Introduction
Hemangiomas are benign lesions of vascular origin. Intraosseous hemangiomas occur most commonly in the vertebral body and skull.1 Intraosseous hemangiomas involving the facial bones are rare.2 Facial bone hemangiomas most commonly involve the maxilla and mandible. Zygomatic bone is a very rare site,2 only 20 being reported as per literature.3 Vertebral and skull hemangiomas are usually asymptomatic, whereas facial hemangiomas are commonly symptomatic.4 They can present with swelling which may be painful or painless, palpable mass or paraesthesias. Here we report a case of intraosseous hemangioma in the zygomatic bone presenting with characteristic CT and MRI findings.
Case report
A 38 year old female patient presented to the surgical outpatient department with a 6 months history of a solitary slow growing, painless swelling on the right side of face. There was no history of any trauma. On examination there was a hard, non-tender, immobile swelling over the right malar eminence.
Plain radiographs of the face were not helpful as the swelling was overlapped by the facial bones and could not be seen. A subsequent CT (Siemens Somatom Emotion, 6 slice MDCT) scan showed a 3 cm, well defined, expansile bony lesion arising from the anterior aspect of right zygomatic arch. The lesion was showing prominent trabeculations in a radiating distribution resulting in a sunburst appearance. There was no periosteal reaction and no soft tissue mass (Fig. 1). A preliminary diagnosis of hemangioma was made based on the CT appearance. MRI (Siemens Magnetom Essenza 1.5 T) showed a T1 intermediate signal intensity and T2 high signal intensity expansile mass involving the right zygomatic arch. The lesion showed tiny areas of signal void, which corresponded to the prominent trabeculations seen on CT scan (Fig. 2). No contrast study was performed. A needle aspiration was performed but was inconclusive. No biopsy was performed in view of risk of hemorrhage.
Fig. 1.
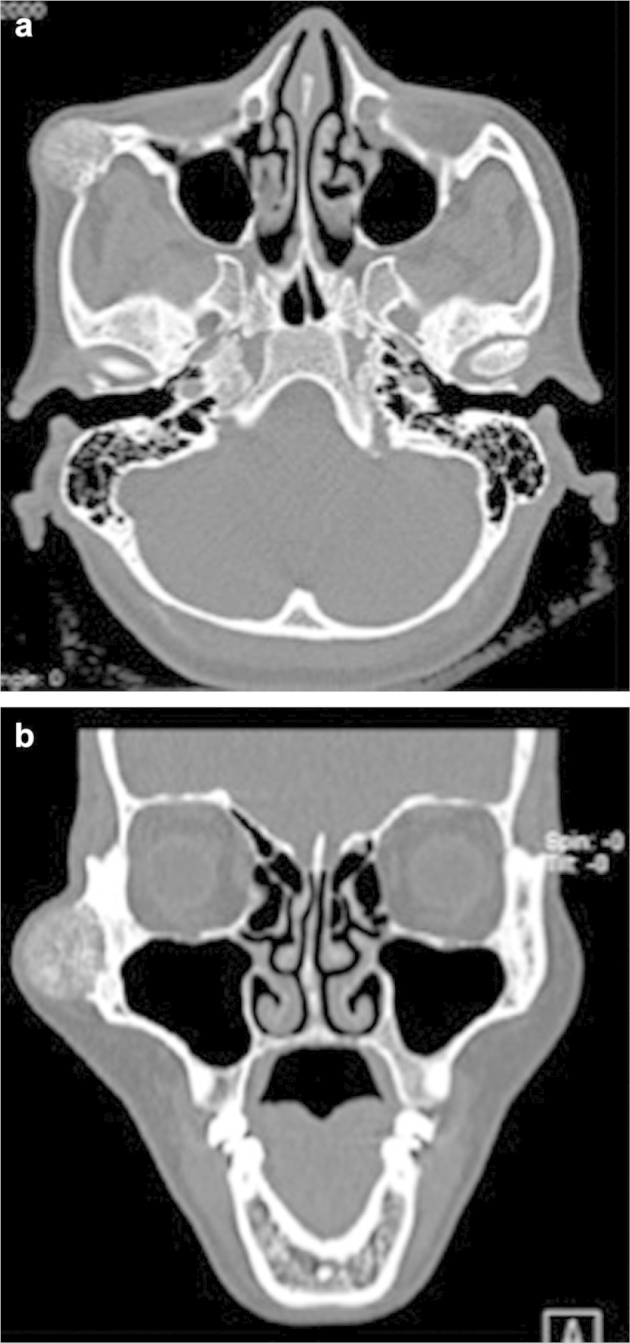
Plain CT Axial (a) and coronal (b) images showing well-defined, expansile bony lesion arising from the anterior aspect of right zygomatic arch.
Fig. 2.
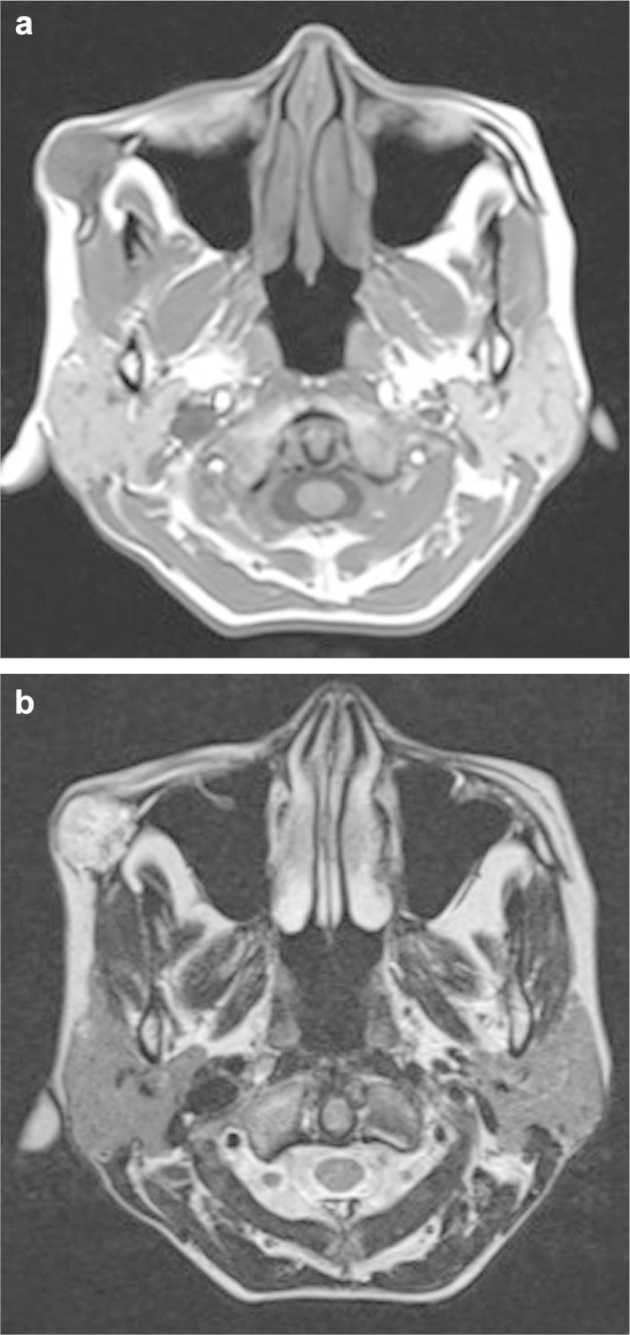
MRI axial T1 (a) and T2 (b) showing T1 intermediate signal intensity and T2 high signal intensity expansile mass involving the right zygomatic arch.
Based on the radiological diagnosis, the patient was taken up for surgery. The lesion was subjected to excision followed by reconstruction of zygomatic bone by bone grafting. There was only minimal intra-operative bleeding. Histological examination of the resected specimen revealed multiple vascular channels filled with red blood cells and lined by endothelial cells. There were multiple bony trabeculae, osteoid and muscle tissue. Histopathological features were consistent with a diagnosis of hemangioma.
Postoperatively, the patient had an uneventful recovery and was discharged after 7 days.
Discussion
Hemangiomas are benign lesions of vascular origin. Intraosseous hemangiomas most commonly involve the vertebral body and skull,1 whereas involvement of facial bones is rare.2 Facial bone hemangiomas most commonly involve the maxilla and mandible. The zygomatic bone is a very rare site,2 only 20 being reported as per literature.3 Hemangiomas within the vertebral body or skull are usually asymptomatic, whereas facial hemangiomas are commonly symptomatic.4 They can present with swelling which may be painful or painless, palpable mass or paraesthesias.
Zygomatic hemangiomas usually occur in the fourth decade of life and there is a 3:1 female predominance.3 The lesion shows left sided predominance and there may be associated prior trauma.3
On radiography, intraosseous hemangiomas can have variable appearances.5 Facial hemangiomas can show a multilocular radiolucency with small loculations resulting in honeycomb appearance or large loculations resulting in a soap-bubble appearance.1 The multilocular lesion may show internal radiopaque striae radiating from the centre resembling spokes of a wheel.1 CT scan gives excellent details of cortical and trabecular pattern and is the best imaging modality for assessing the intraosseous hemangiomas.3, 4
A well-defined expansile lesion showing a sunburst pattern of radiating trabeculae with intact inner and outer tables is the characteristic pattern of intraosseous hemangiomas on CT scan.3, 4 On MRI the appearances of intraosseous hemangiomas vary according to the size of the lesion, the degree of intralesional vascularity and also on the relative proportion of red marrow and fatty marrow within the lesion.3, 4 Typical lesions can show a mottled appearance on MRI.4 Small lesions appear hyperintense on T1 while larger lesions appear hypointense on T1 images. The signal intensity on T2 images is hyperintense.4 Following administration of intravenous gadolinium, lesions show marked enhancement.3, 4
Preoperative angiography to shows feeders from the branches of external carotid artery and preoperative embolisation to minimise intra-operative blood loss are recommended in selective cases. However, some authors feel that if adequate margin of normal bone is resected these measures are not required.3
Histopathologically, hemangiomas show endothelial lined vascular spaces of varying size, interspersed with fibrous connective tissue stroma often admixed with bony trabeculae.5 According to the size of the vascular spaces the hemangiomas are classified into capillary type and cavernous types,5 capillary type showing small vessels with prominent stromal component while the cavernous type shows larger vessels and sparse stroma.5 Hemangiomas of the mixed type show features of both capillary and cavernous types. Histopathological examination provides a definite diagnosis of hemangioma. Needle aspiration is preferable as biopsy can result in severe hemorrhage.5
In the present case, a preoperative diagnosis of intraosseous hemangioma of zygomatic bone was made based on the typical radiological features. The differentials included intraosseous meningioma, fibrous dysplasia, osteochondroma and osteogenic sarcoma. Intraosseous meningiomas show hyperostosis and soft tissue component.6 These features were not present in our case. The present case did not have ground glass appearance typical of fibrous dysplasia; there was no cortico-medullar continuity, which is a feature of osteochondroma. Osteogenic sarcoma was ruled out as a differential as the cortex though thinned-out was preserved and smooth, and there was no associated periosteal reaction or soft tissue involvement.
Treatment options for intraosseous hemangiomas include sclerotherapy, radiotherapy and surgery. Sclerotherapy results in fibrosis and obliteration of vessels but high flow lesions can displace the sclerosing agents too quickly and a curative effect may not be possible.5 Radiotherapy can be performed in lesions that are surgically inaccessible, but can result in scar formation, and rarely result in malignant transformation.3 Surgery is the recommended procedure and is indicated for lesions that show increasing size and for cosmetic reasons.4 Intra-operative bleeding is a complication of surgery and can be minimised by preoperative embolisation. Excision of adequate margin of normal bone can reduce the risk of severe intra-operative hemorrhage.
Conflicts of interest
All authors have none to declare.
References
- 1.Zlotogorski A., Buchner A., Kaffe I., Schwartz-Arad D. Radiological features of central haemangioma of the jaws. Dentomaxillofac Radiol. 2005;34:292–296. doi: 10.1259/dmfr/37705042. [DOI] [PubMed] [Google Scholar]
- 2.Cuesta Gil M., Navarro-Vila C. Intraosseous hemangioma of the zygomatic bone. A case report. Int J Oral Maxillofac Surg. 1992 Oct;21:287–291. doi: 10.1016/s0901-5027(05)80739-8. [DOI] [PubMed] [Google Scholar]
- 3.Moore Sandra L., Chun Jin K., Mitre Sandra A., Som Peter M. Intraosseous hemangioma of the Zygoma: CT and MR findings. AJNR Am J Neuroradiol. 2001;22:1383–1385. [PMC free article] [PubMed] [Google Scholar]
- 4.Gonçalves F.G., Rojas J.P., Hanagandi P.B. Case report: periorbital intraosseous hemangiomas. Indian J Radiol Imaging. 2011 Oct–Dec;21:287–290. doi: 10.4103/0971-3026.90691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eliot Colin A., James T. Intraosseous hemangioma of the anterior mandible. Head Neck Pathol. June 2010;4:123–125. doi: 10.1007/s12105-010-0170-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tokgoz N., Oner Y.A., Kaymaz M. Primary intraosseous meningioma: CT and MRI appearance. AJNR Am J Neuroradiol. 2005;26:2053–2056. [PMC free article] [PubMed] [Google Scholar]


