Abstract
There is a need for longitudinal research to understand how psychopathology relates to the onset and maintenance of substance use from adolescence into young adulthood. Hence, we investigate the longitudinal, reciprocal influences of internalizing (anxiety and depression) and externalizing (oppositional defiance) symptoms on heavy episodic drinking (HED; ≥5 drinks per occasion) and alcohol-related harms in a community-based sample of youth aged 12–27 years. Participants were chosen from the Victoria Healthy Youth Survey, followed six times, biennially between 2003 and 2013 (N = 662). Analyses used cross-lagged panel models to examine reciprocal relations over time. Differences across age and sex were also tested. Defiance symptoms predicted increases in HED, which reciprocally predicted increases in defiance symptoms for females. Internalizing symptoms were related to HED within time for females. Alcohol-related harms had reciprocal positive associations with internalizing and defiance symptoms for both males and females. Associations were largely invariant across age groups, suggesting that the presence and strength of associations persisted across development. While psychopathology preceded the onset of HED and harms, the overall findings suggest that these risk processes are mutually reinforcing across development and that youth may become entrenched in an interdependent cycle that significantly increases their risk of comorbid disorders in adulthood.
Keywords: internalizing symptoms, externalizing symptoms, heavy drinking, alcohol, harm, adolescence, young adulthood, longitudinal
Introduction
A review of prevalence of psychiatric disorders shows that substance use disorders are the most common diagnoses (12%) in adolescence and young adulthood, particularly alcohol use disorders, followed by anxiety (10.7%) and depressive (6%) disorders and behavioral disorders (3%–4%).1,2 Reviews also confirm the high comorbidity of substance use disorders with internalizing and externalizing disorders in both clinical- and community-based samples of adolescents.1,3–8 With some notable exceptions, which include children with family histories of substance use, symptoms of both internalizing and externalizing problems typically precede the onset of substance use disorders in childhood and adolescence.7,8 However, a better understanding is needed of the course and reciprocal effects of these concerns from adolescence to young adulthood. While “adulthood” is often delineated by several legal and social markers (eg, voting rights, moving out of parents’ home, earning a living wage, marriage, and child bearing), researchers have argued that this transitional phase has been elongated in North American youth and the terms “young” or “emerging” adulthood designate youth from ~18 years old into the late 20s.9 This is also a period when symptoms of both mental illness and substance abuse can become entrenched and when prevention or early diagnosis and intervention are possible.
There is a clear need for longitudinal research to increase the understanding of how developing and changing levels of psychopathology are related to the onset and maintenance of substance abuse and related harms from adolescence to young adulthood. However, this longitudinal research is complicated not only by the high comorbidity among these symptoms but also by the past research showing inconsistent findings related to sampling (of clinical- vs community-based youth), sex of participants, measures of psychopathology used (diagnostic categories vs symptom levels), and substance specificity (alcohol, cannabis, or illegal drugs). In this study, we focus on the codevelopment of internalizing (anxiety and depressive symptoms) and externalizing (oppositional defiance, ie, arguing, blaming others, angry, and resentful10) symptoms and problematic substance use by examining the concurrent and cross-lagged associations among these symptoms and heavy episodic drinking (HED) and alcohol-related harms over a period of 10 years, in a community-based sample of youth aged 12–27 years.
Reviews of past research consistently demonstrate the high co-occurrence of substance use disorders and other mental and behavioral problems.6,7 Much of this work has focused on clinical samples of youth who meet diagnostic criteria for these comorbid concerns.6,11,12 However, to inform early diagnosis and prevention efforts, a better understanding of the interrelations among subclinical symptoms and the trajectories of their development and mutual influences is needed before disorders are evident.13,14 While previously considered a disorder of childhood that was either self-limiting or, more rarely, evolved into more serious conduct disorders with deviant and aggressive behaviors by late adolescence, research demonstrates that symptoms of oppositional defiance may be common and stable from adolescence to young adulthood.15 Moreover, these symptoms (ie, defiance, arguing, blaming others, angry, and resentful10) may be particularly problematic by young adulthood, if these behaviors are extended to relationships with authorities at work or school or to romantic partners.16,17 Hence, we focus on the associations between oppositional defiance symptoms and alcohol use problems.
The trajectories of internalizing and externalizing symptoms and of alcohol use differ across the transition from adolescence to young adulthood. Using diagnostic criteria, studies with clinical samples show that internalizing disorders tend to increase or stabilize in the same period,3,18–21 whereas externalizing disorders such as attention-deficit hyperactivity disorder (ADHD) and conduct disorders typically decline in the transition to young adulthood.1 On the contrary, alcohol use becomes increasingly accessible across this age period and increases in the use of alcohol persist well into young adulthood before declines become evident.22,23 How differences in the developmental trajectories of psychopathology and alcohol use effect their associations and mutual influences is not known. In addition, the high comorbidity between internalizing and externalizing problems is rarely accounted for in studies of the effects of internalizing and externalizing symptoms on alcohol use.24
Most research examining the association between the development of substance use disorders and mental illness often consider multiple substances together in studies7,24 There is also some evidence that specific types of psychopathology may be related to specific types of substances. For example, Farmer et al.25 show that externalizing, but not internalizing, disorders predicted cannabis use between ages 16 and 30 years. In this study, we focus on a commonly used substance (ie, alcohol) that becomes increasingly accessible in the transition to young adulthood. More specifically, HED (defined as the consumption of five or more drinks in a single sitting26) may reflect problematic drinking patterns and both HED and experiences of alcohol-related harms may herald the onset of an alcohol use disorder later on.27,28 Again, most research uses clinical diagnosis of an alcohol use disorder as an outcome, with little knowledge of how subclinical, yet meaningful, indicators may emerge in response to early mental health symptoms and similarly how subclinical alcohol indicators influence psychopathology before the emergence of an actual alcohol use disorder.6
With specific focus on alcohol use, research shows that internalizing29–31 and externalizing symptoms32,33 are predictive of alcohol use disorders; yet, most of these studies do not account for both internalizing and externalizing symptoms.29–31 For example, using the National Longitudinal Study of Adolescent Health (Add Health), Marmorstein30 found that depressive symptoms and alcohol-use-related problems (ie, harms) were reciprocally related from early adolescence into young adulthood (ages 12–26 years); however, externalizing symptoms were not accounted for. When the comorbidity between internalizing and externalizing symptoms is controlled for, some studies do not support the unique effects of internalizing symptoms.29,34 Further, we know little about the reciprocal and potentially perpetuating effects (ie, how alcohol use influences psychopathology) while accounting for both forms of symptomatology.
The current study investigates the longitudinal, reciprocal influences of internalizing (anxiety and depression) and externalizing (oppositional defiance) symptoms on early indicators of problematic alcohol use (HED and alcohol-related harms that affect health, work, relationships, and academic achievement resulting from alcohol use) in a community-based sample of youth aged 12–27 years. Based on the earlier literature, we hypothesize that internalizing and externalizing symptoms would predict the alcohol-use-disorder-related outcomes over time.6–8 However, as there is a lack of evidence of the reciprocal effects (eg, alcohol use predicting mental health symptoms) across these developmental periods, we cannot make hypotheses about the effects of indicators of alcohol use on mental health symptomatology. Additionally, we examine whether the strength of the associations varies across developmental time (ie, age groups) by testing for invariance in parameter estimates across age groups. This allows us to determine whether associations among internalizing and externalizing symptoms and alcohol use outcomes are specific to or stronger at identified developmental periods between ages 12 and 27 years.
We also examine sex differences in the associations between internalizing and externalizing symptoms and alcohol use outcomes. Males and females differ in their levels of alcohol use, with males exhibiting higher levels,35 and in the prevalence and trajectories of mental health problems, with females showing higher levels of internalizing symptoms and males showing higher levels of externalizing symptoms.1,20 However, research findings regarding sex differences in the relations between psychopathology and substance abuse are inconsistent. For example, Colder et al.24 found no sex differences in the associations between internalizing and externalizing symptoms and alcohol, tobacco, and marijuana use in adolescence. In contrast, Miettunen et al.32 found similar associations between externalizing symptoms and alcohol use for males and females, but the longitudinal association between internalizing and alcohol use was significant only for females. Although earlier research with this sample shows expected sex differences, with higher levels of internalizing symptoms in females and higher levels of both externalizing symptoms20 and HED23 in males, sex differences in the interrelations among these concerns cannot be predicted from the available scant literature.
Methods
Participants and procedures
Participants were chosen from the Victoria Healthy Youth Survey (V-HYS), a six-wave biennial study conducted between 2003 and 2014 (see Leadbeater et al.20 for further details). The participants were recruited from a medium-sized Canadian city using random digit dialing of 9,500 private telephone listings. Of 1,036 eligible households, 662 youth aged 12–18 years (M = 15.52; standard deviation [SD] = 1.93; 51% female) had parent consent and agreed to participate (64% at Time 1). Retention rates were high across waves; 87% at Time 2, 81% at Time 3, 70% at Time 4, 70% at Time 5, and 72% at Time 6. The sample was 85% Caucasian, 4% Asian, 4% mixed/biracial, 3% Aboriginal, and 4% other. Nineteen percent of both fathers and mothers had no education beyond high school, whereas 43% of fathers and 49% of mothers had college or university training, suggesting an economically diverse sample. Time 1 living situation (59% lived with both of their biological or adoptive parents), parental education, and ethnicity were almost identical to that of the population from which the sample was drawn.25 Attrition was assessed by testing for differences on Time 1 demographics (age, sex, and mother’s education) and the first measurement occasion of study variables (Time 1 internalizing symptoms, oppositional defiance symptoms, Time 1 HED, and Time 3 alcohol-related harms) between youth who remained in the study (n = 478) and those who did not participate at Time 6 (n = 184). The participants who dropped out were more likely to be males, χ2 (1, 662) = 8.77, P = 0.003, had lower levels of mother’s education, F(1, 655) = 14.90, P < 0.001 (M = 2.55 vs 3.01), and higher Time 3 harms, χ2 (1, 538) = 5.00, P = 0.025. No other group differences were noted.
At each wave, youth and one parent or guardian (for youth under the age of 18 years) gave written consent for their participation and received a gift certificate. A trained interviewer administered the V-HYS in individual interviews in the youth’s home or another private place. Skype or phone interviews were also used when necessary to follow youth who moved or were traveling. To enhance privacy and increase responding, questions dealing with private topics (including alcohol use and mental health symptoms) were privately completed using a paper questionnaire. For youth who were interviewed in person, their completed questionnaire was handed over to the interviewer in a sealed envelope. The participants who were not interviewed in person mailed in their responses. This project was approved by the University of Victoria Human Research Ethics Board (protocol #09–292) and this research complied with the principles of the Declaration of Helsinki.
Measures
Alcohol use
HED was assessed using the following item: “How often in the past 12 months have you had five or more drinks on one occasion?” Response options ranged from 0 (never) to 4 (more than once a week). The following definition of a standard drink was provided: “When we use the word ‘drink’, it means: 1) one glass, bottle or can of beer (about 12 oz.); 2) one glass of wine (about 5 oz.) or a wine cooler (about 10 oz.); c) one drink or cocktail with liquor (about 1.5 oz. of liquor).” Due to skewness, HED was dichotomized into: drinking five or more drinks more often than monthly (1), and never or a few times/year (0).36
Alcohol-related harms
Six items from the Harmful Effects of Alcohol Scale (for earlier version see Hilton37) adapted from the Personalized Alcohol Use Feedback Scale (http://notes.camh.net/efeed.nsf/feedback) were collected from Time 3 to Time 6. Youth were asked: “In the last 12 months, was there ever a time that you felt your alcohol use had a harmful effect on your…(1) friendships and social life; (2) physical health; (3) outlook on life; (4) home life or marriage; (5) work, studies or employment; and (6) financial opportunities.” Response options were 0 (no) and 1 (yes). Items were summed and then dichotomized into: no harm (0) and at least one harm (1). This method has been used effectively in the past.38
Internalizing and oppositional defiance symptoms
The brief child and family phone interview (BCFPI)39 assesses criteria for child and adolescent psychiatric disorders using the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV), including symptoms of internalizing (anxiety and depression) and externalizing (oppositional defiance). Items for each symptom category were rated on a three-point scale (0 = never, 1 = sometimes, or 2 = often) in response to the question, “Do you notice that you […item].” Example items include; “…worry about things in the future?” (anxiety; 6 items), “…get no pleasure from your usual activities?” (depression; 6 items), “…are easily annoyed by others?,” and “…argue a lot with others?” (oppositional defiance; 6 items; see Leadbeater and Homel15 for full list of items). Scores ranged from 0 to 24 for the internalizing symptoms and from 0 to 12 for oppositional defiance symptoms. Internal consistencies were high across symptom categories by wave: 0.81–0.89 for internalizing symptoms (0.75–0.82 for anxiety and 0.80–0.86 for depression) and 0.71–0.76 for oppositional defiance symptoms. The BCFPI has been shown to be invariant across sex and time in the previous studies using the V-HYS data.15,20
Socio economic status
Socio economic status (SES) was assessed as a rating of mother’s education on a five-point scale ranging from 1 = less than high school to 5 = finished college/university.
Plan of analyses
To examine the bidirectional associations among internalizing symptoms, oppositional defiance symptoms, and alcohol outcomes from adolescence through young adulthood, the six waves of data were rearranged based on the participant’s age at each interview. Data were grouped into two-year age intervals (ie, ages 12–13, 14–15, 16–17, 18–19, 20–21, 22–23, 24–25, and 26–27 years) to maintain adequate power for analyses. Observations at ages 28–30 years were not included due to low covariance coverage across time. Less than 1% of the sample (n = 3) reported HED at ages 12 and 13 years; thus, HED at these ages was not included in the final models. Alcohol-related harms were measured beginning at ages 16–17 years, and data are not available at earlier ages. All models controlled for mother’s education given that alcohol use tends to be higher among higher SESs.40 Mother’s education was used as a proxy for SES as it is the most commonly used SES measure in the literature.41
First, to examine the longitudinal reciprocal effects among internalizing symptoms, oppositional defiance symptoms, and alcohol outcomes, we used cross-lagged panel models that examined the associations across eight time points representing ages 12–27 years. Models were run separately for HED and alcohol-related harms. Each model included (1) autoregressive paths assessing temporal stability of each construct over time (ie, internalizing symptoms at ages 12–13 years with internalizing symptoms at ages 14–15 years), (2) within-time covariances between constructs (ie, internalizing symptoms at ages 12–13 years with HED at ages 12–13 years), and (3) cross-lagged paths between all constructs (ie, internalizing symptoms at ages 12–13 years with HED at ages 14–15 years). Mother’s education was controlled for in all analyses.
Second, to determine whether the strength of the associations varies across development and to establish the most parsimonious model, we tested whether the autoregressive paths, within-time correlations, and cross-lagged paths were invariant across time. Invariance was tested by comparing changes in model fit resulting from imposing and releasing equality constraints on each of the model parameters following a bottom-up procedure (moving from an unconstrained model to a fully constrained model) as recommended by Bollen and Curran.42 Constraints were tested in the following order: (1) autoregressive paths, (2) within-time covariances, and (3) cross-lagged paths.
Comparisons of the differences in the log-likelihoods and the degrees of freedom between the models were used to test the null hypothesis using the more restricted model fit as well as the less restrictive model. Nonsignificant differences between log-likelihoods indicated the constrained model fit as well as the unconstrained model, signifying that paths were invariant across time and should be constrained to equality. Incorporation of constraints in cross-lagged models has been shown to improve the power to detect the cross-lagged effects.43
Third, we tested whether the strength of the associations varied across sex. Similarly, sex invariance was tested using multiple group models.44 This method compares the changes in model fit resulting from imposing and releasing equality constraints on each of the model parameters following the same bottom-up procedure (moving from an unconstrained model to a fully constrained model) as used for testing invariance across time. Nonsignificant differences between log-likelihoods indicated the constrained model fit as well as the unconstrained model, signifying that paths were invariant across sex and should be constrained to equality.
Final models included all relevant time and sex constraints on parameters, representing the best fitting and most parsimonious model of the longitudinal reciprocal associations among internalizing, externalizing, and alcohol outcomes. All models were fit using MPlus 7.1144 and full-information maximum likelihood estimation for missing data. Standard indices were used to assess model fit (ie, chi-square [χ2] goodness-of-fit test, RMSEA ≤0.08, and CFI ≥0.90 were used to delineate adequate fit). Data were initially run with symptoms of anxiety and depression considered separately; however, the findings for each symptom domain were nearly identical so these were combined to form an overall measure of internalizing to reduce redundancy and facilitate the ease of interpretation in reporting the results.
Results
Descriptive analyses
Means and SDs for symptoms of internalizing and oppositional defiance are presented for males and females in Table 1. Females reported significantly higher levels of internalizing symptoms at ages 14–15 years than males. No other sex differences in mean levels of symptoms were found. The proportions of the sample endorsing HED and experiencing alcohol-related harms are reported in Table 2. The proportion of males reporting HED was >80% in each age group after ages 18–19 years, and it was significantly higher for males than for females (range 25%–74%) in each age group, except at ages 20–21 years (males 84% and females 78%). Females were more likely to report alcohol-related harms in adolescence; however, sex differences in the prevalence of alcohol-related harms were not significant at any age.
Table 1.
Mean levels of psychopathology symptoms by age and sex.
| MALES (48%; n = 320) | FEMALES (52%; n = 342) | F | RANGE | |||||
|---|---|---|---|---|---|---|---|---|
| MEAN | SD | n | MEAN | SD | n | |||
| SES | 3.87 | 1.36 | 315 | 3.89 | 1.39 | 342 | 0.05 | 1–5 |
| Internalizing | ||||||||
| 12–13 | 7.07 | 3.58 | 80 | 7.54 | 4.24 | 93 | 0.60 | 0–19 |
| 14–15 | 7.84 | 3.93 | 160 | 9.03 | 4.43 | 183 | 6.77** | 0–23 |
| 16–17 | 8.96 | 4.19 | 258 | 9.65 | 4.22 | 268 | 3.51 | 1–22 |
| 18–19 | 9.49 | 4.38 | 225 | 10.08 | 4.70 | 260 | 1.98 | 0–24 |
| 20–21 | 9.54 | 4.30 | 195 | 9.48 | 4.61 | 241 | 0.02 | 0–24 |
| 22–23 | 9.18 | 4.76 | 158 | 9.23 | 4.57 | 190 | 0.01 | 0–24 |
| 24–25 | 8.19 | 4.81 | 139 | 8.48 | 4.76 | 156 | 0.27 | 0–21 |
| 26–27 | 8.60 | 5.29 | 104 | 8.76 | 4.39 | 108 | 0.06 | 0–24 |
| Oppositional defiance | ||||||||
| 12–13 | 4.20 | 2.13 | 80 | 3.84 | 2.36 | 93 | 1.12 | 0–11 |
| 14–15 | 4.20 | 2.36 | 160 | 4.53 | 2.50 | 183 | 1.56 | 0–12 |
| 16–17 | 4.22 | 2.25 | 258 | 4.36 | 2.33 | 268 | 0.52 | 0–12 |
| 18–19 | 4.30 | 2.32 | 225 | 3.98 | 2.35 | 260 | 2.22 | 0–12 |
| 20–21 | 3.96 | 2.41 | 195 | 3.55 | 2.16 | 241 | 3.43 | 0–11 |
| 22–23 | 3.55 | 2.30 | 157 | 3.54 | 2.16 | 190 | 0.001 | 0–11 |
| 24–25 | 3.52 | 2.08 | 139 | 3.14 | 2.21 | 156 | 2.35 | 0–11 |
| 26–27 | 3.28 | 2.38 | 104 | 3.12 | 2.11 | 108 | 0.26 | 0–10 |
Notes:
P < 0.001,
P < 0.01,
P < 0.05.
Table 2.
Prevalence of heavy episodic drinking and alcohol-related harms by sex.
| MALES (48%; n = 320) | FEMALES (52%; n = 342) | χ2 | N | |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Heavy episodic drinking | ||||
| 12–13 | 3 (4%) | 0 (0%) | 3.54† | 173 |
| 14–15 | 40 (25%) | 45 (25%) | 0.01 | 343 |
| 16–17 | 167 (65%) | 130 (49%) | 14.07*** | 526 |
| 18–19 | 181 (81%) | 172 (65%) | 12.88*** | 481 |
| 20–21 | 162 (84%) | 187 (78%) | 2.37 | 435 |
| 22–23 | 135 (85%) | 140 (74%) | 7.20** | 348 |
| 24–25 | 120 (86%) | 112 (72%) | 8.72** | 294 |
| 26–27 | 86 (84%) | 61 (57%) | 18.66*** | 209 |
| Alcohol-related harms | ||||
| 16–17 | 13 (21%) | 25 (32%) | 2.01 | 141 |
| 18–19 | 34 (31%) | 51 (41%) | 2.63 | 234 |
| 20–21 | 76 (46%) | 82 (40%) | 1.19 | 368 |
| 22–23 | 63 (40%) | 58 (31%) | 3.32 | 348 |
| 24–25 | 45 (32%) | 52 (33%) | 0.03 | 295 |
| 26–27 | 33 (32%) | 25 (23%) | 2.22 | 210 |
Notes:
P < 0.001,
P < 0.01,
P < 0.05,
P < 0.10.
Internalizing symptoms, oppositional defiance symptoms, and HED
The cross-lagged panel model had an adequate fit to the data (χ2 (171) = 473.09, P < 0.05, RMSEA = 0.05, CFI = 0.91). We examined the longitudinal invariance of the autoregressive, within-time correlations and cross-lagged pathways among internalizing symptoms, oppositional defiance symptoms, and HED by comparing constrained and unconstrained pathways for each. Chi-square difference tests for comparisons of the unconstrained and constrained models revealed the following: autoregressive paths of internalizing and oppositional defiance symptoms were invariant over time (∆χ2 (12) = 10.63, P = 0.56). However, constrained and unconstrained autoregressive paths for HED differed significantly (∆χ2 (5) = 36.02, P < 0.001), suggesting they were not invariant over time (see Fig. 1). Within-time covariances between HED and internalizing symptoms were invariant across time (∆χ2 (6) = 4.71, P = 0.58). Models comparing constrained and unconstrained associations between oppositional defiance symptoms and HED and associations between oppositional defiance and internalizing symptoms differed significantly (∆χ2 (13) = 39.10, P < 0.001). All cross-lagged paths among constructs were invariant over time (∆χ2 (34) = 35.73, P = 0.39), suggesting that cross-lagged associations among constructs do not change with age. The final model with the appropriate time-invariance constraints on autoregressive paths, within-time covariances, and cross paths also fit the data reasonably well (χ2 (223) = 524.16, P < 0.05, RMSEA = 0.05, CFI = 0.91).
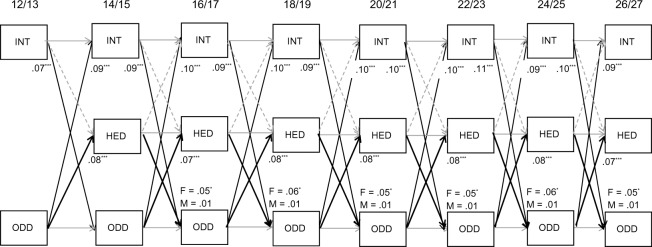
Figure 1.
Autoregressive paths and within-time covariances relating internalizing and oppositional defiant disorder symptoms to regular heavy episodic drinking.
Notes: N = 657, ***P < 0.001, **P < 0.01, *P < 0.05, †P = 0.06. Standardized estimates are shown. Cross-lagged paths estimated in this model are shown in Figure 2 to enhance the readability. Although many unstandardized estimates were constrained to be equal across time and sex, standardized estimates (shown in the figs.) can still be slightly different over time and sex. When coefficients differed between males and females, estimates were delineated with an “F” for female and an “M” for male, all other coefficients were constrained across sex.
Abbreviations: INT, internalizing; ODD, oppositional defiant disorder; HED, heavy episodic drinking.
Sex differences in the paths were also tested using a multiple group model. There was a significant difference (∆χ2 (77) = 212.44, P < 0.001) between the models in which all parameters were constrained across sex and a model in which parameters were unconstrained across sex, suggesting the presence of sex differences in the associations among parameters of interest. A series of constrained and unconstrained model comparisons were used to test for specific sex differences in autoregressive paths, within-time covariances, and cross-lagged paths. Findings revealed significant sex differences in (1) within-time covariances between internalizing symptoms and HED and oppositional defiance symptoms and HED and (2) cross-lagged paths between HED and subsequently levels of oppositional defiance. All remaining paths were invariant across sex (autoregressive paths: ∆χ2 (7) = 9.38, P = 0.23; within-time covariances: ∆χ2 (8) = 11.85, P = 0.16; cross-lagged paths: ∆χ2 (5) = 5.08, P = 0.41).
The final model was a multiple group model that included all relevant time and sex constraints (see Figs. 1 and 2). Model fit for this model was slightly less than adequate due to the reduction in power in the multiple group model (χ2 (545) = 993.16, P < 0.05, RMSEA = 0.05, CFI = 0.88). When data for ages from 12–13 to 26–27 years were removed (these are the ages with the lowest covariance coverage), fit improved (χ2 (333) = 589.73, P < 0.05, RMSEA = 0.05, CFI = 0.91), indicating that poor fit was a reflection of poor covariance coverage at the earliest and latest ages, rather than poor model fit. All data were retained for the final model. We present the standardized estimates for the autoregressive and within-time covariances in Figure 1 and the standardized estimates for the cross-lagged paths in Figure 2 to enhance the readability.
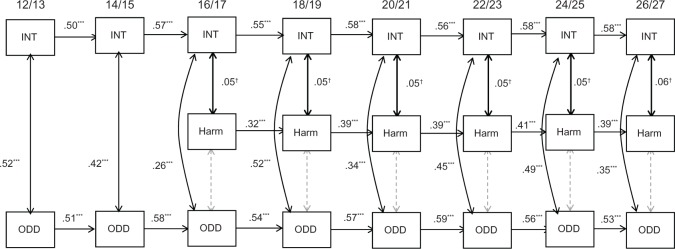
Figure 2.
Cross-lagged paths relating internalizing and oppositional defiance to regular heavy episodic drinking.
Notes: N = 657, ***P < 0.001, **P < 0.01, *P < 0.05, †P = 0.06. Standardized estimates are shown. Although many unstandardized estimates were constrained to be equal across time and sex, standardized estimates (shown in the figs.) can still be slightly different over time and sex. Dashed lines indicate nonsignificant cross-lagged paths. F, female; M, male; all other coefficients are constrained across sex.
Abbreviations: INT, internalizing; ODD, oppositional defiance; HED, heavy episodic drinking.
As shown in Figure 1, autoregressive paths were invariant for internalizing (standardized estimates range = 0.50–0.59) and oppositional defiance (standardized estimates range = 0.49–0.59) symptoms across each of the approximately two-year time lags between assessments and were constrained to equality across sex. HED increased in stability over time for males and females (range = 0.41–0.71). Within-time correlations between internalizing and oppositional defiance symptoms were significant at each time point for males and females at P < 0.001 and standardized coefficients ranged from 0.29 to 0.53. At each age, within-time correlations between internalizing symptoms and HED were marginally significant for females (range = 0.04–0.06, P = 0.06) but were not significant for males. Within-time correlations between oppositional defiance symptoms and HED were significant for females at ages 14–15, 16–17, and 20–21 years (range = 0.14–0.30) but were not significant for males at any age.
Cross-lagged paths from internalizing symptoms to HED and the reciprocal paths from HED to subsequent internalizing symptoms were not significant at any age for males and females (Fig. 2). However, oppositional defiance symptoms predicted increases in HED consistently at every age for both males and females, and the strength of this association was invariant across the two-year time lags (range = 0.07–0.08, P < 0.001) and across sex. Reciprocally, levels of HED also predicted significant increases in oppositional defiance symptoms but only for females (range = 0.05–0.06, P < 0.05).
As expected, the cross-lagged paths from internalizing symptoms to subsequent levels of oppositional defiance symptoms (range = 0.07–0.11, P < 0.001) and reciprocal paths from oppositional defiance to internalizing (range = 0.09–0.10, P < 0.001) symptoms were significant and invariant across the two-year time lags and sex.
Internalizing symptoms, oppositional defiance symptoms, and alcohol-related harms
The cross-lagged panel model examining the associations among internalizing symptoms, oppositional defiance symptoms, and alcohol harms had an adequate fit to the data (χ2 (156) = 439.35, P < 0.05, RMSEA = 0.05, CFI = 0.90). Chi-square difference tests for comparisons of the unconstrained and constrained models revealed the following: autoregressive paths for internalizing symptoms, oppositional defiance symptoms, and alcohol-related harms were all across time (∆χ2 (16) = 16.51, P = 0.42). Within-time covariances between alcohol-related harms and internalizing symptoms and alcohol-related harms and oppositional defiance symptoms were invariant across time (∆χ2 (10) = 8.68, P = 0.56). As previously shown in the HED model, within-time associations between oppositional defiance and internalizing symptoms varied in strength over time (∆χ2 (7) = 25.78, P < 0.001). Cross-lagged paths: as for the alcohol-related harms model, all cross-lagged paths among constructs were invariant over time (∆χ2 (26) = 33.90, P = 0.14), except for the paths from alcohol-related harms to subsequent internalizing symptoms (∆χ2 (4) = 9.38, P = 0.05). The model with the appropriate time-invariant constraints on autoregressive paths, within-time covariances, and cross-lagged paths fit the data reasonably well (χ2 (208) = 498.44, P < 0.05, RMSEA = 0.05, CFI = 0.90).
Sex differences in these paths were tested using a multiple group model, the model in which all parameters were constrained across sex fit as well as the unconstrained model (∆χ2 (56) = 40.32, P = 0.94), suggesting that there are no significant sex differences in any of the parameter estimates. Thus, the final model is presented for the total sample and included all relevant time invariant constraints (χ2 (227) = 516.70, P < 0.05, RMSEA = 0.04, CFI = 0.90). The standardized estimates for the autoregressive and within-time covariances for the alcohol-related harm model are shown in Figure 3 and the standardized estimates for the cross-lagged paths in Figure 4 to enhance the readability.
Figure 3.
Within-time covariances and autoregressives relating internalizing and oppositional defiance to alcohol-related harms.
Notes: N = 657, ***P < 0.001, **P < 0.01, *P < 0.05, †P = 0.06. Standardized estimates are shown. Although many unstandardized estimates were constrained to be equal across time, standardized estimates (shown in the figs.) can still be slightly different over time and sex. Cross-lagged paths estimated in this model are shown in Figure 4 to enhance the readability.
Abbreviations: INT, internalizing; ODD, oppositional defiant disorder; HARM, alcohol-related harms.
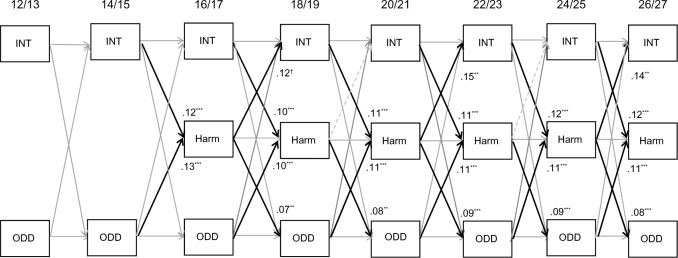
Figure 4.
Cross-lagged paths relating internalizing and oppositional defiant disorder symptoms to alcohol-related harms.
Notes: N = 657 ***P < 0.001, **P < 0.01, *P < 0.05, †P = 0.06. Standardized estimates are shown. Although many unstandardized estimates were constrained to be equal across time, standardized estimates (shown in the figs.) can still be slightly different over time and sex. Gray lines are significant, but coefficients for the cross-lagged paths between INT and ODD are same as in Figure 2 and are not shown here for readability.
Abbreviations: INT, internalizing; ODD, oppositional defiant disorder; HARM, alcohol-related harms.
Autoregressive paths were similar across each age group for internalizing (range = 0.50–0.58) and oppositional defiance symptoms (ranged from 0.51 to 0.59) and alcohol-related harms (range = 0.32–0.41), and thus, were constrained across each time lag. Within-time correlations between internalizing and oppositional defiance symptoms were significant at each time point at P < 0.001, standardized coefficients ranged from 0.26 to 0.52. Within-time correlations between internalizing symptoms and alcohol-related harms were marginally significant at each age (range = 0.05–0.06, P = 0.06). Within-time correlations between oppositional defiance symptoms and alcohol-related harms were nonsignificant at any age.
As shown in Figure 4, cross-lagged paths from internalizing symptoms to alcohol-related harms were significant across every two-year time lag (range = 0.10–0.12), and the strength of the association was invariant over time. The reciprocal paths from alcohol-related harms to subsequent internalizing symptoms were marginally significant at ages 16–17 to 18–19 years (P = 0.06), and significant at ages 20–21 to 22–23 years, and ages 24–25 to 26–27 years (range = 0.12–0.15). Oppositional defiance symptoms predicted increases in levels of alcohol-related harms across each two-year time lag (range = 0.10–0.13, P < 0.001), and the strength of the association was invariant over time. In turn, the levels of alcohol-related harms also predicted significant increases in oppositional defiance symptoms consistently across the two-year time lags (range = 0.07–0.09, P < 0.01). As in the HED model, the cross-lagged paths from internalizing symptoms to subsequent levels of oppositional defiance symptoms and reciprocal paths from oppositional defiance to internalizing symptoms were significant and stable across the two-year time lags. Coefficients are not presented again in Figure 4 to enhance the readability of Figure 4.
Discussion
Research examining associations between alcohol use and either internalizing or externalizing problems confirm their association6,11,33,34,45,46 but has rarely examined each in the context of the other or how these associations change over time. The current study examined the longitudinal, reciprocal relations between internalizing (symptoms of anxiety and depression) and externalizing (symptoms of oppositional defiance) symptoms and two early indicators of alcohol use problems (HED and alcohol-related harms) from adolescence to young adulthood (ages 12–27 years) in a community-based sample.
Consistent with the previous research with this age group, our findings showed that the onset of internalizing and oppositional defiance symptoms typically precedes the onset of HED and alcohol-related problems.6,11,32 While these findings support theories suggesting that psychopathology precipitates increases in substance use (ie, self-medication model), it is also possible that this temporal sequence is simply a function of maturational processes, whereby the psychopathology symptoms tend to manifest earlier in time than substance use47 or before increases in access to alcohol by late adolescence.
In addition, our results replicate the well-established finding that common externalizing symptoms are strong predictors of alcohol use disorders.33,45,47 Oppositional defiance symptoms were consistently related to increases in HED and alcohol-related harms across each age point for both males and females. HED (for females) and experiences of alcohol-related harms (for both males and females), in turn, predicted subsequent increases in oppositional defiance symptoms across all age points. As hypothesized, these findings suggest that HED and alcohol-related harms are both influenced by and contributed to externalizing behaviors, and this reciprocal association persists from adolescence into young adulthood.
The associations between internalizing symptoms and alcohol use are less consistent in the past research,6,29 and studies that have controlled for the comorbidity between internalizing and externalizing symptoms do not support the unique effects of internalizing symptoms.29,34 In the current study, internalizing symptoms had marginally significant within-time associations with HED (for females) and alcohol-related harms and also predicted significant increases in alcohol-related harms consistently across every age point, after controlling for externalizing symptoms. Alcohol-related harms, in turn, predicted further increases in internalizing symptoms across three of five age points. Overall, the findings suggest that both internalizing and externalizing symptoms have unique reciprocal associations with alcohol-related harms and, importantly, these bidirectional associations are stable across time. The results demonstrate developmentally cumulative and persistent interdependent associations between psychopathology and alcohol-related problems across a period of life when health behavior risks and symptoms of mental illness can become entrenched. We discuss the findings for HED and alcohol-related harms separately, indicating that these two concerns are only moderately correlated at each time point (range 0.22–0.37).
Heavy episodic drinking
The current findings showed stable but weak (P = 0.06) within-time associations between HED and internalizing symptoms at all age points, for females in particular. The proportion of females who endorsed HED at each time point was typically lower and more variable than the proportion of males. Indeed, >80% of males at each time point were coded as endorsing HED after ages 16–17 years, proving limited range for our analyses using proportion scores. There were no cross-lagged associations between internalizing symptoms and HED. This may reflect the co-occurring declines in both drinking and internalizing symptoms across the transition to adulthood.15,20,23,48 Previous studies with this sample showed that HED typically increases until the age of ~21 years and then subsequently declines.23 Moreover, males tended to have higher levels of HED and steeper increases in HED across adolescence compared to females. Paralleling this trend in drinking patterns, internalizing symptoms also increase across the transition to young adulthood and then subsequently begin to decline.15,20,23 The lack of associations across time may also reflect the episodic nature of internalizing symptoms. Alternatively, it may have been difficult to detect any unique cross-lagged effects of internalizing symptoms on HED in the presence of externalizing symptoms as well.
Previous research has also found stronger associations between internalizing symptoms and HED for females than males.8,24,30,32,49 There is a higher prevalence of depressive symptoms in females and less consistency in their HED compared to males. It may also be that females are more likely to drink to cope with internalizing symptoms than males or that males who are coping with internalizing symptoms may be more likely to withdraw from social contexts in which drinking occurs.24,49
HED and oppositional defiance symptoms were also associated within time until ages 20–21 years, for females, but not males. Nonsignificant associations at older ages may reflect the steep declines observed in oppositional defiance across the transition to adulthood, particularly for females compared to males, in other studies with this sample.15,20 Consistent with past research, externalizing symptoms predicted increases in HED for both males and females.32,34 However, the reciprocal effect from HED to increases in oppositional defiance symptoms was also seen for females, but not males. Dawson et al.49 showed that externalizing symptoms and alcohol use tend to be more common in males, whereas their association is greater among females.
Alcohol-related harms
In contrast to the results for HED, gender differences in the associations between internalizing and externalizing symptoms and alcohol-related harms were not significant. Oppositional defiance symptoms showed consistent reciprocal effects with alcohol-related harms over time after controlling for within-time associations and autoregressive paths. For the relations between alcohol-related harms and internalizing symptoms, the cross-lagged regressions were also significant at most ages: 16–17 to 18–19, 2–21 to 22–23, and 24–25 to 26–27 years. Overall, these findings add support for the mutual maintenance model in which both psychopathology and substance use serve to maintain or even exacerbate each other over time in a “vicious cycle.”6,47,50
Despite having only weak associations with HED itself, internalizing symptoms may lead to alcohol use problems because of high levels of coping expectancies and motives for drinking among youth who are also coping with internalizing symptoms. Expectations that drinking will aid coping and socialization may result in drinking at inappropriate times or locations, which could lead to problems or harm from their drinking even at low levels of use.37,43 Interpersonal skill deficits as a result of internalizing symptoms could also result in either withdrawal or drinking alone or alternatively, steer some youth away from mainstream peer associations toward more deviant peer groups that provide these socially awkward youth with peer acceptance.29 Alcohol-related harms may also create additional sources of stress for these youth, which fuel internalizing symptoms.51,52
Youth with externalizing pathology were also more likely to experience increases in alcohol-related harms. The strong associations of externalizing symptoms with both HED and harms suggest that the development of these concerns may occur within and be supported by a broader context of antisocial behavior.53 Externalizing problems can lead to HED and related problems by increased affiliation with deviant peers who provide opportunities and reinforcement for alcohol use.45 Oppositional defiance symptoms may also relate to difficulties conforming to legal or social prescriptions, leading to an increased likelihood of experiencing harm from drinking, independent of level of use. Excessive alcohol use may also reduce inhibitions and self-control and fuel other externalizing behaviors that more readily come to the attention of important adults in these youth’s networks.
Developmental variability in associations
As a result of age-related changes in social contexts and drinking behavior across the transition to adulthood, as well as changes in the presentation and prevalence of psychopathology, researchers have hypothesized that the etiological role of internalizing and externalizing symptoms for substance use may change across development.24,29 Yet, few studies have looked at these associations across multiple developmental periods. We did not find evidence of variability in the presence or strength of associations between psychopathology and alcohol outcomes from ages 12 to 27 years for HED and ages 16 to 27 years for alcohol-related harms, respectively. Rather, these associations were largely invariant across developmental age. Overall, the findings suggest that these risk processes are instead developmentally cumulative and that youth may become entrenched in an interdependent cycle that may significantly increase their risk of comorbid disorders in adulthood.
Strengths and limitations
The current study used a prospective longitudinal design, allowing us to examine the possible reciprocal relations of internalizing and externalizing symptoms with HED and alcohol-related harms at various stages of development. We used an economically diverse, randomly recruited, community-based sample, and we measured internalizing and externalizing symptoms rather than psychiatric disorders. Thus, our findings are generalizable to community-based samples of adolescents and young adults but may not be generalizable to clinical or high-risk samples. Moreover, our sample was primarily Caucasian and findings may not generalize to other ethnicities.
Our findings were similar when anxiety and depressive symptoms were assessed separately (results available from the authors). However, associations between alcohol use and a variety of specific other types of internalizing (ie, social anxiety and bipolar) and externalizing (ie, ADHD and conduct disorder) disorders were not examined here. Different types of psychopathology may also have different associations with substance use outcomes. For example, some types of internalizing disorders may act to protect against substance use (eg, separation anxiety), whereas others may increase risk (eg, social anxiety).6,8,54 Similarly, we did not test associations using other types of substance use (ie, marijuana and nicotine) and some research shows differential associations based on substance type.25 Future research using larger samples is needed to investigate these associations. We also did not test potential mechanisms that could explain the links observed between internalizing and externalizing symptoms and alcohol use outcomes, such as coping motives or affiliation with deviant peers, and this remains an important area for future research. Further, we did not include variables related to adult transition roles (eg, postsecondary institution and employment), which may influence associations.55 It is also possible that HED and alcohol-related harms fuel criticisms from important adults (parents, teachers, and work supervisors) and with peers and romantic relationships, which in turn can be perceive as unfair and responded to self-critical dysphoria and defiance.56
All our measures of psychopathology were self-reported. This may increase the strength of the correlations among constructs due to shared reporter variances; however, consistencies in the data over the period of 10 years cannot be attributed only to self-report. Further, the prevalence of drinking and psychopathology symptoms may be underestimated given concerns about social desirability. However, data collection procedures were designed to maximize the protection of privacy of youth’s responses. Moreover, the participants’ own reports of mental health symptoms and substance use may be more accurate over time than reports from parents or teachers, particularly as youth transition into adulthood and parents become less aware of ongoing problems.57 In addition, sex-specific thresholds of heavy drinking were unavailable; thus, rates of heavy drinking among females and the association with mental health symptoms may be underestimated. Finally, our cross-sequential design with cohorts spanning ages 12–27 years may only approximate a “true” picture of the patterns of change that might be found by following a single age group over time. However, research suggests that cross-sequential and true longitudinal design yield similar findings.58
Implications
The current study finds support for reciprocal longitudinal associations between subclinical levels of psychopathology and HED and alcohol-related harms, specifically, from adolescence through late young adulthood. Alcohol-related harms may represent more clinically and functionally significant impairments and, thus, be a stronger precursor for alcohol use disorders. Disruptions in interpersonal relationships, school, and work can be indicators of functional impairments indicative of disorder diagnoses.10 Given the persistent reciprocal relations observed here, early identification will be imperative for interrupting this cycle. Many youth present at emergency rooms as a result of over-consumption or injuries and other harms from drinking,59 providing salient opportunities for screening of mental health symptoms. Additional screening could help catch youth whose subclinical symptoms go unnoticed in other settings, possibility disrupting this vicious cycle and ultimately helping to prevent more serious concerns including alcohol-related deaths, injuries, and suicides. Similarly, for youth who seek medical assistance for mental health symptoms, screening for alcohol use could assist in their recovery. Many young people are unaware that their substance use can negatively impact their mental health or that the reciprocal effects of mental health on substance abuse are also likely. Motivational interviewing and personalizing feedback programs have shown significant promise for increasing self-awareness about the consequences of drinking for young people60 and a focus on helping youth to identify internalizing and externalizing symptoms that fuel their alcohol-related problems could improve these approaches.
Acknowledgments
The authors appreciate the generosity and dedication of our participants.
Footnotes
ACADEMIC EDITOR: Gregory Stuart, Editor in Chief
PEER REVIEW: Six peer reviewers contributed to the peer review report. Reviewers’ reports totaled 2140 words, excluding any confidential comments to the academic editor.
FUNDING: This research was supported by grants from the Canadian Institutes for Health Research (Grants 838-20000-075 and 935330 to BJL and Grant 79917 to Tim Stockwell). The authors confirm that the funder had no influence over the study design, content of the article, or selection of this journal.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Conceived and designed the experiments: KT, BL. Analyzed the data: KT. Wrote the first draft of the manuscript: KT, BL, MA. Contributed to the writing of the manuscript: KT, BL, MA. Agree with manuscript results and conclusions: KT, BL, MA. Jointly developed the structure and arguments for the paper: KT, BL. Made critical revisions and approved final version: KT, BL, MA. All authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Costello EJ, Copeland W, Angold A. Trends in psychopathology across the adolescent years: what changes when children become adolescents, and when adolescents become adults? J Child Psychol Psychiatry. 2011;52:1015–25. doi: 10.1111/j.1469-7610.2011.02446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61:807–16. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 3.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837–44. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization ’s World Mental Health Survey Initiative. World Psychiatry. 2007;6:168–76. [PMC free article] [PubMed] [Google Scholar]
- 5.Sterba SK, Copeland W, Egger H, Costello J, Erkanli A, Angold A. Longitudinal dimensionality of adolescent psychopathology: testing the differentiation hypothesis. J Child Psychol Psychiatry. 2010;51:871–84. doi: 10.1111/j.1469-7610.2010.02234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stewart SH, Grant VV, Mackie CJ, Conrod PJ. Comorbidity of anxiety and depression with substance use disorders. In: Sher KJ, editor. The Oxford Handbook of Substance Use Disorders. Vol. 2. New York: Oxford University Press; 2014. [Google Scholar]
- 7.Stone AL, Becker LG, Huber AM, Catalano RF. Review of risk and protective factors of substance abuse and problem use in emerging adulthood. Addict Behav. 2010;37:747–75. doi: 10.1016/j.addbeh.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 8.Storr CL, Pacek LR, Martins SS. Substance abuse disorders and adolescent psychopathology. Public Health Rev. 2010;34:1–42. [Google Scholar]
- 9.Arnett J. Emerging adulthood: the cultural psychology of a new life stage. In: Jensen L, editor. Bridging Cultural and Developmental Approaches to Psychology: New Syntheses in Theory, Research, and Policy. New York: Oxford University Press; 2011. pp. 255–75. [Google Scholar]
- 10.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 11.O’Neil KA, Conner BT, Kendall PC. Internalizing disorders and substance abuse disorders in youth: comorbidity, risk, temporal order, and implications for intervention. Clin Psychol Rev. 2011;31:104–12. doi: 10.1016/j.cpr.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Chan YF, Dennis ML, Funk RR. Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. J Subst Abuse Treat. 2008;34:14–24. doi: 10.1016/j.jsat.2006.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klein DN, Shankman SA, Lewinsohn PM, Seeley JR. Subthreshold depression in adolescents: predictors of escalation to full syndrome depressive disorders. J Am Acad Child Adolesc Psychiatry. 2009;48:703–10. doi: 10.1097/CHI.0b013e3181a56606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shankman S, Lewinsohn P, Klein D, Small J, Seeley J, Altman S. Subthreshold conditions as precursors for full syndrome disorders: a 15-year longitudinal study of multiple diagnostic classes. J Child Psychol Psychiatry. 2009;50:1485–94. doi: 10.1111/j.1469-7610.2009.02117.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leadbeater BJ, Homel J. Irritable and defiant sub-dimensions of odd: their stability and prediction of internalizing symptoms and conduct problems from adolescence to young adulthood. J Abnorm Child Psychol. 2015;43:407–21. doi: 10.1007/s10802-014-9908-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burke JD, Rowe R, Boylan K. Functional outcomes of child and adolescent ODD symptoms in young adult men. J Child Psychol Psychiatry. 2014;55:264–72. doi: 10.1111/jcpp.12150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stringaris A, Goodman R. Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. J Am Acad Child Adolesc Psychiatry. 2009;48:404–12. doi: 10.1097/CHI.0b013e3181984f30. [DOI] [PubMed] [Google Scholar]
- 18.Fanti KA, Henrich CC. Trajectories of pure and co-occurring internalizing and externalizing problems from age 2 to age 12: findings from the National Institute of Child Health and Human Development Study of Early Child Care. Dev Psychol. 2010;46:1159–75. doi: 10.1037/a0020659. [DOI] [PubMed] [Google Scholar]
- 19.Hale WW, Raaijmakers Q, Muris P, van Hoof A, Meeus W. Developmental trajectories of adolescent anxiety disorder symptoms: a 5-year prospective community study. J Am Acad Child Adolesc Psychiatry. 2008;47:556–64. doi: 10.1097/CHI.0b013e3181676583. [DOI] [PubMed] [Google Scholar]
- 20.Leadbeater BJ, Thompson K, Gruppuso V. Co-occurring trajectories of symptoms of anxiety, depression, and oppositional defiance from adolescence to young adulthood. J Clin Child Adolesc Psychol. 2012;41:719–30. doi: 10.1080/15374416.2012.694608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Oort FVA, Greaves-Lord K, Verhulst FC, Ormel J, Huizink AC. The developmental course of anxiety symptoms during adolescence: the TRAILS study. J Child Psychol Psychiatry. 2009;50:1209–17. doi: 10.1111/j.1469-7610.2009.02092.x. [DOI] [PubMed] [Google Scholar]
- 22.Maggs JL, Schulenberg JE. A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. J Stud Alcohol Drugs. 2002;14:54–70. doi: 10.15288/jsas.2002.s14.54. [DOI] [PubMed] [Google Scholar]
- 23.Thompson K, Stockwell T, Leadbeater B, Homel J. Association among different measures of alcohol use across adolescence and emerging adulthood. Addiction. 2014;109:894–903. doi: 10.1111/add.12499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Colder CR, Scalco M, Trucco EM, et al. Prospective associations of internalizing and externalizing problems and their co-occurrence with early adolescent substance use. J Abnorm Child Psychol. 2013;41:667–77. doi: 10.1007/s10802-012-9701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Farmer RF, Seeley JR, Kosty DB, et al. Internalizing and externalizing psychopathology as predictors of cannabis use disorder onset during adolescence and early adulthood. Psychol Addict Behav. 2015;29(3):541–51. doi: 10.1037/adb0000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jackson KM. Heavy episodic drinking: determining the predictive utility of five or more drinks. Psychol Addict Behav. 2008;22:68–77. doi: 10.1037/0893-164X.22.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Archie S, Kazemi AZ, Akhtar-Danesh N. Concurrent binge drinking and depression among Canadian youth: prevalence, patterns, and suicidality. Alcohol. 2012;46:165–72. doi: 10.1016/j.alcohol.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 28.Deas D. Adolescent substance use and psychiatric comorbidities. J Clin Psychiatry. 2006;67:18–23. [PubMed] [Google Scholar]
- 29.Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychol Addict Behav. 2011;25:390. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marmorstein NR. Longitudinal associations between alcohol problems and depressive symptoms: early adolescence through early adulthood. Alcohol Clin Exp Res. 2009;33:49–59. doi: 10.1111/j.1530-0277.2008.00810.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McKenzie M, Jorm AF, Romaniuk H, Olsson CA, Patton GC. Association of adolescent symptoms of depression and anxiety with alcohol use disorders in young adulthood: findings from the Victorian Adolescent Health Cohort Study. Med J Aust. 2011;195:S27–30. doi: 10.5694/j.1326-5377.2011.tb03262.x. [DOI] [PubMed] [Google Scholar]
- 32.Miettunen J, Murray GK, Jones PB, et al. Longitudinal associations between childhood and adulthood externalizing and internalizing psychopathology and adolescent substance use. Psychol Med. 2014;44:1727–38. doi: 10.1017/S0033291713002328. [DOI] [PubMed] [Google Scholar]
- 33.Pardini D, White HR, Stouthamer-Loeber M. Early adolescent psychopathology as a predictor of alcohol use disorders by young adult hood. Drug Alcohol Depend. 2008;88:S38–49. doi: 10.1016/j.drugalcdep.2006.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99:1548–59. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- 35.Albrecht AK, Galambos NL, Jansson SM. Adolescents’ internalizing and aggressive behaviors and perceptions of parents’ psychological control: a panel study examining direction of effects. J Youth Adolesc. 2007;26:673–84. [Google Scholar]
- 36.Evans-Polce RJ, Vasilenko SA, Lanza ST. Changes in gender and racial/ethnic disparities in rates of cigarette use, regular heavy episodic drinking, and marijuana use: ages 14 to 32. Addict Behav. 2014;41:218–22. doi: 10.1016/j.addbeh.2014.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hilton M. Drinking patterns and drinking problems in 1984: results from a general population survey. Alcohol Clin Exp Res. 1987;11:167–75. doi: 10.1111/j.1530-0277.1987.tb01283.x. [DOI] [PubMed] [Google Scholar]
- 38.Conrod PJ, Stewart SH, Comeau MN, Maclean M. Efficacy of cognitive behavioral interventions targeting personality risk factors for youth alcohol misuse. J Clin Child Adolesc Psychol. 2006;35:550–63. doi: 10.1207/s15374424jccp3504_6. [DOI] [PubMed] [Google Scholar]
- 39.Cunningham CE, Boyle MH, Hong S, Pettingill P, Bohaychuk D. The brief child and family phone interview (BCFPI) 1: rationale, development, and description of computerized children’s mental health intake and outcome assessment tool. J Child Psychol Psychiatry. 2009;50:416–23. doi: 10.1111/j.1469-7610.2008.01970.x. [DOI] [PubMed] [Google Scholar]
- 40.Patrick ME, Wightman P, Schoeni RF, Schulenberg JE. Socioeconomic status and substance use among young adults: a comparison across constructs and drugs. J Stud Alcohol Drugs. 2012;73:772–82. doi: 10.15288/jsad.2012.73.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ensminger ME, Fothergill KE. A decade of measuring SES: what it tells us and where to go from here. In: Bornstein MH, Bradley RH, editors. Socioeconomic Status, Parenting, and Child Development. New Jersey: Erlbaum; 2003. pp. 13–28. [Google Scholar]
- 42.Bollen KA, Curran PJ. Latent Curve Models: A Structural Equation Approach. Hoboken, NJ: Wiley; 2006. [Google Scholar]
- 43.Bentler PM, Mooijart A. Choice of structural model via parsimony: a rationale based on precision. Psychol Bull. 1989;106:315–7. doi: 10.1037/0033-2909.106.2.315. [DOI] [PubMed] [Google Scholar]
- 44.Muthén LK, Muthén BO. Mplus User’s Guide-Seventh Edition. Los Angeles, CA: Muthén & Muthén;; 1998–2012. [Google Scholar]
- 45.Dodge KA, Malone PS, Lansford JE, Miller S, Pettit GS, Bates JE. A dynamic cascade model of the development of substance-use onset. Monogr Soc Res Child Dev. 2009;74:vii–119. doi: 10.1111/j.1540-5834.2009.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zucker RA, Donovan JE, Masten AS, Mattson ME, Moss HB. Early developmental processes and the continuity of risk for underage drinking and problem drinking. Pediatrics. 2008;121:S252–72. doi: 10.1542/peds.2007-2243B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mackie CJ, Conrod PJ, Brady K. Current issues in the comorbid association between depression and substance use. In: Verster JC, Conrod PJ, Brady K, Galanter M, editors. Drug Abuse and Addiction in Medical Illness: Causes, Consequences, and Treatment. Totowa, NJ: Humana Press; 2012. pp. 275–84. [Google Scholar]
- 48.Leadbeater BJ, Thompson K, Sukhawathanakul P. It gets better or does it? Peer victimization and internalizing problems in the transition to young adulthood. Dev Psychopathol. 2014;26:675–88. doi: 10.1017/S0954579414000315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dawson DA, Goldstein RB, Moss HB, Li TK, Grant BF. Gender differences in the relationship of internalizing and externalizing psychopathology to alcohol dependence: likelihood, expression and course. Drug Alcohol Depend. 2010;112:9–17. doi: 10.1016/j.drugalcdep.2010.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stewart SH, Conrod PJ. Anxiety disorder and substance use disorder co-morbidity: common themes and future directions. In: Stewart SH, Conrod PJ, editors. Anxiety and Substance Use Disorders: The Vicious Cycle of Comorbidity. New York: Springer; 2008. pp. 239–57. [Google Scholar]
- 51.Stice E, Barrera M, Jr, Chassin L. Prospective differential prediction of adolescent alcohol use and problem use: examining mechanisms of effect. J Abnorm Psychol. 1998;107:616–28. doi: 10.1037//0021-843x.107.4.616. [DOI] [PubMed] [Google Scholar]
- 52.Sher KJ, Grekin ER. Alcohol and affect regulation. In: Gross J, editor. Handbook of Emotion Regulation. New York: Guilford Press; 2007. pp. 560–80. [Google Scholar]
- 53.Zucker RA, Heitzeg MM, Nigg JT. Parsing the undercontroldisinhibition pathway to substance use disorders: a multilevel developmental problem. Child Dev Perspect. 2011;5:248–55. doi: 10.1111/j.1750-8606.2011.00172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kushner MG, Krueger R, Frye B, Peterson J. Epidemiological perspectives on co-occurring anxiety disorder and substance use disorder. In: Stewart SH, Conrod PJ, editors. Anxiety and Substance Use Disorders: The Vicious Cycle of Comorbidity. New York: Springer; 2008. pp. 3–17. [Google Scholar]
- 55.Thompson K, Stockwell T, Leadbeater B, Homel J. The effect of types of post-secondary education on drinking: Does age of enrollment matter? Emerg Adulthood. 2015;3:154–65. doi: 10.1177/2167696814561999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Leadbeater BJ, Kuperminc GP, Blatt SJ, Hertzog C. A multivariate model of gender differences in adolescents’ internalizing and externalizing problems. Dev Psychol. 1999;35:1268–82. doi: 10.1037//0012-1649.35.5.1268. [DOI] [PubMed] [Google Scholar]
- 57.Bradford S, Rickwood D. Psychosocial assessments for young people: a systematic review examining acceptability, disclosure and engagement, and predictive utility. Adolesc Health Med Ther. 2012;3:111–25. doi: 10.2147/AHMT.S38442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Little T. Longitudinal Structural Equation Modeling. New York: Guilford Press; 2013. [Google Scholar]
- 59.Lea S, Black K, Asbridge M. An overview of injuries to adolescents and young adults related to substance use: data from Canadian emergency departments. CJEM. 2009;11:330–6. doi: 10.1017/s1481803500011374. [DOI] [PubMed] [Google Scholar]
- 60.Scott-Sheldon LA, Carey KB, Elliott JC, Garey L, Carey MP. Efficacy of alcohol interventions for first-year college students: a meta-analytic review of randomized controlled trials. J Consult Clin Psychol. 2014;82:177. doi: 10.1037/a0035192. [DOI] [PMC free article] [PubMed] [Google Scholar]