Abstract
A major drawback of conventional fixator system is the penetration of fixator pins into the medullary canal. The pins create a direct link between the medullary cavity and outer environment, leading to higher infection rates on conversion to intramedullary nailing. This study was designed to prospectively evaluate the role of new rapid pinless external fixators in primary stabilization of open tibial shaft fractures. In our study, a prospective study of 96 consecutive patients of open tibial shaft fractures treated with new rapid pinless external fixator and reamed intramedullary nail was carried out. The bone healing status, ability to maintain alignment were examined for radiologic outcome, whereas initial management, length of hospital stay, associated morbidity, range of knee and ankle motion, time to partial and full weight-bearing, employment status and perioperative and postoperative complications were used for clinical evaluation. We followed up for over two years for the patients underwent clinical and radiologic after the surgery. The mean hospital stay was 15 days (ranges, 8-68). Bone healing was achieved for all cases except 3 patients who were lost to follow-up study. No patient suffered compartment syndromes. There was no statistically significance in range of motion among the knees of injury and uninjured limbs at final follow-up (P > 0.05). To the last follow-up, there were no cases of deep infection or implant-related fractures. Seventy-one patients who were employed before the injury returned to work after the operation, 16 had changed to less strenuous work. We concluded that better results can be achieved on clinical and radiologic evaluation of primary stabilization with rapid pinless external fixator and early exchange reamed intramedullary nail for suitable patients with open tibial shaft fractures. The incident rate of relative complications is low. The rapid pinless external fixator can be combined favorably with the reamed intramedullary nail and is a valuable addition to the conventional external fixator systems.
Keywords: Open tibial fracture, pinless fixator, intramedullary nailing
Introduction
Because of the lack of anteromedial muscle coverage and immediate proximity to wounding forces and the ground, the tibia is the most common bone associated with an open soft tissue wound. For the open tibia, soft tissue debridement and early definitive coverage has been of critical importance. Improvement in stabilization techniques has played an equal role in enhancing the outcomes of treatment. In its most advanced form, External fixator is considered to be the optimum treatment for severe wounds associated with tibial fracture. External fixator can offer excellent stability in the primary treatment of fractures with severe damage to the soft tissue, and can be less revitalization of normal cortical bone microcirculation adjacent to the fracture compared with internal fixation. There are commonly difficulties in treating the most severe fractures to union because of the problem of pin loosening and healing times of 4-6 months. For this reason, efforts are generally made to transfer from an external to an internal fixation device as soon as possible. Good results may be achieved if reamed intramedullary nail follows a short period of standard external fixation [1], but all fixator models in current use have one serious disadvantage, namely that they require screws or pins which penetrate the intact cortical bone and open the medullary cavity. This creates a direct communication between the medullary cavity, the bone and the exterior, in other words the situation which exists in an open fracture. A survey of the literature on deep infection following conversion on tibiae from external fixator to intramedullary nail shows a significant risk in this devastating complication [2-6]. With a bone grasping mechanism rapid pinless external fixator does not penetrate the medullary cavity; the medulla of the bone remains sterile. This facilitates early soft tissue coverage by offering adequate stability to the limb without penetration of the bone. Early conversion to intramedullary nail is facilitated as the nail can be placed while the apparatus is maintaining alignment. Additional benefits are gleaned by the fact that no drill or power equipment is necessary for frame application. This fracture device offers distinct advantages in the disaster or battlefield setting.
Pinless external fixator has gained acceptance in the treatment of open tibial shaft fractures, especially in cases with polytrauma or high-energy injuries. The objective of this study was to present a large cohort of patients with open tibial shaft fractures treated with two-staged with rapid pinless external fixator and reamed intramedullary nail with a minimum two-year follow-up. We sought to describe clinical outcomes and to determine the rate of complications using a validated measure.
Material and methods
Study population
Approval of the experimental design by the authors’ institutional review board was obtained prior to initiation of this study. An approved consent form was signed by each patient before any testing was performed. The criteria included specified participants between ages 18 to 60 years, open tibial shaft fractures which underwent immediate fixation with a new design rapid pinless external fixator after the injury. The distal fragment or proximal fragment was large enough for two clamps. The exclusion criteria involved major fractures of other sites and significant associated injury to any other major organ systems requiring hospital admission and active management, pathologic or osteoporotic fractures, fractures in extremities that underwent amputation during the first hospital admission post injury, or were not available for adequate follow-up.
From March 2008 to September 2010, a total of 96 consecutive patients with a diagnosis of open tibial shaft fractures were prospectively enrolled from the practice of three surgeons from three academic institutions. These patients were treated with a two-staged treatment (primary rapid pinless external fixator followed by intramedullary nail). All frames were applied in the operating room under general or regional anesthesia and sterile conditions. All patients were followed up for at least two years.
Fixation system
Rapid pinless external fixator system (RPEF) was provided by Double Engine Medical Material Company, China. Elements of the RPEF included universal clamp with adjustable dual hinges (central and top), carbon fiber rod (offering different length), rod-to-rod clamp and tube-to-rod clamp (Figures 1 and 2). The universal clamp is similar to skull retractor. The shape of the clamp tip was arc bifurcated. According to the different fracture site of the tibia, the large size or small size clamps were used. All implants were manufactured using 317L stainless steel except rod.
Figure 1.

Elements of the REPF: carbon fiber rods, tube-to-tube clamps, universal clamps.
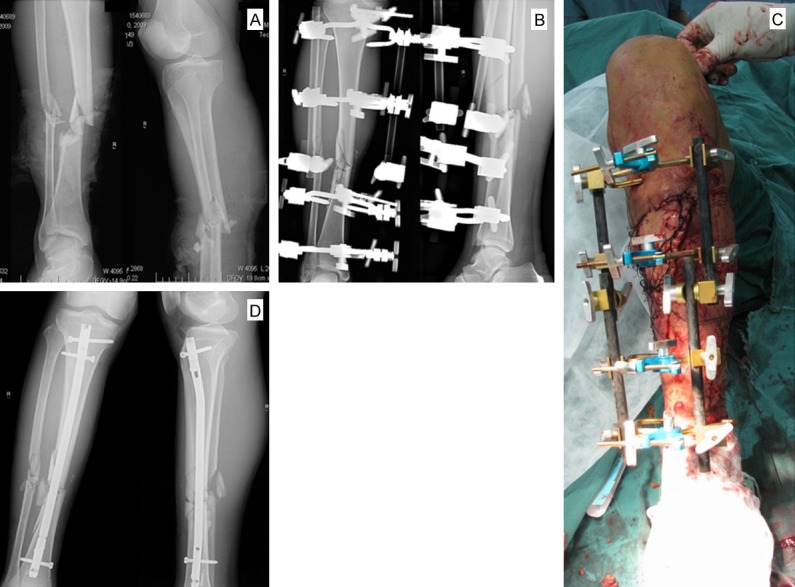
Figure 2.

A 26-year-old-man sustained a second degree compound fracture of the tibia (AO classification 42B3) together with multiple injuries. A. Anteroposterior and lateral radiographs. B. Postoperative radiograph shows well aligned fracture stabilized with REPF. C. Mobilization on the 3th day postoperative with partial weight-bearing. D. Once the general condition of the patient had improved, a conversion procedure to a reamed intramedullary nail was done on the 7th day. Postoperative radiograph AP and lateral of the fracture showing good reduction and fixation with reamed tibial nail.
Surgical technique
The fixator was applied under spinal anesthesia. There is no need for a traction table. The patients were in the supine position with the fracture leg elevated on a frame and the knee flexed at 45°. A transverse stab incision was made at the planned clamp insertion site. The skin was incised followed by a vertical blunt dissection to the bone. Depending on the geometry of fracture and condition of soft tissues, each main fragment received two clamps. Due care was taken to avoid impaling tibial tubercle patellar tendon by the clamps in the proximal part. Damage to the saphenous vein and nerve must be avoided in the distal part. The muscle compartments should remain intact so that the clamps are in the so-called “safe corridor” [7]. The traction and reduction was then performed by an assistant, if possible with intraoperative radiologic image control. Once adequate reduction has been achieved, the RPEF was stabilized by tightening the hinges. Then the universal clamp was connected to a carbon fiber rod with tube-to-rod clamp. Attempt was made to achieve soft tissue cover by loose closure of soft tissue. All patients received a second generation cephalosporin intravenously for 3-5 days after surgery. Once there were no signs of local wound infection, patients were allowed for definitive internal fixation with reamed intramedullary nail.
Assessment methods
Preoperative radiographic and clinical evaluations were performed within 1 day of surgery and postoperative evaluations were performed at three months, six months, twelve months and two years. All the fractures were classified as per AO fracture classification [8] for fracture anatomy and Gustilo and Anderson classification [9] for nature of open injury. All the fractures selected were of the diaphysis segment.
The authors’ evaluation, mainly concerned with the capabilities and limitations of RPEF, focuses on initial management, time to debridement, soft tissue coverage, ease of wound access, neurovascular compromise, length of hospital stay, associated morbidity, bone healing status, ability to maintain alignment, range of knee and ankle motion, time to partial and full weight-bearing, employment status and perioperative and postoperative complications. The evaluations were performed independently by 3 authors on 3 separate occasions and in a blinded manner, and the results were then averaged.
Statistical analysis
Statistical analysis, including mean values, standard deviations (SD), and comparison between preoperative and postoperative data were performed using the paired t test by SPSS software (SPSS, Chicago, IL, USA). Difference among groups was analyzed by Student’s t-test, with a p value (two-tailed) less than 0.05 considered statistically significant.
Results
One hundred and five fractures (96 patients) were analyzed. Fifty-nine patients (61%) were men, and thirty-seven were women. The ages ranged from a minimum of 18 years to a maximum of 59 years, with a mean of 34.1 years (SD, 8.8). Severity of fractures was classified according to AO/ASIF classification [8]: type A, 52 fractures; type B, 42; type C, 11. Two fractures were in the proximal third of the tibial shaft; 99 were in the middle third; four were in the distal third. Forty-two patients (44%) suffered Gustilo grade I fractures, 33 (34%) grade II fractures and 21 (22%) grade III fractures. Within the Grade III fractures, 12 suffered Grade III a, 7 suffered Grade III b and two suffered Grade III c. Eighty-seven patients were injured in motor vehicle accidents, four patients were injured in labor accidents, and the remaining five patients were injured in other causes (Table 1). Fifty-six of the 96 patients (58%) had associated injuries. Not including injuries to skin and subcutaneous tissue, 49 patients (51%) had local injuries, e.g., peroneal nerve lesions, loss of compartments, bone loss, and transection of the peroneal or a tibial artery. Twenty-one patients had sustained 41 fractures elsewhere. There were 34 associated head, thorax, or abdominal injuries in twenty-four patients. The mean injury severity score was 12 (range 9-16).
Table 1.
Patient profiles of Fractures
| Classification | Patient No | Cause of Fractures | Age | |
|---|---|---|---|---|
| Grade I | 42 | Motor vehicle accidents | 87 | 18-59 (SD=8.8) |
| Grade II | 33 | Lab accidents | 4 | |
| Grade III | 21 | Other | 5 | |
| Total | 96 (59 men, 37 women) |
Perioperative data
The fractures were stabilized with four clamps (two per main fragment) on the tibia and two carbon fiber rods placed anteromedially according to the technique described above. The mean time between injury and surgery was 5.9 h (S.D±3.7 h). The surgeons received instruction pre- and intraoperatively from the author. The average time of insertion for a rapid pinless external fixator for three different surgeons was 15 minutes (S.D±5.8 mins). The appropriate management of these 105 tibial fractures involved 113 debridements; 7 soft tissue procedures, e.g., split-thickness grafts, muscle pedicle flaps, and free flaps; and 4 bony procedures in the form of primary and secondary bone grafting and osteotomies. All of these procedures were performed without significant interference by the external fixator. Ninety-four wounds were closed at the initial debridement. Prophylactic fasciotomies were performed in four patients; however, no compartment syndromes were seen. With well reduced tibiae and bony contact of the main fragments, patients were encouraged to take active part or full weight (supplemented with crutches) on the second day after surgery. In cases of bone defect or angular deviation of the reduced tibia, weight-bearing was considered inadvisable. Once the patient’s general condition has been stabilized, definitive treatment of the fracture with reamed intramedullary nail can be carried out. The time of conversion to intramedullary nail was an average of 9 days (5 days to 6 weeks). Following definitive internal fixation, no additional soft tissue procedure was required in most cases. The mean hospital stay was 15 d (ranges, 8-68 d). Typical cases are shown in Figures 2 and 3.
Figure 3.
Open tibial fracture (AO classification 42C3) with severe soft tissue injury in a 43-year-old-man who was involved in an automobile accident. A. Anteroposterior and lateral radiographs. B and C. Primary treatment included application of the REPF and muscle pedicle flaps. D. Conversion to a reamed intramedullary nail on the 14th day.
Follow-up data
The patients were prospectively followed up for minimum 2 years. Three patients were lost to follow-up study before the final examination. Pre- and post-operative images were available for all patients. The 93 patients progressed to complete soft tissue and bony consolidation, i.e., full unsupported weight-bearing, after a median of 127 days (range, 91-312 days). Measurements were obtained in 101 open tibial fractures (93 patients). The differences in range of motion between the knees of the injured and uninjured limbs were statistically insignificant at final follow-up (P > 0.05). The ankle motion of injured sides changed slightly (6°) but not significantly compared with uninjured sides at the last follow-up (P > 0.05). For most patients this loss was barely noticeable. Five fractures healed with a residual angulation of more than 5°; one in varus (7°), two in valgus (8° and 12°). Seventy-one patients who had been working before injury returned to original work without restrictions, 16 had changed to less strenuous work. The remaining 6 patients were unemployed.
Complications
Twenty-four complications (9.8%) occurred in the treatment of the 105 fractures. Three superficial wound infections developed, two of these patients suffered Grade II fractures and the other was Grade III fractures, all of the patients responded to treatment with antibiotics. No patient developed deep infection. One patient developed a partial flap failure, after which the necrotic skin was resected. Two were delayed union requiring dynamization. No trans fixation of tendons or adjacent nerves and vessels occurred. No thromboembolic complications or implant-related fractures were noted. There were not any additional postoperative compartment syndromes. Penetration of the cortex by the trocar points occur three times. Most penetrations were located within the metaphysis and were without any sequelae. The clamps were left in place until the pinless external fixator was removed in a second procedure.
Discussion
The surgical technique for treatment of severe open tibial fractures represents a difficult challenge for many surgeons. As is known to all, intramedullary nail is the gold standard for treatment of tibial fractures. It can safely and reproducibly stabilize most kind of tibial fractures [10]. However, primary nailing may not be feasible in cases of high-energy open fractures and polytrauma. Conventional external fixator for the primary treatment of tibial shaft fractures before secondary intramedullary nail always is accompanied with the risk of pin tract and deep infection. Most authors report rates between approximately 5% and 25% [1,11,12]. The risk of deep infection is higher if one of the pin entrance points has shown any signs of infection during the primary treatment. Before any internal fixation is done, it is recommended to remove the external fixator and wait until the pin tract infection is healed [11]. In an attempt to overcome these problems pinless external fixator has been developed to permit fixation of tibial fracture without penetrating the medullary cavity [12]. A bone barrier remains intact and possible pin tract infections will remain local without the risk of germ transmission to the medullary canal. The basic idea of the pinless fixator was its use as a temporary stabilizer for open tibial fractures until soft tissue consolidation to be followed by intramedullary nail [13,14]. Generally, the ideal pinless fixator should have the following characteristics, including simplicity, stability, rapid application, minimal damage and easier technology [15]. However, some problems of AO-pinless fixator that have been brought out by some studies, including poor stability, inconvenient installation, skin necrosis, impalement of musculotendinous units [14,16]. To some degree, these defects make the technique limited in application at the current time. It should be taken into consideration to aim at optimising the clinically acceptable pinless external fixator.
The main problem of AO-pinless fixator is poor stability and pin loosening. After mounting the pinless fixator and attaching a longitudinal rod, a certain amount of instability was evident both intraoperatively and in the postoperative period. Most experts emphasize that AO-pinless fixator are more frequently being applied as temporary devices. Stene tried to simulate the reaction of the bone to a pinless clamp on a sheep tibia with the clamp being loaded with cyclical tilting movements over five weeks. The clamp was found to maintain 72% of the initially applied clamping force after 5 weeks of in vivo application and it was found to be tight at removal [17]. Therefore some authors think the application time of AO-pinless fixator can be extended to five weeks [18]. However, the other mechanical tests have demonstrated the lower stiffness of the AO-pinless fixator compared with the conventional AO-tubular device. The axial stiffness was only 36% of the comparable tubular construction [14]. When removing the pinless fixator at the conversion of intramedullary nail, the clamps were described as loose by every treating surgeon. For fear of pin loosening of AO-pinless fixator, postoperative weight-bearing functional exercise are limited by most every doctors [18]. This situation often lasts until the replacement procedure is completed. Taking these issues into consideration, it is considered that the geometry of pinless fixator should be modified. Some authors recommended a two rod construction and a sharper trocar tips to increase the stability of the fixator and reduce slippage [19]. For these reasons, a new RPEF system has been introduced and tested in a series of 96 consecutive patients with open tibial shaft fractures. Liu in his study showed that the RPEF configurations with 4-clamps and 2-bar pressure showed stiffness values (as a percentage of the corresponding AO-tubular fixator): 82% axial stiffness, 91% bending stiffness perpendicular to the reference plane, 64% bending stiffness parallel to the reference plane, and 60% torsional stiffness. According to the experimental data, it is confident in using the RPEF as a better support device for the lower leg. RPEF can offer more axial stability and, in particular, can allow active mobilization of the knee joint during the period before definitive internal fixation. Patient care is also expected to be easier and comfort improved. If the need arises for later adjustment of the fixation, this can be performed easily in all planes by loosening the fixation.
RPEF can also be used to maintain fracture reduction while exchange intramedullary nail is performed under image intensifier. It is a definite procedural advantage. If the primary reduction has proven satisfactory and stable, subsequent nailing will not be difficult. This avoids unnecessary manipulation of the limb to achieve reduction, thus preventing further damage to the soft tissue [15,18,20]. After using pinless fixator early, most authors choose to convert un-reamed intramedullary nail [16,18,21,22]. However, its intrinsic lack of stability might restrict the use of the un-reamed intramedullary nail to severe open tibial fractures only. The AO Group recommends that the un-reamed intramedullary nail be used for temporary fixation of severe tibial fractures and that further procedures depend on the circumstances. Literature reveals malalignment rates after un-reamed nailing of all tibial shaft fractures to be between 9% and 50%. Some recent studies which comparing reamed with un-reamed intramedullary nail for tibial fractures indicates that reamed intramedullary nail may lead to significantly lower risks of nonunion, failure of the interlocking bolts, implant exchange, and dynamization without increasing operative complications [23-25]. It should also be mentioned that not all trauma hospitals have experience with un-reamed nails or even use these nails. In contrast, reamed intramedullary nail are in use by every surgeon all over the world. Therefore, we think it is a better choice for tibial fractures to replace un-reamed intramedullary nail by reamed one. This requires bone shafts with higher stability, when importing reamed intramedullary nail. In the authors’ patient sample, reamed intramedullary nail were used in nearly all patients, the surgeon did not run into any obstacles while importing nailing. The radiologic results indicated correct axial alignment at follow-up in 96% of those cases. After the procedure of importing intramedullary nail, RPEF can also be used in combination with intramedullary nail as an external locking device for increasing stability in highly unstable fractures to avoid primary and secondary malalignment. After converted to reamed intramedullary nail, 3 patients keep RPEF in position until bone healing.
In conclusion, good clinical and radiologic evaluation results of two-staged operation and reconstruction with RPEF and reamed intramedullary nail for open tibial shaft fractures can be achieved in this study. The advantages of RPEF are its no-penetrating clamp, its simplicity of application, its better stability and its use as a reduction aid for conversion to reamed intramedullary nail. It may be of particular value to many clinicians who are not well experienced in the treatment of severe open fractures (transfer to a centre, re-evaluation) and also for those working with reamed nails as one of their secondary treatment options for open tibial fractures. Experience and results achieved indicate that the pinless external fixator is a valuable addition to the existing external fixator system.
Disclosure of conflict of interest
None.
References
- 1.Blachut PA, Meek RN, O’Brien PJ. External fixation and delayed intramedullary nailing of open fractures of the tibial shaft. A sequential protocol. J Bone Joint Surg Am. 1990;72:729–735. [PubMed] [Google Scholar]
- 2.Bone LB, Johnson KD. Treatment of tibial fractures by reaming and intramedullary nailing. J Bone Joint Surg Am. 1986;68:877–887. [PubMed] [Google Scholar]
- 3.Schmidt NF, Tarbet WJ. The effect of oral rinses on organoleptic mouth odor ratings and levels of volatile sulfur compounds. Oral Surg Oral Med Oral Pathol. 1978;45:876–883. doi: 10.1016/s0030-4220(78)80009-7. [DOI] [PubMed] [Google Scholar]
- 4.McGraw JM, Lim EV. Treatment of open tibial-shaft fractures. External fixation and secondary intramedullary nailing. J Bone Joint Surg Am. 1988;70:900–911. [PubMed] [Google Scholar]
- 5.Perry CR, Pearson RL, Miller GA. Accuracy of cultures of material from swabbing of the superficial aspect of the wound and needle biopsy in the preoperative assessment of osteomyelitis. J Bone Joint Surg Am. 1991;73:745–749. [PubMed] [Google Scholar]
- 6.Tornqvist H. Tibia nonunions treated by interlocked nailing: increased risk of infection after previous external fixation. J Orthop Trauma. 1990;4:109–114. doi: 10.1097/00005131-199004020-00001. [DOI] [PubMed] [Google Scholar]
- 7.Behrens F, Searls K. External fixation of the tibia. Basic concepts and prospective evaluation. J Bone Joint Surg Br. 1986;68:246–254. doi: 10.1302/0301-620X.68B2.3514629. [DOI] [PubMed] [Google Scholar]
- 8.Dedek T, Fiala O, Grmela M, Mihula A, Zahorak K, Ulybin B. Our contribution to the external fixation in traumatology. Sb Ved Pr Lek Fak Karlovy Univerzity Hradci Kralove. 1991;34:419–436. [PubMed] [Google Scholar]
- 9.Gustilo RB, Gruninger RP, Davis T. Classification of type III (severe) open fractures relative to treatment and results. Orthopedics. 1987;10:1781–1788. [PubMed] [Google Scholar]
- 10.Brumback RJ. Open tibial fractures: Current orthopaedic management. Instr Course Lect. 1992;41:101–117. [PubMed] [Google Scholar]
- 11.Hansis M, Hontzsch D. [Risk of infection and prevention of infection in changing the surgical procedure from fixateur externe to tibial intramedullary nailing] . Unfallchirurg. 1988;91:465–468. [PubMed] [Google Scholar]
- 12.Swiontkowski MF. The pinless fixator-Part II. Injury. 1994;25(Suppl 3) doi: 10.1016/0020-1383(94)90040-x. S-C1-2. [DOI] [PubMed] [Google Scholar]
- 13.Maurer DJ, Merkow RL, Gustilo RB. Infection after intramedullary nailing of severe open tibial fractures initially treated with external fixation. J Bone Joint Surg Am. 1989;71:835–838. [PubMed] [Google Scholar]
- 14.Remiger AR. Mechanical properties of the Pinless external fixator on human tibiae. Injury. 1992;23(Suppl 3):S28–43. doi: 10.1016/0020-1383(92)90005-d. [DOI] [PubMed] [Google Scholar]
- 15.Frigg R. The development of the Pinless external fixator: from the idea to the implant. Injury. 1992;23(Suppl 3):S3–8. doi: 10.1016/0020-1383(92)90003-b. [DOI] [PubMed] [Google Scholar]
- 16.Kulshrestha V. Incidence of infection after early intramedullary nailing of open tibial shaft fractures stabilized with pinless external fixators. Indian J Orthop. 2008;42:401–409. doi: 10.4103/0019-5413.43382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stene GM, Frigg R, Schlegel U, Swiontkowski M. Biomechanical evaluation of the Pinless external fixator. Injury. 1992;23(Suppl 3):S9–27. doi: 10.1016/0020-1383(92)90004-c. [DOI] [PubMed] [Google Scholar]
- 18.Remiger AR, Magerl F. The pinless external fixator-relevance of experimental results in clinical applications. Injury. 1994;25(Suppl 3) doi: 10.1016/0020-1383(94)90043-4. S-C15-29. [DOI] [PubMed] [Google Scholar]
- 19.Winkler H, Hochstein P, Wentzensen A. Experience with the pinless fixator in the treatment of fractures of the lower leg. Injury. 1994;25(Suppl 3) doi: 10.1016/0020-1383(94)90042-6. S-C8-14. [DOI] [PubMed] [Google Scholar]
- 20.Court-Brown CM, Keating JF, McQueen MM. Infection after intramedullary nailing of the tibia. Incidence and protocol for management. J Bone Joint Surg Br. 1992;74:770–774. doi: 10.1302/0301-620X.74B5.1527132. [DOI] [PubMed] [Google Scholar]
- 21.Haas N, Schutz M, Wagenitz A, Krettek C, Sudkamp N. Routine application of the pinless external fixator. Injury. 1994;25(Suppl 3) doi: 10.1016/0020-1383(94)90041-8. S-C3-7. [DOI] [PubMed] [Google Scholar]
- 22.Schutz M, Sudkamp N, Frigg R, Hoffman R, Stockle U, Haas N. Pinless external fixation. Indications and preliminary results in tibial shaft fractures. Clin Orthop Relat Res. 1998:35–42. [PubMed] [Google Scholar]
- 23.Xia L, Zhou J, Zhang Y, Mei G, Jin D. A metaanalysis of reamed versus unreamed intramedullary nailing for the treatment of closed tibial fractures. Orthopedics. 2014;37:e332–338. doi: 10.3928/01477447-20140401-52. [DOI] [PubMed] [Google Scholar]
- 24.Salem KH. Unreamed intramedullary nailing in distal tibial fractures. Int Orthop. 2013;37:2009–2015. doi: 10.1007/s00264-013-1998-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deleanu B, Prejbeanu R, Poenaru D, Vermesan D, Haragus H. Reamed versus unreamed intramedullary locked nailing in tibial fractures. Eur J Orthop Surg Traumatol. 2014;24:1597–1601. doi: 10.1007/s00590-013-1401-0. [DOI] [PubMed] [Google Scholar]


