Abstract
Objective
Evaluate trajectories of type 1 diabetes health indicators from high school through the first year of college.
Participants
Seventy-four students with type 1 diabetes who maintained pediatric endocrinology care during the first year of college.
Methods
HbA1c, blood glucose monitoring frequency, BMI, and clinic attendance data were collected via retrospective medical chart review in spring, 2012. Group-based trajectory models evaluated diabetes-related health indicators over time and identified distinct growth trajectory groups.
Results
BMI increased and clinic attendance decreased in the first year of college. Trajectories for other health indicators were heterogeneous and stable over time; 69% of students were classified as having stable good glycemic control. Racial minority youth and youth on conventional insulin regimens were disproportionally represented in higher-risk groups.
Conclusions
Diabetes health indicators are stable or decline upon college entrance. Results signal the need for targeted support for college students with type 1 diabetes.
Diabetes affects 1 in 433 youth under age 20,1 and over 53,000 students with type 1 diabetes (T1DM) currently attend college across the U.S.2 T1DM management requires frequent blood glucose (BG) monitoring, insulin administration, and attention to diet, physical activity, and acute complications.3 Young adults are at increased risk for T1DM-related complications, and >80% of young adults with T1DM routinely fail to meet recommendations for glycemic control.4 Limited research suggests that clear trajectories of glycemic control first emerge by age 17 and are maintained or further diverge across early adulthood.5
Entering college is a seminal time when many young adults assume independent responsibility for T1DM management.6 However, changes in routine, decreased parental involvement, and increased exposure to risky behaviors during college may disrupt diabetes self-care and potentially set the stage for enduring health outcomes.7, 8 Prior research with young adults with T1DM has failed to disentangle developmental transitions, such as entering college, from the transfer from pediatric to adult care.9, 10 Yet research suggests that up to 50% of young adults remain in pediatric endocrinology care the first year after high school.9, 11 Evaluation of health indicators in rising college students with T1DM can direct prevention and intervention efforts of health care providers.
This study employed retrospective medical chart review to explore change in T1DM health indicators, including hemoglobin A1c (HbA1c), BG monitoring frequency, body mass index (BMI), and medical visit frequency, across the transition from high school to college for students maintaining T1DM care in a pediatric endocrinology practice. It was hypothesized that T1DM health indicators would remain stable or worsen during the first year of college.
Methods
Participants
Participants were 74 college students with T1DM receiving treatment at a mid-Atlantic pediatric diabetes center. The sample included young adults (53% male; 65% Caucasian) ages 17–20 years (M age upon entering college=18.6±.5) enrolled in higher education (65% in-state college; 35% out-of-state college). Most students were prescribed intensive insulin regimens (82%; e.g., multiple daily injections, pump therapy), which offer flexibility in insulin administration, versus conventional insulin regimens, which require a fixed number of insulin doses per day. Participants were diagnosed with T1DM for a mean of 9.0 years±4.0 years.
Procedures
This retrospective cohort study utilized medical chart review to identify patients with T1DM who were freshmen in college from 2007–2010, were seen in the pediatric setting for at least one year after entering college, and did not have another major medical condition (e.g. cystic fibrosis). A patient list was generated from the electronic medical record and clinic letters were reviewed to confirm a “transition point” (i.e., discrete move from high school to college) so that clinical data could be isolated for one year prior to one year following the identified transition point. The initial medical record extraction identified 178 patients; 75 were ineligible due to age, diagnosis, or lack of college attendance. Additionally, 17 patients had no visits during college and 12 patients had insufficient information to determine college status and/or health indicators, resulting in a final sample of 74 participants. Data were independently reviewed by two coders and de-identified to protect personal health information. This study was approved by the Institutional Review Board.
Sex, race, date of birth, diagnosis date, and insulin regimen were obtained for all participants via medical chart review. HbA1c, height/weight, and number of clinic visits over the two year period were collected from review of medical charts and physician-generated medical clinic letters. BG monitoring frequency (30 days) was collected from downloaded glucometer data or analysis of written BG data. The number of medical clinic visits one year pre- and post-college entrance was summed.
Analyses
Descriptive statistics were generated for all variables pre- and post-college entrance, including HbA1c, BG monitoring frequency, BMI, and clinic visit attendance. Correlational analyses (continuous variables, i.e. age) and chi square analyses (categorical variables, i.e. race) evaluated relations among demographic characteristics and T1DM indicators pre-college. Paired t-tests were used to investigate differences over time for HbA1c, BG frequency, BMI, and clinic attendance. Group-based trajectory models, using SAS Proc Traj procedure, were applied for longitudinal analysis on health outcome change over time; the unknown a priori trajectory groups of the T1DM indicators were identified and participants were classified into their most likely trajectory group.12, 13 Relations between group membership and individual characteristics were examined.
Results
Demographics and T1DM Health Indicators
Age at diagnosis was significantly correlated with pre-college HbA1c. Young adults diagnosed at older ages had better glycemic control. Intensive insulin regimens were associated with lower HbA1c and higher BG monitoring frequency. Caucasian students had lower HbA1c, higher BG monitoring frequency, and lower BMI than non-Caucasian students. No other significant differences were found for T1DM health indicators.
Change from Pre- to Post-College Entrance
Paired t-tests revealed a significant increase in BMI from pre-college (M=20.8±4.1) to post-college start (M=21.7±4.3; t=−2.29, p<.05, Cohen’s d=.27). The number of clinic visits decreased after starting college, with participants attending a mean of 3.2 medical visits (±0.8) the last year of high school vs. 2.2 medical visits (±0.8) the first year of college (t=9.14, p < .01, d=1.06). This difference was not related to college location, as in-state students (2.27 visits) attended a similar number of visits as out-of-state students (2.04 visits), (t=1.89, p=.24). There were no significant changes from pre- to post-college start for HbA1c or BG monitoring frequency.
Group-Based Trajectory Models
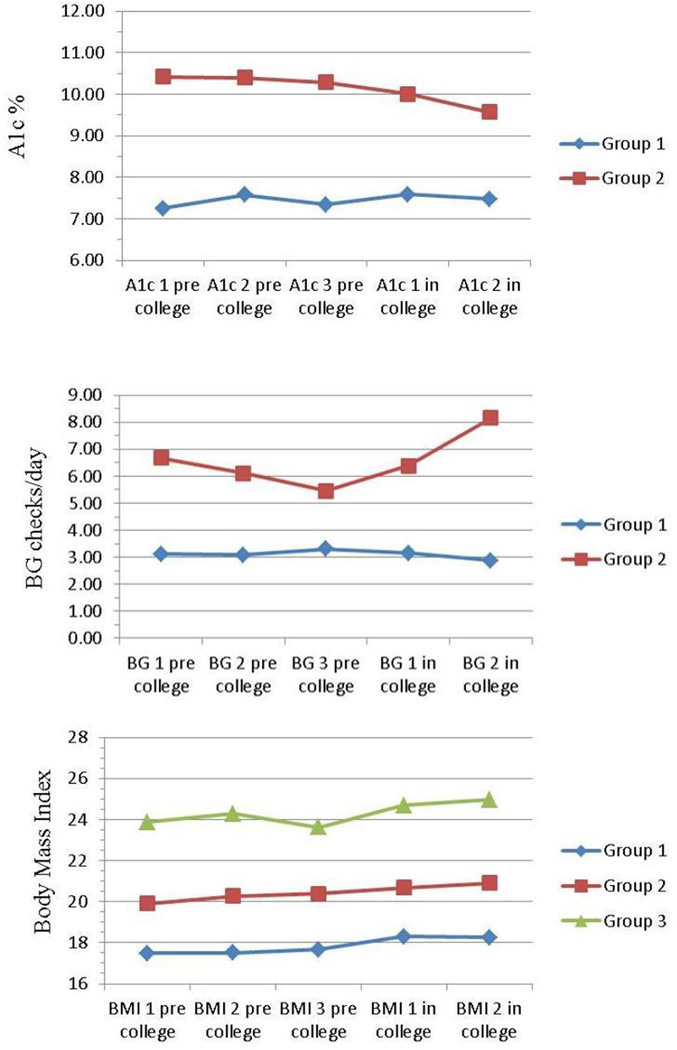
The goal of group-based trajectory models was to test possible heterogeneity of growth trajectories over the last year of high school and the first year of college. For each T1DM health indicator, several models with varying numbers of trajectory groups were implemented and model results were compared. Model selection was based on Bayesian Information Criterion (BIC); the smaller the BIC, the better the model fits the data. In addition, a minimum number of cases (n>5) per group was ensured. The model results show that the growth trajectories of HbA1c, BG monitoring frequency, and BMI were heterogeneous (Figure 1). Individuals were classified into specific groups based on their most likely class membership estimated from the Bayesian approach. Individuals are similar within group, but different across groups in regard to the corresponding growth trajectories.
Figure 1.
Group-based Trajectory Models for T1DM Health Indicators
For HbA1c, two distinct groups emerged. Sixty-nine percent of students fell in Group 1 (stable good glycemic control; baseline HbA1c=7.4%) and 31% of students were in group 2 (poor glycemic control; baseline HbA1c=10.5%). Model results indicate that change in HbA1c over time were not statistically significant in Group 1 (β=0.05, p=0.54) or Group 2 (β=−0.14, p=0.24). Students in the poor glycemic control group were more likely to be non-Caucasian and prescribed conventional insulin regimens (ps<.05). Similarly, two distinct groups for BG monitoring frequency emerged. Group 1 included 85% of students and represented stable low BG monitoring frequency (baseline BG monitoring frequency=3.2 checks/day). Group 2 included 15% of students with relatively high BG monitoring frequency (baseline BG monitoring frequency=6.2 checks/day). BG monitoring frequency did not change significantly over time in Groups 1 (β=−0.01, p=0.84) or 2 (β=0.35, p=0.07). There were no demographic differences when comparing groups.
Three distinct BMI groups emerged. Students were split among a low/average BMI group (Group 1; 32%; baseline BMI=17.5); an average BMI group (Group 2; 43%; baseline BMI=20.3); and a high/average BMI group (Group 3; 25%; baseline BMI=24.1). BMI significantly increased over time in Groups 1 (β =0.22, p=0.04) and 2 (β=0.24, p=0.01). The change in BMI for Group 3 was not statistically significant (β=0.23, p=0.05) but was variable over time. Students in the high/average BMI group were more likely to be non-Caucasian and prescribed conventional insulin regimens (ps<.05).
Comment
This study prospectively evaluates change in T1DM health indicators across the first year of college. Data were drawn from chart review and are representative of a population of rising college students in a large pediatric diabetes practice. Trajectories of T1DM health indicators did not significantly change over the first year of college and group membership was maintained. Surprisingly, 69% of students demonstrated stable good glycemic control and the mean baseline HbA1c for this group was below recommendations for youth <19 years (HbA1c≤7.5%).14 Maintaining care in a pediatric practice may be protective during the first year of college, as other studies have demonstrated early transition to adult care is associated with poorer glycemic control.9 Conversely, college students may also be better equipped to manage diabetes due to other factors (e.g. executive functioning). The majority of students (85%) were in a group checking BG levels less than 4×/day, suggesting that students did not increase BG monitoring frequency to adapt to changing schedules. Patterns of glycemic control and BG monitoring frequency are likely stable by early young adulthood.5, 15
BMI increased in college and students who entered college with a higher BMI experienced more BMI variability. Although none of the BMI trajectories indicated overweight, the average student gains 3.86 pounds during freshman year,16 and weight gain may have health consequences for students with T1DM in later years. Paradoxically, weight gain is sometimes observed when glycemic control improves;17 however, in this sample, glycemic control was maintained as BMI increased, suggesting that other factors like declining physical activity may be driving this change.18 The first year of college – or earlier – may be a critical period for intervention to prevent further weight gain.19
Non-Caucasian race and conventional insulin regimens were associated with representation in subgroups of poor glycemic control and higher BMI. Racial minority status is a known risk factor for poor glycemic control,15 and minority students may particularly benefit from integrated interventions to promote T1DM health in college. Only 18% of the total sample utilized conventional insulin regimens, but these regimens likely do not offer the flexibility needed for college students. Intensive insulin regimens should be considered for this group.20
Mean clinic attendance decreased by 1 visit from high school to college. Declines in clinic attendance are typically observed in young adulthood and are often ascribed to disjointed transition from pediatric to adult medical care.21 Competing life events and developmental milestones, such as entering college, also contribute to decreased clinic attendance, particularly as college location did not influence attendance. Maintaining a consistent source of endocrinology care during the college transition is important,9 and college students should engage local endocrinology services to maintain adequate medical supervision during this potentially risky period. Increased flexibility to meet the needs of college students with chronic conditions, such as evening and walk-in appointments, electronic health portals, and telemedicine, may improve access to medical care. T1DM student groups exist on many college campuses and also can provide support. The College Diabetes Network (https://collegediabetesnetwork.org/) is a national organization dedicated to promoting adjustment for college students, and over 75 local chapters offer resources, peer support, and targeted events.
Limitations
This study utilized medical chart data from one pediatric diabetes practice. Participants were excluded if college attendance and maintenance of pediatric T1DM care could not be confirmed from medical records. While the use of retrospective chart data eliminates some of the recruitment bias found with research volunteers,22 some youth may have been excluded for insufficient documentation. Data could not discriminate among students who transferred to adult care versus those with no medical visits during the first year of college, and neither group were included in analyses. Information about health care utilization with other providers and other factors potentially associated with T1DM outcomes (e.g. income) was not available. Future research should consider prospective enrollment prior to college entrance to track key health indicators in college students with T1DM and obtain more specific information on T1DM self-care and health care utilization.
Conclusion
College students with T1DM are at increased risk for weight gain, and disengagement from routine endocrinology care may occur during the first year of college. College-based health care providers and advocacy groups are uniquely poised to meet the needs of this group and can proactively identify on- and off-campus health-related services to promote T1DM self-care. Glycemic control and BG monitoring patterns are relatively stable, suggesting that students with suboptimal health behaviors may require increased support to improve T1DM self-care. The first year of college may represent a critical point to intervene to promote healthy diabetes care.19
Acknowledgments
Dr. Monaghan is supported by NIH K23DK099250. This work was also supported by the Clinical and Translational Science Institute at Children’s National (CTSI-CN) and the NIH National Center for Advancing Translational Sciences (UL1TR000075; KL2TR000076). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
References
- 1.Pettitt D, Talton J, Dabelea D, et al. Prevalence of diabetes in U.S. youth in 2009: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2014;37(2):402–408. doi: 10.2337/dc13-1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roth C. Supporting young adults with diabetes: changing systems to address the issues. American Association for Diabetes Educators 2014 Annual Meeting & Exhibition; August, 2014; Orlando, FL. [Google Scholar]
- 3.American Diabetes Association. Standards of medical care in diabetes-2013. Diabetes Care. 2013;36(1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peters A, Laffel L The American Diabetes Association Transitions Working Group. Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems. Diabetes Care. 2011;34:2477–2485. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luyckx K, Seiffge-Krenke I. Continuity and change in glycemic control trajectories from adolescence to emerging adulthood: relationships with family climate and self-concept in type 1 diabetes. Diabetes Care. 2009;32(5):797–801. doi: 10.2337/dc08-1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hanna KM, Weaver MT, Stump TE, et al. Initial findings: primary diabetes care responsibility among emerging adults with type 1 diabetes post high school and move out of parental home. Child Care Health Dev. 2013;39(1):61–68. doi: 10.1111/j.1365-2214.2011.01320.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanna KM, Stupiansky N, Weaver M, Slaven J, Stump T. Alcohol use trajectories after high school graduation among emerging adults with type 1 diabetes. J Adolesc Health. 2014;55(2):201–208. doi: 10.1016/j.jadohealth.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramchandani N, Cantey-Kiser J, Alter C, et al. Self-reported factors that affect glycemic control in college students with type 1 diabetes. Diabetes Educ. 2000:656–666. doi: 10.1177/014572170002600413. [DOI] [PubMed] [Google Scholar]
- 9.Helgeson VS, Reynolds KA, Snyder PR, et al. Characterizing the transition from paediatric to adult care among emerging adults with type 1 diabetes. Diabet Med. 2013;30(5):610–615. doi: 10.1111/dme.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weissberg-Benchell J, Wolpert H, Anderson B. Transitioning from pediatric to adult care: a new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care. 2007;30(10):2441–2446. doi: 10.2337/dc07-1249. [DOI] [PubMed] [Google Scholar]
- 11.Lotstein DS, Seid M, Klingensmith G, et al. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatr. 2013;131(4):e1062–e1070. doi: 10.1542/peds.2012-1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones B, Nagin D, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29:374–393. [Google Scholar]
- 13.Nagin D. Group-Based Modeling of Development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 14.Chiang JL, Kirkman MS, Laffel LMB, Peters AL. Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes Care. 2014;37(7):2034–2054. doi: 10.2337/dc14-1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hilliard ME, Wu YP, Rausch J, Dolan LM, Hood KK. Predictors of deteriorations in diabetes management and control in adolescents with type 1 diabetes. J Adolesc Health. 2013;52:28–34. doi: 10.1016/j.jadohealth.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vella-Zarb RA, Elgar FJ. The 'Freshman 5': A meta-analysis of weight gain in the freshman year of college. J Am Coll Health. 2010;58(2):161–166. doi: 10.1080/07448480903221392. [DOI] [PubMed] [Google Scholar]
- 17.Nansel T, Lipsky L, Iannotti R. Cross-sectional and longitudinal relationships of body mass index with glycemic control in children and adolescents with type 1 diabetes mellitus. Diabetes Res Clin Pract. 2013;100(1):126–132. doi: 10.1016/j.diabres.2012.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Laska MN, Pasch KE, Lust K, Story M, Ehlinger E. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prev Sci. 2009;10:376–386. doi: 10.1007/s11121-009-0140-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nelson M, Story M, Larson N, Neumark-Sztainer D, Lytle L. Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obes. 2008;16(10):2205–2211. doi: 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- 20.Hendricks M, Monaghan M, Soutor S, Chen R, Holmes CS. A profile of self-care behaviors in emerging adults with type 1 diabetes. Diabetes Educ. 2013;39(2):195–203. doi: 10.1177/0145721713475840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hynes L, Byrne M, Dinneen SF, McGuire BE, O'Donnell M, Mc Sharry J. Barriers and facilitators associated with attendance at hospital diabetes clinics among young adults (15–30 years) with type 1 diabetes mellitus: a systematic review. Pediatr Diabetes. 2014 doi: 10.1111/pedi.12198. [DOI] [PubMed] [Google Scholar]
- 22.Whittemore R, Jaser S, Faulkner M, et al. Type 1 diabetes eHealth psychoeducation: youth recruitment, participation, and satisfaction. J Med Internet Res. 2013;15(1):e15. doi: 10.2196/jmir.2170. [DOI] [PMC free article] [PubMed] [Google Scholar]