Abstract
Objective: To evaluate short-term and medium-term outcomes of microendoscopy-assisted minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) and open TLIF for lumbar degenerative disease. Methods: In this prospective, randomized control study, 50 cases received microendoscopy-assisted MIS-TLIF (MIS group), while another well-matched 50 cases accepted open TLIF (open group). Parameters between both groups, including surgical duration, intraoperative blood loss and radiologic exposure, postoperative analgesic usage and ambulatory time, visual analogue scale (VAS) for back and leg, functional scores, self-evaluation of surgical outcome (modified MacNab criteria), interbody fusion rate, adjacent segment degeneration (ASD) rate, as well as complication incidence were compared at 1 month and 24 months postoperatively. Results: Intraoperative blood loss and postoperative analgesic usage were significantly reduced in MIS group (P<0.05). Patients undergoing microendoscopy-assisted MIS-TLIF were able to ambulate earlier postoperatively than those receiving open TLIF (P<0.05). However, it showed prolonged surgical duration and enhanced radiologic exposure in MIS group (P<0.05). At 1 month postoperatively, MIS group was associated with more improvement of VAS and functional scores compared with open group (P<0.05). While at 24 months postoperatively, both groups revealed similar VAS and functional scores (P>0.05). Excellent and perfect scale rating by modified MacNab criteria, interbody fusion rate, ASD rate and complication incidence between both groups were nearly the same (P>0.05). Conclusions: Microendoscopy-assisted MIS-TLIF owns advantages of less iatrogenic injury, decreased blood loss, reduced analgesic usage and earlier rehabilitation, while it has drawbacks of more surgical duration and radiologic exposure. It is superior than open TLIF in terms of short-term clinical outcomes and has similar medium-term clinical outcomes.
Keywords: Minimally invasive, transforaminal lumbar interbody fusion, fixed-diameter endoscopy, lumbar degenerative disease
Introduction
Recent years have witnessed the widespread application of minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) for lumbar degenerative disease [1-3], while most researches are associated with use of expandable dilator or retractor to create a muscular tunnel to the pedicle entry point [4-8]. Since microendoscopic discectomy (MED) has become an extremely developed technique [9-11], it is able to extend its application to canal decompression and interbody fusion [3,12]. Isaacs published the first report comparing patients receiving microendoscopic TLIF with those undergoing posterior lumbar interbody fusion and found the former owns clinical benefits of decreased blood loss, hospital stay and postoperative narcotic agent use [12]. However, some shortcomings still existed in previous studies, such as small sample size, lack of radiation evaluation and self-evaluation of surgical outcome. In order to further illustrate clinical outcomes of microendoscopy-assisted MIS-TLIF, this prospective, randomized control study was conducted with more detailed evaluations in larger sample size.
Materials and methods
General data
A total of 100 single-level cases, who were refractory to conservative treatments, such as medication and physical therapy for at least six weeks were included in this study. All patients were randomly assigned into minimally invasive group (MIS group) of 50 cases or open group of remaining 50 cases, receiving microendoscopy-assisted MIS-TLIF or open TLIF respectively. In this study, sample size calculation was based on tendencies of preliminary test results (8 cases for either group), meanwhile, random number method was used during randomization procedure. Inclusion criteria were as follows: lumbar disc herniation with segmental instability; lumbar spinal canal stenosis with potential for intraoperative instability; lumbar spondylolisthesis (less than Meyerding Grade II). In this series, all open and minimally invasive surgeries were performed by one senior surgeon, who is proficient in both surgical techniques, meanwhile, all cases were on the plateau stage of this surgeon’s learning curves. Our study was approved by institutional ethic committee of the hospital and informed consents were obtained from all participants.
Surgical procedures for microendoscopy-assisted MIS-TLIF
Following general anesthesia, patient was evenly positioned prone on the radiolucent table. Under fluroscopic guidance, pedicle images of the desired vertebrae were confirmed and then corresponding paracentral 2.0 cm transverse incisions were made to insert Jamshidi needle. It was first placed at the lateral margin of the pedicle image (at three or nine o’clock position) and then slowly advanced into the center of pedicle image, Inner stylet of Jamshidi needle was removed to allow kirschner wire to be inserted into the pedicle. Dilators were sequentially placed over each other through the incision, and then working cannula was inserted. Partial facetectomy and laminectomy, along with removal of ligamentum flavum were performed to accomplish canal decompression. Then working channel was tilted to the contralateral side where indicated through the same incision to perform further decompression. Following removal of intervertebral disc and preparation of end plates, interbody cage filled with autologous bone and the remaining bone particles were medially packed into intervertebral space through working cannula. Then pedicle screws and rods were inserted through the same incision percutaneously. Bilateral compression was applied before final tightening of the pedicle screw-rod construct. Finally, closure in layers was performed after wound haemostasis and irrigation. For spondylolisthesis cases, contralateral placement of pedicle screws and rods were performed before cage implantation.
Surgical procedures for open TLIF
Patient under general anesthesia was maintained in prone position. Through a midline incision, the fascia was incised and paraverterbral muscles were mechanically detached from the bony structure, then bilateral pedicle screws were inserted, followed by bilateral laminectomy and facetectomy. Discectomy was performed and endplates were prepared through curetting. After placement of autologous bone graft and interbody cage filled with it, rods were inserted and tightened. Haemostasis and irrigation were done before suturing the wound.
Clinical assessment and statistical analysis
One independent assessor, who was blinded to all included cases evaluated the following parameters. Surgical duration, intraoperative blood loss and radiologic exposure (fluroscopic time and skin entrance dose), postoperative ambulatory time and non-steroidal anti-inflammatory drug (NSAID) usage between both groups were compared using independent t-test. Based on visual analogue score (VAS) for back and leg, Japanese Orthopaedics Association score (JOA), Oswestry disability index (ODI) at 1 month and 24 months postoperatively, comparisons on clinical outcomes inter-groups and intra-group were tested by independent and paired t-test respectively. At 24 months postoperation, modified MacNab criteria was applied to assess patients’ satisfaction, meanwhile, adjacent segment degeneration (ASD) cephalad or caudad to the fusion segment, as well as interbody fusion were evaluated using the criteria introduced by Ghiselli and Cook [13,14]. Chi-squared test was applied to compare complication incidence and aforementioned categorical data. In this study, statistical analysis was performed using SPSS version 17.0 and significance was defined as P<0.05.
Results
Both groups were well matched in terms of preoperative demographic data (P>0.05, Table 1). MIS group was associated with less intraoperative blood loss and postoperative NASID usage compared with open group (P<0.05, Table 2). Patients who underwent microendoscopy-assisted MIS-TLIF were able to ambulate earlier postoperatively (2.1 days versus 4.0 days, P<0.05, Table 2). However, there were more surgical duration, fluroscopic time and skin entrance dose in MIS group versus open group (P<0.05, Table 2). In this study, all cases were regularly followed up. At 1 month postoperatively, both groups showed significant improvement in terms of VAS (back and leg), JOA and ODI compared with preoperation (P<0.05, Table 3), while MIS group was associated with more improvement (P<0.05, Table 3). At 24 months postoperatively, when comparing VAS (back and leg), JOA and ODI with those at 1 month postoperation, it also revealed statistical difference (P<0.05, Table 3), while these functional scores between both groups demonstrated no significant difference (P>0.05, Table 3). According to modified MacNab criteria, there were 48 cases ranking excellent or perfect in MIS group, however, there were only 46 cases rated as excellent or perfect in open group, although showing no statistical significance (P>0.05, Table 3). ASD rate was 12% in MIS group and 18% in open group, also demonstrating no statistical significance (P>0.05, Table 3). Interbody fusion rate between MIS group and open group was nearly the same (88% versus 90%, P>0.05, Table 3, Figure 1).
Table 1.
Preoperative Comparison of Demographic Data Between Minimally Invasive and Open Group
| Minimally invasive TLIF | Open TLIF | p value | |
|---|---|---|---|
| Age (year-old) | 58.0±13.4 | 56.1±11.0 | 0.439 |
| Gender (Male/Female) | 18/32 | 23/27 | 0.309 |
| Operated level | |||
| L2-L3 | 0 | 1 | 1.000 |
| L3-L4 | 1 | 2 | 1.000 |
| L4-L5 | 39 | 41 | 0.617 |
| L5-S1 | 10 | 6 | 0.275 |
| Disease etiology | |||
| Spinal stenosis | 24 | 28 | 0.423 |
| Spondylolisthesis | 20 | 17 | 0.534 |
| Disc herniation with segmental instability | 6 | 5 | 0.749 |
| Major comorbidities (hypertension, diabetes, hyperlipemia and coronary heart disease) | |||
| One comorbidity | 14 | 11 | 0.488 |
| Two comorbidities | 4 | 4 | 1.000 |
| Three comorbidities | 2 | 3 | 1.000 |
| Four comorbidities | 1 | 1 | 1.000 |
| Clinical evaluation | |||
| VAS (back) | 5.1±1.7 | 5.4±1.2 | 0.216 |
| VAS (leg) | 5.8±1.5 | 5.5±1.2 | 0.393 |
| JOA | 13.9±3.2 | 14.9±3.4 | 0.137 |
| ODI | (50.7±14.5)% | (49.0±11.3)% | 0.501 |
TLIF indicates transforaminal lumbar interbody fusion; VAS, visual analogue score; JOA, Japanese. Orthopaedics Association score; ODI, Oswestry disability index.
Table 2.
Perioperative comparison between minimally invasive and open group
| Minimally invasive TLIF | Open TLIF | p value | |
|---|---|---|---|
| Operative duration (minute) | 178.5±17.7 | 146.3±18.8 | 0.000 |
| Intraoperative blood loss (ml) | 183.9±24.2 | 490.7±75.3 | 0.000 |
| Intraoperative fluroscopic time (second) | 59.8±4.8 | 22.4±3.4 | 0.000 |
| Intraoperative skin entrance dose (mGy) | 136.6±12.5 | 61.0±7.2 | 0.000 |
| Postoperative ambulatory time (day) | 2.1±0.5 | 4.0±0.5 | 0.000 |
| Postoperative NASID use (mg) | 44.2±6.5 | 65.2±9.1 | 0.000 |
NASID indicates non-steroidal anti-inflammatory drug.
Table 3.
Clinical outcome comparison between minimally invasive and open group
| Minimally invasive TLIF | Open TLIF | p value | |
|---|---|---|---|
| VAS (back) | |||
| 1 month postoperation | 2.5±1.0※ | 3.2±0.7※ | 0.000 |
| 24 months postoperation | 0.8±0.8※,# | 1.1±1.1※,# | 0.117 |
| VAS (leg) | |||
| 1 month postoperation | 2.7 ± 0.9※ | 3.2±0.8※ | 0.009 |
| 24 months postoperation | 0.8±0.8※,# | 0.9±0.9※,# | 0.291 |
| JOA | |||
| 1 month postoperation | 19.5±1.7※ | 18.5±2.7※ | 0.033 |
| 24 months postoperation | 25.2±2.1※,# | 25.5±1.8※,# | 0.483 |
| ODI | |||
| 1 month postoperation | (29.2±10.2)%※ | (33.6±10.0)%※ | 0.024 |
| 24 months postoperation | (11.6±6.3)%※,# | (12.0±6.2)%※,# | 0.754 |
| Modified MacNab | |||
| Perfect or Good | 48 | 46 | 0.674 |
| Fair or Poor | 2 | 4 | 0.674 |
| Interbody fusion rate | 44/50 | 45/50 | 0.749 |
| ASD rate | 6/50 | 9/50 | 0.401 |
| Complication rate | 5/50 | 4/50 | 1.000 |
ASD indicates adjacent segment degeneration;
Comparing with preoperation, P<0.05;
Comparing with 1 month postoperation, P<0.05.
Figure 1.
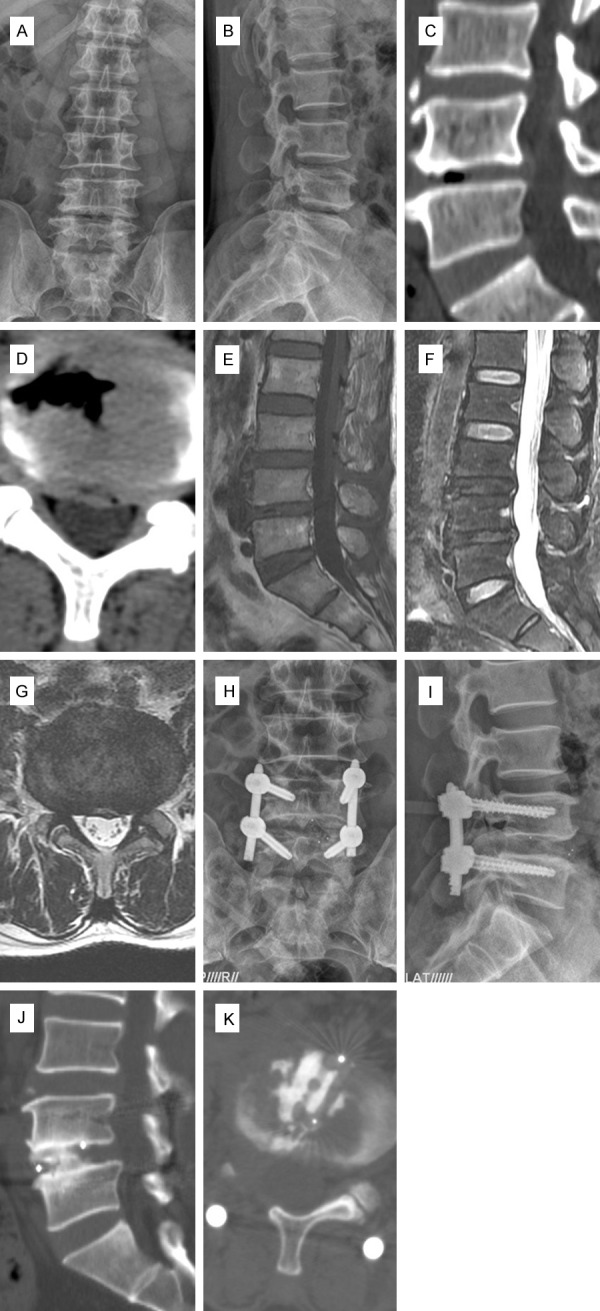
Preoperative radiographs of one 58 year-old male suffering from back pain for ten years and neurological intermittent claudication for one year (VAS: 7, JOA: 11, ODI: 58%), demonstrating discogenic back pain and pathological lumbar canal stenosis at L4-5 level (A-G). Microendoscopy-assisted MIS-TLIF accomplished bilateral canal decompression via the right approach, and patient’s symptoms relieved significantly following surgery (VAS:1, JOA:25, ODI:8%) (H-I). Lumbar CT scan demonstrated satisfactory interbody fusion during postoperative follow-up (J-K).
When referring to perioperative complication, there were 5 cases in MIS group. For one patient, the anterior cortical wall of operated vertebrae was penetrated by kirschner wire due to severe osteoporosis, however, no vascular or visceral injury was observed. For another patient, operated level was mistaken by the surgeon and corrected immediately. Intraoperative dural laceration occurred in one patient, and well recovery was acquired following conservative treatments. One of the remaining two patients suffered from urinary infection and the other patient showed delirium postoperatively, and they both got recovery following medications. For 4 complications in open group, there was one case of displaced bone graft compressing nerve root, leading to restricted limb motion postoperatively, which was well managed conservatively. One of the remaining three patients suffered from pneumonia and the other two patients showed delirium postoperatively. All of them underwent conservative managements and recovered well. Thus, perioperative complication rate was 10% for MIS group and 8% for open group, showing no significant difference (P>0.05, Table 3).
Discussion
In this research, microendoscopy-assisted MIS-TLIF was accomplished only through small paracentral incisions, thus avoiding wild stripping of paraspinal soft tissues and preserve posterior midline spinal structures [15,16]. Previous study has demonstrated that excessive stripping of ending points of multifidus and damage to posterior ramus of spinal nerves can lead to denervation of deep back muscles and scarring of muscle fibers, which then ends up with decreased back muscle function and flaws postoperative recovery, so minimally invasive procedure for lumbar spinal fusion owns benefit of less soft tissue injury [15]. The incision for placement of access system could be also used for pedicle screw insertion, so extra incision was not required. These advantages lead to further decreased iatrogenic damage to soft tissues [16]. Therefore, less intraoperative blood loss was found in minimally invasive procedure. Postoperatively, the amount of postoperative analgesic usage following minimally invasive technique was significantly reduced based on the superiority of decreased intraoperative injury. Patients receiving microendoscopy-assisted MIS-TLIF also ambulated earlier when comparing with open TLIF, thus may decrease the incidence of limb venous thrombosis. Modified MacNab assessment showed microendoscopy-assisted MIS-TLIF was associated with little higher rate of perfect or good scale, and ASD incidence following minimally invasive surgery was also slightly less than that in open group. All these results clearly elucidate clinical benefits of microendoscopy-assisted MIS-TLIF. In this series, patients who would undergo minimally invasive procedure had little more severe symptoms preoperatively, revealing higher VAS for leg, ODI and lower JOA. While patients receiving this surgical technique revealed more relief of symptoms at 1 month postoperatively, showing greater improvement of functional scores in comparison with patients undergoing open TLIF. However, functional scores between both groups were of no statistical difference at 24 months postoperatively. This fact demonstrates clinical advantages of microendoscopy-assisted MIS-TLIF is within short-term period postoperation, which is similar with previous reports [5,16,17].
In this study, more fluroscopic time and skin entrance dose were found in microendoscopy-assisted MIS-TLIF. For the majority of its surgical procedures, including inserting Jamshidi needle and pedicle screw, placing rod and working tunnel, as well as observing interbody cage position are all under fluroscopic guidance. Compared with the fact that most surgical procedures of open TLIF are able to be accomplished under direct vision, it shows more technically challenging for microendoscopy-assisted MIS-TLIF, and this may be its internal drawback. However, as with all new surgical techniques, following dedicated repetition and experience acquisition of surgeon, radiologic exposure of microendoscopy-assisted MIS-TLIF may be decreased. When referred to perioperative complication, there were 5 cases in minimally invasive surgery and 4 cases in open surgery respectively, almost the same with previous reports [7,18]. While nearly half of them are not involved with surgical technique and would be avoided if promptly observed and properly managed. As to technical complication, well preparation before operation and meticulous manipulation during surgery may be the best prophylaxis [7]. On one hand, MIS-TLIF is associated with less tissue injury during operation and allows patients to ambulate earlier after operation, thus reducing perioperative complication rate [19,20]; on the other hand, patients receiving MIS-TLIF had older age and more comorbidities in this series, and these facts are generally considered to be responsible for higher perioperative complication rate [21,22]. So considering aforementioned facts in totality, one cannot assume one fact cancels out the other, and final outcome should be weighted by both points. Like most other researches [17,23,24], this study also showed longer operating time for MIS-TLIF, and the reason may be due to increased technical challenge of performing minimally invasive surgery. While one study revealed shortened time length of MIS-TLIF in comparison with open TLIF [16]. Varying proficiency levels of surgeons from different agencies may be accountable for this contradictory.
From this study, it is fully demonstrated that canal decompression and autograft bone implantation are able to be accomplished using microendoscopy access system. Diameter of its working cannula is only 20 mm, smaller than other dilatable access systems available now, leading to reduced incision. During surgical manipulation, dilatation using fixed-diameter working cannula is in the blunt way and located just around upper part of muscular layer tunnel, so the traction and dilatation imposed on paraspinal soft tissues, such as muscle and fascia can be decreased to some extent. With the assistance of microendoscopy image system, operative field can be amplified, providing surgeons with better visibility so that safety of surgical procedure is more guaranteed, thus minimizing the possibility of accidental injury [25]. Finally, if more extensive canal decompression is required, the tubular working channel can be angled directly to facilitate direct decompression of other zones, such as contralateral nerve root canal [16]. On account of these advantages, it is believed that fixed-diameter microendoscopy tunnel will gain more popularity over expandable dilator when performing MIS-TLIF.
Some drawbacks of our study should be acknowledged. First, due to lack of thin-section helical computed tomography (CT) scan of all patients at final radiologic follow-up, we only evaluated interbody fusion through plain film image, so there may be some deviations compared with fusion assessment using CT scan. Second, some parameters measuring functional improvement, such as ambulatory time and modified MacNab evaluation may be potentially affected by ward nursing, patient’s own expectation and their emotional state, causing outcome bias to some extent. However, these limitations are not considered to generate obvious deviation to conclusion.
In conlusion, microendoscopy-assisted MIS-TLIF provides patients with more beneficial short-term and comparable medium-term clinical outcomes compared with open TLIF. Although it is associated with increase of operative duration and intraoperative radiologic exposure, microendoscopy-assisted MIS-TLIF is superior than open TLIF in terms of less iatrogenic injury, reduced intraoperative blood loss, decreased postoperative analgesic usage and earlier rehabilitation.
Acknowledgements
This study was supported by Sun Yat-sen University Clinical Research 5010 Program (grant no. 2013006).
Disclosure of conflict of interest
None.
References
- 1.Tian W, Xu YF, Liu B, Liu YJ, He D, Yuan Q, Lang Z, Han XG. Computer-Assisted Minimally Invasive Transforaminal Lumbar Interbody Fusion May Be Better than Open Surgery for Treating Degenerative Lumbar Disease. J Spinal Disord Tech. 2014 doi: 10.1097/BSD.0000000000000165. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Niesche M, Juratli TA, Sitoci KH, Neidel J, Daubner D, Schackert G, Leimert M. Percutaneous pedicle screw and rod fixation with TLIF in a series of 14 patients with recurrent lumbar disc herniation. Clin Neurol Neurosurg. 2014;124:25–31. doi: 10.1016/j.clineuro.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 3.Shen X, Zhang H, Gu X, Gu G, Zhou X, He S. Unilateral versus bilateral pedicle screw instrumentation for single-level minimally invasive transforaminal lumbar interbody fusion. J Clin Neurosci. 2014;21:1612–1616. doi: 10.1016/j.jocn.2013.11.055. [DOI] [PubMed] [Google Scholar]
- 4.Tsahtsarlis A, Wood M. Minimally invasive transforaminal lumber interbody fusion and degenerative lumbar spine disease. Eur Spine J. 2012;21:2300–2305. doi: 10.1007/s00586-012-2376-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodríguez-Vela J, Lobo-Escolar A, Joven E, Muñoz-Marín J, Herrera A, Velilla J. Clinical outcomes of minimally invasive versus open approach for one-level transforaminal lumbar interbody fusion at the 3- to 4-year follow-up. Eur Spine J. 2013;22:2857–2863. doi: 10.1007/s00586-013-2853-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim JS, Jung B, Lee SH. Instrumented Minimally Invasive spinal-Transforaminal Lumbar Interbody Fusion (MIS-TLIF); Minimum 5-years Follow-up With Clinical and Radiologic Outcomes. J Spinal Disord Tech. 2012 doi: 10.1097/BSD.0b013e31827415cd. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Wu WJ, Liang Y, Zhang XK, Cao P, Zheng T. Complications and clinical outcomes of minimally invasive transforaminal lumbar interbody fusion for the treatment of one- or twolevel degenerative disc diseases of the lumbar spine in patients older than 65 years. Chin Med J (Engl) 2012;125:2505–2510. [PubMed] [Google Scholar]
- 8.Xiaolong S, Lei W, Hailong Z, Xin G, Guangfei G, Shisheng H. Radiographic Analysis of One-level Minimally Invasive Transforaminal Lumbar Interbody Fusion (MI-TLIF) With Unilateral Pedicle Screw Fixation for Lumbar Degenerative Diseases. J Spinal Disord Tech. 2013 doi: 10.1097/BSD.0000000000000042. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Hussein M, Abdeldayem A, Mattar MM. Surgical technique and effectiveness of microendoscopic discectomy for large uncontained lumbar disc herniations: a prospective, randomized, controlled study with 8 years of follow-up. Eur Spine J. 2014;23:1992–1999. doi: 10.1007/s00586-014-3296-9. [DOI] [PubMed] [Google Scholar]
- 10.Kulkarni AG, Bassi A, Dhruv A. Microendoscopic lumbar discectomy: Technique and results of 188 cases. Indian J Orthop. 2014;48:81–87. doi: 10.4103/0019-5413.125511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoshimoto M, Iwase T, Takebayashi T, Ida K, Yamashita T. Microendoscopic discectomy for far lateral lumbar disk herniation: less surgical invasiveness and minimum 2-year follow-up results. J Spinal Disord Tech. 2014;27:E1–E7. doi: 10.1097/BSD.0b013e3182886fa0. [DOI] [PubMed] [Google Scholar]
- 12.Isaacs RE, Podichetty VK, Santiago P, Sandhu FA, Spears J, Kelly K, Rice L, Fessler RG. Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine. 2005;3:98–105. doi: 10.3171/spi.2005.3.2.0098. [DOI] [PubMed] [Google Scholar]
- 13.Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 2004;86-A:1497–1503. doi: 10.2106/00004623-200407000-00020. [DOI] [PubMed] [Google Scholar]
- 14.Cook SD, Patron LP, Christakis PM, Bailey KJ, Banta C, Glazer PA. Comparison of methods for determining the presence and extent of anterior lumbar interbody fusion. Spine (Phila Pa 1976) 2004;29:1118–1123. doi: 10.1097/00007632-200405150-00013. [DOI] [PubMed] [Google Scholar]
- 15.Stevens KJ, Spenciner DB, Griffiths KL, Kim KD, Zwienenberg-Lee M, Alamin T, Bammer R. Comparison of minimally invasive and conventional open posterolateral lumbar fusion using magnetic resonance imaging and retraction pressure studies. J Spinal Disord Tech. 2006;19:77–86. doi: 10.1097/01.bsd.0000193820.42522.d9. [DOI] [PubMed] [Google Scholar]
- 16.Lee KH, Yue WM, Yeo W, Soeharno H, Tan SB. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. 2012;21:2265–2270. doi: 10.1007/s00586-012-2281-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seng C, Siddiqui MA, Wong KP, Zhang K, Yeo W, Tan SB, Yue WM. Five-year outcomes of minimally invasive versus open transforaminal lumbar interbody fusion: a matched-pair comparison study. Spine (Phila Pa 1976) 2013;38:2049–2055. doi: 10.1097/BRS.0b013e3182a8212d. [DOI] [PubMed] [Google Scholar]
- 18.Lee JC, Jang HD, Shin BJ. Learning curve and clinical outcomes of minimally invasive transforaminal lumbar interbody fusion: our experience in 86 consecutive cases. Spine (Phila Pa 1976) 2012;37:1548–1557. doi: 10.1097/BRS.0b013e318252d44b. [DOI] [PubMed] [Google Scholar]
- 19.Shunwu F, Xing Z, Fengdong Z, Xiangqian F. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine (Phila Pa 1976) 2010;35:1615–1620. doi: 10.1097/BRS.0b013e3181c70fe3. [DOI] [PubMed] [Google Scholar]
- 20.Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine. 2008;9:560–565. doi: 10.3171/SPI.2008.9.08142. [DOI] [PubMed] [Google Scholar]
- 21.Schoenfeld AJ, Ochoa LM, Bader JO, Belmont PJ Jr. Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program. J Bone Joint Surg Am. 2011;93:1577–1582. doi: 10.2106/JBJS.J.01048. [DOI] [PubMed] [Google Scholar]
- 22.Carragee EJ. The increasing morbidity of elective spinal stenosis surgery: is it necessary? JAMA. 2010;303:1309–1310. doi: 10.1001/jama.2010.402. [DOI] [PubMed] [Google Scholar]
- 23.Brodano GB, Martikos K, Lolli F, Gasbarrini A, Cioni A, Bandiera S, Di Silvestre M, Boriani S, Greggi T. Transforaminal Lumbar Interbody Fusion in Degenerative Disc Disease and Spondylolisthesis Grade I: Minimally Invasive Versus Open Surgery. J Spinal Disord Tech. 2013;28:E559–64. doi: 10.1097/BSD.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 24.Gu G, Zhang H, Fan G, He S, Cai X, Shen X, Guan X, Zhou X. Comparison of minimally invasive versus open transforaminal lumbar interbody fusion in two-level degenerative lumbar disease. Int Orthop. 2014;38:817–824. doi: 10.1007/s00264-013-2169-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foley KT, Lefkowitz MA. Advances in minimally invasive spine surgery. Clin Neurosurg. 2002;49:499–517. [PubMed] [Google Scholar]


