Abstract
Introduction:
Metallosis occurs when periprosthetic soft tissues, synovium, and/or bone is infiltrated by metallic debris secondary to metal-on-metal wear. This debris can cause a chronic inflammatory reaction leading to joint instability, pain, and swelling, and may cause osteolysis, implant looseningand ultimately implant failure.
Case Report:
An 81 year old female, with a history of primary left total knee arthroplasty, presented with a 6 month history of left knee pain, swelling, and limited range of motion following a fall. Radiographs and joint aspiration were performed, with results that showed no evidence of periprosthetic trauma or infection but were suspicious for chronic metallosis. The patient underwent revision total knee replacement of the left knee which revealed extensive necrotic black metal debris throughout the joint space. Histopathology confirmed the diagnosis of a foreign body reaction consistent with metallosis.
Conclusion:
This case is a rare example of chronic metallosis presenting 26 years following total knee replacement. Treatment with revision total knee replacement is the consensus management choice to avoid further destruction of the bone and joint capsule that can occur with metal-induced inflammation.
Keywords: Aseptic loosening, severe osteolysis, metallosis, Metal-induced synovitis, bubble sign, metal-line sign, cloud sign
Introduction
Metallosis occurs when periprosthetic soft tissues, synovium, and/or bone is infiltrated by metallic debris secondary to metal- on-metal wear. This debris can cause a chronic inflammatory reaction leading to joint instability, pain, and swelling, and may cause osteolysis, implant loosening and ultimately implant failure. Metallosis is well documented in the total hip arthroplasty literature, mainly from the use of metal heads and liners. However, this condition is much less common following primary total knee arthroplasty (TKA). The TKA literature is limited to mainly case reports and series with patients generally presenting with chronic symptoms between 5 to 10 years out from the primary procedure [1-8].
Evaluation to rule out aseptic loosening, implant failure, trauma, and most importantly infection is performed with radiographs, bloodwork, and joint aspiration. Radiography is the most effective non-invasive method to diagnosis metallosis, with three radiographic signs – “bubble”, “cloud” and “metal-line” signs - cited in the literature [1-8]. Furthermore, serological tests and arthrocentesis need to be performed to rule out an infectious etiology. In general, persistent chronic elevations of erythrocyte sedimentation rate (ESR) and C-Reactive protein (CRP) following TKA are suspicious for an infected implant [9]. Regarding synovial fluid leukocyte count and differential, results that might point us to consider infection include: > 1100 WBC/ml with a neutrophil (PMN) percentage > 64% (8 8% and 94% specificity, respectively) [10-11]. If both the synovial fluid leukocyte count and differential are below these numbers, infection is highly unlikely with a negative predictive value of nearly 99% [10]. As such, in the presence of radiographic signs of metallosis and absence of infectious markers, a diagnosis of metallosis can be made with relative accuracy [4, 5, 7, 8].
When described in total knee replacement, most cases of metallosis are secondary to a metal-backed patellar implant grinding on the femoral component [5]. Here we describe a case report of severe metallosis occurring in an 81 year old patient, and detail the diagnostic, treatment, and postoperative protocols used for her management.
Case report
An 81-year-old female presented with 6 months of left knee pain, instability and swelling after a ground-level fall. The patient had a history of primary left total knee arthroplasty to treat rheumatoid arthritis performed in 1988. She otherwise had no pertinent past medical history. The patient reported severe pain with weight-bearing and knee flexion, and had been taking anti-inflammatory medication as needed, and has been using a cane for ambulation. She denied any constitutional symptoms indicative of infection. On physical exam, the patient had a slight joint effusion and passive range of motion from 5 degrees to 100 degrees. The knee was unstable on varus and valgus testing, in extension, mid flexion, and 90 degrees of flexion. There was slight joint line tenderness medially and laterally as well as palpable crepitus and grinding when ranging the knee.
Knee radiographs revealed amorphous densities in the posterior capsule and the suprapatellar recess consistent with the “cloud sign” (Fig 1a) and curved radiodensities around the distal femur and joint capsule both medially and laterally, consistent with the “bubble sign” (Fig 1b). There was severe osteolysis with loosening of both the femoral implant and tibial base plate. A knee arthrocentesis was done in clinic, with significant amounts of black-tinged fluid aspirated (Fig 2). Infection was ruled out with joint fluid analysis resulting in a WBC count of 406 and PMN % of 6. Bloodwork was obtained, with CRP and ESR levels within normal range. Given the severe pain, evidence of implant aseptic loosening and high clinical suspicion for metallosis, the recommendation was made for the patient to undergo left revision total knee arthroplasty.
Figure 1.
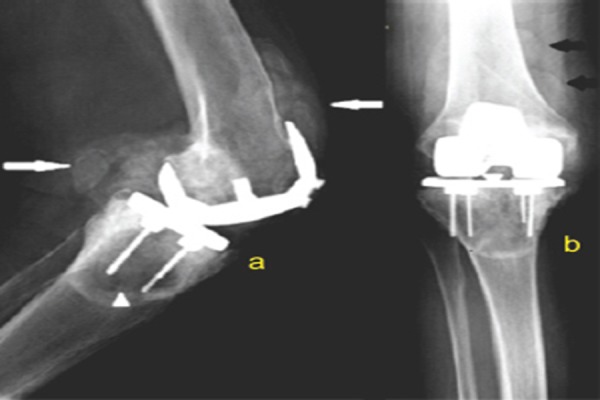
a) Lateral radiograph of the left knee showing severe osteolysis beneath the tibial component (white arrowhead) and amorphous curved densities, known as “Cloud” sign (white arrows). b) Postero-anterior radiograph of the left knee showing semicircular radio densities representing metal deposition outlining the synovium and joint capsule, known as “Bubble” sign (black arrows)
Figure 2.
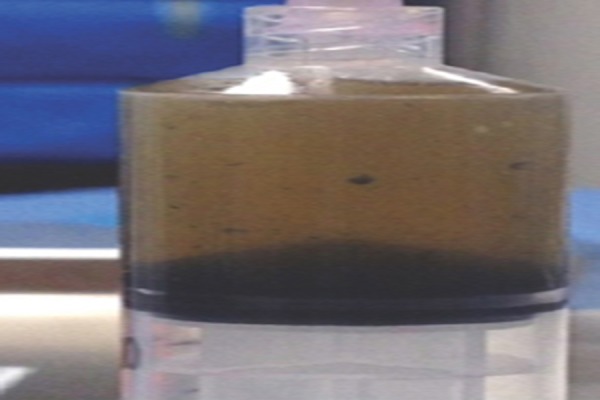
Arthrocentesis of the joint pre - operatively yielded a black-tinged fluid suspicious for metallosis.
During the operation, there was extensive necrotic black material overlying the entire knee joint after arthrotomy (Fig 3a). A complete synovectomy was performed at the medial and lateral gutters and suprapatellar and infrapatellar regions to remove metallic debris (Fig 3b). The patellar button was noted to be a metal-backed. The tibial polyethylene liner was found to be severely worn but it was not fractured or worn through at any area. The femoral component had evidence of aseptic loosening as well as severe distal femoral osteolysis. After component removal, there was evidence of severe osteolysis of both posterior condyles and extensive metal debris overlying the femoral canal (Fig 4a). Similarly, there was evidence of severe osteolysis underneath the tibial baseplate with bone resorption into the proximal tibial metaphysis after the tibial component was removed (Fig 4b).
Figure 3.

a) Black necrotic metallic debris material noted in the joint space. b) resected synovium with extensive black metallic debris material noted throughout
Figure 4.
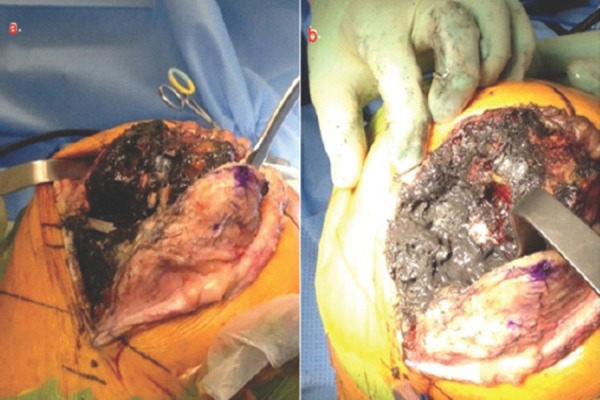
a) Extensive black metallic debris material noted over the distal femur and femoral canal upon removal of the femoral component, b) Extensive black metal debris material noted over the tibia following removal of the tibial component.
Close inspection of the implants revealed metallic wear secondary to grinding on both the femoral component (Fig 5a) and metal backed patella (Fig 5b), as well as along the lateral surface of the tibial plate (Fig 5c). After irrigation and debridement, most of the metal debris was removed. The revision implants included long press-fit diaphysis fitting stems in both the femur and tibia and a varus-valgus constrained component with tibial and femoral wedges used to reconstitute the bone loss and restore the anatomical joint line. An oxidized zirconium femoral component was used to prevent repeat metallic wear (Smith & Nephew, Memphis, TN). The patellar component was removed in its entirety and not replaced due to insufficient bone stock to support a new patella button (Figs 6a and 6b).
Figure 5.

a) The femoral component showing metal wear and erosion. b) Metallic wear of the patella button, c) Erosion of the edge of the lateral tibial base plate.
Figure 6.
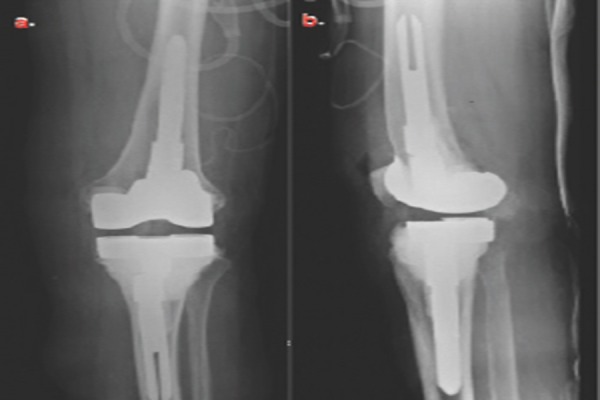
a) Antero-posterior postoperative radiograph showing revision TKA b) lateral post operative radiograph showing revision TKA
Intraoperative joint fluid analysis was again negative for infection, with WBC count 243 and PMN % of 10. Histologic examination of the periprosthetic tissues demonstrated extensive fibrosis (Fig 7a) with multiple histiocytes (Fig 7b) and multi-nucleated giant cells (Fig 8) consistent with the diagnosis of metallosis.
Figure 7.
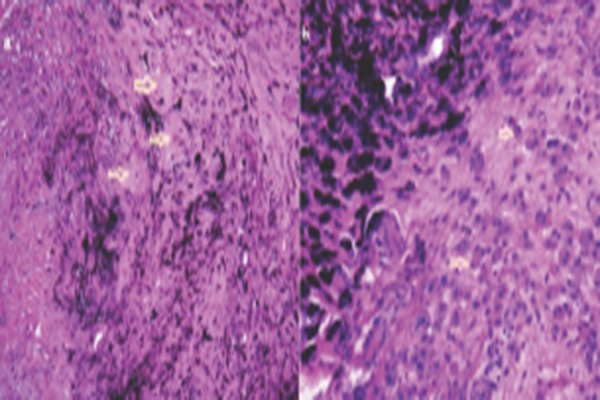
Synovial microscopic histology showing : a) black pigment interspersed within extensive fibrosis (white arrows). b) black pigment (left) neighboring multiple histiocytes (white arrows)
Figure 8.
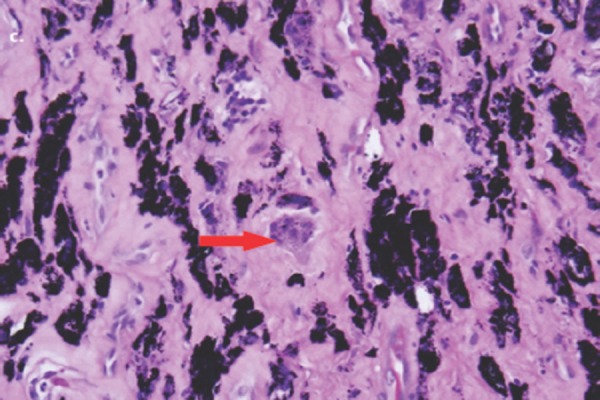
Synovial microscopic histology showing a multinucleated giant cell (red arrow)
The patient was allowed to be weight-bearing as tolerated with an unlocked Bledsoe brace. She was able to ambulate and perform range of motion exercises with physical therapy and was discharged on postoperative day 3. At 6 weeks follow-up, her incision was healed, she was ambulating well without an assistance device, and her range of motion was 0-110 degrees. The knee was stable to varus and valgus stress.
Discussion
In this case report we describe a patient with symptomatic metal-induced synovitis, commonly referred to as metallosis, which presented as a late complication of total knee arthroplasty. After appropriate diagnostic studies ruled out other etiologies of her implant failure, a revision total knee arthroplasty was performed and the patient was able to regain a functional ambulatory status.
Most cases of metallosis after total knee replacement are due to wear of a metal-backed polyethylene patellar prosthesis [5], and this was the likely source of our patient’s TKA aseptic failure based on the significant patellar destruction. Metal-backed patellar implants are no longer commonly used, but close evaluation should be kept on patients with these components and metallosis should be at the top of the differential if they present with complaints such as effusion, grinding and pain. In addition, the patient in our case also had wear of the titanium tibial and femoral components with both components showing signs of erosion. A review of the current literature revealed that titanium components appear to have an increased association with metal wear leading to metallosis as compared to chromium-cobalt comprised implants [8]. Newer implants such as the one used in this case (Smith and Nephew’s Oxinium) are composed of oxidized zirconium with the goal of reducing metal wear and should result in fewer incidences of metallosis in the future [12]. These components should preferentially be used during revision cases to limit any additional spread of metal debris.
Metallosis can be suspected pre-operatively with radiographic signs such as the “cloud sign,” “bubble sign” and the “metal-line signs”, with our patient displaying the former two on lateral and PA radiograph images. The “cloud” sign is the most commonly cited radiographic indication of possible metallosis and is described as amorphous, fluffy densities in periprosthetic soft tissues, most commonly found posterior to the knee implant [1, 2, 5] Additionally, bubbly appearing radiodensities representing metal deposition outlining the synovium are known as the “bubble” sign. Finally, the “metal-line” sign is a thin linear radiodense line that outlines part of the joint capsule (most commonly in the suprapatellar pouch) and is fairly specific for metal-induced synovitis. Evidence of these signs on imaging should prompt a close evaluation for metallosis. Serology and arthrocentesis also need to be performed to rule out infectious etiology. In general, a peripheral WBC count is not useful diagnostic measure since it is generally normal in TKA infections while persistent elevation of ESR, with abnormal levels defined as > 30 mm/hr three months to one year after TKA, is often indicative of infection (specificity of 87%) [9]. Similarly, elevated CRP levels defined as > 10 pg/ml at least 14-21 days after TKA also point to an infectious etiology (specificity 83%) [9]. Regarding synovial fluid leukocyte count and differential, the numbers to consider a possible infection, include >1100 WBC/ml with a PMN percentage > 64% (88% and 94% specificity, respectively) [10-11]. As such, in the presence of radiographic signs of metallosis and absence of infectious markers, a diagnosis of metallosis can be made with relative accuracy [4, 5, 7, 8].
If clinically and radiographically suspected, treatment with irrigation and debridement along with synovectomy and revision total knee replacement is the consensus management choice to avoid further destruction of the bone and joint capsule that can occur with metal induced inflammation [1-2]. A thorough debridement should be performed, to both remove the source of inflammation and to decrease the particle count that could lead to third body wear. All components should be removed and replaced, preferably with implants with coatings that have high resistance to metallic debris. A more constrained system should be used to limit postoperative instability in cases of severe bone loss and ligament compromise. With a significant amount of bone loss likely from chronic osteolysis, augments or bone grafting may be needed to reconstitute the joint line.
Conclusion
Metallosis after TKA is an uncommon complication that can lead to significant functional impairment. Orthopaedic surgeons should be aware of the pertinent clinical and radiographic signs and be prepared to perform an extensive revision surgery to restore joint function. As seen with this case of severe chronic metallosis, appropriate diagnosis and treatment can lead to a successful result.
Clinical Messege
Although rare after total knee arthroplasty, orthopaedic surgeons should be aware of the pertinent clinical and radiographic signs of metallosis and be prepared to perform an extensive revision surgery to restore joint function.
Biography

Footnotes
Conflict of Interest: Nil
Source of Support: None
Reference
- 1.Helito CP, Buarque de Gusmão CV, Angelini FJ, et al. Severe metallosis following total knee arthroplasty: a case report and review of radiographic signs. Skeletal Radiol. 2014 Aug;43(8):1169–73. doi: 10.1007/s00256-014-1860-3. [DOI] [PubMed] [Google Scholar]
- 2.Vivegananthan B, Shah R, Karuppiah AS, Karuppiah SV. Metallosis in a total knee arthroplasty. BMJ Case Rep 2014. 2014 Mar 18; doi: 10.1136/bcr-2013-202801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O’Brien ST, Burnell CD, Hedden DR, Brandt JM. Abrasive wear and metallosis associated with cross-linked polyethylene in total hip arthroplasty. J Arthroplasty. 2013 Jan;28(1):197.e17–21. doi: 10.1016/j.arth.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 4.Keene GC, Oakeshott RD. Early metallosis-related failure after total knee replacement: a report of 15 cases. J BoneJointSurg Br. 2011 Feb;93(2):205–9. doi: 10.1302/0301-620X.93B2.25150. [DOI] [PubMed] [Google Scholar]
- 5.Romesburg JW, Wasserman PL, Schoppe CH. Metallosis and Metal-Induced Synovitis Following Total Knee Arthroplasty: Review of Radiographic and CT Findings. J Radiol Case Rep. 2010;4(9):7–17. doi: 10.3941/jrcr.v4i9.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paydar A, Chew FS, Manner PA. Severe periprosthetic metallosis and polyethylene liner failure complicating total hip replacement: the cloud sign. Radiology case reports. 2007;2:1–6. doi: 10.2484/rcr.v2i4.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Su EP, Callander PW, Salvati EA. The bubble sign: a new radiographic sign in total hip arthroplasty. J Arthroplasty. 2003;18:110–12. doi: 10.1054/arth.2003.50007. [DOI] [PubMed] [Google Scholar]
- 8.Weissman BN, Scott RD, Brick GW, Corson JM. Radiographic detection of metalinduced synovitis as a complication of arthroplasty of the knee. J Bone Joint Surg Am. 1991 Aug;73(7):1002–7. [PubMed] [Google Scholar]
- 9.Greidanus NV, Masri BA, Garbuz DS, et al. Use of erythrocyte sedimentation rate and C-reactive protein level to diagnose infection before revision total knee arthroplasty. A prospective evaluation. J Bone Joint Surg Am. 2007 Jul;89(7):1409–16. doi: 10.2106/JBJS.D.02602. [DOI] [PubMed] [Google Scholar]
- 10.Ghanem E, Parvizi J, Burnett RS, et al. Cell count and differential of aspirated fluid in the diagnosis of infection at the site of total knee arthroplasty. J Bone Joint Surg Am. 2008 Aug;90(8):1637–43. doi: 10.2106/JBJS.G.00470. [DOI] [PubMed] [Google Scholar]
- 11.Kalore NV, Gioe TJ, Singh JA. Diagnosis and management of infected total knee arthroplasty. OpenOrthop J. 2011 Mar 16;5:86–91. doi: 10.2174/1874325001105010086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Essner A, Herrera L, Hughes P, Kester M. The influence of material and design on total knee replacement wear. JKneeSurg. 2011 Mar;24(1):9–17. doi: 10.1055/s-0031-1275390. [DOI] [PubMed] [Google Scholar]


