Abstract
Purpose
This study evaluated a culturally relevant, social cognitive theory–based, Internet-enhanced physical activity (PA) pilot intervention developed for overweight/obese African American (AA) female college students.
Design
Using a 3-month, single group, pretest–posttest design, participants accessed a culturally relevant PA promotion website and engaged in four moderate-intensity PA sessions each week.
Results
Study completers (n = 25, mean age = 21.9 years) reported a decrease in sedentary screen time (p < .0001); however, no changes in moderate-to-vigorous PA were reported (p = .150). A significant increase in self-regulation for PA (p < .0001) and marginally significant increases in social support (p = .052) and outcome expectations (p = .057) for PA were observed. No changes in body mass index (p = .162), PA enjoyment (p = .151), or exercise self-efficacy (p = .086) were reported.
Conclusions
Findings of this exploratory study show some preliminary support for Internet-enhanced approaches to promote PA among overweight/obese AA women.
Implications for Practice
Future studies with larger samples are needed to further explore culturally relevant Internet-enhanced PA programs in this underserved population.
Keywords: health disparities, women’s health, African American, Black, physical activity, college, exercise
Introduction
African American (AA) women are the least active demographic group in the United States with only 36% meeting the national physical activity (PA) recommendations (Centers for Disease Control and Prevention, 2010). This is of particular public health concern given AA women are disproportionally burdened by a myriad chronic diseases associated with insufficient PA levels (i.e., obesity, colon cancer, type II diabetes, and cardiovascular disease; U.S. Cancer Statistics Working Group, 2013). The low PA levels and disparate chronic disease burden among AA women highlights the need for innovative theory-based interventions to promote PA in this underserved population.
Researchers have used a variety of strategies to deliver culturally relevant PA promotion programs to AA women in recent years. Examples of these strategies include the following: mailed print materials (Pekmezi et al., 2013), print materials plus telephone counseling (Parra-Medina et al., 2011), face-to-face and/or group session counseling (Fitzgibbon et al., 2010; Rodriguez, Christopher, Johnson, Wang, & Foody, 2012; Stolley et al., 2009), faith-based programs (Peterson & Cheng, 2011; Whitt-Glover, Hogan, Lang, & Heil, 2008), and cable television programming (Risica, Gans, Kumanyika, Kirtania, & Lasater, 2013). Results of these approaches have varied with some researchers reporting favorable outcomes for increased PA (Pekmezi et al., 2013; Peterson & Cheng, 2011), while others have reported null or inconsistent findings according to the postintervention follow-up period (Fitzgibbon et al., 2010; Risica et al., 2013) or PA assessment method (Parra-Medina et al., 2011). The varied outcomes of these studies indicate the need for researchers to further explore strategies in which to intervene and promote PA in this underserved population.
One potential strategy that has received considerably less attention by researchers over the years is the use of Internet-based approaches to promote PA in AA women (Joseph, Durant, Benitez, & Pekmezi, 2014). In fact, to our knowledge, only two published studies (Joseph et al., 2013; Pekmezi et al., 2010) have evaluated Internet-based efforts promoting PA among AA women. The paucity of studies using the Internet to promote PA among AA women is particularly surprising given the high prevalence of Internet use in this population (Duggan & Smith, 2013; Pew Internet and American Life Project, 2013) and the established success of many previous Internet-based PA programs with predominately White populations (Davies, Spence, Vandelanotte, Caperchione, & Mummery, 2012; Joseph et al., 2014).
The first published study evaluating an Internet-based approach to promote PA among AA women was conducted by Pekmezi et al. (2010) and retrospectively evaluated the feasibility of an Internet-based PA intervention among a subset of middle-aged AA women enrolled in a larger randomized controlled trial (Marcus, Lewis, et al., 2007). AA women in this study reported increased PA levels and favorable outcomes for the feasibility and acceptability of the approach. The second published study, conducted by our research team (Joseph et al., 2013), evaluated a prospectively designed culturally relevant, Internet-enhanced intervention designed to promote PA among overweight and obese young adult AA women enrolled in college. Results of this 6-month pilot study showed a significant increase in PA at 3 months (p = .02); however, PA was attenuated by 6 months and was no longer different from baseline PA levels (p = .31). Significant increases in several psychosocial outcomes (including self-regulation for PA, p = .02; and social support for PA, p = .02) were also observed at 6 months.
The purpose of the current investigation was to extend our previous research on culturally relevant Internet-enhanced PA promotion efforts among young adult AA women by evaluating a 3-month Internet-enhanced intervention grounded in social cognitive theory (SCT) and designed to reduce screen time and promote moderate-to-vigorous intensity PA among overweight and obese AA female college students. In this article, we report the intervention’s effect on moderate-to-vigorous intensity PA, sedentary screen time, and select SCT variables. Findings from the current study add to the limited existing literature on Internet-enhanced approaches to promoting PA in overweight and obese young adult AA women.
Method
Study Design
A single group pretest–posttest research design was used to test the acceptability and feasibility of a culturally relevant Internet-enhanced PA intervention for overweight and obese young adult AA women. The study was powered to detect a meaningful improvement in minutes per week of moderate-to-vigorous of aerobic PA. Accordingly, based on a published review of Internet-based PA interventions at the time of study conception (van den Berg, Schoones, & Vliet Vlieland, 2007), we anticipated that participants would report a mean of 70 minutes per week of moderate-to-vigorous PA at baseline, and that PA would increase to 112 minutes per week by the end of the 3-month intervention (mean increase of 52 minutes per week, SD = 80). Based on these assumptions, we recruited a minimum sample size of 29 to achieve 80% power using a two-tailed paired t test with an alpha level of .05.
Intervention Description Overview: An Internet-Enhanced Physical Activity Program
Young women enrolled in the study agreed to participate in a minimum of four 30–60 minute moderate-intensity walking/exercise sessions per week for 3 months and use a culturally relevant Internet-based application as a PA monitoring and promotion tool. The study protocol was informed by our formative research with overweight and obese AA college females and is briefly described below.
Intervention Development
The study website and intervention protocol were developed through two formative phases. In Phase I, focus groups (n = 4) were conducted with the target population to identify features young overweight and obese AA women desire in a culturally relevant PA promotion web-site (Durant et al., 2014). Data collected were used to inform the development of the study website. In Phase II, a 6-week demonstration trial of the study protocol was conducted. In this phase, participants (n = 29) accessed the study website while concurrently attending alternating weeks of supervised moderate-intensity walking sessions (monitored by study staff) and “think aloud” (Ericsson & Simon, 1993) discussion group sessions. Data collected through the demonstration trial were used to identify and repair technical problems associated with the website.
Intervention Website
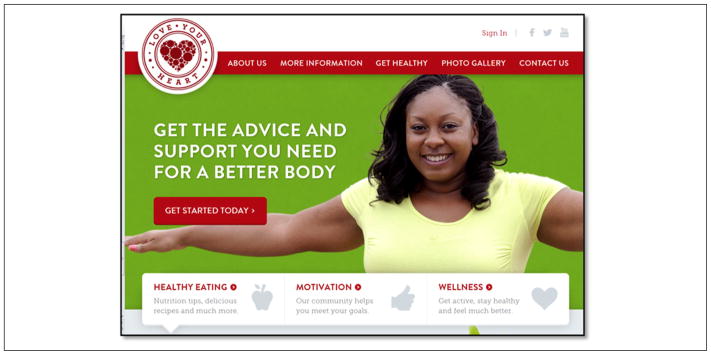
The final version of the website used in the current study (www.loveyourheartaha.com) contained features grounded in the constructs of the SCT (i.e., social support, self-regulation, self-efficacy, and outcome expectations) and provided culturally relevant information to facilitate PA among overweight and obese young adult AA women. The website was divided into a public site for all Internet users to access and a secure, private site that only participants could access. The public site contained the following features for the general public to view: (a) nutrition blog, (b) physician blog, (c) wellness blogs, (d) tips for natural hair care, and (e) a photo gallery.
Study participants logged into the secure, private site using a username and passcode via a link on the public site’s home page. The secure site included additional features to promote PA, including (a) personal profile page, (b) dietary tracking, (c) PA self-tracking/monitoring tools, (d) exercise demonstration videos, (e) online recipes, (f) blogs, and (g) message boards (see Table 1). The profile page allowed participants to create their own personal profiles where they could share photos and other personal information about themselves (similar to Facebook and other social networking sites).
Table 1.
Overview of the Application of the Social Cognitive Theory to Intervention Activities.
| Social cognitive theory construct | Component associated with the Internet-enhanced program |
|---|---|
| Self-efficacy | Social modeling and persuasion from participating with similar peers in the program (via supervised exercise sessions and website profiles) |
| Observational learning | Exercise Videos |
| Outcome expectations | Blog posts of young African American women providing personal testimonials on the benefits of being physical activity Videos of African American women performing physical activity |
| Self-regulation | Exercise tracker |
| Social support | Message boards and blogs discussing and encouraging performance of physical activity Wall posts where participants post messages promoting physical activity |
| Behavioral capability | Exercise plans Exercise videos Blogs |
Based on participant feedback from our formative research, three features were included on the study website to ensure cultural relevance: (a) images of AA women with diverse body types, (b) links to community-based PA groups for AA women, and (c) links to websites with guidance on natural hair care. The website was accessible via cellular phone using the website’s iPhone application, and the web-site could be viewed and operated on any cell phone via the mobile phone site. Table 1 depicts the study website features and how each feature maps to specific constructs of the SCT. Screenshots of the website are shown in Figures 1 and 2.
Figure 1.
Homepage of the Love Your Heart website.
Figure 2.
Blog post illustrating hair care tips.
Exercise Component
Participants were encouraged to engage in four moderate-intensity exercise sessions each week. Specifically, participants were asked to perform 30 to 60 minutes of at least moderate-intensity PA (defined as 50% to 70% of the maximum heart rate; Centers for Disease Control and Prevention, 2011) during each of the four weekly exercise sessions. For two of the weekly PA sessions, participants walked the indoor track of the university’s recreation center while being monitored by trained research assistants. For the other two sessions, participants had the option to walk on their own or participate in a cardiovascular-based group exercise class (i.e., Zumba, kick-boxing, aerobics, etc.). Participants wore pedometers and heart rate monitors to self-monitor their PA during all exercise sessions. Heart rate monitors were individually programmed to alert participants if their heart rates dropped below a moderate-intensity level.
Participants
Women enrolled in the study met the following inclusion criteria: (a) aged 19 to 30 years at time of study enrollment, (b) body mass index (BMI) greater than 25 kg/m2, (c) self-identified as AA, (d) enrolled as an undergraduate or graduate student at the university, and (e) absence of any self-reported medical conditions that would inhibit or limit performance of PA. Exclusion criteria included (a) concurrent participation in another PA, nutrition, or weight loss program (commercial or research); and (b) uncontrolled high blood pressure (defined as greater than 140/90).
Measures
Demographic Information
Demographic data were collected via a self-report questionnaire. This questionnaire has been used in previous research (Joseph et al., 2013) and assessed age, marital status, current education level, and parents’ education levels.
Physical Activity
The 7-Day Physical Activity Recall (7-Day PAR; Sallis et al., 1985) was the primary measure used to assess PA. This instrument assesses moderate-to-vigorous intensity PA performed in bouts of 10 minutes or greater over a previous 7-day period. The 7-Day PAR has demonstrated significant test–retest reliability estimates (r = .81, r = .99; Gross, Sallis, Buono, Roby, & Nelson, 1990; Sallis, Buono, Roby, Micale, & Nelson, 1993), has strong interrater reliability (r = .78) for assessments performed by multiple interviewers with the same subject (Sallis, Patterson, Buono, & Nader, 1988), and has been validated against more objective measures of PA, such as doubly labeled water (Washburn, Jacobsen, Sonko, Hill, & Donnelly, 2003) and accelerometers (Sloane, Snyder, Demark-Wahnefried, Lobach, & Kraus, 2009).
To corroborate self-report PA findings, participants were asked to wear an ActiGraph accelerometer (GT3X+ models) during all waking hours for a 7-day period at baseline and at the 6-month follow-up. This 7-day period precisely overlapped with the days assessed by the 7-Day PAR. Accelerometer data were prepared for analyses according to the protocol described by Troiano et al. (2008). Accordingly, to be considered as a valid assessment (and subsequently included in analyses), participants were required to wear the accelerometer for at least 10 hours per day for a minimum of 4 days during the 7-day assessment period. To corroborate data collected by the 7-Day PAR, only PA performed in bouts of 10 minutes or greater were included in analyses (known as a modified 10-minute bout; Troiano et al., 2008).
Sedentary Screen Time
Sedentary screen time was assessed with two items taken from a previously published sedentary behavior scale (Norman, Schmid, Sallis, Calfas, & Patrick, 2005). Participants were asked, “How much time on a typical day do you spend doing the following: (a) ‘Watching television (including videos on VCR/DVD)’; (b) ‘Playing computer or video games.’” Separate estimates were obtained for weekdays and weekends. This two-item measure has been used in previous research (Gibbs et al., 2013).
Social Cognitive Theory Variables
Self-efficacy for PA was assessed by the Exercise Confidence Survey (Sallis, Pinski, Grossman, Patterson, & Nader, 1988). This 12-item survey has previously established reliability and validity (Sallis, Pinski et al., 1988) and has demonstrated reliability estimates (Cronbach’s alpha) of .65 and .78 at baseline and 3 months, respectively, in the current study.
Social support for exercise was evaluated using the Social Support for Exercise Survey (Sallis, Grossman, Pinski, Patterson, & Nader, 1987). This scale provides two separate outcomes for social support, one in reference to family support (13 items) and the other in reference to support from friends (10 items). The Social Support for Exercise Scale has previously established validity (Sallis et al., 1987). In the current study, reliability estimates for the family subscale were 0.89 and 0.91 at baseline and 3 months; estimates for the friends subscale were 0.89 and 0.91.
Self-regulation for PA was assessed by the Self-Regulation Scale from the Health Beliefs Survey (Anderson, Winett, Wojcik, & Williams, 2010; Anderson, Wojcik, Winett, & Williams, 2006). This 10-item survey has been validated for use across various adult populations (Anderson et al., 2006; Anderson et al., 2010). In the current study, the Self-Regulation Scale demonstrated reliability estimates (Cronbach’s alpha) of .64 and .74 at baseline and 3 months, respectively.
The nine-item Outcome Expectation Scale for Exercise (Resnick, Zimmerman, Orwig, Furstenberg, & Magaziner, 2000) was used to assess outcome expectations for PA. This scale has been validated in AA populations (Resnick, Luisi, Vogel, & Junaleepa, 2004) and has demonstrated reliability estimates (Cronbach’s alpha) of .80 and .81 in the current study.
Enjoyment of PA was assessed using the PA Enjoyment Scale (Kendzierski & DeCarlo, 1991). This 18-item questionnaire has previously established validity (Kendzierski & DeCarlo, 1991) and has demonstrated internal consistency estimates of .86 and .92 in the current study.
Body Mass Index
BMI was calculated from measurements collected from a trained senior research staff member. To ensure consistency, the same staff member conducted measurements for BMI calculations for all study participants. Weights were measured to the nearest kilogram using a Scale-Tronix (Wheaton, IL) digital scale. Height was measured to the nearest inch using the Digi-kit stadiometer by Measurement Concepts and Quick Medical (North Bend, WA).
Website Usage
The website tracked participant activity and awarded “points” based on the amount of time spent on the website and the number and type of applications used. Thus, the more frequently participants logged onto the website and used the available applications, the higher number of points they accumulated during the study (Table 2 illustrates the website point algorithm).
Table 2.
Overview of Points Awarded to Participants for Website Utilization.
| Website activity | Assigned point value |
|---|---|
| Submitting workout on the activity tracker | 10 |
| Updating personal weight | 10 |
| Updating body measurements (waist, hips, thigh, etc.) | 2 |
| Updating personal profile status | 5 |
| Uploading a profile picture | 50 |
| Requesting to be friends with another user | 1 |
| Posting on another user’s wall | 2 |
| Commenting on another user’s wall post | 1 |
| Joining a group | 2 |
| Posting on a group’s wall | 2 |
| Posting on a challenge’s wall | 2 |
| Replying to a message board thread | 2 |
| Having other users reply to message board thread you created | 2 |
| Setting up a personal blog | 10 |
| Commenting on an exercise, workout plan, or diet plan | 2 |
Exercise Session Attendance
Exercise session attendance was documented on logs collected by staff weekly at the university recreation center. Logs contained (a) activity date, (b) activity type, (c) activity duration, (d) average heart rate, and (e) total pedometer steps. For supervised walking sessions at the university’s campus recreation center, study staff recorded participant attendance and verified information in the logs. For exercise sessions participants completed on their own, logs were completed independently by participants.
Feasibility and Acceptability
Feasibility and acceptability of the intervention were assessed using a 36-item consumer satisfaction measure adapted from previous research (Pekmezi et al., 2009; Pekmezi et al., 2012; Pekmezi et al., 2013) and were administered to participants at the conclusion of the study. This measure assessed participant satisfaction regarding the study website, exercise sessions, and study protocols. Sample questions include, “Overall, how helpful do you find the study website?” and “Would you recommend the study to a friend?”
Procedure
Participants were recruited via convenience sampling methods (i.e., flyers, recruitment tables at the university center, word-of-mouth) from the university campus during the Spring 2013 semester. Potential participants were screened for eligibility via telephone. Eligible participants were scheduled for their baseline study assessment.
Baseline assessment procedures required participants to attend two clinic visits approximately 1 week apart. At the initial baseline visit, informed consent was obtained; behavioral, psychosocial, and anthropometric data were collected; and blood draws were performed. Participants were also provided an accelerometer to wear during all waking hours for the next 7 days. One week following each participant’s initial visit, participants returned their accelerometer to study staff and completed the 7-Day PAR. The 3-month data collection procedures were similar to baseline.
Statistical Analysis
Normality of the data was assessed using box plots, histograms, and QQplots. Despite the small sample size, the majority of outcomes met assumptions for normality. Paired t tests were used to evaluate pre–post intervention changes for variables meeting normality assumptions. PA and sedentary screen time data did not meet normality assumptions and were accordingly analyzed using Wilcoxon signed rank tests. Complete case analysis was conducted using only data from participants (n = 25) who provided both baseline and the 3-month follow-up data. All data analyses were conducted using SAS version 9.3.
Results
Participant Characteristics
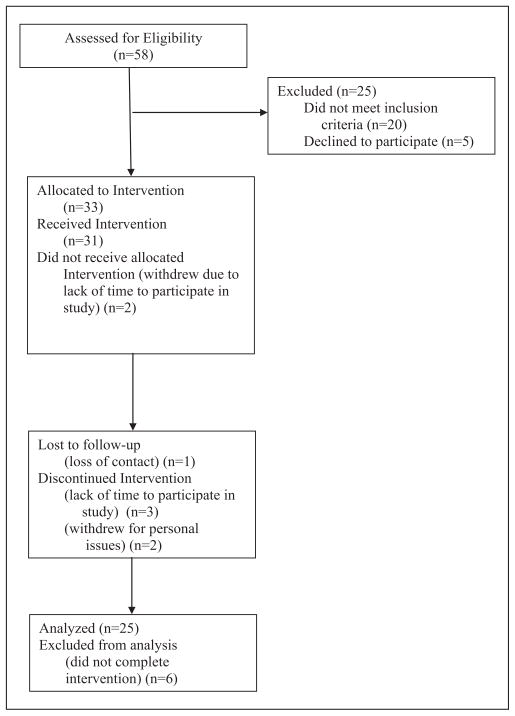
Figure 3 shows participant flow for the 3-month program. At baseline, participants (n = 31) had a mean age 21.3 years (SD = 3.1 years) and were mostly obese (mean BMI = 32.8 kg/m2, SD = 5.7; see Table 3). Twenty-five participants completed the 3-month follow-up assessment (81% retention). There were no differences in demographic characteristics (p < .05) among participants who completed the study versus those who did not complete the study.
Figure 3.
CONSORT diagram illustrating participant flow.
Table 3.
Demographic Characteristics of Participants at Baseline.
| Variable | Complete sample at baseline (N = 31)
|
Study completers (N = 25)
|
||
|---|---|---|---|---|
| M | SD | M | SD | |
| Age (years) | 21.3 | 3.2 | 21.9 | 3.3 |
| Body mass index | 33.8 | 5.7 | 32.9 | 6.0 |
| n | Percentage | n | Percentage | |
|---|---|---|---|---|
| African American | 31 | 100 | 25 | 100 |
| Marital status | ||||
| Never married | 29 | 93.5 | 23 | 92.0 |
| Single | 2 | 6.5 | 2 | 8.0 |
| Degree currently obtaining | ||||
| Undergraduate | 25 | 80.1 | 20 | 80.0 |
| Masters | 4 | 12.9 | 3 | 12.0 |
| PhD | 2 | 6.5 | 2 | 8.0 |
| Highest degree father obtained | ||||
| Less than high school | 0 | 0 | 0 | 0 |
| High school or GED | 11 | 34.4 | 11 | 44.0 |
| Associates degree | 5 | 16.1 | 5 | 20.0 |
| Bachelors degree | 6 | 19.4 | 2 | 8.0 |
| Masters degree | 5 | 16.1 | 5 | 20.0 |
| Doctorate | 0 | 0 | 0 | 0 |
| No answer | 4 | 12.9 | 2 | 8.0 |
| Highest degree mother obtained | ||||
| Less than high school | 2 | 6.5 | 1 | 4.0 |
| High school or GED | 10 | 32.3 | 9 | 36.0 |
| Associates degree | 3 | 9.7 | 3 | 12.0 |
| Bachelors degree | 6 | 19.4 | 2 | 8.0 |
| Masters degree | 7 | 22.6 | 7 | 28.0 |
| Doctorate | 3 | 9.7 | 3 | 12.0 |
| No answer | 0 | 0 | 0 | 0 |
Website Utilization and Exercise Session Adherence
Participants (n = 25) engaged in a mean of 64.9% (SD = 24.0%) of the recommended exercise sessions, which equates to participating in approximately 2.6 exercise sessions each week. Sixty-four percent (n = 16) of participants self-reported logging onto the study website at least one time per week. The median number of website points accumulated by participants over the 3-month study was 100 (range 0–1,039; M = 187.77, SD = 245.4).
Physical Activity
Correlation analyses showed that self-reported PA (measured by the 7-Day PAR) and accelerometer-measured PA were significantly correlated at baseline (Spearman’s ρ = .43, p = .03) but not at 3 months (Spearman’s ρ = .03, p = .92). Comparison of PA outcomes indicated that participants over-reported PA on the 7-Day PAR when compared with accelerometer data. No significant pre- and postintervention changes in moderate-to-vigorous PA were observed (7-Day PAR, p = .15; accelerometer p = .08). PA outcomes are presented in Table 4.
Table 4.
Physical Activity and Sedentary Behavior Outcomes (N = 25).
| Baseline
|
3 months
|
Baseline to 3-month change
|
|||
|---|---|---|---|---|---|
| M (SD) | Median (range) | M (SD) | Median (range) | Wilcoxon p | |
| 7-Day Physical Activity Recall (minutes/week) | 99.4 (103.8) | 80.0 (0–399) | 134.7 (119.5) | 100.0 (0–485) | .15 |
| Accelerometera (minutes/week) | 45.0 (51.6) | 22.0 (0–183) | 29.8 (37.28) | 12.0 (0–117) | .08 |
| Sedentary Behavior Weekday (hours/week) | 2.83 (1.9) | 3.0 (0–7) | 0.84 (0.87) | 0.5 (0–4) | <.0001 |
| Sedentary Behavior Weekend (hours/week) | 3.85 (1.63) | 4.0 (0.5–6) | 1.47 (1.17) | 1.0 (0–4) | <.0001 |
Only 17 participants provided valid accelerometer data and were included in accelerometer outcome analysis.
Sedentary Screen Time
At baseline, participants reported a median of 3 hours per day of sedentary screen time on a typical weekday and 4 hours per day on a typical weekend day. At 3 months, participants reported significantly lower sedentary screen time on both weekdays (Mdn = 5 hours/day, p < .0001) and weekend days (Mdn = 1 hour/day p < .0001; Table 4).
Social Cognitive Theory Outcomes
Table 5 shows pre–post intervention changes in SCT variables. Participants reported a significant increase in self-regulation for PA over the duration of the study (p = .0001). Trends for enhanced outcome expectations (p = .057), social support from family (p = .052), and social support from friends (p = .052) were also observed; however, improvements in these variables did not reach statistical significance. No changes in exercise self-efficacy (p = .086) or PA enjoyment (p = .150) were reported.
Table 5.
Pre–Post Intervention Changes for Social Cognitive Theory and BMI Outcomes.
| Social cognitive theory variables | Range | Baseline | 3 months | Baseline to 3-month change | p |
|---|---|---|---|---|---|
| Exercise self-efficacy | 1–5 | 3.95 (0.40) | 3.76 (0.55) | 0.19 (0.53) | .086 |
| Outcome expectations | 1–5 | 4.17 (0.46) | 4.31 (0.48) | 0.13 (0.35) | .057 |
| Self-regulation | 1–5 | 2.21 (0.65) | 2.88 (0.74) | 0.67 (0.66) | <.0001 |
| Social support from family | 0–60 | 48.12 (14.23) | 51.52 (16.12) | 3.40 (8.34) | .052 |
| Social support from friends | 0–60 | 48.12 (14.23) | 51.52 (16.12) | 3.40 (8.34) | .052 |
| Enjoyment | 1–7 | 5.33 (0.78) | 5.59 (1.04) | 0.25 (0.86) | .150 |
| Body mass index | 32.94 (6.02) | 32.65 (3.03) | 29 (1.01) | .162 |
Feasibility and Acceptability
Results from consumer satisfaction survey were favorable. Ninety-two percent of participants (n = 23) identified the study website as being “somewhat” to “very helpful” for promoting PA, and 76% reported gaining knowledge regarding PA from the website. In reference to the supervised exercise sessions, 84% (n = 20) of participants reported gaining knowledge associated with PA from participating in the exercise sessions, and 88% identified the exercise sessions as “somewhat” to “very helpful” for promoting PA. Lastly, all participants (n = 25) reported being “somewhat” to “very satisfied” with the study, and 76% (n = 20) said they would recommend the study to a friend.
Discussion
The aim of the current study was to evaluate a 3-month, culturally relevant Internet-enhanced intervention based on SCT and designed to reduce screen time and promote moderate-intensity PA among AA female college students. Study results show several positive outcomes; including a significant decrease in sedentary screen time, an increase in self-regulation for PA, and favorable consumer satisfaction outcomes for the acceptability and feasibility of the Internet-enhanced approach.
Participants reported a significant reduction in sedentary screen time from baseline to 3 months; however, improvements in moderate-to-vigorous PA at 3 months were not reported (p = .15). The lack of a significant increase in moderate-to-vigorous PA was somewhat surprising and may suggest that the intervention lacked components necessary to successfully promote increased PA, highlighting the need for researchers to further explore Internet-based strategies to motivate and increase PA among AA women. However, the nonsignificant PA outcomes may have been associated with the time period in which follow-up data were collected. The 3-month follow-up assessment was performed at the end of the semester during final exams. Study staff conducting the 7-Day PAR interviews reported that participants commonly identified end of semester coursework and final exams as interfering with their normal PA patterns. In future research, scientists should consider academic schedules when designing all intervention activities, including the timing of PA assessments, to ensure the integrity of study outcomes.
Comparison of self-reported and accelerometer-measured PA indicated that participants over self-reported their PA at both study assessment periods. Over self-reporting of PA is a commonly reported issue (LeBlanc & Janssen, 2010; Westerterp, 2009), and future studies should incorporate strategies to correct the overreporting of PA. One potential strategy could involve having participants exercise at a moderate-intensity level prior to completing a subjective PA assessment, which would provide a reference point for participants to appropriately estimate the intensity and duration of their PA.
Participants reported a significant increase in self-regulation for PA (p < .001) over the 3-month study and similar trends, although not statistically significant, for enhanced social support from family (p = .052), social support from friends (p = .052), and outcome expectations (p = .057) for PA. The significant increase in self-regulation mirrors the results of a previous Internet-enhanced approach to promoting PA among AA women (Joseph et al., 2013) and suggests that the website features targeting this construct (i.e., PA tracker) were successful in increasing self-regulatory processes associated with PA. Similarly, trends for enhanced social support were promising given the breadth of research suggesting that social support is a salient factor associated with PA engagement among AA women (Anderson et al., 2010; Fleury & Lee, 2006). The trend for increased social support from friends suggests that the message boards, blog posts, and social networking tools available on the study website may have promoted social support among participants. Moreover, enhanced social support from family was somewhat surprising given the intervention did not include a family-based component. Perhaps, participants shared their study experiences with family members and received encouragement/feedback to continue engaging in PA.
The lack of improvement for PA enjoyment was similar to the results observed in the previous culturally adapted, Internet-enhanced PA intervention for young adult AA women conducted by our research team (Joseph et al., 2013). However, our outcomes contrast with studies evaluating this construct in middle-aged and older AAs, which have shown significant improvements in enjoyment of PA over the duration of their respective interventions (Bopp et al., 2009; Papandonatos et al., 2012). Similarly, exercise self-efficacy did not significantly change from baseline to 3 months. This finding was unexpected given that participation in PA usually results in increased exercise self-efficacy; however, comparable results have been reported by other PA studies with AA women (Pekmezi et al., 2013; Thompson, Berry, & Hu, 2013; Zoellner et al., 2010). Perhaps, through attending the exercise sessions, participants realized that regular participation in moderate-to-vigorous PA was more difficult than they had anticipated, which resulted in the lack of change for this variable.
Adherence to the study’s recommended exercise sessions was also less than ideal; suggesting that this component of the intervention may not have been well received by participants. Overall, participants engaged in 65% of the recommended 4 exercise sessions each week; which equates to attending approximately 2.6 exercise sessions per week. Despite the modest engagement in these sessions, most participants reported gaining PA-related knowledge from the sessions (84%) and identified the sessions as “somewhat helpful” to “very helpful” for promoting PA (88%). These outcomes indicate that even though most participants reported gaining knowledge from the supervised exercise sessions, they did not enjoy them or had trouble attending them due to competing demands for their time. Adherence rates to the exercise sessions in our study are similar to findings of studies conducted by other researchers using similar exercise session protocols (Anton et al., 2011; Fitzgibbon et al., 2010; Joseph et al., 2013) and emphasize the need for researchers to further explore strategies to overcome barriers to PA in this underserved population. Potential strategies may include enhancing in-person group support components of the program (Ingram, Wilbur, McDevitt, & Buchholz, 2011), placing a greater emphasis on the physical and mental health benefits of PA (as opposed to focusing on weight loss; Harley, Odoms-Young, Beard, Katz, & Heaney, 2009; Pekmezi et al., 2013), incorporating family-based components (Wilcox et al., 2013), and further exploring the use of physically active AA women as role models (i.e., celebrities, community leaders) to promote PA (Harley et al., 2009; Ingram et al., 2011).
Findings from the consumer satisfaction survey were favorable and supported the acceptability and feasibility of the Internet-enhanced approach. For example, 80% of participants indicated that they would recommend the study to a friend, 92% identified the study as being “somewhat” to “very helpful” for promoting PA, and most (76%) reported learning new information associated with PA as a result of the program. Moreover, our attrition rate of 19% was slightly lower than the mean attrition found in a recent review of Internet-based PA interventions (22%; Joseph et al., 2014), further suggesting the feasibility of Internet-enhanced approaches to promote PA in young AA women.
Several study limitations must be noted. Participants were a convenience sample of university students, which limits generalizability of findings to AA women not enrolled in a university. Additionally, based on our a priori sample size calculation, we were underpowered to detect a significant improvement in moderate-to-vigorous of PA even if study completers (n = 25) achieved the anticipated 52-minutes per week increase in PA form baseline to 3 months. Other limitations include lack of a control group, small sample size, limited associated association between objective and self-reported measures of PA, and the method in which web-site usage was assessed. The point algorithm employed by the study website provided an approximate measure of website usage; however, more precise data (e.g., from analytic tracking software) would have been beneficial in evaluating website utilization.
Despite these limitations, the study has several strengths. This is one of few studies assessing a culturally relevant Internet-enhanced approach to promote PA in AA women. To our knowledge, only one other study (conducted by our research team) has explored a culturally relevant theory-based Internet-enhanced approach to promote PA among overweight and obese young adult AA women. Findings of the current study provide some preliminary support for the use of Internet-enhanced approaches to promote PA among overweight and obese young adult AA women while also highlighting potential limitations of this approach. Another strength of this work was the iterative, participant-informed process used to develop the study website. Incorporating participant feedback throughout study development helped ensure study activities met the needs and preferences of our target population.
This exploratory study is an important first step in understanding the potential role of technology to deliver culturally relevant PA programs to overweight and obese young adult AA women. Study findings suggest that an Internet-enhanced approach was associated with reducing screen time and enhancement of various PA-related SCT constructs (i.e., self-regulation, social support, and outcome expectations). The lack of a significant increase in moderate-to-vigorous intensity PA was unexpected and should be explored in future research. As technology continues to advance at a rapid pace, future studies should attempt to incorporate new and emerging technologies (i.e., text-messaging, smartphone applications, etc.) into Internet-enhanced PA promotion efforts.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the Robert Wood Johnson Foundation, American Heart Association, University of Alabama at Birmingham (UAB) Minority Health and Health Disparities Research Center, UAB Nutrition Obesity Research Center under Grant DK056336, and the UAB Center for Clinical and Translational Science under Grant UL1TR000165 from the National Center for Advancing Translational Sciences and National Center for Research Resources component of the National Institutes of Health. Research assistance for data analysis and manuscript development was supported by training funds from the National Institutes of Health/National Institute on Nursing Research, award T32 1T32NR012718-01—Transdisciplinary Training in Health Disparities Science (C. Keller, Principal Investigator).
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health or the National Institute on Nursing Research.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Anderson ES, Winett RA, Wojcik JR, Williams DM. Social cognitive mediators of change in a group randomized nutrition and physical activity intervention: Social support, self-efficacy, outcome expectations and self-regulation in the guide-to-health trial. Health Psychology. 2010;15:21–32. doi: 10.1177/1359105309342297. [DOI] [PubMed] [Google Scholar]
- Anderson ES, Wojcik JR, Winett RA, Williams DM. Social-cognitive determinants of physical activity: The influence of social support, self-efficacy, outcome expectations, and self-regulation among participants in a church-based health promotion study. Health Psychology. 2006;25:510–520. doi: 10.1037/0278-6133.25.4.510. [DOI] [PubMed] [Google Scholar]
- Anton SD, Manini TM, Milsom VA, Dubyak P, Cesari M, Cheng J, Perri MG. Effects of a weight loss plus exercise program on physical function in overweight, older women: A randomized controlled trial. Clinical Interventions in Aging. 2011;6:141–149. doi: 10.2147/cia.s17001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bopp M, Wilcox S, Laken M, Hooker SP, Parra-Medina D, Saunders R, McClorin L. 8 Steps to Fitness: A faith-based, behavior change physical activity intervention for African Americans. Journal of Physical Activity & Health. 2009;6:568–577. doi: 10.1123/jpah.6.5.568. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. US physical activity statistics. 2010 Retrieved from http://www.cdc.gov/physicalactivity/data/facts.html.
- Centers for Disease Control and Prevention. Target heart rate and estimated maximum heart rate. 2011 Retrieved from http://www.cdc.gov/physicalactivity/everyone/measuring/heartrate.html.
- Davies CA, Spence JC, Vandelanotte C, Caperchione CM, Mummery WK. Meta-analysis of internet-delivered interventions to increase physical activity levels. International Journal of Behavioral Nutrition and Physical Activity. 2012;9:52. doi: 10.1186/1479-5868-9-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan M, Smith A. Cell Internet use 2013. 2013 Retrieved from http://www.pewinternet.org/files/old-media/Files/Reports/2013/PIP_CellInternetUse2013.pdf.
- Durant N, Joseph R, Cherrington A, Cuffee Y, Knight B, Lewis D, Allison JJ. Recommendations for a culturally relevant internet-based tool to promote physical activity among overweight young African American women, Alabama, 2010–2011. Preventing Chronic Disease. 2014;11:130169. doi: 10.5888/pcd11.130169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ericsson K, Simon H. Protocol analysis: Verbal reports as data. Cambridge: MIT Press; 1993. [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Sharp LK, Singh V, Dyer A. Obesity Reduction Black Intervention Trial (ORBIT): 18-month results. Obesity. 2010;18:2317–2325. doi: 10.1038/oby.2010.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleury J, Lee SM. The social ecological model and physical activity in African American women. American Journal of Community Psychology. 2006;37:129–140. doi: 10.1007/s10464-005-9002-7. [DOI] [PubMed] [Google Scholar]
- Gibbs B, Reis J, Schelbert E, Craft L, Sidney S, Lima J, Lewis C. Sedentary screen time and left ventricular structures and function: The CARDIA study. Medicine & Science in Sports & Exercise. 2013;46:276–283. doi: 10.1249/MSS.0b013e3182a4df33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross LD, Sallis JF, Buono MJ, Roby JJ, Nelson JA. Reliability of interviewers using the Seven-Day Physical Activity Recall. Research Quarterly for Exercise and Sport. 1990;61:321–325. doi: 10.1080/02701367.1990.10607494. [DOI] [PubMed] [Google Scholar]
- Harley AE, Odoms-Young A, Beard B, Katz ML, Heaney CA. African American social and cultural contexts and physical activity: Strategies for navigating challenges to participation. Women & Health. 2009;49:84–100. doi: 10.1080/03630240802690861. [DOI] [PubMed] [Google Scholar]
- Ingram D, Wilbur J, McDevitt J, Buchholz S. Women’s walking program for African American women: Expectations and recommendations from participants as experts. Women & Health. 2011;51:566–582. doi: 10.1080/03630242.2011.606357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph RP, Durant NH, Benitez TB, Pekmezi DW. Internet-based physical activity interventions. American Journal of Lifestyle Medicine. 2014;8(1):42–67. doi: 10.1177/1559827613498059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph RP, Pekmezi DW, Lewis T, Dutton G, Turner LW, Durant NH. Physical activity and Social Cognitive Theory outcomes of an Internet-enhanced physical activity intervention for African American female college students. Journal of Health Disparities Research and Practice. 2013;6(2):18. [PMC free article] [PubMed] [Google Scholar]
- Kendzierski D, DeCarlo KJ. Physical Activity Enjoyment Scale: Two validation studies. Journal of Sport & Exercise Psychology. 1991;13:50–64. [Google Scholar]
- LeBlanc AG, Janssen I. Difference between self-reported and accelerometer measured moderate-to-vigorous physical activity in youth. Pediatric Exercise Science. 2010;22:523–534. doi: 10.1123/pes.22.4.523. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Lewis BA, Williams DM, Dunsiger S, Jakicic JM, Whiteley JA, Parisi AF. A comparison of Internet and print-based physical activity interventions. Archives of Internal Medicine. 2007;167:944–949. doi: 10.1001/archinte.167.9.944. [DOI] [PubMed] [Google Scholar]
- Norman GJ, Schmid BA, Sallis JF, Calfas KJ, Patrick K. Psychosocial and environmental correlates of adolescent sedentary behaviors. Pediatrics. 2005;116:908–916. doi: 10.1542/peds.2004-1814. [DOI] [PubMed] [Google Scholar]
- Papandonatos GD, Williams DM, Jennings EG, Napolitano MA, Bock BC, Dunsiger S, Marcus BH. Mediators of physical activity behavior change: Findings from a 12-month randomized controlled trial. Health Psychology. 2012;31:512–520. doi: 10.1037/a0026667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parra-Medina D, Wilcox S, Salinas J, Addy C, Fore E, Poston M, Wilson DK. Results of the Heart Healthy and Ethnically Relevant Lifestyle trial: A cardiovascular risk reduction intervention for African American women attending community health centers. American Journal of Public Health. 2011;101:1914–1921. doi: 10.2105/ajph.2011.300151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekmezi D, Dunsiger S, Gans K, Bock B, Gaskins R, Marquez B, Marcus B. Rationale, design, and baseline findings from Seamos Saludables: A randomized controlled trial testing the efficacy of a culturally and linguistically adapted, computer-tailored physical activity intervention for Latinas. Contemporary Clinical Trials. 2012;33:1261–1271. doi: 10.1016/j.cct.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekmezi D, Marcus B, Meneses K, Baskin ML, Ard JD, Martin MY, Demark-Wahnefried W. Developing an intervention to address physical activity barriers for African-American women in the deep South (USA) Women’s Health. 2013;9:301–312. doi: 10.2217/whe.13.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekmezi DW, Neighbors CJ, Lee CS, Gans KM, Bock BC, Morrow KM, Marcus BH. A culturally adapted physical activity intervention for Latinas: A randomized controlled trial. American Journal of Preventive Medicine. 2009;37:495–500. doi: 10.1016/j.amepre.2009.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekmezi DW, Williams DM, Dunsiger S, Jennings EG, Lewis BA, Jakicic JM, Marcus BH. Feasibility of using computer-tailored and internet-based interventions to promote physical activity in underserved populations. Telemedicine and eHealth. 2010;16(4):498–503. doi: 10.1089/tmj.2009.0135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson JA, Cheng AL. Heart and soul physical activity program for African American women. Western Journal of Nursing Research. 2011;33:652–670. doi: 10.1177/0193945910383706. [DOI] [PubMed] [Google Scholar]
- Pew Internet and American Life Project. Demographics of Internet users. 2013 Retrieved from http://pewinternet.org/Trend-Data-(Adults)/Whos-Online.aspx.
- Resnick B, Luisi D, Vogel A, Junaleepa P. Reliability and validity of the self-efficacy for exercise and outcome expectations for exercise scales with minority older adults. Journal of Nursing Measurement. 2004;12:235–247. doi: 10.1891/jnum.12.3.235. [DOI] [PubMed] [Google Scholar]
- Resnick B, Zimmerman SI, Orwig D, Furstenberg AL, Magaziner J. Outcome expectations for exercise scale: Utility and psychometrics. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2000;55:S352–S356. doi: 10.1093/geronb/55.6.s352. [DOI] [PubMed] [Google Scholar]
- Risica PM, Gans KM, Kumanyika S, Kirtania U, Lasater TM. SisterTalk: Final results of a culturally tailored cable television delivered weight control program for Black women. International Journal of Behavioral Nutrition and Physical Activity. 2013;10:141. doi: 10.1186/1479-5868-10-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez F, Christopher L, Johnson CE, Wang Y, Foody JM. Love your heart: A pilot community-based intervention to improve the cardiovascular health of African American women. Ethnicity & Disease. 2012;22:416–421. [PubMed] [Google Scholar]
- Sallis JF, Buono MJ, Roby JJ, Micale FG, Nelson JA. Seven-day recall and other physical activity self-reports in children and adolescents. Medicine & Science in Sport & Exercise. 1993;25:99–108. doi: 10.1249/00005768-199301000-00014. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Preventive Medicine. 1987;16:825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, Paffenbarger RS., Jr Physical activity assessment methodology in the Five-City Project. American Journal of Epidemiology. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Patterson TL, Buono MJ, Nader PR. Relation of cardiovascular fitness and physical activity to cardiovascular disease risk factors in children and adults. American Journal of Epidemiology. 1988;127:933–941. doi: 10.1093/oxfordjournals.aje.a114896. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Pinski RB, Grossman RM, Patterson TL, Nader PR. The development of self-efficacy scales for health-related diet and exercise behaviors. Health Education Research. 1988;3:283–292. [Google Scholar]
- Sloane R, Snyder DC, Demark-Wahnefried W, Lobach D, Kraus WE. Comparing the 7-day physical activity recall with a triaxial accelerometer for measuring time in exercise. Medicine & Science in Sport & Exercise. 2009;41:1334–1340. doi: 10.1249/MSS.0b013e3181984fa8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolley MR, Fitzgibbon ML, Schiffer L, Sharp LK, Singh V, Van Horn L, Dyer A. Obesity Reduction Black Intervention Trial (ORBIT): Six-month results. Obesity. 2009;17:100–106. doi: 10.1038/oby.2008.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson WM, Berry D, Hu J. A church-based intervention to change attitudes about physical activity among Black adolescent girls: A feasibility study. Public Health Nursing. 2013;30:221–230. doi: 10.1111/phn.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Medicine & Science in Sports & Exercise. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- U.S. Cancer Statistics Working Group. United States cancer statistics: 1999–2010 incidence and mortality data. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2013. Retrieved from http://apps.nccd.cdc.gov/uscs/ [Google Scholar]
- van den Berg MH, Schoones JW, Vliet Vlieland TP. Internet-based physical activity interventions: a systematic review of the literature. Journal of Medical Internet Research. 2007;9(3):e26. doi: 10.2196/jmir.9.3.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washburn RA, Jacobsen DJ, Sonko BJ, Hill JO, Donnelly JE. The validity of the Stanford Seven-Day Physical Activity Recall in young adults. Medicine & Science in Sports & Exercise. 2003;35:1374–1380. doi: 10.1249/01.mss.0000079081.08476.ea. [DOI] [PubMed] [Google Scholar]
- Westerterp KR. Assessment of physical activity: A critical appraisal. European Journal of Applied Physiology. 2009;105:823–828. doi: 10.1007/s00421-009-1000-2. [DOI] [PubMed] [Google Scholar]
- Whitt-Glover MC, Hogan PE, Lang W, Heil DP. Pilot study of a faith-based physical activity program among sedentary blacks. Preventing Chronic Disease. 2008;5(2):A51. [PMC free article] [PubMed] [Google Scholar]
- Wilcox S, Parrott A, Baruth M, Laken M, Condrasky M, Saunders R, Zimmerman L. The faith, activity, and nutrition program: A randomized controlled trial in African-American churches. American Journal of Preventive Medicine. 2013;44:122–131. doi: 10.1016/j.amepre.2012.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoellner J, Connell C, Powers A, Avis-Williams A, Yadrick K, Bogle ML. Does a six-month pedometer intervention improve physical activity and health among vulnerable African Americans? A feasibility study. Journal of Physical Activity & Health. 2010;7:224–231. doi: 10.1123/jpah.7.2.224. [DOI] [PubMed] [Google Scholar]