INTRODUCTION
Esophageal hematomas develop from the dissection of the mucosa from the mu scular layers of the esophageal wall and represent an uncommon condition affecting all ages[1-3]. Although the most common cause of esophageal hematomas is iatrogenic mechanical injury-induced by prolonged nasogastric intubation, difficult or forceful endoscopic intubation, or the result of variceal injection sclerotherapy-some may be spontaneous, particularly in patients receiving anticoagulants[3-6]. Presenting symptoms most commonly include dysphagia, hematemesis, and sub-sternal or epigastric pain[5,9].
In this report, we present four cases of esophageal hematomas diagnosed endoscopically, describe their clinical and endoscopic characteristics and propose a classification. As our cases exemplify, therapy is conservative and a favorable prognosis is the rule. Although the diagnosis has traditionally been made by barium esophagography[1] or CAT scanning[1,10], the increased use of endoscopy will allow increased recognition of esophageal hematomas even at a subclinical (asymptomatic) stage and ultimately lead to a better understanding of their etiopathogenesis and their prevention.
CASE REPORTS
Case 1 A 90-year-old man with a history of hypertension, con gestive heart failure, and mild aortic stenosis was refered for upper endoscopy to determine the cause of iron deficiency anemia. A colonoscopy had previously revealed diver ticular disease. Laboratory values included a hematocrit of 30%, iron of 90 mg/L and a TIBC of 358. Coagulation studies were normal. Endoscopy revealed salmon-colored mucosa extending from 28 cm-34 cm from the incisors, consistent with Barrett’s esophagus. A densely red, elevated lesion, consistent with a hematoma was noted at 19 cm (Figure 1A). No therapy was given. A follow-up endoscopy, performed one week later, showed complete resolution of the hematoma. Because of its location, the hematoma was attributed to a difficult, possibly traumatic, endoscopic intubation.
Figure 1.
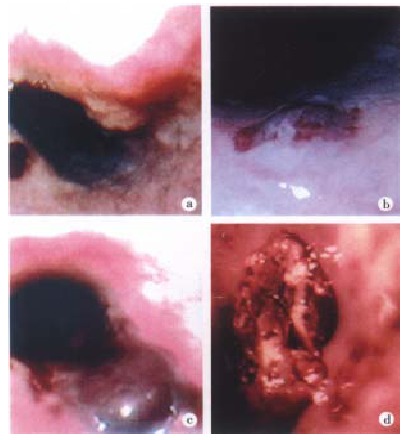
Endoscopic appearance of esophageal hematom as. a: Stage I esophageal hematoma. There is no surrounding edema. Patient was asymptomatic; b. Stage II esophageal hematoma after an esophageal biopsy. Note the surrounding tissue edema; c. Stage III hematoma induced by esopha geal dilation of a stricture. There is edema and separation of the surface mucosal layer that is partially obliterating the lumen. Patient was asymptomatic; d. Stage IV esophageal hematoma related to recent transesophageal echocardiography. Edema and clot formation led to complete obliteration of the esophageal lumen and hematemesis.
Case 2 A 59-year-old man was referred for upper endoscopy because of chronic reflux symptoms. His medications included omeprazole 20 mg po-daily, and aspirin 325 mg po-daily. Endoscopy revealed confluent esophageal erosions and ulcers consistent with Savary stage III esophagitis from 36 cm-33 cm. Upon biopsy of the esophagus, a purple-red, elevated lesion, consistent with a hematoma was noted at 35 cm (Figure 1B). Histologic examination of the biopsy sample revealed changes consistent with ref lux esophagitis. The hematoma was attributed to the mucosal biopsy obtained in the context of aspirin intake.
Case 3 A 90-year-old man with solid food dysphagia was refered for esophageal dilation. He had a history of metastatic (stage 4) squamous esophageal cancer treated with radiation therapy and esophageal dilation. He had mild anemia, but no thrombocytopenia or coagulation abnormalities. Endoscopy revealed a mid-esophageal stricture at 5 cm-29 cm which was dilated with minimal resistance using Savary dilators over a guide wire. This resulted in a 1 cm-long submucosal hematoma at 26 cm (Figure 1c). No biopsy was obtained. Because the patient’s dysphagia resolved, there was no follow-up endoscopy.
Case 4 A 51-year-old male with a history of rheumatic heart disease, status post aortic valve replacement, was hospitalized for mitral valve replacement. Because his postoperative course was complicated by enterococcal sepsis, a transesophageal echocardiogram was performed which excluded the presence of endocarditis. The following day, hematemesis was noted. Coagulation parameters were within the expected therapeutic range for prosthetic valves. An emergency upper endoscopy revealed a 3 cm-long, dark red esophageal mass at the GE junction, completely obliterating the esophageal lumen (Figure 1D). Biopsies obtained from the surface of the mass revealed organized clot and acute esophageal mucosal inflammation (not shown). Broad spectrum antibiotics and H2 receptor antagonists were administered intravenously; effective anticoagul-ation was also continued. Although there was no more evidence of gastrointestinal hemorrhage, the patient eventually succumbed to sepsis ten days later. Autopsy revealed severe herpetic tracheobronchitis without any evidence of esophageal injury.
DISCUSSION
Esophageal hematomas appear as raised purplish-red lesions, mostly sub-mucosal in location, but occasionally obliterating the esophageal lumen. Depending on their etiology, they may be classified as spontaneous or traumatic. Based on the above observations, we propose that esophageal hematomas can be further classified according to the degree of involvement of the lumen in four stages (Table 1). Esophageal hematoma formation[11,12], is an uncommon condition in which an intramural hemorrhage leads to a variable degree of submucosal dissection of the esophageal wall ranging from single or multiple localized he matomas to complete dissection of the esophagus[1]. Esophageal hematomas may be spontaneous, associated with sudden changes in the transmural wall pressures due to a variety of causes including coughing, retching or protracted vomiting[13], or may result from iatrogenic instrumentation, such as esophageal variceal sclerotherapy[3,14,15] or transesophageal ultrasonography[6] (Table 2). Hematomas may also be associated with direct trauma from abrasive foodstuffs such as taco shells[16], pill-induced esophageal injury[17], or with a coagulopathy, with little or no history of esophageal barotrauma[5]. Other probable causes include esophageals tricture, diverticulum, esophageal arteriovenous malformation, and aspirin use[18]. The majority of patients with esophageal hematomas are older than 70 year, although isolated reports of patients as young as 21 year have been made. In some studies, there seems to be a predilection for the female gender[1].
Table 1.
Stages of esophageal hematomas
| I: Hematoma without surrounding tissue edema |
| II: Hematoma with surrounding tissue edema |
| III: Hematoma with edema plus compression of esophageal lumen |
| IV: Complete obliteration of the lumen with hematoma, edema, and organized clot formation |
Table 2.
Causes of esophageal hematomas
| Spontaneous | Associated with coughing, retching, protracted vomiting |
| Esophageal barotrauma | |
| Pill-induced esophageal injury | |
| Use of anticoagulants or aspirin | |
| Esophageal diverticulum A-V malformation | |
| Traumatic | Endoscopic intubation, biopsy, dilation |
| Variceal sclerotherapy | |
| Transesophageal echocardiography | |
| Foreign body ingestion |
The clinical presentation is variable. Although mostly asymptomatic, esophageal hematomas may present with dramatic chest pain, severe dysphagia, and hematemesis. In such instances, they should be differentiated from Mallory-Weiss tear and Boorhaave’s syndrome, conditions which they may closely mimic[19-21]. Typically barium swallow or CAT scan have been used for the diagnosis, showing intraluminal filling defects or a double-barrelled appearance of the esophagus[22]. More recently, endoscopy is the preferred investigation, especially when hematemesis is the presenting symptom[23]. Because spontaneous resolution is the rule, the treatment of esophageal hematomas is conservative and consists of a regimen of nil by mouth, intravenous alimentation and antibiotics in severe cases[1]. Surgery is reserved only for rare instances, to drain a hematoma and close an esophageal mucosal tear[24].
In our study, all four patients were male, the hematoma was visualized end oscopically, and was traumatic either from insertion of the scope (cases 1 and 4), or from endoscopic manipulation (cases 2 and 3). In 3 out of 4 of our patients the hematomas were asymptomatic. Because of the increased utilization of endoscopy for diagnosis and therapy, it is expected that esophageal hematomas will be encountered more frequently. This is particularly true in cases of esophageal dilation of strictures, repetitive multiple biopsies for surveillance of Barrett’s esophagus, esophageal variceal sclerotherapy, and transesophageal echocardiography.
Hematomas related sclerotherapy seem to occur 2 d-4 d after injection, when tissue necrosis that extends into the submucosa reaches its maximum. Contributing factors include volume of sclerosant per injection, interval between treatments, paravariceal versus intra-variceal injection, bleeding diathesis, and occurrence of retching or prolonged Valsalva during or shortly after the treatment[3-5]. Early endoscopy is useful in establishing the diagnosis and reveals an intraluminal bulge of the mucosa with dark blue discoloration.
The blind insertion of a transesophageal endosonographic probe for diagnosis of valvular heart disease[25], and its increased utilization during cardiothoracic surgery[6] represents an additional risk for esophageal hematoma formation, as exemplified in case 4 of this report. A recent review of the literature on the association of transesophageal echocardiography during cardiac surgery and gastrointestinal bleeding revealed that the overall percentage of postoperative gastrointestinal complaints following the procedure was 11%, and frank upper gastrointestinal bleeding was 2.1%[6]. Another multicenter survey of 10419 examinations on the safety of transesophageal echocardiography revealed only 2 patients who developed bleeding complications which necessitated interruption of the examination[7]. Realising that the risk of gastrointestinal bleeding is small but present, most authors recommend careful review of upper digestive symptoms to rule out preexisting esophageal pathology, ample lubrication of the endosonographic tip, and avoidance of fixation of the probe in a flexed position for prolonged periods in order to avoid contact pressure and esophageal mucosal damage[8].
In conclusion, our study reviews the endoscopic features of esophageal hematomas and classifies them in terms of etiology and appearance. With the widespread use of esophageal instrumentation, these lesions will be increasingly recognized endoscopically. Depending on their severity and endoscopic stage, esophageal hematomas may or may not be associated with symptoms. Treatment is generally conservative and favorable prognosis is the rule.
Footnotes
Edited by Pan BR
Proofread by Ma JY
References
- 1.Meulman N, Evans J, Watson A. Spontaneous intramural haematoma of the oesophagus: a report of three cases and review of the literature. Aust N Z J Surg. 1994;64:190–193. doi: 10.1111/j.1445-2197.1994.tb02176.x. [DOI] [PubMed] [Google Scholar]
- 2.Marks IN, Keet AD. Intramural rupture of the oesophagus. Br Med J. 1968;3:536–537. doi: 10.1136/bmj.3.5617.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Low DE, Patterson DJ. Complete esophageal obstruction secondary to dissecting intramural hematoma after endoscopic variceal sclerotherapy. Am J Gastroenterol. 1988;83:435–438. [PubMed] [Google Scholar]
- 4.Salomez D, Ponette E, Van Steenbergen W. Intramural hematoma of the esophagus after variceal sclerotherapy. Endoscopy. 1991;23:299–301. doi: 10.1055/s-2007-1010694. [DOI] [PubMed] [Google Scholar]
- 5.Shay SS, Berendson RA, Johnson LF. Esophageal hematoma. Four new cases, a review, and proposed etiology. Dig Dis Sci. 1981;26:1019–1024. doi: 10.1007/BF01314765. [DOI] [PubMed] [Google Scholar]
- 6.Hulyalkar AR, Ayd JD. Low risk of gastroesophageal injury associated with transesophageal echocardiography during cardiac surgery. J Cardiothorac Vasc Anesth. 1993;7:175–177. doi: 10.1016/1053-0770(93)90212-4. [DOI] [PubMed] [Google Scholar]
- 7.Daniel WG, Erbel R, Kasper W, Visser CA, Engberding R, Sutherland GR, Grube E, Hanrath P, Maisch B, Dennig K. Safety of transesophageal echocardiography. A multicenter survey of 10, 419 examinations. Circulation. 1991;83:817–821. doi: 10.1161/01.cir.83.3.817. [DOI] [PubMed] [Google Scholar]
- 8.Urbanowicz JH, Kernoff RS, Oppenheim G, Parnagian E, Billingham ME, Popp RL. Transesophageal echocardiography and its potential for esophageal damage. Anesthesiology. 1990;72:40–43. doi: 10.1097/00000542-199001000-00008. [DOI] [PubMed] [Google Scholar]
- 9.No authors listed. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 44-1989. A 74-year-old woman with subxiphoid pain and narrowing of the esophagus. N Engl J Med. 1989;321:1249–1259. doi: 10.1056/NEJM198911023211807. [DOI] [PubMed] [Google Scholar]
- 10.Herbetko J, Delany D, Ogilvie BC, Blaquiere RM. Spontaneous intramural haematoma of the oesophagus: appearance on computed tomography. Clin Radiol. 1991;44:327–328. doi: 10.1016/s0009-9260(05)81268-1. [DOI] [PubMed] [Google Scholar]
- 11.Talley NA, Nicks R. Spontaneous submucosal haematoma of the oesophagus: "oesophageal apoplexy". Med J Aust. 1969;2:146–150. doi: 10.5694/j.1326-5377.1969.tb105664.x. [DOI] [PubMed] [Google Scholar]
- 12.Smith G, Brunnen PL, Gillanders LA, Teo HS. Oesophageal apoplexy. Lancet. 1974;1:390–392. doi: 10.1016/s0140-6736(74)93152-3. [DOI] [PubMed] [Google Scholar]
- 13.Joffe N, Millan VG. Postemetic dissecting intramural hematoma of the esophagus. Radiology. 1970;95:379–380. doi: 10.1148/95.2.379. [DOI] [PubMed] [Google Scholar]
- 14.Mosimann F, Brönnimann B. Intramural haematoma of the oesophagus complicating sclerotherapy for varices. Gut. 1994;35:130–131. doi: 10.1136/gut.35.1.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones DB, Frost RA, Goodacre RL. Intramural hematoma of the esophagus--a complication of endoscopic injection sclerotherapy. Gastrointest Endosc. 1986;32:239–240. doi: 10.1016/s0016-5107(86)71819-1. [DOI] [PubMed] [Google Scholar]
- 16.Klygis LM. Esophageal hematoma and tear from a taco shell impaction. Gastrointest Endosc. 1992;38:100. doi: 10.1016/s0016-5107(92)70359-9. [DOI] [PubMed] [Google Scholar]
- 17.Piccione PR, Winkler WP, Baer JW, Kotler DP. Pill-induced intramural esophageal hematoma. JAMA. 1987;257:929. [PubMed] [Google Scholar]
- 18.Biagi G, Cappelli G, Propersi L, Grossi A. Spontaneous intramural haematoma of the oesophagus. Thorax. 1983;38:394–395. doi: 10.1136/thx.38.5.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sen A, Lea RE. Spontaneous oesophageal haematoma: a review of the difficult diagnosis. Ann R Coll Surg Engl. 1993;75:293–295. [PMC free article] [PubMed] [Google Scholar]
- 20.Kerr WF. Spontaneous intramural rupture and intramural haematoma of the oesophagus. Thorax. 1980;35:890–897. doi: 10.1136/thx.35.12.890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yeoh NT, McNicholas T, Rothwell-Jackson RL, Goldstraw P. Intramural rupture and intramural haematoma of the oesophagus. Br J Surg. 1985;72:958–960. doi: 10.1002/bjs.1800721208. [DOI] [PubMed] [Google Scholar]
- 22.Ackert JJ, Sherman A, Lustbader IJ, McCauley DI. Spontaneous intramural hematoma of the esophagus. Am J Gastroenterol. 1989;84:1325–1328. [PubMed] [Google Scholar]
- 23.Tim LO, Segal I, Mirwis J. Intramural haematoma of the oesophagus. The role of endoscopy. S Afr Med J. 1982;61:798–800. [PubMed] [Google Scholar]
- 24.Folan RD, Smith RE, Head JM. Esophageal hematoma and tear requiring emergency surgical intervention. A case report and literature review. Dig Dis Sci. 1992;37:1918–1921. doi: 10.1007/BF01308089. [DOI] [PubMed] [Google Scholar]
- 25.Seward JB, Khandheria BK, Oh JK, Abel MD, Hughes RW, Edwards WD, Nichols BA, Freeman WK, Tajik AJ. Transesophageal echocardiography: technique, anatomic correlations, implementation, and clinical applications. Mayo Clin Proc. 1988;63:649–680. doi: 10.1016/s0025-6196(12)65529-3. [DOI] [PubMed] [Google Scholar]


