Abstract
Objective: To investigate the outcomes and prognostic factors for patients with coronary artery disease and low left ventricular ejection fraction (LVEF≤40%) undergoing off-pump coronary artery bypass grafting OPCAB). Methods: From 2001 to 2004, 71 patients with low EF undergoing OPCABG in our hospital, the mean age is 65.0±9.0 years (from 37 to 81), 49 males and 16 females, the mean EF was 33.8±5.0%. Regular follow-up evaluation was completed. Draw the Kaplan-Meier survival curves, Use the log-rank test and Cox regression model to find out the factors that affect the long-term result. Results: 71 low LVEF patients, 6 patients died perioperative, 63 patients discharged successfully, the follow-up time was 64.9±30.4 months. 6 patients lost of follow up, 19 patients died during follow-up including 10 patients (15.9%) who had cardiac-related death. The survival rate at 1, 3, 5 and 8 years was 95.1%, 93.3%, 86.3%, 77.7%, respectively. Univariate analysis shows EF≤30% and acute myocardial infarction within 30 days are risk factors for the long-term survival (P<0.05). Cox regression analysis showed that EF≤30% (RR=6.446, P<0.05) and acute myocardial infarction within 30 days (RR=5.993, P<0.05) are two independent risk factors for the cardiac-related death after discharge. Conclusions: The patients with low eject fraction ventricular have satisfactory outcomes after OPCAB. LVEF≤30% and acute myocardial infarction within 30 days are two independent risk factors that affect the long-term outcome.
Keywords: Low eject fraction, off-pump, artery bypass grafting, survival analysis
Introduction
Off-Pump Coronary Artery Bypass Grafting (OPCAB) allows surgeons to perform CABG on a beating heart. OPCAB have no reperfusion injury because the blood supply not interrupt and avoid the bad effect of cardiopulmonary bypass, so favor to preserve the heart function. The low left ventricular eject fraction (LVEF) patients have fragile heart function and may not be able to tolerate the ischemia and reperfusion in conventional CABG. So the low LVEF patients could be the best candidate for OPCAB [1,2]. Our previous research shows OPCAB in low LVEF patients have good feasibility and short-term outcome [3], but the long-term effect needs further observation.
In this study, the low LVEF patients undergoing OPCAB in 2001 to 2004 are accepted follow-up, the prognosis and long-term survival are investigated.
Patients and methods
Patients
From 2001 to 2004, 1073 patients had received CABG by a single surgeon in our center, 1007 patients had received OPCAB, 71 patients’ LVEF is less than or equal to 40%. These 71 patients were included in this research. Patients were selected on the basis of coronary angiography, with significant stenosis in the LAD, diagonal, Cx, and RCA branches. Patients who underwent an emergency operation or reoperation were excluded.
Surgical technique
General anesthesia was performed. The chest is open via a Medline sternotomy. The left internal thoracic arteries and great saphenous veins are harvested. After the harvesting is done, the patients are heparinized (1 mg/kg). In cases of patients of poor heart function in preoperative evaluation, we preparation for extracorporeal circulation with tubing system prepared (Wet-preparation). The heart was exposed by sternum retractor. Target coronary vessel was stabilized by special devices. Coronary shunt was used to keep the operative field clear and maintain continuous blood supply.
Follow-up
The follow-up was completed by out-patient, telephone and mail. Define heart-related death as the end point, including sudden cardiac death, myocardial infarction, heart failure and so on. Define lost to follow-up, died of non-cardiac event and alive as censored data.
Statistical analysis
Statistical calculations were performed using SPSS 16.0 (SPSS Inc, Chicago, IL). The measurement data expressed as the mean ± standard deviation, count data are expressed by percentile. Using the Kaplan-Meier method to draw survival curves of patients. Select the age, gender, diabetes, hypertension, LVEF, AMI<30 d, NYHA classification and left main disease as factors that may affect the survival rate. Use single factor log-rank test and Cox regression model to find the independent risk factors that affecting the survival rate. Define P<0.05 as statistically significant difference.
Results
Baseline data
65 patients were discharged. Of the 65 patients, 49 patients were male and 16 patients were female, the average age was (65.0±9.0) years. The Echocardiography preoperative shows that the mean LVEF was 33.8%±5.0%. The NYHA class of heart function was 2.3±0.9 level. The coronary angiography showed 15 patients had unprotected left main coronary artery disease (ULMCA), 52 patients were triple vessel disease, and 8 patients were double vessel disease. 12 (18.5%) patients accepted OPCAB within 30 days after acute myocardial infarction (AMI<30 days). The baseline date was showed as follows (Table 1).
Table 1.
Baseline data (n=65)
| Clinical data | Cases | Percentage (%) |
|---|---|---|
| Sex (male) | 49 | 75.4 |
| Age (year) | 65.0±9.0 | |
| Diabetes | 27 | 41.5% |
| Hypertension | 38 | 58.5% |
| Smoke | 27 | 41.5% |
| Left main lesions | 16 | 24.6% |
| Triple vessel disease | 55 | 84.6% |
| LVEF | 33.8±5.0% | |
| AMI<30 days | 12 | 18.5% |
| NYHA class | ||
| Grade II | 41 | 63.1% |
| Grade III | 15 | 23.1% |
| Grade IV | 9 | 13.8% |
| Number of bypass | 3.4±1.0 | |
Perioperative data
The mean operation time is 195±24 min. The ICU time is 23.4±14.0 h. The LOS (length of stay) is 21.9±10.5 d. The hospital mortality (defined as death within 30 days or at any time after operation if the patient did not leave the hospital alive) was 8.5% (6/71). 2 patients died of stroke, 2 patients died of sudden cardiac arrest, 1 patient died of Lower limb arterial thrombosis, 1 patient of recurrent ventricular fibrillation. 65 patients discharge, of these patients. 2 patients suffer from wound infection (one in leg and other in chest), 3 patients had Low Cardiac Output Syndrome, 1 patient had renal insufficiency, 4 patients had incidental atrial fibrillation. The patients had complication all recovered and the outcome was favorable.
Long-term outcomes
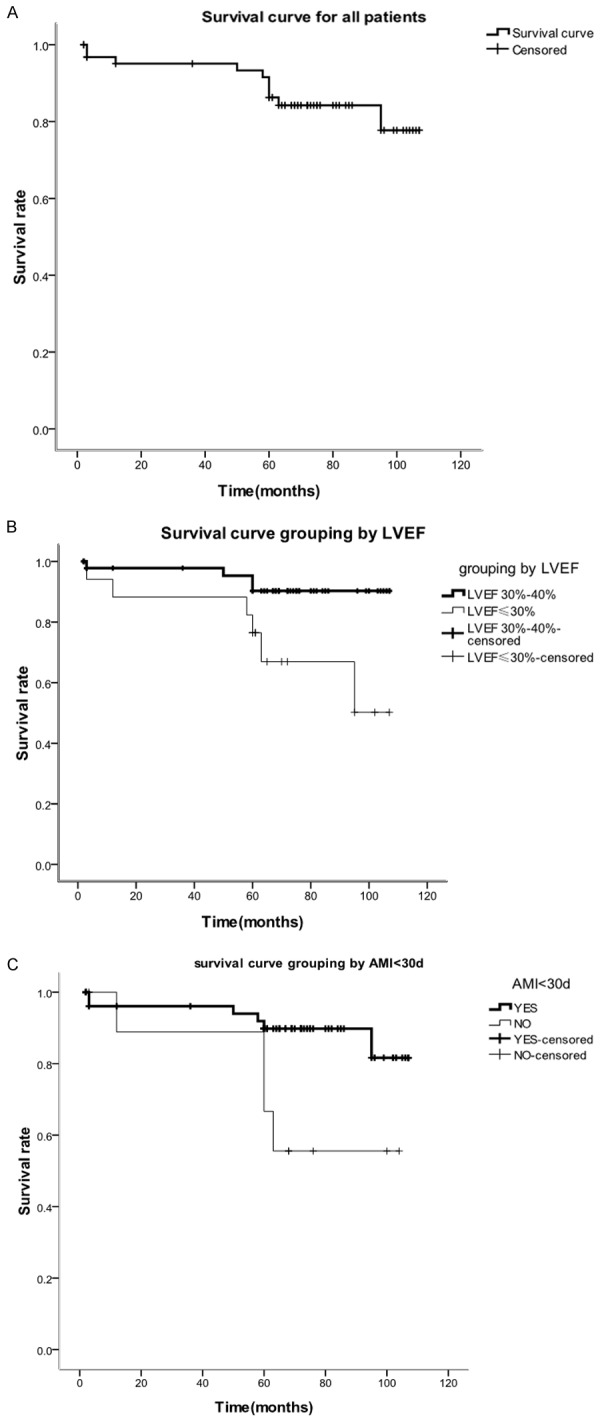
All 65 patients were undergoing regular follow-up, the mean anastomosis was 3.4±1.0. The last follow-up time was Dec 26, 2009. The mean follow-up time was 3-107 (64.9±30.4) month. 6 patients lost of follow-up, the loss rate was 8.5% (6/71). Until the last follow-up time, 40 (61.5%) patients was still alive, 19 (29.2%) patients died. In the death cases, 10 (15.4%) patients died of cardiac-related events. 9 patients died of non-cardiac events, including 2 patients died of stroke, 6 patients died of malignant tumor, 1 patient died of ileus. In the 40 patients that still alive at the end of follow-up, 1 patient suffer from oliguria and edema of lower extremity occasionally, the rest patients didn’t have symptoms of angina, and all patients had good cardiac function. The survival rate at 1, 3, 5 and 8 years was 95.1%, 93.3%, 86.3%, 77.7%, respectively. The Kaplan-Meier curve is showed in Figure 1A.
Figure 1.
Analysis of overall survival of breast cancer subtypes by Kaplan-Meier. ER-positive cases were determined to have longer survival rates when compared to non-luminal HER2+, ER-PR-HER2- and luminal B (ER-PR+) tumors.
Univariate analysis
We choose the following risk factors that may affect the mortality were taken into analysis, there are age, gender, diabetes, hypertension, LVEF, AMI<30 d, NYHA (III, IV), unprotected left main coronary artery disease (ULMCA). Log-rank tests show that LVEF≤30%, AMI<30d were factors that affect the long-term mortality (Table 2).
Table 2.
Univariate analysis
| Risk factors | Cases (percents) | 5 years survival | P values |
|---|---|---|---|
| Ages | |||
| >65 | 37 (56.9%) | 88.50% | 0.424 |
| ≤65 | 28 (43.1%) | 87.30% | |
| Gender | |||
| Male | 49 (75.4%) | 84.10% | 0.236 |
| Female | 16 (24.6%) | 92.30% | |
| Diabetes | |||
| YES | 27 (41.5%) | 91.60% | 0.420 |
| NO | 38 (58.5%) | 82.40% | |
| Hypertension | |||
| YES | 38 (58.5%) | 87.10% | 0.233 |
| NO | 27 (41.5%) | 84.30% | |
| NYHA class | |||
| ≥3 | 24 (36.9%) | 82.50% | 0.110 |
| <3 | 41 (63.1%) | 88.90% | |
| LVEF | |||
| ≤30% | 17 (27.0%) | 76.50% | 0.017 |
| 30%<EF≤40% | 46 (73.0%) | 90.30% | |
| LMCA | |||
| YES | 16 (24.6%) | 91.90% | 0.325 |
| NO | 49 (75.4%) | 83.90% | |
| AMI<30 d | |||
| YES | 11 (16.9%) | 66.70% | 0.033 |
| NO | 54 (83.1%) | 91.90% |
Cox regression analysis
To further confirmed the risk factors that relevant with heart-related death. These factors were taken into Multivariate Cox regression analysis. The results show that LVEF≤30%, AMI<30 d are Independent risk factors that affect long-term mortality (Table 3). The survival curves are show in Figure 1B and 1C.
Table 3.
Cox regression analysis
| Risk factors | B | SE | RR values | 95% CI | P value | |
|---|---|---|---|---|---|---|
|
| ||||||
| lower | upper | |||||
| AMI<30 d | 1.690 | 0.666 | 6.446 | 1.470 | 19.971 | 0.011 |
| LVEF≤30% | 1.638 | 0.669 | 5.993 | 1.386 | 19.093 | 0.014 |
Discussion
Although off-pump or on-pump is a hot-debated problem, and there is still no definitive conclusion. OPCAB can avoid the Ischemia-reperfusion injury and cardiopulmonary bypass damage, so it is used more and more at present. For the patient have poor ventricular function or too weak to tolerate the cardiopulmonary bypass, OPCAB can have obvious benefit compare with ONCAB.
The previous research shows, is about 40%, patients of left ventricular dysfunction have poor outcome, the 5-year survival rate of medical-treatment is about 40%. And conventionally on-pump CABG exceed 60% [4]. In our research, the five years survival rate of patients with left ventricular eject fraction less than 40% undergoing coronary artery bypass grafting is 86.3%, which is superior to medical treatment and ONCAB in previous study. Even so, OPCAB is far from perfect for patients with ventricular dysfunction, as low left ventricular eject fraction will bring lots of problem in surgery. Attaran S and colleagues [5] reported that there are no statistically differences in aspects of in-hospital mortality, mid-term and long-term survival rate between OPCAB and ONCAB in patients with left ventricular dysfunction. He suggests that if myocardial protection had been taken finely during operation, ONCAB had no shortage comparing with OPCAB. On the other hand, several previous researches [6-8] had compared the clinical outcomes between OPCAB and ONCAB in patients with left ventricular dysfunction, they shows that OPACB has significant advantage in operation time, Organ dysfunction post operation, Length of Stay and re-admission. This contrary conclusion may derive from different cases selection, surgical technique and Statistical methods; even so, for patients with left ventricular dysfunction, the problem of on-pump or off-pump still has no certain answers. Our research shows that OPCAB in patients with low LVEF have satisfactory short-term and long-term outcomes.
Surgical contraindications of OPCAB in patients with low LVEF are still undefined. Some researchers have reported that LVEF<10% is a contraindications for CABG, also other researchers consider that as long as there are suitable target vessels, it worth to operation [9]. But when applied in OPCAB, all the conclusions need to be carefully reconsidered. In all research, the lowest LVEF is 19%, this patient recovered smoothly after surgery. His symptoms had relieved and he was still alive at the last follow-up. Meanwhile, we find that LVEF<30% is still an independent risk factor for heart-related death in follow-up. This is consistent with Euroscore [10]. So, we insist that for patients undergoing Elective OPCAB with low LVEF, preoperative preparation is important, we should try to improve the left ventricular ejection fraction by medication, all these can lead to better outcomes after OPCAB. Besides, our research show that AMI<30 days (RR=5.544, P<0.05) is another independent risk factor affecting the long-term prognosis. It means that when surgery are taken in 30 days after acute myocardial infarction, the long-term risk of cardiac-related deaths increased by 5.544 times. The patients with low LVEF and in acute phase of AMI have poor cardiac function, they often occur hypotension and cardiac arrhythmias when move the heart in surgery. It not only brings about difficulty to expose the coronary artery, but also result in poor perfusion of the heart and other important organs. All these lead to worse long-term outcomes for patients undergoing OPCAB within 30 days after AMI.
We believe that it is entirely feasible for low LVEF underwent OPCAB. However, In order to obtain good surgical results, we must first fully assess coronary artery conditions, choose appropriate surgical technique for each patient, and achieve complete revascularization. Maintaining hemodynamic intraoperative is of significant important. When hemodynamic is hard to maintain by vasoactive drugs, we need to convert to on-pump rather than continue off-pump reluctantly. OPCAB in patients with low LVEF need surgeon’s experience and teamwork. All of our patients were operated by a single surgeon; he had more than 1,000 surgical experiences in OPCAB. As shows above, the mean number of bypass is 3.4±1.0 and all cases had complete revascularization. So the long-term outcome is favorable.
This is a single-center study, the sample size is small and lack of comparison. These need to be improved in further research.
In summary, the patients with low left ventricular eject fraction have satisfactory outcomes after OPCAB. LVEF≤30% and acute myocardial infarction within 30 days are two independent risk factors that affect the long-term outcome. The OPCAB should be fully prepared to improve the LVEF and try to avoid operate within 30 days after acute myocardial infarction.
Disclosure of conflict of interest
None.
References
- 1.Puskas JD, Edwards FH, Pappas PA, O’Brien S, Peterson ED, Kilgo P, Ferguson TB Jr. Off-pump techniques benefit men and women and narrow the disparity in mortality after coronary bypass grafting. Ann Thorac Surg. 2007;84:1447–1454. doi: 10.1016/j.athoracsur.2007.06.104. [DOI] [PubMed] [Google Scholar]
- 2.Tabata M, Takanashi S, Fukui T, Horai T, Uchimuro T, Kitabayashi K, Hosoda Y. Offpump coronary artery bypass grafting in patients with low eject fraction. Ann Thorac Surg. 2002;17:383–385. doi: 10.1016/j.athoracsur.2004.06.040. [DOI] [PubMed] [Google Scholar]
- 3.Cooper EA, Edelman JJ, Wilson MK, Bannon PG, Vallely MP. Off-pump coronary artery bypass grafting in elderly and high-risk patients--a review. Heart Lung Circ. 2011;20:694–703. doi: 10.1016/j.hlc.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 4.O’connor CM, Velazquez EJ, Gardner LH, Smith PK, Newman MF, Landolfo KP, Lee KL, Califf RM, Jones RH. Comparison of coronary artery bypass grafting versus medical therapy on long-term outcome in patients with ischemic cardiomyopathy (a 25-year experience from the Duke Cardiovascular Disease Databank) Am J Cardiol. 2002;90:101–107. doi: 10.1016/s0002-9149(02)02429-3. [DOI] [PubMed] [Google Scholar]
- 5.Attaran S, Shaw M, Bond L, Pullan MD, Fabri BM. Does off-pump coronary artery revascularization improve the long-term survival in patients with ventricular dysfunction? Interact Cardiovasc Thorac Surg. 2010;11:442–446. doi: 10.1510/icvts.2010.237040. [DOI] [PubMed] [Google Scholar]
- 6.Caputti GM, Palma JH, Gaia DF, Buffolo E. Offpump coronary artery bypass surgery in selected patients is superior to the conventional approach for patients with severely depressed left ventricular function. Clinics (Sao Paulo) 2011;66:2049–2053. doi: 10.1590/S1807-59322011001200009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldstein DJ, Beauford RB, Luk B, Karanam R, Prendergast T, Sardari F, Burns P, Saunders C. Multivessel off-pump revascularization in patients with severe left ventricular dysfunction. Eur J Cardiothorac Surg. 2003;24:72–80. doi: 10.1016/s1010-7940(03)00174-x. [DOI] [PubMed] [Google Scholar]
- 8.Cleveland JC Jr, Shroyer AL, Chen AY, Peterson E, Grover FL. Off-pump coronary artery bypass grafting decreases risk-adjusted mortality and morbidity. Ann Thorac Surg. 2001;72:1282–1289. doi: 10.1016/s0003-4975(01)03006-5. [DOI] [PubMed] [Google Scholar]
- 9.Elefteriades JA, Morales DL, Gradel C, Tollis G Jr, Levi E, Zaret BL. Results of coronary artery bypass grafting by a single surgeon in patients with left ventricular ejection fractions < or = 30% Am J Cardiol. 1997;79:1573–1578. doi: 10.1016/s0002-9149(97)00201-4. [DOI] [PubMed] [Google Scholar]
- 10.Nashef S, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE) Eur J Cardiothorac Surg. 1999;16:9–13. doi: 10.1016/s1010-7940(99)00134-7. [DOI] [PubMed] [Google Scholar]


