Abstract
To investigate the method and outcome from direct clipping of a blister-like aneurysm (BBA) of the internal carotid artery supraclinoid segment. This study featured nine BBA patients, including eight females and one male. The patients presented subarachnoid hemorrhage (SAH) as the initial symptom and were diagnosed with BBA in the supraclinoid segment through a vascular exam and imaging. During the exam, the internal carotid artery was pressed to block the blood flow, and a transcranial Doppler (TCD) was performed to examine the blood flow in the (BBA) ipsilateral middle cerebral artery. The results showed that the blood flow was reduced by less than 40% in all nine patients. During surgery, a pterional craniotomy was used to fully expose the aneurysm for clipping. While clipping the aneurysm, the arterial wall at the root of the aneurysm was also clipped to improve stability. Intraoperative ultrasonography was performed before and after clipping to examine the blood flow in the parent artery, middle cerebral artery and anterior cerebral artery. Moreover, a TCD was performed within one week after surgery to monitor intracranial blood flow. During BBA clipping, four patients exhibited stenosis of the parent artery, but intraoperative ultrasonography showed adequate blood flow in the anterior cerebral artery and middle cerebral artery. TCD was performed within one week after surgery to examine the blood flow in the middle cerebral artery on the operative side; the TCD showed adequate blood flow. The patients recovered well after surgery and were discharged. Digital subtraction angiography (DSA) or computed tomography angiography (CTA) was performed six to 12 months after the surgery and showed no aneurysm relapse. Moreover, six patients exhibited no stenosis of the parent artery, 20% stenosis was observed in one patient, 30% stenosis was observed in one patient, and 50% stenosis was observed in one patient; none of the patients showed clinical symptoms, and all patients exhibited good collateral circulation. Therefore, if a pre-operative TCD shows adequate compensatory contralateral blood flow in the (BBA) ipsilateral middle cerebral artery after the internal carotid artery is pressed to block the blood flow, then direct clipping of the BBA is a simple and feasible treatment strategy. However, when the aneurysm is clipped, the artery wall at the root of the aneurysm must also be clipped to improve stability. With adequate compensation, partial stenosis of the parent artery is acceptable.
Keywords: Supraclinoid segment of the internal carotid artery, blister-like aneurysm, direct clipping, transcranial doppler
Introduction
An intracranial blister-like aneurysm (BBA) is most common in the supraclinoid segment of the internal carotid artery and typically lacks a normal aneurysm wall structure. Thus, the BBA body is merely the thin arterial adventitia, and a hematoma typically forms around the ruptured BBA [1,2]. A BBA is difficult to treat due to its pathological anatomy. Currently, BBA treatments primarily include direct clipping, aneurysm wrapping, aneurysm trapping plus revascularization and an interventional treatment with a flow-diverting device [3,4]. Except for direct clipping, such methods are complex and difficult to perform. Direct clipping is advantageous because it is a simple operation; however, it tends to induce stenosis or occlusion of the parent artery, thereby producing ischemic complications. However, with an adequate pre-operative assessment of the collateral circulation, direct clipping is practical and effective for cases with adequate blood flow compensation [5]. This study provides a retrospective analysis of clinical data from nine cases of a ruptured BBA in the supraclinoid segment treated with direct clipping. A pre-operative transcranial Doppler (TCD) was conducted to assess the collateral circulation before directly clipping the BBA with satisfactory treatment outcomes. The relevant clinical treatment experience is summarized below.
Materials and methods
General data
This study features nine patients, including eight females and one male, ages 31-57 (mean: 46.8 years). The patients presented subarachnoid hemorrhage (SAH) as the initial symptom. A pre-operative Hunt-Hess classification showed that six cases were grade II and three cases were grade III. Digital subtraction angiography (DSA) or computed tomography angiography (CTA) showed a BBA in the supraclinoid segment with four cases in the dorsal side of the internal carotid artery supraclinoid segment, two cases were in the internal side of the internal carotid artery supraclinoid segment, two cases were in the internal and inferior side of the carotid artery supraclinoid segment, and one case was in the internal and posterior side of the internal carotid artery supraclinoid segment. Before surgery, the internal carotid artery was pressed to block blood flow, and a TCD was performed to examine the blood flow in the (BBA) ipsilateral middle cerebral artery. The results show that the blood flow decreased by 20% in three cases, 30% in five cases and 40% in one case.
Treatment
Surgical method
Ipsilateral pterional access was used for craniotomy. After part of the sphenoid wing was drilled and removed, the dura mater was cut to expose and separate the brain tissue along the lateral fissure. Next, the carotid cistern and optic cistern were exposed, and the arachnoid was opened to fully expose the internal carotid artery supraclinoid segment, the anterior cerebral artery A1 segment and the middle cerebral artery M1 segment. The BBA in the internal carotid artery supraclinoid segment was fully exposed followed by temporarily clipping the internal carotid artery on both sides of the BBA. The appropriate size aneurysm clip for the BBA was selected based on the site and shape of the aneurysm, and the arterial wall at the root of the aneurysm was also clipped to improve stability after clipping and prevent the aneurysm clip from slipping. Intraoperative ultrasonography was performed before and after clipping to examine the blood flow in the internal carotid artery, middle cerebral artery and anterior cerebral artery. The skull was closed using the standard procedure after BBA clipping.
Post-operative treatment
The patients received the standard symptomatic treatment after surgery. To prevent hypoperfusion, during surgery, patients with stenosis of the parent artery after clipping received a treatment to manage blood pressure after the surgery. TCD was performed one week after surgery to monitor intracranial blood flow and evaluate the blood flow in the ipsilateral middle cerebral artery. For severe SAH, continuous lumbar drainage was performed to release bloody cerebrospinal fluid.
Follow-up
The patients visited our hospital for a follow-up CTA or DSA six to 12 months after surgery to check for relapse of aneurysm, patency of the parent artery and compensatory collateral circulation. Moreover, the patients were followed up by telephone twice to check their status of daily activities and limb movement.
Results
Surgery outcome
During surgery, a cross-vascular clip was used to clip the BBA at the internal and inferior side of the internal carotid artery supraclinoid segment (two cases). For the seven cases of BBA in the dorsal or internal sides of the internal carotid artery supraclinoid segment, a single straight or curved aneurysm clip was used to clip the aneurysm in five cases, and a combination of two aneurysm clips was used to clip the aneurysm in two cases. During clipping, three patients had BBA rupture and hemorrhage, and the clipping was secured and confirmed thereafter. After BBA clipping, four patients had stenosis of the parent artery. In each patient, intraoperative vascular ultrasonography performed after the BBA clipping showed adequate blood flow in the anterior cerebral artery and middle cerebral artery.
Post-operative treatment and follow-up
In each patient, a TCD performed within one week after surgery showed adequate blood flow in the ipsilateral middle cerebral artery. The patients recovered well after surgery and were discharged with no limb movement disorders. A follow-up DSA or CTA six to 12 months after surgery showed no stenosis of the parent artery in six patients, 20% stenosis in one patient, 30% stenosis in one patient and 50% stenosis in one patient. The three patients with stenosis did not exhibit clinical symptoms. The detailed clinical data are shown in Table 1.
Table 1.
Summary of the clinical data
| No. | Age | Gender | Preoperative HH | Site | Arterial blood flow after the internal carotid artery was pressed* | Clipping method | Intraoperative rupture and hemorrhage | Intraoperative stenosis of the parent artery | Intraoperative arterial ultrasonography** | Postoperative DSA or CTA of the parent artery | Prognosis |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 46 | Female | II | Dorsal side of the supraclinoid segment | Reduced by 30% | A Single curved clip | No | No | Adequate blood flow | No vascular stenosis | Good |
| 2 | 51 | Female | II | Internal and inferior side of the supraclinoid segment | Reduced by 20% | A single cross-vascular clip | No | No | Adequate blood flow | No vascular stenosis | Good |
| 3 | 31 | Male | II | Internal and inferior side of the supraclinoid segment | Reduced by 30% | A single cross-vascular clip | No | Yes | Adequate blood flow | 30% stenosis | Good |
| 4 | 45 | Female | II | Internal side of the supraclinoid segment | Reduced by 30% | A single straight clip | No | Yes | Adequate blood flow | 20% stenosis | Good |
| 5 | 48 | Female | III | Dorsal side of the supraclinoid segment | Reduced by 40% | A single curved clip | Yes | No | Adequate blood flow | No vascular stenosis | Good |
| 6 | 52 | Female | II | Dorsal side of the supraclinoid segment | Reduced by 20% | A single straight clip | No | No | Adequate blood flow | No vascular stenosis | Good |
| 7 | 50 | Female | III | Dorsal side of the supraclinoid segment | Reduced by 30% | Two curved clips | Yes | Yes | Adequate blood flow | No vascular stenosis | Good |
| 8 | 57 | Female | II | Internal side of the supraclinoid segment | Reduced by 20% | Two curved clips | Yes | No | Adequate blood flow | No vascular stenosis | Good |
| 9 | 41 | Female | III | Dorsal and internal side of the supraclinoid segment | Reduced by 30% | A single curved clip | No | Yes | Adequate blood flow | 50% stenosis | Good |
HH: Hunt-Hess classification;
The BBA side of the internal carotid artery was pressed to examine the decrease in blood flow at the BBA side of the middle cerebral artery;
Intraoperative arterial ultrasonography: the blood flow in the parent artery, middle cerebral artery and anterior cerebral artery was examined.
Discussion
BBA accounts for approximately 0.3-1% of all intracranial aneurysms and 0.9-6.6% of internal carotid artery aneurysms; the internal carotid artery supraclinoid segment is the most common BBA site [6,7]. Therefore, BBAs are not uncommon in clinical practice; however, nearly all BBA cases are difficult and tricky to treat, mainly due to the specific pathological anatomy of BBAs. Based on histological features, a BBA is not a true cerebral aneurysm but rather a pseudoaneurysm formed following the tearing of an arterial wall dissection. A BBA does not have an internal elastic layer or tunica media and is merely composed of blood clots, fibrous tissue and arterial adventitia [4,6]. Due to its pathological anatomy characteristics, a BBA is fragile. An unruptured BBA appears as a bloody blister or blister in the hand or foot [8]. Considering the typical Case 1, 8, 9 herein as examples (Figures 1, 2 and 3), during surgery, the BBA exhibited a thin wall and was prone to rupture and hemorrhage with clearly visible blood flow inside the BBA. Among the nine BBA patients in this study, three patients had rupture and hemorrhage during clipping, and the clipping was secured and confirmed thereafter, which indicates that the BBA is fragile. Morphologically, a BBA is similar to a bloody blister and thus lacks the cystic aneurysm imaging features; instead, it appears as a flat lesion sprawling on the arterial wall, and certain BBAs may not be detected using CTA and may be missed in the DSA two-dimensional lateral perspective. Therefore, an oblique view or three-dimensional reconstruction is required for examination. Hence, if SAH is concentrated in the carotid cistern, and a CTA scan shows a small protrusion on the internal carotid artery supraclinoid segment, especially without an arterial branch around the protrusion, clinicians must consider the possibility of a BBA in the internal carotid artery supraclinoid segment [9]. In this study, the patients exhibited these imaging features and exhibited a BBA through DSA following negative CTA findings. Furthermore, the BBA detection rate is improving with the development of imaging techniques. For instance, in 2011, Horie et al. detected a BBA inside a hematoma using high-resolution magnetic resonance imaging [10]. Therefore, more BBA cases may be detected and treated in the future.
Figure 1.
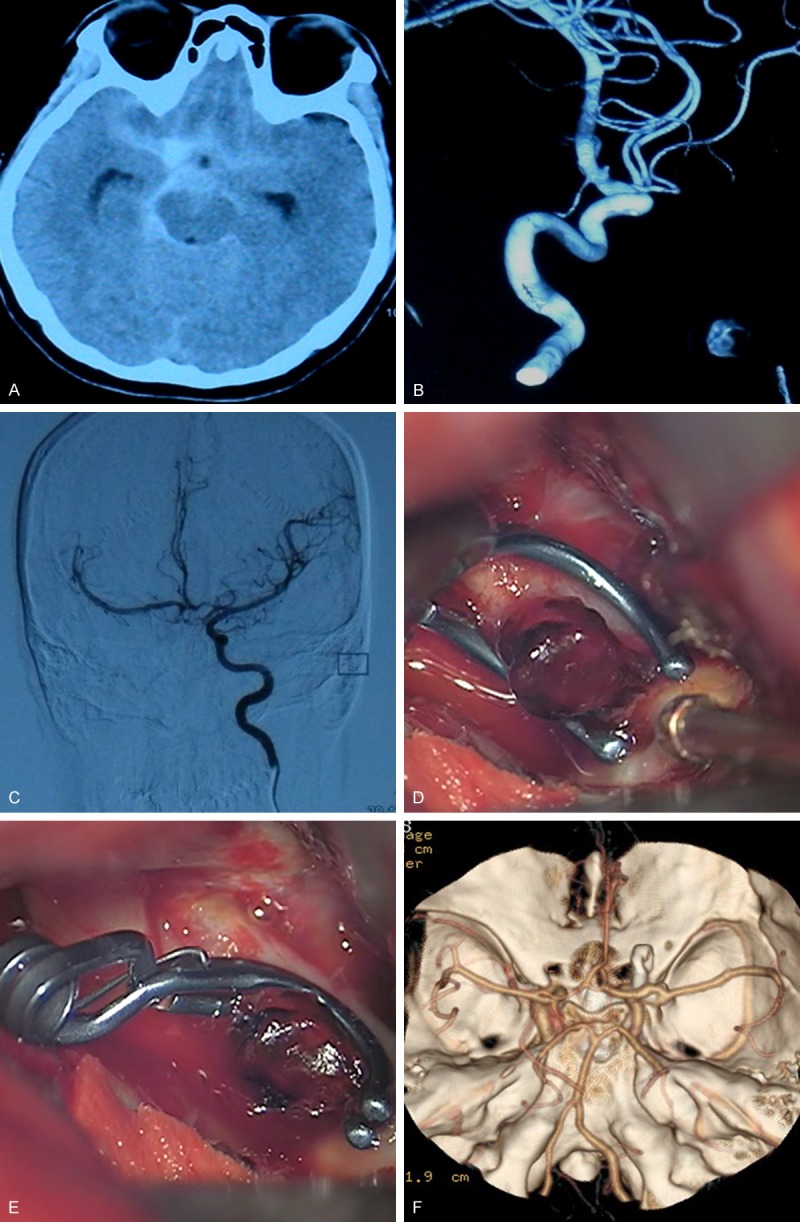
Imaging for Case 1: A. Head CT shows SAH concentrated in the right carotid cistern. B. Head DSA shows a BBA in the right internal carotid artery supraclinoid segment. C. DSA shows that, after the right internal carotid artery was pressed, the blood flow in the right internal carotid artery was compensated by the blood flow from the anterior communicating artery. D, E. Surgical clipping of the BBA with blood clots observed around the BBA. F. Follow-up CTA after clipping shows no relapse of the aneurysm.
Figure 2.
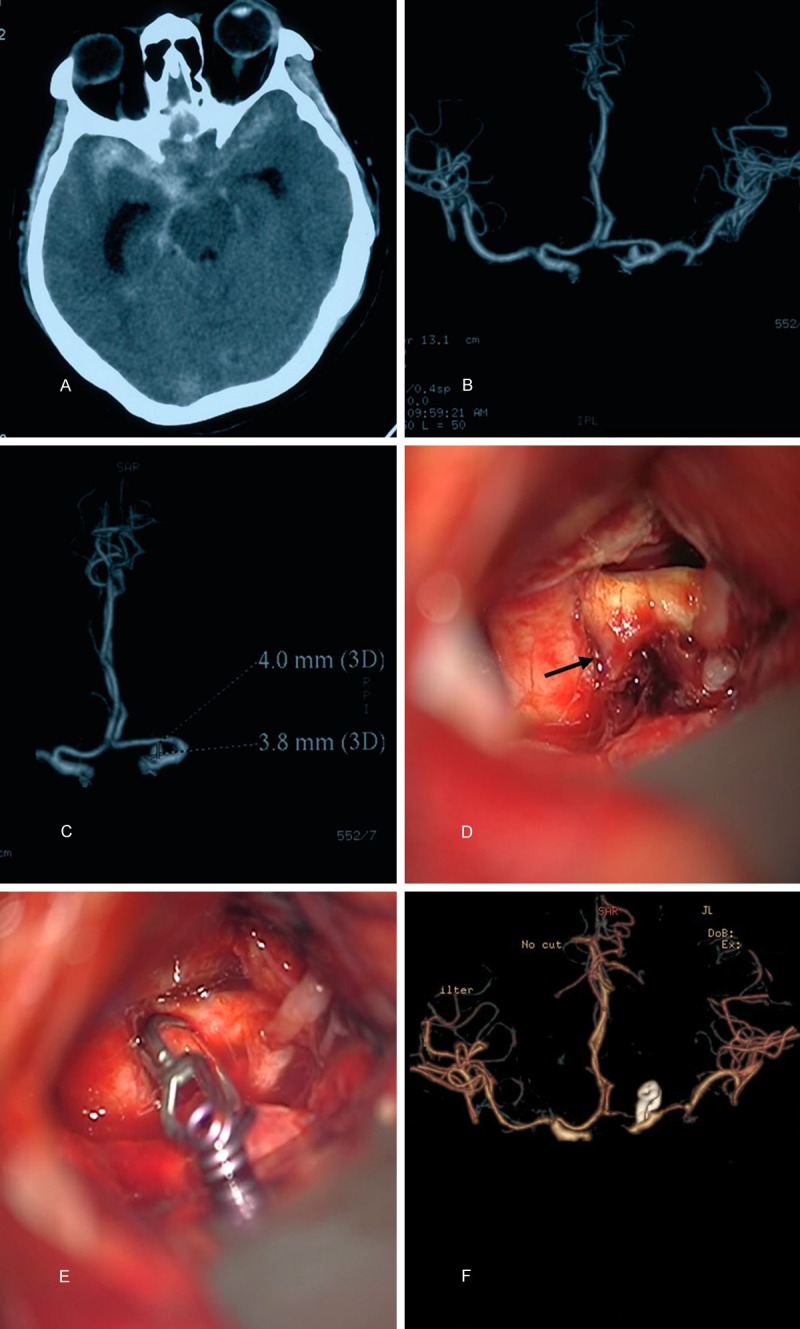
Imaging for Case 8: A. Head CT shows SAH concentrated in the right carotid cistern. B, C. Head CTA shows a BBA in the internal side of the right internal carotid artery supraclinoid segment. D, E. During surgery, the BBA exhibited a thin wall, and two aneurysm clips were used to clip the aneurysm. F. Follow-up CTA after clipping showed no relapse of the aneurysm or stenosis of the parent artery.
Figure 3.
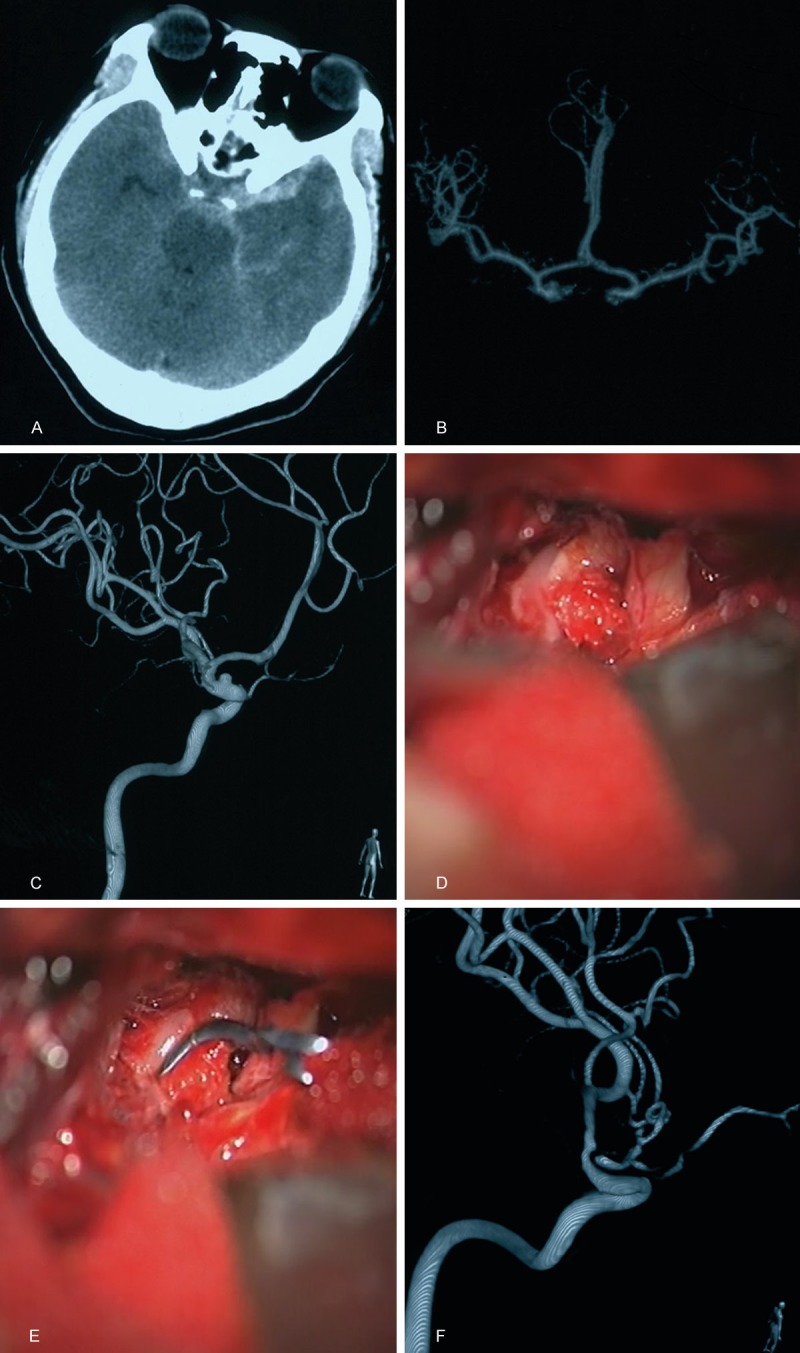
Imaging for Case 9: A. Head CT shows SAH concentrated in the left carotid cistern. B, C. Head CTA and DSA show BBA in the left internal carotid artery supraclinoid segment. D, E. Surgical clipping of the BBA with blood clots around the fragile BBA. F. Follow-up CTA after clipping shows no relapse of the aneurysm and 50% stenosis of the parent artery.
Once diagnosed, most intracranial BBA cases require surgical treatment. In particular, once a BBA ruptures, the risk of re-rupture is high; thus, the current consensus is that a BBA must be treated [11]. At present, a BBA is mainly treated using surgical and interventional treatments; the surgical methods include clipping, wrapping, arterial suture and trapping. In certain cases, trapping must be combined with a vascular bypass. Interventional methods include direct embolization, stent assisted embolization, coil or balloon occlusion of the aneurysm and parent artery, conventional multilayer stents and blood flow-diverting device [12-14]. Recently, more BBA cases in the supraclinoid segment have been treated with bypass-assisted BBA clipping or trapping and an interventional treatment using a conventional multilayer stent or a blood flow-diverting device. In 2014, Kazumata et al. reported good outcomes for 20 cases of a ruptured BBA in the internal carotid artery treated with a radial artery graft bypass and sacrificing the parent artery [15]. In addition to craniotomy and clipping, a conventional stent superposition is also an effective treatment. For instance, in 2014, Walsh et al. conducted a retrospective analysis of clinical data from eight BBA cases treated with a conventional stent superimposition and with good outcomes [16]. A novel blood flow-diverting device provides an additional option for interventional treatment of BBA in the internal carotid artery supraclinoid segment. In 2015, Aydin et al. reported satisfactory outcomes for 11 BBA cases treated with a silk blood flow-diverting device [4]. Moreover, many studies have reported other types of blood flow-diverting devices [2,17]. Although these complex techniques might effectively treat BBA, certain BBA cases can still be effectively treated with simple aneurysm embolization and clipping if the cases are screened and indicated for such treatments.
In 2014, Kim et al. reported clinical data for 11 BBA cases. After assessing the collateral circulation, seven patients underwent direct occlusion of the aneurysm and parent artery with satisfactory outcomes [18]. Because direct coil embolization and occlusion of BBA and the parent artery can be adopted in cases with satisfactory compensatory collateral circulation, a craniotomy with direct clipping should also be a safe and feasible treatment for BBA with more advantages and greater value mainly due to the potential for complete or partial preservation of the parent artery during BBA clipping. Thus, some blood flow can be provided even with arterial stenosis during clipping. As shown herein, the nine patients underwent a pre-operative assessment and exhibited adequate compensatory collateral circulation; thus, the patients were treated with craniotomy and direct clipping of the BBA. The BBA lacks an aneurysm’s anatomical structure and is merely composed of a layer of fibrous tissue and arterial adventitia, which leads to poor stability after clipping and a likelihood that the BBA will break during clipping and cause arterial leak and hemorrhage. Thus, herein, during direct clipping of the BBA, the arterial wall at the root of the BBA was also clipped to improve stability after clipping and prevent the aneurysm clip from slipping, but this may also cause stenosis of the parent artery. In this study, three patients exhibited stenosis of the internal carotid artery supraclinoid segment after clipping, but they and the remaining patients (nine patients total) exhibited satisfactory outcomes due to adequate compensatory collateral circulation. During BBA clipping, it is important to select an appropriate size aneurysm clip based on the site and shape of the aneurysm. In this study, a cross-vascular clip was used in two BBA cases in the internal side of the internal carotid artery supraclinoid segment, and more than one aneurysm clip was used in two patients.
For BBA in the internal carotid artery supraclinoid segment, compensatory collateral circulation must be thoroughly assessed before selecting a complex treatment regimen. For patients with adequate compensatory collateral circulation, a craniotomy with direct clipping is feasible. Currently, a balloon occlusion test (BOT) is the best method for evaluating collateral circulation. If no clinical symptoms are observed during a BOT of the internal carotid artery, then the patient has adequate compensatory collateral circulation and is indicated for internal carotid artery occlusion. BBA clipping is safe, and concerns over potential stenosis of the parent artery are unnecessary [19]. However, a BOT involves complex procedures, and repeat BOTs can be difficult to perform; in contrast, a TCD is simple and convenient to perform [20,21]. When using a TCD to assess collateral circulation, Hetzel et al. believed that a less than 60% decrease in blood flow in the middle cerebral artery is safe [20]. Herein, the nine patients underwent TCD to assess the blood flow in the middle cerebral artery before surgery. The results showed that after the internal carotid artery was pressed, the decrease in blood flow in the middle cerebral artery was less than 40%, and no clinical symptoms were observed. Thus, the patients were considered suitable for direct clipping of the BBA. During direct clipping of the BBA, the blood flow in the supraclinoid segment of the internal carotid artery, anterior cerebral artery and middle cerebral artery was monitored and adequate. The patients exhibited satisfactory outcomes after surgery. Therefore, if a pre-operative TCD shows adequate compensatory contralateral blood flow in the (BBA) ipsilateral middle cerebral artery after the internal carotid artery is pressed to block the blood flow, then direct clipping of the BBA is simple and feasible. However, during clipping of the aneurysm, the artery wall at the root of the aneurysm must also be clipped to improve stability. With adequate compensation, partial stenosis of an parent artery is acceptable.
Disclosure of conflict of interest
None.
References
- 1.Gonzalez AM, Narata AP, Yilmaz H, Bijlenga P, Radovanovic I, Schaller K, Lovblad KO, Pereira VM. Blood blister-like aneurysms: single center experience and systematic literature review. Eur J Radiol. 2014;83:197–205. doi: 10.1016/j.ejrad.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 2.Nerva JD, Morton RP, Levitt MR, Osbun JW, Ferreira MJ, Ghodke BV, Kim LJ. Pipeline Embolization Device as primary treatment for blister aneurysms and iatrogenic pseudoaneurysms of the internal carotid artery. J Neurointerv Surg. 2015;7:210–216. doi: 10.1136/neurintsurg-2013-011047. [DOI] [PubMed] [Google Scholar]
- 3.Regelsberger J, Matschke J, Grzyska U, Ries T, Fiehler J, Koppen J, Westphal M. Blisterlike aneurysms-a diagnostic and therapeutic challenge. Neurosurg Rev. 2011;34:409–416. doi: 10.1007/s10143-011-0313-x. [DOI] [PubMed] [Google Scholar]
- 4.Aydin K, Arat A, Sencer S, Hakyemez B, Barburoglu M, Sencer A, Izgi N. Treatment of ruptured blood blister-like aneurysms with flow diverter SILK stents. J Neurointerv Surg. 2015;7:202–209. doi: 10.1136/neurintsurg-2013-011090. [DOI] [PubMed] [Google Scholar]
- 5.Kalani MY, Zabramski JM, Kim LJ, Chowdhry SA, Mendes GA, Nakaji P, McDougall CG, Albuquerque FC, Spetzler RF. Long-term followup of blister aneurysms of the internal carotid artery. Neurosurgery. 2013;73:1026–1033. doi: 10.1227/NEU.0000000000000147. discussion 1033. [DOI] [PubMed] [Google Scholar]
- 6.Ishikawa T, Nakamura N, Houkin K, Nomura M. Pathological consideration of a “blisterlike” aneurysm at the superior wall of the internal carotid artery: case report. Neurosurgery. 1997;40:403–405. doi: 10.1097/0006123-199702000-00038. discussion 405-406. [DOI] [PubMed] [Google Scholar]
- 7.Kim JH, Kwon TH, Kim JH, Park YK, Chung HS. Internal carotid artery dorsal wall aneurysm with configurational change: Are they all false aneurysms? Surg Neurol. 2006;66:441–443. doi: 10.1016/j.surneu.2005.12.030. discussion 443. [DOI] [PubMed] [Google Scholar]
- 8.Mooney MA, Kalani MY, Nakaji P, Albuquerque FC, McDougall CG, Spetzler RF, Zabramski JM. Long-term Patient Outcomes After Microsurgical Treatment of Blister-Like Aneurysms of the Basilar Artery. Neurosurgery. 2015;11(Suppl 3):387–393. doi: 10.1227/NEU.0000000000000866. [DOI] [PubMed] [Google Scholar]
- 9.Tsuzuki N, Katoh H, Toyooka T, Uozumi Y, Shima K. Subarachnoid clot distribution in anterior wall saccular aneurysms of the internal carotid artery. J Clin Neurosci. 2007;14:242–244. doi: 10.1016/j.jocn.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Horie N, Morikawa M, Fukuda S, Hayashi K, Suyama K, Nagata I. Detection of blood blister-like aneurysm and intramural hematoma with high-resolution magnetic resonance imaging. J Neurosurg. 2011;115:1206–1209. doi: 10.3171/2011.8.JNS11909. [DOI] [PubMed] [Google Scholar]
- 11.Szmuda T, Sloniewski P, Waszak PM, Springer J, Szmuda M. Towards a new treatment paradigm for ruptured blood blister-like aneurysms of the internal carotid artery? A rapid systematic review. J Neurointerv Surg. 2015 doi: 10.1136/neurintsurg-2015-011665. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Kubo Y, Koji T, Yoshida K, Saito H, Ogawa A, Ogasawara K. High-flow bypass and wrap-clipping for ruptured blood blister-like aneurysm of the internal carotid artery using intraoperative monitoring of cerebral hemodynamics. Vasc Health Risk Manag. 2015;11:297–302. doi: 10.2147/VHRM.S73779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cikla U, Baggott C, Baskaya MK. How I do it: treatment of blood blister-like aneurysms of the supraclinoid internal carotid artery by extracranial-to-intracranial bypass and trapping. Acta Neurochir (Wien) 2014;156:2071–2077. doi: 10.1007/s00701-014-2212-8. [DOI] [PubMed] [Google Scholar]
- 14.Baskaya MK, Ahmed AS, Ates O, Niemann D. Surgical treatment of blood blister-like aneurysms of the supraclinoid internal carotid artery with extracranial-intracranial bypass and trapping. Neurosurg Focus. 2008;24:E13. doi: 10.3171/FOC/2008/24/2/E13. [DOI] [PubMed] [Google Scholar]
- 15.Kazumata K, Nakayama N, Nakamura T, Kamiyama H, Terasaka S, Houkin K. Changing treatment strategy from clipping to radial artery graft bypass and parent artery sacrifice in patients with ruptured blister-like internal carotid artery aneurysms. Neurosurgery. 2014;10(Suppl 1):66–72. doi: 10.1227/NEU.0000000000000076. discussion 73. [DOI] [PubMed] [Google Scholar]
- 16.Walsh KM, Moskowitz SI, Hui FK, Spiotta AM. Multiple overlapping stents as monotherapy in the treatment of ‘blister’ pseudoaneurysms arising from the supraclinoid internal carotid artery: a single institution series and review of the literature. J Neurointerv Surg. 2014;6:184–194. doi: 10.1136/neurintsurg-2013-010648. [DOI] [PubMed] [Google Scholar]
- 17.Leung GK, Tsang AC, Lui WM. Pipeline embolization device for intracranial aneurysm: a systematic review. Clin Neuroradiol. 2012;22:295–303. doi: 10.1007/s00062-012-0178-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim BC, Kwon OK, Oh CW, Bang JS, Hwang G, Jin SC, Park H. Endovascular internal carotid artery trapping for ruptured blood blisterlike aneurysms: long-term results from a single centre. Neuroradiology. 2014;56:211–217. doi: 10.1007/s00234-014-1317-3. [DOI] [PubMed] [Google Scholar]
- 19.Yu-Tse L, Ho-Fai W, Cheng-Chi L, Chu-Mei K, Yi-Chou W, Tao-Chieh Y. Rupture of symptomatic blood blister-like aneurysm of the internal carotid artery: clinical experience and management outcome. Br J Neurosurg. 2012;26:378–382. doi: 10.3109/02688697.2011.631617. [DOI] [PubMed] [Google Scholar]
- 20.Hetzel A, von Reutern G, Wernz MG, Droste DW, Schumacher M. The carotid compression test for therapeutic occlusion of the internal carotid artery. Comparison of angiography with transcranial Doppler sonography. Cerebrovasc Dis. 2000;10:194–199. doi: 10.1159/000016056. [DOI] [PubMed] [Google Scholar]
- 21.Galego O, Nunes C, Morais R, Sargento-Freitas J, Sales F, Machado E. Monitoring balloon test occlusion of the internal carotid artery with transcranial Doppler. A case report and literature review. Neuroradiol J. 2014;27:115–119. doi: 10.15274/NRJ-2014-10014. [DOI] [PMC free article] [PubMed] [Google Scholar]


