case report. Clin Neurol Neurosurg. 81(1):39–44. doi: 10.1016/s0303-8467(79)80005-0. [DOI] [PubMed] [Google Scholar]
- 6.Spellberg B, Edwards J, Jr, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. ClinMicrobiol Rev. 2005;18:556–69. doi: 10.1128/CMR.18.3.556-569.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prabhu RM, Patel R. Mucormycosis and entomophthoramycosis: a review of theclinical manifestations, diagnosis and treatment. Clin Microbiol Infect. 2004 Mar;10(Suppl 1):31–47. doi: 10.1111/j.1470-9465.2004.00843.x. [DOI] [PubMed] [Google Scholar]
- 8.Sharma R, Shivanand G, Kumar R, Prem S, Kandpal H, Das CJ, Sharma MC. Isolatedrenal mucormycosis: an unusual cause of acute renal infarction in a boy withaplastic anaemia. Br J Radiol. 2006 Jul;79(943):e19–21. doi: 10.1259/bjr/17821080. [DOI] [PubMed] [Google Scholar]
- 9.Han S. R, Choi C. Y, Joo M, Whang C. J. Isolated cerebral mucormycosis. J. Korean Neurosurg. Soc. 2007;42:400–402. doi: 10.3340/jkns.2007.42.5.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma MC, Gill SS, Kashyap S, Kataria R, Gupta DK, Sahni P, Acharya SK. Gastrointestinal mucormycosis--an uncommon isolated mucormycosis. Indian J Gastroenterol. 1998 Oct Dec;17(4):131–3. [PubMed] [Google Scholar]
- 11.Spellberg B, Walsh TJ, Kontoyiannis DP, Edwards J, Jr, Ibrahim AS. Recentadvances in the management of mucormycosis: from bench to bedside. Clin InfectDis. 2009 Jun 15;48(12):1743–51. doi: 10.1086/599105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spellberg B, Ibrahim AS. Recent advances in the treatment of mucormycosis. Curr Infect Dis Rep. 2010 Nov;12(6):423–9. doi: 10.1007/s11908-010-0129-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


