Abstract
This study aimed to investigate the clinical application and efficacy of percutaneous kyphoplasty via unilateral pedicular approach with the reference of preoperative CT image data. 73 cases (a total of 112 vertebrae) with thoracic and lumbar osteoporotic vertebral compression fractures (OVCF) received in our department were collected in this study and underwent percutaneous kyphoplasty via unilateral pedicular approach directed by CT image measurement with the operative time and fluoroscopic times recorded. Visual analogue scale (VAS) and Oswestry disability index (ODI) were used to assess the pain status and functional activity before and after operation and at the last follow-up, while X-ray and CT image were used to measure the height of the injured spinal middle column and kyphotic Cobb angle before and after operation. 73 cases (112 vertebrae) underwent percutaneous kyphoplasty successfully. Cement leakage occurred in 7 cases without obvious neurological symptoms, and they were followed up for 10 to 60 months with the average of 23 months; adjacent vertebral refractures occurred in 3 cases during the follow-up, and their symptoms were relieved after the second surgery. There was significant difference in the height of the injured spinal middle column and kyphotic Cobb angle before and after operation (P<0.05); there was significant difference in preoperative and postoperative VAS score and ODI values (P<0.05). Postoperative CT image data showed that puncture paths of the 110 vertebrae were consistent with preoperative ones sketched using the CT image, and the consistent rate of preoperative and postoperative measurement data was 98%. All patients could ambulate with brace within 2 days after operation without serious complications. In conclusion, percutaneous kyphoplasty via unilateral pedicular approach guided by preoperative CT image data is effective in treatment of osteoporotic vertebral compression fractures, and it is convenient and safe with high puncture accuracy, shorter operative time and less radiation exposure for patients and operators.
Keywords: Percutaneous kyphoplasty, unilateral pedicular approach, vertebral compression fractures, CT image
Introduction
Percutaneous kyphoplasty (PKP) is a kind of minimally invasive spine operations in the treatment of osteoporotic vertebral compression fracture (OVCF), and its working principle is to expand the collapsed vertebrae with balloons, and then to inject bone cement into the vertebral body in order to correct kyphosis deformity with advantages of immediate pain relief, improvement in kyphosis and low possibility of cement leakage [1,2]. Nowadays, PKP for the treatment of OVCF has been widely applied in clinical because of easy and safe operation and less trauma to patients. PKP via bilateral pedicular approach is a classic mode of puncture, and it has advantages of uniformly distributed bone cement in vertebral body and disadvantages of long operative time and much X-ray exposure. With the gradual promotion of PKP surgery in clinical practices, the radiation injury to surgeons and patients during operation has gradually been concerned [3,4]. Therefore, in order to reduce the radiation exposure of X-ray, save the operation cost and reduce the complications caused by puncture, some scholars try to use PKP via unilateral pedicular approach to treat OVCF, and obtain a better outcome [5,6]. Related studies confirmed that injured vertebrae could obtain considerable stiffness and strength if puncture needle reached or crossed the vertebral midline and bone cement diffused to the contralateral side during PKP via unipedicular approach. These scholars suggested that the optimal target point in unipedicular PKP should be located in 1/3 anterior and middle region of the vertebral body, so bone cement could diffuse to the contralateral side with a satisfactory clinical outcome obtained [7-9].
Successful puncture can not only reduce the incidence of related complications, but also obtain good dispersion of bone cement in the vertebral body. However, the current PKP surgery via unipedicular approach in the clinical application is mainly based on the experience of operators, because pedicle morphology of each person is not the same, the operators may require multiple fluoroscopy adjustments in determining the puncture point, resulting in puncture injury as well as operators and patients absorbing a lot of radiation with serious injury to the body, which brings difficulty and risk to further clinical application of unipedicular PKP. In addition, osteoporotic vertebral compression fractures in elderly patients often combine with degenerative spinal scoliosis, kyphotic and rotational deformity and pedicle variation, which increase difficulty in puncture. Although spine navigation system can make the operation safe and accurate [10], its initial investment is large, so general hospitals are difficult in popularization. In clinical work, we have found that some key parameters, including the skin insertion site of the needle, the media inclination angle, and the candal inclination angle, can be obtained via preoperative simulated CT image measurement, which can guide unipedicular PKP surgery, so more accurate operative procedures can be obtained without increasing the cost of investment, which can increase the safety and success rate of unilateral puncture. In order to evaluate the operability and safety of PKP via unilateral pedicular approach guided by preoperative CT image data, this study retrospectively reviewed 73 cases of elderly patients with thoracic and lumbar OVCF treated with unipedicular approach PKP.
Subjects and methods
Subjects
73 cases (112 vertebrae) with OVCF received in our department from April 2009 to December 2013 were treated with PKP via unilateral pedicular approach. The 54 patients were composed of 17 males and 56 females, and all of them were in the 50-90 age range with the average of 70.8 years old. The injured vertebrae were T42, T56, T66, T78, T812, T97, T108, T119, T1215, L112, L212, L310 and L45. 46 cases of them suffered from single vertebral fracture, 17 cases of them suffered from bi-segment vertebral fractures, 8 cases with tri-segment vertebral fractures and 2 cases with quadri-segment vertebral fractures. In addition, low back pain was manifested in all patients with remission at supine position prior to surgery, and the pain got worse when changing position while the symptoms slightly reduced after supine rest. Physical examination showed tenderness and percussion pain in the corresponding segment of spinous process without nerve injury. Preoperative X-ray, CT, MRI and bone density examination confirmed fresh fractures in all patients, the basic integrity of the inner and posterior wall of vertebral pedicle, and no significant compression in spinal cord and nerve root. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Tongji Hospital. Written informed consent was obtained from all participants.
CT image measurement and surgical methods
CT image measurement was performed on the injured vertebrae of 72 patients by PACS system (Picture Archiving and Communication Systems) in Imaging Department of our hospital before operation, and several key parameters required in surgery, including the distance from the skin insertion site of the needle to the spinous process median line, the medial inclination angle and the candal inclination angle, were obtained (Figure 1).
Figure 1.
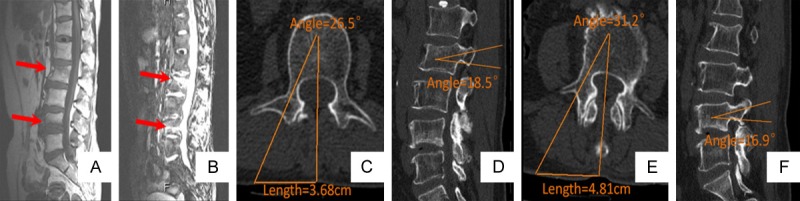
CT image measurement and surgical methods. A, B: L2 and L4 being fractured of a 61-year-old female patient through preoperative lumbar MRI; C-F: Several key parameters including the medial inclination angle and the caudal inclination angle in percutaneous kyphoplasty via unilateral approach about L2 and L4 being measured on pre-operative CT images.
General anesthesia was adopted in the surgery. Patients were placed at prone position with abdomen vacant, and then were performed for postural reduction, and C-arm fluoroscopy was used to determine the fractured vertebrae. Puncture procedures of unipedicular approach PKP based on preoperative image parameters: 1. determination of the skin insertion site of the needle: according to the distance from the skin insertion site of the needle to the spinous process measured before surgery, the puncture point was marked in the body surface with routine disinfection and draping, and 0.5 cm skin was incised at insertion site with a sharp blade; 2. determination of the osseous insertion site of the needle: as the needle continued deeply, when its end touched the bone structure behind the injured vertebra, the position of the needle end was determined via C-arm anteroposterior fluoroscopy to ensure that the puncture needle end was about 2-3 mm in the lateral margin of the outer wall of the pedicle; 3. determination of the direction of needle insertion: puncture needle was performed along the medial inclination angle and the candal inclination angle measured before surgery to 1/3 middle and anterior region of the vertebral body along the pedicle. When it reached the inner wall of the pedicle, the position of the needle was ensured to reach the posterior wall of the vertebral body via C-arm lateral fluoroscopy.
After good position of the needle was determined via C-arm two-angle fluoroscopy, the needle was removed. Next the dilated cannula and working cannula were implanted along the needle. A balloon was put into the vertebral cancellous bone along the working cannula with slowly injection of contrast agent into the balloon under the C-arm close surveillance for balloon dilatation. The contrast agent was extracted when vertebral height restored appropriately, and then the balloon was taken out when it retracted to a vacuum. Poly methyl methacrylate (PMMA, Italy Tecres SPA) was injected at low pressure with C-arm fluoroscopy, and the injection was stopped unless good dispersion of cement. Once leakage, stop surgery. Ejector sleeve and working cannula were removed after cement hardening. C-arm fluoroscopy was needed to monitor all surgical procedures (Figure 2). All patients needed postoperative conventional anti-osteoporosis medicines (calcium, vitamin D, and calcitonin). Postoperative X-ray and CT were performed for measuring the related parameters of the puncture path, which were compared with the preoperative data to verify the accuracy of the preoperative data (Figure 3). Disposable supplies for vertebroplasty and balloons were provided by Kaili Tai Medical Technology Co., Ltd, Shanghai, China.
Figure 2.
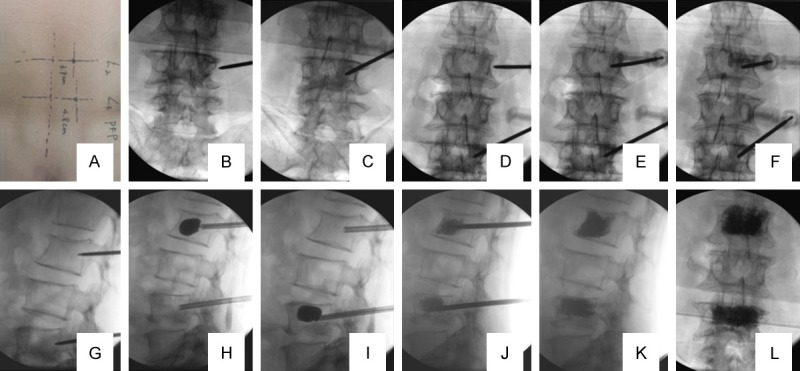
The key steps of PKP. A: Ascertaining the skin insertion site of the needle; B, D: Ascertaining the osseous insertion site of the needle; C, E-L: Performing the operation guided by the preoperative key parameters.
Figure 3.
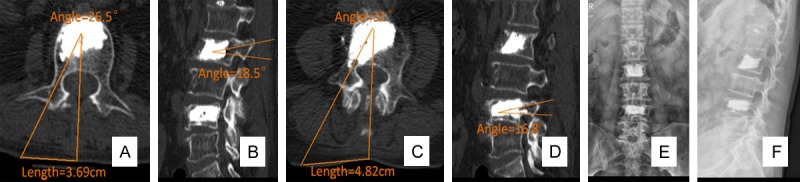
Postoperative X-ray and CT evaluation. A-D: The post-operative key parameters being consistent with the preoperative key parameters by CT image measurement; E, F: The X-ray films of the final follow-up.
Evaluation of surgical treatment
Visual analogue scale (VAS) was used to assess the pain status before and after surgery and the final follow-up respectively (VAS score being from 0 to 10, 0 for pain free, 10 points for the maximum pain). Oswstry disability index (ODI) was used to evaluate the level of functional impairment in patients before and after surgery.
Statistical analysis
All statistical analyses were performed using SPSS 17.0. Comparison of VAS score and ODI score data at different time points was analyzed, and the height of the injured spinal middle column and kyphotic Cobb angle were compared at pre-operation, post-operation and the final follow-up using paired t test. The data was showed as the mean ± SD. P<0.05 was statistically significant.
Results
73 cases (112 vertebrae) with thoracic and lumbar OVCF were admitted with percutaneous kyphoplasty successfully. The time of single-vertebral surgery was 25-30 min with the average of 27 ± 2 min; the times of the X-ray were 25-40 with the average of 29 ± 4, and 5-15 ml bleeding with the average of 10 ± 3 ml. The injection volume ranged 3-5 ml in the thoracic vertebrae and 5-9 ml in the lumbar vertebrae with the average of 5.3 ± 1.5 ml.
In the 73 patients, the symptoms of 69 patients (94.52%) had complete remission, 4 patients (5.48%) had partial remission and the effective rate was 100%. VAS scores and ODI values at postoperation and the last follow-up were statistical significant compared with preoperative data (P<0.05). Postoperative measurement results showed that puncture paths of the 110 vertebrae were consistent with preoperative ones sketched using the CT image, and the consistent rate of preoperative and postoperative measurement data was 98%.
All patients could ambulate with brace within 2 days after operation. Cement leakage occurred in 7 cases: 1 case with leakage into the spinal canal, 1 case with leakages into paravertebral vein, 2 cases with leakage into the intervertebral disc and 3 leakages into the paraspinal soft tissues. There was no significant neurological dysfunction.
Postoperative X-ray showed that the fracture was basically reset, and the cement distribution crossed the midline of the vertebral body. The height of the injured spinal middle column and kyphotic Cobb angle were statistical significant compared with preoperative data (P<0.05; Table 1).
Table 1.
Comparison of the kyphotic Cobb angle, height of the middle part of injured vertebrae, ODI and VAS scores before surgery, after surgery and final follow-up
| Items | Preoperative | Postoperative 2 days | Final follow-up |
|---|---|---|---|
| Cobb angle (°) | 11.03 ± 7.86 | 8.24 ± 6.08* | 8.21 ± 5.98* |
| Height of the middle part of injured vertebrae (cm) | 1.61 ± 0.41 | 1.76 ± 0.35* | 1.71 ± 0.30* |
| ODI score | 46.4 ± 3.1 | 20.1 ± 3.5* | 13.5 ± 2.9* |
| VAS score | 8.81 ± 0.88 | 2.21 ± 0.75* | 2.34 ± 0.44* |
Note: Compared with pre-operative data;
P<0.05.
73 patients in total were followed up for 10-60 months with the average of 23 months, and 3 of them sustained new adjacent vertebral fractures at the 2nd, 6th, 10th month respectively during follow-up with fracture healing after additional surgery.
Discussion
PKP has been widely recognized with the advantages of relieving pain, regaining the height of the fractured vertebra and stabilizing the fractured vertebra as well as making patients early ambulant. However, as for specific procedures of PKP surgery, there are still many surgeons who have different views, and some of them use unilateral pedicle puncture while the others adopt bilateral pedicle puncture. Which approach is more safe and effective and can bring greater benefits to patients, and both issues have been controversial [11,12]. At present, more generally accepted view is unipedicular approach PKP surgery, and its optimal target location was 1/3 anterior and middle region of the vertebral body as well as bone cement can diffuse to the contralateral side, which could obtain the same satisfactory clinical outcome as bipedicular approach PKP.
Traditionally, the determination of the puncture path is based on the experience of the surgeon, the C arm machine is used for fluoroscopy positioning of the center point on the pedicle with making a mark. In general, accurate positioning requires multiple fluoroscopies. This study chose the intersection point of spinous process and the maximum section of the pedicle as the anchor point on CT-scanning film, and 1/3 anterior and middle region of the vertebral body as the optimal target location, which provided a more accurate point marker rather than a surface marker for unipedicular PKP. Accurate measurement of the distance from the skin insertion site of the needle to the spinous process and the medial inclination angle was to determine the path of puncture needle. The best caudal inclination was the angle between vertebral inferior endplate and the linked connection from the middle point of pedicle to the anterior lower margin of vertebral body via lateral fluoroscopy [7], and the height of the fractured vertebra was fully regained in this position. In practice, accurate location of the osseous insertion site of the needle is important, and if the position deviates, puncture needle can not reach the target site and easily break the inner wall of the pedicle resulting in spinal cord or nerve damage. Measurement of the puncture path of the injured vertebral body showed that the osseous insertion site was located in about 2-3 mm in the lateral margin of the outer wall of the pedicle. With determination of the osseous insertion site and preoperative measurement data, unipedicular PKP could be safely conducted, meanwhile, the puncture complications were reduced and its clinical efficacy was ensured.
In this study, patients treated with unipedicular PKP gained immediate relief pain and significant improvement of vertebral height, posterior convex angle and disability index compared with preoperative data. In respect of operative time and X-ray radiation exposure, the results showed that the average operative time of single vertebra was 27 ± 2 min and its average fluoroscopy times was 29 ± 4 for 112 fractured vertebrae in total accepted unipedicular PKP, which was superior to 200 cases in our department treated with bipedicular PKP with the average operative time of 42 ± 15 min and the average fluoroscopy times of 58 ± 18 as well as to the results of Wang et al. [13] with the average operation time of 45 ± 16 min and fluoroscopy times of 37 ± 12. Above advantages had the following reasons: ① Each patient underwent CT image measurement with simulation of puncture path. As for patients with vertebral pedicle deformity, such as small diameter of pedicle, PKP via bilateral pedicular approach or via lateral transpedicular approach, instead of unipedicular approach PKP, was chosen before surgery. ② Several key parameters of the skin insertion site, the osseous insertion site, the medial inclination angle and the candal inclination angle were obtained based on preoperative data of CT image measurement. And under the C-arm monitoring, effective puncture was achieved with 5-6 times of X-ray, thus rarely adjusting. ③ Because the direction and location of the puncture was accurate, only 3-4 fluoroscopy times were needed for replacement of working cannula. ④ The balloon was placed according to preoperative measurement data, and most of them crossed the vertebral midline. After about 2-3 ml dilation, the balloon was taken out with 3-4 fluoroscopy times. ⑤ High viscosity of bone cement was chosen and injected in the paste period. The total injection volume ranged 3~5 ml in the thoracic vertebrae and 5~9 ml in the lumbar vertebrae with slow injection under C-arm monitoring to prevent the leakage into the spinal canal, paravertebral vein and intervertebral disc.
Unipedicular approach PKP can reduce operative time and X-ray radiation exposure as well as the damage to surgeons and patients. However, patients’ safety and fewer complications are taken as the prerequisite for surgery, so fluoroscopy for the key steps can not be omitted, otherwise serious complications will be caused. In our study, 7 cases in total suffered from cement leakage: 1 case with leakage into the spinal canal, 1 case with leakage into paravertebral vein, 2 cases with leakage into the intervertebral disc and the remaining 3 cases with leakage into the paraspinal soft tissues, and the amount of cement leakage was less 0.5 ml, meanwhile, there were no significant neurological dysfunction in above patients, because the injection of cement was strictly observed. The experience of the author showed that the high-risk periods were respectively after the injection of 1.5 ml cement into the middle thoracic vertebrae, after the injection of 3ml cement into the lower thoracic vertebrae, and after the injection of 5 ml cement into the lumbar vertebrae, which should be closely monitored.
Cement leakage is a common complication during bone cement perfusion, and it can leak into the spinal canal through the crack in the fractured vertebra, the inner wall of impaired pedicle and the nutrient vessels in the realm of the vertebrae [14], which can cause severe neurological dysfunction. Once such complications occur, emergency surgery is needed for oppression relief. Papadopoulos et al. [5] showed that the incidence of cement leakage in unipedicular approach PKP was 10.73%, while Wang et al. [13] showed the rate in the study was 12.9%. In this study, 7 of 112 vertebrae suffered cement leakage with the incidence of 6.25%, which was slightly lower than that reported in the literature. According to our experience, the prevention of bone cement leakage was summarized as the following: a) For patients with fractured end plate, the puncture site should be far away from the fractured end plate and the injection speed of cement was not fast; b) After the success of puncture, the cut was packed with a small piece of hemostatic gauze and the front wall was sealed; c) The times of X-ray increased correspondingly when bone cement diffused to 1/4 posterior vertebral body, and the procedures were monitored with C-arm; d) Seizing the injection timing of cement was important, and it was the paste period; e) Once leakage, stop surgery. Multiple injections or additional injection was adopted for treating early leakage; f) After the completion of the bone cement injection, the cannula was closed using solid push rod; g) After the solidification pf bone cement, the cannula was pulled out with rotation. As for adjacent vertebral refractures, Li et al. [15] showed that there was no significant difference between unilateral and bilateral puncture. In this study, only 3 cases suffered from adjacent vertebral refractures and gained fracture healing after surgical treatment, and severe osteoporosis with multi-segmental fractures in the 3 cases was the reason of their additional fractures. In conclusion, all cases in this study had a satisfied outcome without severe complications, such as neurological and spinal cord injury and pulmonary embolism.
73 cases of elderly patients with thoracic and lumbar OVCF treated with unipedicular approach PKP were retrospectively reviewed in this study, and the results showed that unilateral approach PKP was applied for most of OVCF patients, especially for mild or moderate thoracolumbar vertebral compression fractures with the compression less than 1/2 of the vertebral height. Unilateral PKP should be used in the treatment of multiple OVCF to reduce radiation exposure, while bilateral PKP was chosen for treating patients with obese or the compression more than 1/2 of the vertebral height, and this was because more cement could be injected via bilateral approach to improve the resistance to compression of vertebral body and reduce the risk of secondary collapse and spine kyphosis of injured vertebrae. In addition, PKP via bilateral pedicular approach or via lateral transpedicular approach was chosen for patients with very small vertebral pedicle of spine, because the 1/3 anterior and middle region of the vertebral body, which was the optimal target location, was difficult to reach via unipedicular puncture [16], while PKP via transcostovertebral approach was adopted for thoracic OVCF patients with small pedicle, which also could achieve a good clinical outcome.
In conclusion, Percutaneous kyphoplasty via unilateral pedicular approach guided by preoperative CT image data is effective in treatment of thoracic and lumbar osteoporotic vertebral compression fractures, and it is convenient and safe with high puncture accuracy, shorter time and less radiation exposure for patients and surgeons. Its clinical results were satisfactory, so it is worth further promotion in clinical practice. However, because of the small sample size, short follow-up time and limited reference value of the relevant measurement data, therefore, it still needs a large number of muti-center and prospective studies for the complications of PKP via unilateral pedicular approach.
Acknowledgements
This study was supported by the scientific research project of Shanghai Municipal Health Bureau (No. 2009138).
Disclosure of conflict of interest
None.
References
- 1.Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976) 2001;26:1511–1515. doi: 10.1097/00007632-200107150-00002. [DOI] [PubMed] [Google Scholar]
- 2.Chang X, Lv YF, Chen B, Li HY, Han XB, Yang K, Zhang W, Zhou Y, Li CQ. Vertebroplasty versus kyphoplasty in osteoporotic vertebral compression fracture: a meta-analysis of prospective comparative studies. Int Orthop. 2015;39:491–500. doi: 10.1007/s00264-014-2525-5. [DOI] [PubMed] [Google Scholar]
- 3.Mroz TE, Yamashita T, Davros WJ, Lieberman IH. Radiation exposure to the surgeon and the patient during kyphoplasty. J Spinal Disord Tech. 2008;21:96–100. doi: 10.1097/BSD.0b013e31805fe9e1. [DOI] [PubMed] [Google Scholar]
- 4.Srinivasan D, Than KD, Wang AC, La Marca F, Wang PI, Schermerhorn TC, Park P. Radiation safety and spine surgery: systematic review of exposure limits and methods to minimize radiation exposure. World Neurosurg. 2014;82:1337–1343. doi: 10.1016/j.wneu.2014.07.041. [DOI] [PubMed] [Google Scholar]
- 5.Papadopoulos EC, Edobor-Osula F, Gardner MJ, Shindle MK, Lane JM. Unipedicular balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures: early results. J Spinal Disord Tech. 2008;21:589–596. doi: 10.1097/BSD.0b013e31815d6997. [DOI] [PubMed] [Google Scholar]
- 6.McGirt MJ, Parker SL, Wolinsky JP, Witham TF, Bydon A, Gokaslan ZL. Vertebroplasty and kyphoplasty for the treatment of vertebral compression fractures: an evidenced-based review of the literature. Spine J. 2009;9:501–508. doi: 10.1016/j.spinee.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 7.Hoh BL, Rabinov JD, Pryor JC, Hirsch JA. Balloon kyphoplasty for vertebral compression fracture using a unilateral balloon tamp via a uni-pedicular approach: technical note. Pain Physician. 2004;7:111–114. [PubMed] [Google Scholar]
- 8.Chen B, Li Y, Xie D, Yang X, Zheng Z. Comparison of unipedicular and bipedicular kyphoplasty on the stiffness and biomechanical balance of compression fractured vertebrae. Eur Spine J. 2011;20:1272–1280. doi: 10.1007/s00586-011-1744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang XM, Wu TL, Xu HG, Wang H, Liu P, Wang LT, Chen XW. Modified unilateral transpedicular percutaneous vertebroplasty for treatment of osteoporotic vertebral compression fractures. Orthop Surg. 2011;3:247–252. doi: 10.1111/j.1757-7861.2011.00154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Izadpanah K, Konrad G, Südkamp NP, Oberst M. Computer navigation in balloon kyphoplasty reduces the intraoperative radiation exposure. Spine (Phila Pa 1976) 2009;34:1325–1329. doi: 10.1097/BRS.0b013e3181a18529. [DOI] [PubMed] [Google Scholar]
- 11.Tohmeh AG, Mathis JM, Fenton DC, Levine AM, Belkoff SM. Biomechanical efficacy of unipedicular versus bipedicular vertebroplasty for the management of osteoporotic compression fractures. Spine (Phila Pa 1976) 1999;24:1772–1726. doi: 10.1097/00007632-199909010-00004. [DOI] [PubMed] [Google Scholar]
- 12.Chen L, Yang H, Tang T. Unilateral versus bilateral balloon kyphoplasty for multilevel osteoporotic vertebral compression fractures: a prospective study. Spine (Phila Pa 1976) 2011;36:534–540. doi: 10.1097/BRS.0b013e3181f99d70. [DOI] [PubMed] [Google Scholar]
- 13.Wang Z, Wang G, Yang H. Comparison of unilateral versus bilateral balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. J Clin Neurosci. 2012;19:723–726. doi: 10.1016/j.jocn.2011.08.023. [DOI] [PubMed] [Google Scholar]
- 14.Chung HJ, Chung KJ, Yoon HS, Kwon IH. Comparative study of balloon kyphoplasty with unilateral versus bilateral approach in osteoporotic vertebral compression fractures. Int Orthop. 2008;32:817–820. doi: 10.1007/s00264-007-0439-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li LH, Sun TS, Liu Z, Zhang JZ, Zhang Y, Cai YH, Wang H. Comparison of unipedicular and bipedicular percutaneous kyphoplasty for treating osteoporotic vertebral compression fractures: a meta-analysis. Chin Med J (Engl) 2013;126:3956–3961. [PubMed] [Google Scholar]
- 16.Wang S, Wang Q, Kang J, Xiu P, Wang G. An imaging anatomical study on percutaneous kyphoplasty for lumbar via a unilateral transverse process-pedicle approach. Spine (Phila Pa 1976) 2014;39:701–706. doi: 10.1097/BRS.0000000000000243. [DOI] [PubMed] [Google Scholar]


