Abstract
Purpose: Although many total hip bearing implants are widely used all over the world, simultaneous comparisons across the numerous available bearing surfaces are rare. The purpose of this study was to compare the survivorship of total hip arthroplasty (THA) with six available bearing implants. Methods: We conducted a systematic review of randomized controlled trials (RCTs) reporting survivorship or revision of ceramic-on-ceramic (CoC), ceramic-on-conventional polyethylene (CoPc), ceramic-on-highly-crosslinked polyethylene (CoPxl), metal-on-conventional polyethylene (MoPc), metal-on-highly-crosslinked polyethylene (MoPxl), or metal-on-metal (MoM) bearing implants. The synthesis of present evidence was performed by both the traditional direct-comparison meta-analysis and network meta-analysis. Results: In total, 40 RCTs involving a total of 5321 THAs were identified. The pooled data of network meta-analysis showed no difference in relative risk (RR) of revision across CoC, CoPc, CoPxl and MoPxl bearings. However, the MoM bearing was demonstrated with a significant higher risk of revision compared with CoC (RR 5.10; 95% CI=1.62 to 16.81), CoPc (RR 4.80; 95% CI=1.29 to 17.09), or MoPxl (RR 3.85; 95% CI=1.16 to 14.29), and the MoPc bearing was indicated with a higher risk of revision compared with CoC (RR 2.83; 95% CI=1.20 to 6.63). The ranking probabilities of the effective interventions also revealed the inferiority of the MoM and MoPc implants in survivorship (both 0%, 95% CI=0% to 0%) compared with CoC (39%, 95% CI=0% to 100%), CoPc (33%, 95% CI=0% to 100%), CoPxl (7%, 95% CI=0% to 100%) or MoPxl (21%, 95% CI=0% to 100%). Conclusions: The present evidence indicated the similar performance in survivorship among CoC, CoPc, CoPxl and MoPxl bearing implants, and that all likely have superiority compared with the MoM and MoPc bearing implants in THA procedures. Long-term RCT data are required to confirm these conclusions and better inform clinical decisions.
Keywords: Total hip arthroplasty, bearing surface, survivorship, network meta-analysis, randomized controlled trial
Introduction
Total hip arthroplasty (THA) has proven to be one of the most successful procedures for surgical treatment of advanced degenerative hip diseases for last decades [1,2]. Currently, a number of different total hip bearing components are available to orthopaedic surgeons worldwide [3]. Modern materials such as ceramics, highly cross-linked polyethylene, and metal-on-metal (MoM) articulations with excellent wear characteristics have been widely used to reduce the implants associated osteolysis and loosening, and increase the longevity of THA implants [4,5]. For the last two decades, several systematic reviews and a number of clinical randomized controlled trials (RCTs) comparing the survivorship of THA implants with different bearing surfaces have been reported [6-47]. However, the results of these studies are still much debated and inconsistent.
The objective of our study was to conducted a systematically review of literature and meta-analysis of RCTs to compare the survivorship or the risk of revision among commonly used THA bearing surfaces, including ceramic-on-ceramic (CoC), ceramic-on-conventional polyethylene (CoPc), ceramic-on-highly-crosslinked polyethylene (CoPxl), metal-on-conventional polyethylene (MoPc), metal-on-highly-crosslinked polyethylene (MoPxl), and metal-on-metal (MoM) articulations. We investigated whether there exists difference in survivorship of total hip arthroplasty with different bearing surfaces. The synthesis of present evidence on this issue was performed by both the traditional direct-comparison meta-analysis and network meta-analysis. Unlike the traditional meta-analysis, network meta-analysis permits simultaneous comparison of no less than 3 interventions. Using a Bayesian evidence analysis, all indirect comparison could be taken into account to arrive at a single, integrated estimate of effect of all included treatments based on all the available evidences [48]. Therefore, network meta-analysis seems to be optimal methodological tool for the above question.
Materials and methods
Search strategy and eligibility criteria
Our systematic review was performed in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [49]. Updating to May 2015, all RCTs comparing survivorship or revision rates between THA bearing surfaces for the treatment of degenerative hip diseases in English were identified through an electronic search and manual research by two clinical librarians (S Yin and D Zhang) independently. The sources of electronic searching include MEDLINE (PubMed), EMBASE and The Cochrane Central Register of Controlled Trials. The following key words were used for search: (total hip arthroplasty OR hip replacement OR hip prosthesis) AND (metal OR ceramic OR chromium OR cobalt OR alumina OR aluminum oxide OR polyethylene OR highly cross-linked). (Supplementary 1) In addition, bibliographies of all selected full text articles were reviewed to identify additional articles.
After applying the search strings, we identified 467 potentially eligible articles. Two reviewers (S Yin and D Zhang) independently checked the titles and abstracts of all articles. Of the 467 articles, 45 were duplicates (Figure 1). Two hundred and sixty-five articles were excluded based on their titles and abstracts with apparent lack of relevance. This left 157 articles. The eligibility criteria of the included studies were: (1) patients younger than 75 years of age at the time of surgery, (2) use of random allocation of THA bearing surfaces, (3) inclusion of arms treated with THA procedures with different bearing surfaces, such as CoC, CoPc, CoPxl, MoPc, MoPxl or MoM bearings, (4) patients in included studies were followed up at least 2 year after operation, (5) included studies had to report valid data of survivorship or revision rates of bearing prostheses. Using these criteria, another 103 of the 157 manuscripts were excluded after the abstracts were reviewed.
Figure 1.
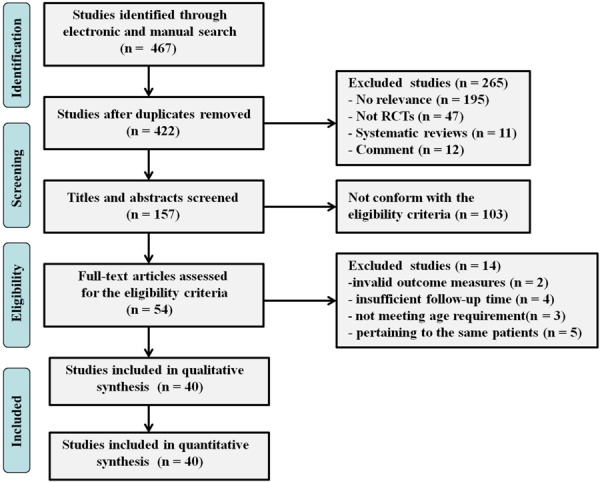
The flow chart shows the article selection process we performed. RCT = randomized controlled trials.
The full texts of all 54 remaining articles were assessed by the same two reviewers. If no agreement could be reached, a third reviewer (Y Qiu) made the final decision. Of these, 14 were excluded for invalid outcome measures, insufficient follow-up times, not meeting age requirement, or pertained to the same patients. Forty eligible trials were eventually identified in present study.
Data extraction and assessment for risk of bias
Two investigator (S Yin and D Zhang) independently reviewed the full manuscripts of eligible studies, extracted the relevant data and reached consensus on each item. If no agreement could be reached, a third reviewer (Z Yin) made the final decision. Data included demographics, methodological characteristics, inclusion and exclusion criteria, implant types of bearing prostheses, implant revision events, length of follow-up period, and number of participants lost to follow-up. The implant survivorship or revision rate for any reason at last follow-up was considered to be ultimate outcome measure.
The risk of bias was independently assessed by two reviewers (S Yin and D Zhang) using the 12 criteria recommended by the Cochrane Back Review Group [50]. The reviewers tried to reach consensus on each criteria. Based on the recommendation by the Cochrane Back Review Group, studies were rated as having a “low risk of bias” when at least 6 of the 12 criteria were met without serious flaws. Studies with serious flaws, or those in which fewer than 6 of the criteria were met were rated as having “high risk of bias”.
Statistical analysis
The numbers of implants with different bearing surfaces requiring revision at last follow-up were reported as events and compared with relative risks (RRs) with 95% confidence intervals (CIs). We first performed a traditional direct-comparison meta-analysis with Review Manager software (version 5.1.6) provided by the Cochrane Collaboration. The statistical method of Mantel-Haenszel with random effects method was used for dichotomous outcomes. The heterogeneity was assessed by using the chi-squared test. The value of I 2 greater than 50% would be considered substantial heterogeneity [51].
For indirect comparisons, a network meta-analysis was conducted using WinBUGS software (version 1.4.3, MRC Biostatistics Unit, Cambridge, UK) and R software GeMTC package (version 2.15.2; http://www.R-project.org) with random effects chaimani models (Supplementary 2). The network meta-analysis could provide information about ranking of all evaluated bearing implants for outcome [52]. A sensitivity analysis was performed for the measured effects omitting the study which may largely influence the clinical findings. In order to evaluate the mid-long term effects among the implants with different bearing surfaces, a subanalysis including only RCTs with a minimum 10-year follow-up was also performed.
Results
Description of included studies
The process of identifying eligible studies is summarized in Figure 1. Forty eligible trials were eventually identified in our meta-analysis, with a total of 5321 hips randomized to receive any of 6 THA bearing implants mentioned above [8-47]. The average follow-up was 6.6 years (range, 2-12.4 years). Of all the included articles, nine reports no less than 10 years follow-up. The investigation included several comparisons: one MoPc versus MoPxl versus CoPc versus CoPxl [8], one MoPc versus MoPxl versus CoC [9], one MoPc versus MoM versus CoPc [10], eleven MoPc versus MoPxl [11-21], five MoPc versus MoM [22-26], four CoC versus CoPc [27-30], four CoC versus CoPxl [31-34], three CoC versus MoPc [35-37], three MoPc versus CoPc [38-40], two MoPxl versus CoPxl [41,42], two MoPxl versus MoM [43,44], one CoC versus MoPxl [45], one CoC versus MoM [46], and one CoPc versus MoM [47]. The characteristics of included studies are summarized in Table 1 and the network evidence of these trials are summarized in Figure 2.
Table 1.
Summary of the included studies
| Study | Follow up (years) | Interventions | Group A | Group B | Group C | Group D | ||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Number of hips | Number of revisions | Number of hips | Number of revisions | Number of hips | Number of revisions | Number of hips | Number of revisions | |||
| Morison 2014 | 6.8 | MoPc VS MoPxl VS CoPc VS CoPxl | 21 | 2 | 24 | 0 | 22 | 1 | 24 | 2 |
| Nikolaou 2012 | 5 | MoPc VS MoPxl VS CoC | 36 | 2 | 32 | 0 | 34 | 0 | NR | NR |
| Bjorgul 2013 | 7 | MoPc VS MoM VS CoPc | 137 | 3 | 129 | 8 | 131 | 1 | NR | NR |
| Engh 2012 | 10 | MoPc VS MoPxl | 114 | 11 | 116 | 2 | NR | NR | NR | NR |
| García-Rey 2013 | 10 | MoPc VS MoPxl | 45 | 0 | 45 | 1 | NR | NR | NR | NR |
| Johanson 2012 | 10 | MoPc VS MoPxl | 30 | 1 | 31 | 2 | NR | NR | NR | NR |
| Geerdink 2009 | 8 | MoPc VS MoPxl | 26 | 1 | 22 | 0 | NR | NR | NR | NR |
| Thomas 2011 | 7 | MoPc VS MoPxl | 27 | 0 | 27 | 0 | NR | NR | NR | NR |
| Mutimer 2010 | 5.5 | MoPc VS MoPxl | 61 | 3 | 61 | 0 | NR | NR | NR | NR |
| Digas 2007 | 5 | MoPc VS MoPxl | 29 | 0 | 32 | 1 | NR | NR | NR | NR |
| Geerdink 2006 | 5 | MoPc VS MoPxl | 67 | 2 | 66 | 0 | NR | NR | NR | NR |
| Triclot 2007 | 4.9 | MoPc VS MoPxl | 53 | 1 | 49 | 1 | NR | NR | NR | NR |
| Calvert 2009 | 3 | MoPc VS MoPxl | 60 | 0 | 59 | 0 | NR | NR | NR | NR |
| Glyn-Jones 2008 | 3 | MoPc VS MoPxl | 27 | 0 | 27 | 0 | NR | NR | NR | NR |
| Zijlstra 2010 | 10 | MoPc VS MoM | 98 | 2 | 102 | 4 | NR | NR | NR | NR |
| Lombardi 2004 | 6 | MoPc VS MoM | 97 | 1 | 98 | 0 | NR | NR | NR | NR |
| Hanna 2012 | 3 | MoPc VS MoM | 23 | 0 | 28 | 0 | NR | NR | NR | NR |
| Zijlstra 2014 | 3 | MoPc VS MoM | 54 | 0 | 50 | 4 | NR | NR | NR | NR |
| Malviya 2011 | 2 | MoPc VS MoM | 50 | 2 | 50 | 2 | NR | NR | NR | NR |
| Lewis 2010 | 10 | CoC VS CoPc | 30 | 1 | 26 | 1 | NR | NR | NR | NR |
| Ochs 2007 | 8.1 | CoC VS CoPc | 35 | 1 | 31 | 1 | NR | NR | NR | NR |
| Amanatullah 2011 | 5 | CoC VS CoPc | 196 | 11 | 161 | 3 | NR | NR | NR | NR |
| Cai 2012 | 3 | CoC VS CoPc | 51 | 2 | 62 | 3 | NR | NR | NR | NR |
| Kim 2013 | 12.4 | CoC VS CoPxl | 100 | 1 | 100 | 1 | NR | NR | NR | NR |
| Lombardi 2010 | 6 | CoC VS CoPxl | 65 | 3 | 45 | 3 | NR | NR | NR | NR |
| Beaupre 2013 | 5 | CoC VS CoPxl | 48 | 0 | 44 | 2 | NR | NR | NR | NR |
| Hamilton 2010 | 3 | CoC VS CoPxl | 177 | 4 | 87 | 2 | NR | NR | NR | NR |
| Vendittoli 2013 | 12.3 | CoC VS MoPc | 71 | 1 | 69 | 8 | NR | NR | NR | NR |
| D’Antonio 2012 | 10 | CoC VS MoPc | 194 | 6 | 95 | 10 | NR | NR | NR | NR |
| Seyler 2006 | 7 | CoC VS MoPc | 158 | 6 | 52 | 3 | NR | NR | NR | NR |
| Dahl 2013 | 10 | MoPc VS CoPc | 23 | 2 | 20 | 2 | NR | NR | NR | NR |
| Kim 2005 | 7.1 | MoPc VS CoPc | 52 | 0 | 52 | 2 | NR | NR | NR | NR |
| Kraay 2006 | 4 | MoPc VS CoPc | 30 | 0 | 30 | 0 | NR | NR | NR | NR |
| Nakahara 2010 | 6.7 | MoPxl VS CoPxl | 51 | 0 | 51 | 0 | NR | NR | NR | NR |
| Kawate 2009 | 5 | MoPxl VS CoPxl | 30 | 0 | 32 | 0 | NR | NR | NR | NR |
| Engh 2014 | 5 | MoPxl VS MoM | 37 | 1 | 63 | 1 | NR | NR | NR | NR |
| Jacobs 2004 | 3.7 | MoPxl VS MoM | 76 | 1 | 95 | 1 | NR | NR | NR | NR |
| Bascarevic 2010 | 4.2 | CoC VS MoPxl | 82 | 0 | 75 | 2 | NR | NR | NR | NR |
| Pabinger 2003 | 2 | CoPc VS MoM | 29 | 0 | 32 | 1 | NR | NR | NR | NR |
| Desmarchelier 2013 | 9 | CoC VS MoM | 125 | 1 | 125 | 3 | NR | NR | NR | NR |
Abbreviation: MoPc = metal-on-conventional polyethylene, MoPxl = metal-on-highly crosslinked polyethylene, CoPc = ceramic-on-conventional polyethylene, CoPxl = ceramic-on-highly crosslinked polyethylene, CoC = ceramic-on-ceramic, MoM = metal-on-metal, NR = no report.
Figure 2.
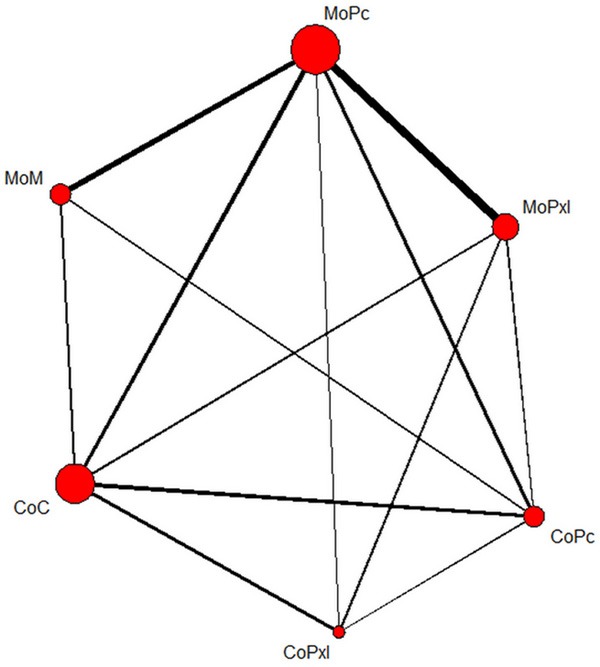
Network evidence of included studies. The size of red circles represent the total hips number of each invention. The thickness of solid lines represent the number of trials comparing the connected inventions. MoPc = metal-on-conventional polyethylene, MoPxl = metal-on-highly crosslinked polyethylene, CoPc = ceramic-on-conventional polyethylene, CoPxl = ceramic-on-highly crosslinked polyethylene, CoC = ceramic-on-ceramic, MoM = metal-on-metal.
Risk of bias in included studies
The risk of bias for the included studies was summarized in Figure 3. Twenty-four studies (60%) reported adequate allocation sequences and twenty-three (57.5%) reported adequate allocation concealments. Five studies (12.5%) described blinding of patients, surgeons, and outcome assessors. Although none of the included studies met fewer than 6 of the criteria, two studies Lombardi et al. [23] and Amanatullah et al. [29] with significant patient loss to follow-up (49.2% and 38.4%, respectively) were considered with serious flaws and rated as having “high risk of bias”.
Figure 3.
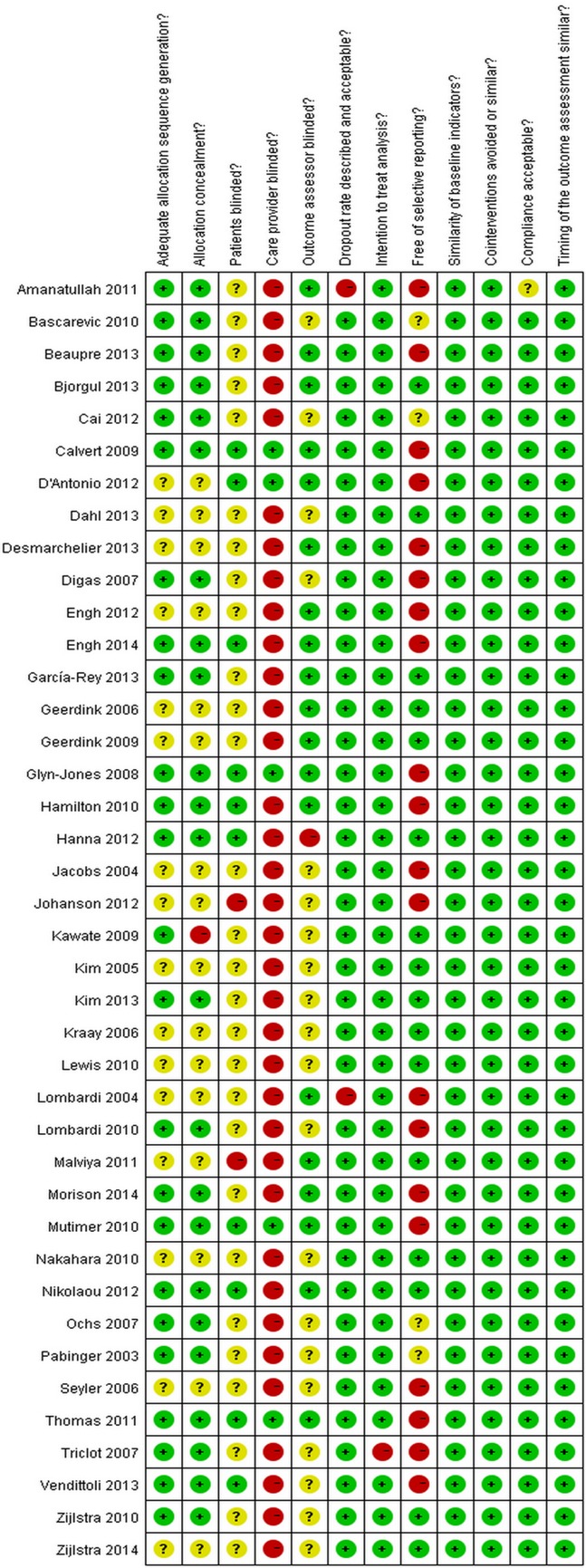
The risk of bias for the included studies.
Direct-comparison meta-analysis
In the possible pair-wise comparison between the bearing types, fourteen had been studied directly in one or more trials. Table 2 showed the relative risks of revision surgery for each of these direct comparisons. In all direct comparisons, there was no observed heterogeneity. A total of ten trials reported a direct comparison of MoPxl versus MoPc implants. Overall pair-wise meta-analysis found MoPc associated with a significant trend towards an increased risk of revision when compared with MoPxl implants (RR 0.43; 95% CI=0.19 to 0.96; P<0.05) (Figure 4). Another pair-wise meta-analysis was performed for 4 RCTs comparing CoC versus MoPc implants. The pooled relative risk for revision showed a significant difference favoring CoC over MoPc implants (RR 0.33; 95% CI=0.16 to 0.67; P<0.01) (Figure 5). The third direct-comparison meta-analysis was conducted pooling only two studies comparing CoPc versus MoM implants (RR 0.17; 95% CI=0.03 to 0.96; P<0.05) (Figure 6), revealing a significantly increased risk of revision in MoM bearing implants over CoPc. There were no differences in the risk of revision in other possible direct-comparison meta-analyses among bearing types.
Table 2.
Relative risk of revision surgery for direct-comparison meta-analysis and network meta-analysis including all RCTs
| CoC | 1.99 (0.64-7.42) | 1.07 (0.42-3.05) | 5.10 (1.62-16.81) | 1.34 (0.41-4.34) | 2.83 (1.20-6.63) |
| 0.71 (0.26-1.92) | CoPxl | 0.52 (0.13-2.33) | 2.56 (0.51-12.16) | 0.68 (0.14-3.06) | 1.42 (0.35-5.46) |
| 1.62 (0.66-4.00) | 1.83 (0.18-18.84) | CoPc | 4.80 (1.29-17.09) | 1.26 (0.32-4.34) | 2.64 (0.89-7.04) |
| 0.33 (0.04-3.16) | - | 0.17 (0.03-0.96) | MoM | 0.26 (0.07-0.86) | 0.55 (0.20-1.43) |
| 0.45 (0.06-3.42) | 1.57 (0.31-7.98) | 3.26 (0.14-76.10) | 0.68 (0.10-4.78) | MoPxl | 2.10 (0.82-5.48) |
| 0.33 (0.16-0.67) | 0.88 (0.13-5.68) | 0.85 (0.27-2.64) | 2.02 (0.88-4.65) | 0.43 (0.19-0.96) | MoPc |
Relative risk (RR) of revision surgery lower than 1 favor the column-defining treatment. RRs in lower left of the table represented the results of direct-comparison meta-analysis, and the upper right of the table represented the results of network meta-analysis. Abbreviation: MoPc = metal-on-conventional polyethylene, MoPxl = metal-on-highly crosslinked polyethylene, CoPc = ceramic-on-conventional polyethylene, CoPxl = ceramic-on-highly crosslinked polyethylene, CoC = ceramic-on-ceramic, MoM = metal-on-metal, NR = no report.
Figure 4.
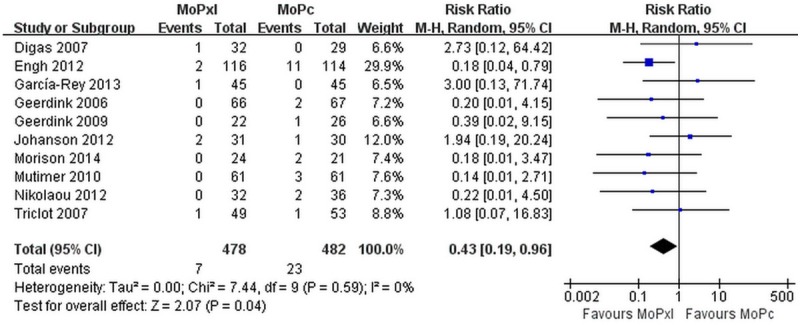
The forest plot of pair-wised meta-analysis comparing survivorship between MoPxl and MoPc bearings. MoPc = metal-on-conventional polyethylene, MoPxl = metal-on-highly crosslinked polyethylene.
Figure 5.
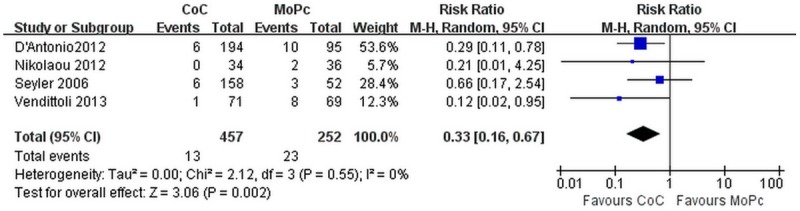
The forest plot of pair-wised meta-analysis comparing survivorship between CoC and MoPc bearings. CoC = ceramic-on-ceramic, MoPc = metal-on-conventional polyethylene.
Figure 6.
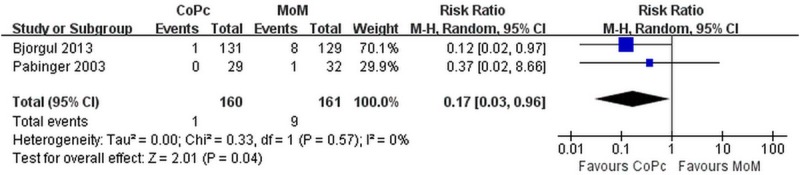
The forest plot of pair-wised meta-analysis comparing survivorship between CoPc and MoM bearings. CoPc = ceramic-on-conventional polyethylene, MoM = metal-on-metal.
Table 3 showed the relative risks of revision surgery for direct-comparison meta-analysis including RCTs with at least 10 years follow-up. There was also no observed heterogeneity in all 6 possible pair-wise comparisons. With a minimum 10-year follow-up, only one pair-wise meta-analysis demonstrated a significant trend with 4-fold increased risk of revision to MoPc when compared with the CoC implants (RR 0.25; 95% CI=0.10 to 0.60; P<0.01) (Figure 7). For the other five pair-wise meta-analyses, no differences in the risk of revision across bearing types were observed any more.
Table 3.
Relative risk of revision surgery for direct-comparison meta-analysis and network meta-analysis including RCTs with at least 10 years follow-up
| CoC | 0.92 (0.01-68.63) | 3.13 (0.20-47.86) | 10.86 (0.33-317.71) | 2.75 (0.24-55.96) | 4.73 (0.75-29.39) |
| 1.00 (0.06-15.77) | CoPxl | 3.05 (0.02-494.64) | 11.11 (0.05-2969.49) | 2.97 (0.02-578.01) | 4.84 (0.05-575.65) |
| 0.87 (0.06-13.18) | - | CoPc | 3.51 (0.07-177.98) | 0.92 (0.04-29.05) | 1.52 (0.11-21.63) |
| - | - | - | MoM | 0.25 (0.11-11.18) | 0.43 (0.02-7.82) |
| - | - | - | - | MoPxl | 1.70 (0.18-9.55) |
| 0.25 (0.10-0.60) | - | 1.15 (0.18-7.43) | 1.92 (0.36-10.25) | 0.73 (0.11-4.98) | MoPc |
Relative risk (RR) of revision surgery lower than 1 favor the column-defining treatment. RRs in lower left of the table represented the results of direct-comparison meta-analysis, and the upper right of the table represented the results of network meta-analysis. Abbreviation: MoPc = metal-on-conventional polyethylene, MoPxl = metal-on-highly crosslinked polyethylene, CoPc = ceramic-on-conventional polyethylene, CoPxl = ceramic-on-highly crosslinked polyethylene, CoC = ceramic-on-ceramic, MoM = metal-on-metal, NR = no report.
Figure 7.
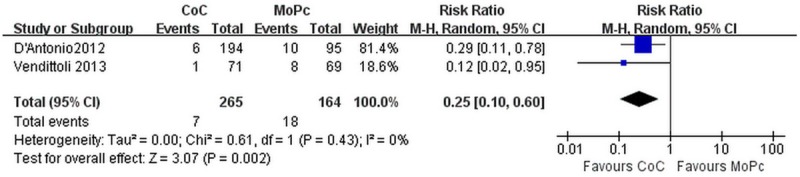
The forest plot of pair-wised meta-analysis comparing survivorship between CoC and MoPc bearings including RCTs with at least 10 years follow-up. CoC = ceramic-on-ceramic, MoPc = metal-on-conventional polyethylene, RCT-randomized controlled trials.
Network meta-analysis
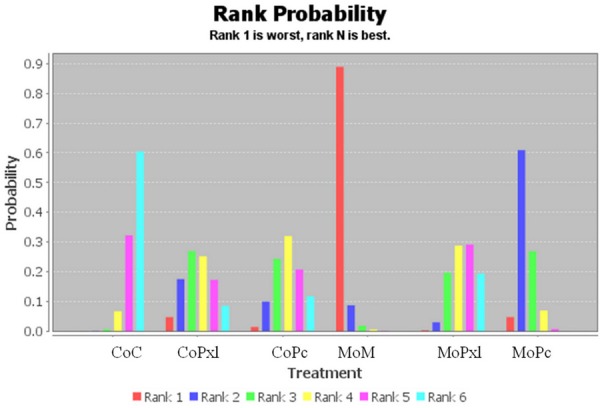
A network meta-analysis was performed for all 40 included studies (Table 2). The pooled data of network meta-analysis showed no difference in terms of risk of revision among CoC, CoPc, CoPxl and MoPxl implants. However, MoM implants were associated with significant higher risks of revision when compared with CoC (RR 5.10; 95% CI=1.62 to 16.81), CoPc (RR 4.80; 95% CI=1.29 to 17.09), MoPxl (RR 3.85; 95% CI=1.16 to 14.29), and a non-significant trend towards a increased risk of revision when compared with CoPxl implants (RR 2.56; 95% CI=0.51 to 12.16). Meanwhile, the MoPc implants were demonstrated with a significant increased risk of revision compared with CoC (RR 2.83; 95% CI=1.20 to 6.63), and non-significant trends of higher risk of revision when compared with CoPc (RR 2.64; 95% CI=0.89 to 7.04), CoPxl (RR 1.42; 95% CI=0.35 to 5.46) and MoPxl (RR 2.10; 95% CI=0.82 to 5.48) implants. Moreover, a rank probability analysis was performed to test the superiority among the bearing types (Figure 8). As a consequence, CoC bearing implants achieved the highest probability to be the best intervention (39%, 95% CI=0% to 100%). The following probabilities of being ranked the best intervention were 33% (95% CI=0% to 100%) for CoPc, 21% (95% CI=0% to 100%) for MoPxl, and 7% (95% CI=0% to 100%) for CoPxl. The MoM and MoPc implants achieved the lowest probabilities to be the best intervention (both 0%, 95% CI=0% to 0%).
Figure 8.
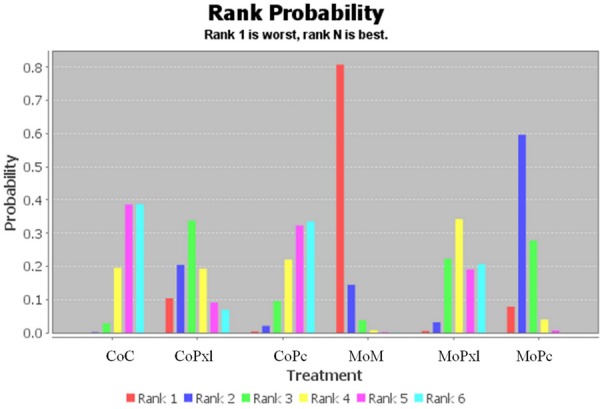
Rank probabilities for survivorship among different bearing implants including all studies. MoPc = metal-on-conventional polyethylene, MoPxl = metal-on-highly crosslinked polyethylene, CoPc = ceramic-on-conventional polyethylene, CoPxl = ceramic-on-highly crosslinked polyethylene, CoC = ceramic-on-ceramic, MoM = metal-on-metal.
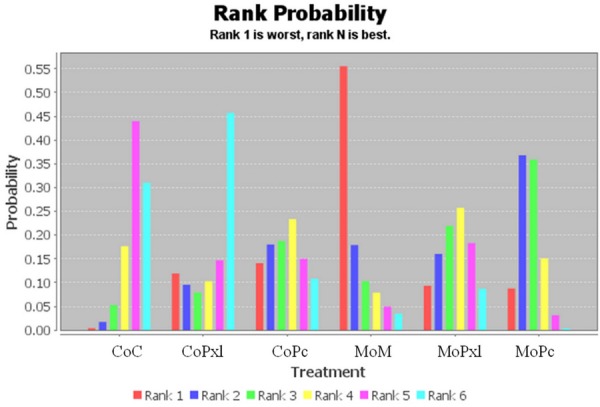
A sensitivity analysis was performed by repeating the network analysis after omitting two studies Lombardi et al. [23] and Amanatullah et al. [29] with “high risk of bias”. The pooled results of the sensitivity analysis were summarized in Table 4. The probabilities of being ranked the best intervention were 60% (95% CI=0% to 100%) for CoC, 19% (95% CI=0% to 100%) for MoPxl, 12% (95% CI=0% to 100%) for CoPc, 9% (95% CI=0% to 100%) for CoPxl, and 0% (95% CI=0% to 0%) for MoM and MoPc implants (Figure 9).
Table 4.
Relative risk of revision surgery for network meta-analysis after the sensitivity analysis
| CoC | 1.95 (0.68-6.60) | 1.74 (0.60-5.32) | 6.45 (2.20-22.35) | 1.50 (0.51-4.48) | 3.07 (1.49-7.30) |
| CoPxl | 0.88 (0.19-3.66) | 3.26 (0.74-14.28) | 0.74 (0.17-3.01) | 1.56 (0.43-5.05) | |
| CoPc | 3.59 (1.05-16.15) | 0.86 (0.20-3.20) | 1.74 (0.58-5.24) | ||
| MoM | 0.23 (0.05-0.72) | 0.48 (0.17-1.19) | |||
| MoPxl | 2.04 (0.89-5.09) | ||||
| MoPc |
Relative risk (RR) of revision surgery lower than 1 favor the column-defining treatment. Abbreviation: MoPc = metal-on-conventional polyethylene, MoPxl = metal-on-highly crosslinked polyethylene, CoPc = ceramic-on-conventional polyethylene, CoPxl = ceramic-on-highly crosslinked polyethylene, CoC = ceramic-on-ceramic, MoM = metal-on-metal, NR = no report.
Figure 9.
Rank probabilities for survivorship among different bearing implants after sensitivity analysis by omitting two studies with significant patient loss to follow-up. MoPc = metal-on-conventional polyethylene, MoPxl = metal-on-highly crosslinked polyethylene, CoPc = ceramic-on-conventional polyethylene, CoPxl = ceramic-on-highly crosslinked polyethylene, CoC = ceramic-on-ceramic, MoM = metal-on-metal.
When the network meta-analysis was restricted to trials with at least 10 years follow-up time, the MoM implants were non-significantly associated with a 11-fold, 11-fold, 4-fold and 4-fold increased risks of revision when compared with CoPxl, CoC, MoPxl, and CoPc implants, respectively (Table 3). Meanwhile, the MoPc implants were non-significantly associated with a 5-fold, 5-fold, 2-fold and 2-fold increased risks of revision when compared with CoPxl, CoC, MoPxl, and CoPc implants, respectively. The probabilities of being ranked the best intervention were 46% (95% CI=0% to 100%) for CoPxl, 31% (95% CI=0% to 100%) for CoC, 11% (95% CI=0% to 100%) for CoPc, 9% (95% CI=0% to 100%) for MoPxl, and 3% (95% CI=0% to 100%) for MoM and 0% (95% CI=0% to 0%) for MoPc (Figure 10).
Figure 10.
Rank probabilities for survivorship among different bearing implants including trials with at least 10 years follow-up period. MoPc = metal-on-conventional polyethylene, MoPxl = metal-on-highly crosslinked polyethylene, CoPc = ceramic-on-conventional polyethylene, CoPxl = ceramic-on-highly crosslinked polyethylene, CoC = ceramic-on-ceramic, MoM = metal-on-metal.
Discussion
In the past decades, numerous efforts have been made to improve the survival probability of primary THA implants. Submicron debris generated by the process of osteolysis and implant loosening remains a significant problem in THA procedure [53]. Therefore, the longevity of different bearing surfaces has become primary research interest of the prosthetic implant. However, there is still much debate about the appropriate bearings. Shetty et al. [6] conducted a meta-analysis comparing survivorship among MoM, CoC and MoP bearing implants in patients younger than 55 years old, determining that the MOM bearing provided the best survival rate and superiority in young active patients. The systematic review did not strictly apply to the principle of PRISMA, and the included studies were not randomized controlled trials only. With the advances and widely use of ceramics and highly cross-linked polyethylene in recent years, the superiority of bearing implants deserves a fresh analysis by updating the literatures with high quality. Several systematic reviews and meta-analyses were also performed to compare the survivorship or revision rates between two bearing implants [7,54-58]. However, the scarcity of relevant RCT literatures limited performing a direct meta-analysis, and it was difficult to draw a comprehensive conclusion comparing survivorship of more than two bearing implants. Network analysis is a optimal method for this problem by creating indirect comparisons, and it also could identify whether the superiority in survivorship exists or not across all different bearing implants. The network analysis is also applied to increase the power of the tests and reduce type I statistical errors [59].
Our present study integrated the direct comparison and network meta-analysis that summarized all the available evidence from RCTs comparing survivorship of all commonly used THA bearing implants including CoC, CoPc, CoPxl, MoPc, MoPxl and MoM articulations. Forty RCTs involving 5321 hips were identified for both direct-comparison meta-analysis and network meta-analysis. Considering the heterogeneity in follow-up period among the included studies, a subanalysis was performed including only RCTs with a minimum 10-year follow-up to evaluate the mid-long term effects. Based on the 12 criteria recommended by the Cochrane Back Review Group, the methodological qualities of all included studies were accessed. Of all 40 reports, two studies Lombardi et al. and Amanatullah et al. with significant patient loss to follow-up (49.2% and 38.4%, respectively) were rated as “high risk of bias”. A sensitivity analysis was conducted by repeating the network analysis after omitting the two trials.
Our collaborative meta-analysis indicates that four bearing implants including CoC, CoPc, CoPxl and MoPxl prostheses perform similarly in survivorship or revision rates, and that all likely have superiority compared with the MoM and MoPc bearing implants. The pooled results of pair-wise comparison and network meta-analysis showed no difference in terms of risks of revision among CoC, CoPc, CoPxl and MoPxl bearing implants. Meanwhile, the inferiorities of MoM and MoPc bearings compared with other four bearing implants were demonstrated by the network meta-analysis. The ranking probabilities of the effective interventions for both MoM and MoPc bearing implants in survivorship were 0% with credible interval from 0% to 0%, representing the significant inferiorities in comparison to other four bearing prostheses. A sensitivity analysis omitting two studies with high risk of bias and a subanalysis including only RCTs with a minimum 10-year follow-up also showed the similar results.
Readers should be aware of limitations in the literature in general and our study in particular. First, for maximizing the number of eligible studies, the length of follow-up time differed greatly (ranging from 2 years to 12.4 years). Second, owning to the lack of high quality research with more than 10 years follow-up, it was difficult to draw conclusions regarding the long-term results of followup. Although a subanalysis including only RCTs with a minimum 10-year follow-up was conducted in our present study, the absence of significant statistical differences in pooled data demonstrated once more the lack of relevant literature. Third, the low event rates in most of included studies (only 150 events in 5321 hips, 2.8%) created a degree of imprecision. The persistently wide confidence intervals especially in the subanalysis including RCTs with a minimum 10-year follow-up indicated the possibility of Type II statistical errors. Fourth, the longevity of different bearing surfaces may also depend on the methods of fixation, design, femoral head size, and other operative or implant-related factors. In present study, we could not conduct a subgroup analysis based on these factors owning to the scarcity in relevant literature. Other clinical outcome such as patient pain, function of hip joint, dislocation rate, patient satisfaction and employment rate had not been involved in our research.
The emphasis in present study was placed on the survivorship or revision rates of different bearing prostheses. However, many other factors such as implant-specific issues, cost of the implant, familiarity with the design and instruments, and ease of use also influence the surgeon’s choice of a particular total hip implant. There are several major concerns for the MoM bearing implants, including aseptic lymphocytic vasculitis associated lesion (ALVAL), pseudotumor, and elevated blood metal ion levels [60,61]. There are also growing evidences from national joint registry data and multicentre randomized controlled trials that hip replacements with MoM bearing implants have significantly higher revision rates compared to other bearing prostheses, that in agreement with our result [58,62]. Owing to these suspected harmful complications, high revision rates, recalls of two models made by DePuy Orthopedics, and FDA requirements for surveillance, the MoM bearing implants should be used with caution. The disadvantages of the CoC bearing implants include component-related noise and ceramic fracture risk. The incidence of component-related noise was reported between 0.3% and 21% in CoC THA prostheses, that was 14.7 times higher than CoP bearings [56,63]. The occurrence of ceramic fracture is reported to occur in between 0.013% and 3.7% of patients who have undergone a COC THA [46,64]. Recently another notable implant-specific complication reported as a potential clinical concern was trunnionosis at the head-neck taper junction in MoP and MoPxl THA prostheses [65].
The present systematic review and network meta-analysis indicated the similar performance in survivorship among CoC, CoPc, CoPxl and MoPxl bearing implants, and that all likely have superiority compared with the MoM and MoPc bearing implants in THA procedures. In addition, surgeons should also consider about other factors such as implant-specific complications, cost of the implant, familiarity with the design and instruments to make the appropriate choice of different bearing implants for THA procedures. Future studies with high methodologic quality and long-term follow-up periods are needed for updated analyses to better evaluate the long-term survivorship among different THA bearing prostheses.
Disclosure of conflict of interest
None.
Supporting Information
References
- 1.Keurentjes JC, Fiocco M, So-Osman C, Onstenk R, Koopman-Van Gemert AW, Pöll RG, Kroon HM, Vliet Vlieland TP, Nelissen RG. Patients with severe radiographic osteoarthritis have a better prognosis in physical functioning after hip and knee replacement: a cohort-study. PLoS One. 2013;8:e59500. doi: 10.1371/journal.pone.0059500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keurentjes JC, Fiocco M, Nelissen RG. Willingness to undergo surgery again validated clinically important differences in health-related quality of life after total hip replacement or total knee replacement surgery. J Clin Epidemiol. 2014;67:114–120. doi: 10.1016/j.jclinepi.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Murray DW, Carr AJ, Bulstrode CJ. Which primary total hip replacement? J Bone Joint Surg Br. 1995;77:520–527. [PubMed] [Google Scholar]
- 4.Kress AM, Schmidt R, Holzwarth U, Forst R, Mueller LA. Excellent results with cementless total hip arthroplasty and alumina-on-alumina pairing: minimum ten-year follow-up. Int Orthop. 2011;35:195–200. doi: 10.1007/s00264-010-1150-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harris WH. Highly cross-linked, electron-beamirradiated, melted polyethylene: some pros. Clin Orthop Relat Res. 2004;429:63–67. doi: 10.1097/01.blo.0000149827.55160.42. [DOI] [PubMed] [Google Scholar]
- 6.Shetty V, Shitole B, Shetty G, Thakur H, Bhandari M. Optimal bearing surfaces for total hip replacement in the young patients: a metaanalysis. Int Orthop. 2011;35:1281–1287. doi: 10.1007/s00264-010-1104-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keurentjes JC, Pijls BG, Van Tol FR, Mentink JF, Mes SD, Schoones JW, Fiocco M, Sedrakyan A, Nelissen RG. Which implant should we use for primary total hip replacement? A systematic review and meta-analysis. J Bone Joint Surg Am. 2014;96(Suppl 1):79–97. doi: 10.2106/JBJS.N.00397. [DOI] [PubMed] [Google Scholar]
- 8.Morison ZA, Patil S, Khan HA, Bogoch ER, Schemitsch EH, Waddell JP. A randomized controlled trial comparing Oxinium and cobaltchrome on standard and cross-linked polyethylene. J Arthroplasty. 2014;29:164–168. doi: 10.1016/j.arth.2014.04.046. [DOI] [PubMed] [Google Scholar]
- 9.Nikolaou VS, Edwards MR, Bogoch E, Schemitsch EH, Waddell JP. A prospective randomized controlled trial comparing three alternative bearing surfaces in primary total hip replacement. J Bone Joint Surg Br. 2012;94:459–465. doi: 10.1302/0301-620X.94B4.27735. [DOI] [PubMed] [Google Scholar]
- 10.Bjorgul K, Novicoff WN, Andersen ST, Ahlund OR, Bunes A, Wiig M, Brevig K. High rate of revision and a high incidence of randiolucent lines around Metasul metal-on-metal total hip replacements: results from a randomized controlled trials of three bearings after seven years. Bone Joint J. 2013;95-B:881–886. doi: 10.1302/0301-620X.95B7.31067. [DOI] [PubMed] [Google Scholar]
- 11.Engh CA Jr, Hopper RH Jr, Huynh C, Ho H, Sritulanondha S, Engh CA Sr. A prospective, randomized study of cross-linked and noncross-linked polyethylene for total hip arthroplasty at 10-year follow-up. J Arthroplasty. 2012;27:2–7. doi: 10.1016/j.arth.2012.03.048. [DOI] [PubMed] [Google Scholar]
- 12.García-Rey E, García-Cimbrelo E, Cruz-Pardos A. New polyethylenes in total hip replacement: A ten- to 12-year follow-up study. Bone Joint J. 2013;95-B:326–332. doi: 10.1302/0301-620X.95B3.29456. [DOI] [PubMed] [Google Scholar]
- 13.Johanson PE, Digas G, Herberts P, Thanner J, Kärrholm J. Highly crosslinked polyethylene does not reduce aseptic loosening in cemented THA 10-year findings of a randomized study. Clin Orthop Relat Res. 2012;470:3083–3093. doi: 10.1007/s11999-012-2400-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geerdink CH, Grimm B, Vencken W, Heyligers IC, Tonino AJ. Cross-linked Compared with Historical Polyethylene in THA: a 8-year clinical study. Clin Orthop Relat Res. 2009;467:979–984. doi: 10.1007/s11999-008-0628-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomas GE, Simpson DJ, Mehmood S, Taylor A, McLardy-Smith P, Gill HS, Murray DW, Glyn-Jones S. The seven-year wear of highly crosslinked polyethylene in total hip arthroplasty: a double-blind, randomized controlled trial using radiostereometric analysis. J Bone Joint Surg Am. 2011;93:716–722. doi: 10.2106/JBJS.J.00287. [DOI] [PubMed] [Google Scholar]
- 16.Mutimer J, Devane PA, Adams K, Horne JG. Highly crosslinked polyethylene reduces wear in total hip arthroplasty at 5 years. Clin Orthop Relat Res. 2010;468:3228–3233. doi: 10.1007/s11999-010-1379-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Digas G, Kärrholm J, Thanner J, Herberts P. 5-year experience of highly cross-linked polyethylene in cemented and uncemented sockets: two randomized studies using radiostereometric analysis. Acta Orthop. 2007;78:746–754. doi: 10.1080/17453670710014518. [DOI] [PubMed] [Google Scholar]
- 18.Geerdink CH, Grimm B, Ramakrishnan R, Rondhuis J, Verburg AJ, Tonino AJ. Crosslinked polyethylene compared to conventional polyethylene in total hip replacement: pre-clinical evaluation, in-vitro testing and prospective clinical follow-up study. Acta Orthop. 2006;77:719–725. doi: 10.1080/17453670610012890. [DOI] [PubMed] [Google Scholar]
- 19.Triclot P, Grosjean G, El Masri F, Courpied JP, Hamadouche M. A comparison of the penetration rate of two polyethylene acetabular liners of different levels of cross-linking. A prospective randomised trial. J Bone Joint Surg Br. 2007;89:1439–1445. doi: 10.1302/0301-620X.89B11.19543. [DOI] [PubMed] [Google Scholar]
- 20.Calvert GT, Devane PA, Fielden J, Adams K, Horne JG. A double-blind, prospective, randomized controlled trial comparing highly crosslinked and conventional polyethylene in primary total hip arthroplasty. J Arthroplasty. 2009;24:505–510. doi: 10.1016/j.arth.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 21.Glyn-Jones S, McLardy-Smith P, Gill HS, Murray DW. The creep and wear of highly cross-linked polyethylene: a three-year randomised, controlled trial using radiostereometric analysis. J Bone Joint Surg Br. 2008;90:556–561. doi: 10.1302/0301-620X.90B5.20545. [DOI] [PubMed] [Google Scholar]
- 22.Zijlstra WP, van Raay JJ, Bulstra SK, Deutman R. No superiority of cemented metal-on-metal over metal-on-polyethylene THA in a randomized controlled trial at 10-year follow-up. Orthopedics. 2010:33. doi: 10.3928/01477447-20100129-19. [DOI] [PubMed] [Google Scholar]
- 23.Lombardi AV Jr, Mallory TH, Cuckler JM, Williams J, Berend KR, Smith TM. Mid-term results of a polyethylene-free metal-on-metal articulation. J Arthroplasty. 2004;19:42–47. doi: 10.1016/j.arth.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 24.Hanna SA, Sewell MD, Sri-Ram K, Miles J, Aston WJ, Pollock RC, Carrington RW, Briggs TW. The effect of femoral head size on functional outcome in primary total hip arthroplasty: a single-blinded randomised controlled trial. Hip Int. 2012;22:592–597. doi: 10.5301/HIP.2012.10360. [DOI] [PubMed] [Google Scholar]
- 25.Zijlstra WP, van der Veen HC, van den Akker-Scheek I, Zee MJ, Bulstra SK, van Raay JJ. Acetabular bone density and metal ions after metal-on-metal versus metal-on-polyethylene total hip arthroplasty; short-term results. Hip Int. 2014;24:136–143. doi: 10.5301/hipint.5000087. [DOI] [PubMed] [Google Scholar]
- 26.Malviya A, Ramaskandhan JR, Bowman R, Hashmi M, Holland JP, Kometa S, Lingard E. What advantage is there to be gained using large modular metal-on-metal bearings in routine primary hip replacement? A preliminary report of a prospective randomised controlled trial. J Bone Joint Surg Br. 2011;93:1602–1609. doi: 10.1302/0301-620X.93B12.27533. [DOI] [PubMed] [Google Scholar]
- 27.Lewis PM, Al-Belooshi A, Olsen M, Schemitch EH, Waddell JP. Prospective randomized trial comparing alumina ceramic-on-ceramic with ceramic-on-conventional polyethylene bearings in total hip arthroplasty. J Arthroplasty. 2010;25:392–397. doi: 10.1016/j.arth.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 28.Ochs U, Ilchmann T, Ochs BG, Marx J, Brunnhuber K, Lüem M, Weise K. EBRA migration patterns of the Plasmacup with ceramic or polyethylene inserts: a randomized study. Z Orthop Unfall. 2007;145(Suppl 1):S20–S24. doi: 10.1055/s-2007-965655. [DOI] [PubMed] [Google Scholar]
- 29.Amanatullah DF, Landa J, Strauss EJ, Garino JP, Kim SH, Di Cesare PE. Comparison of surgical outcomes and implant wear between ceramic-ceramic and ceramic-polyethylene articulations in total hip arthroplasty. J Arthroplasty. 2011;26:72–77. doi: 10.1016/j.arth.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 30.Cai P, Hu Y, Xie J. Large-diameter Delta ceramic-on-ceramic versus common-sized ceramic-on-polyethylene bearings in THA. Orthopedics. 2012;35:e1307–1313. doi: 10.3928/01477447-20120822-14. [DOI] [PubMed] [Google Scholar]
- 31.Kim YH, Park JW, Kulkarni SS, Kim YH. A randomised prospective evaluation of ceramic-onceramic and ceramic-on-highly cross-linked polyethylene bearings in the same patients with primary cementless total hip arthroplasty. Int Orthop. 2013;37:2131–2137. doi: 10.1007/s00264-013-2036-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lombardi AV Jr, Berend KR, Seng BE, Clarke IC, Adams JB. Delta ceramic-on-alumina ceramic articulation in primary THA: prospective, randomized FDA-IDE study and retrieval analysis. Clin Orthop Relat Res. 2010;468:367–374. doi: 10.1007/s11999-009-1143-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Beaupre LA, Manolescu A, Johnston DW. A randomized trial of ceramic-on-ceramic bearing versus ceramic-on-crossfire-polyethylene bearing in total hip arthroplasty: five-year outcomes. J Arthroplasty. 2013;28:485–489. doi: 10.1016/j.arth.2012.07.027. [DOI] [PubMed] [Google Scholar]
- 34.Hamilton WG, McAuley JP, Dennis DA, Murphy JA, Blumenfeld TJ, Politi J. THA with Delta ceramic on ceramic: results of a multicenter investigational device exemption trial. Clin Orthop Relat Res. 2010;468:358–366. doi: 10.1007/s11999-009-1091-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vendittoli PA, Rivière C, Lavigne M, Lavoie P, Alghamdi A, Duval N. Alumina on alumina versus metal on conventional polyethylene: a randomized clinical trial with 9 to 15 years followup. Acta Orthop Belg. 2013;79:181–190. [PubMed] [Google Scholar]
- 36.D’Antonio JA, Capello WN, Naughton M. Ceramic bearings for total hip arthroplasty have high survivorship at 10 years. Clin Orthop Relat Res. 2012;470:373–381. doi: 10.1007/s11999-011-2076-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seyler TM, Bonutti PM, Shen J, Naughton M, Kester M. Use of an alumina-on-alumina bearing system in total hip arthroplasty for osteonecrosis of the hip. J Bone Joint Surg Am. 2006;88(Suppl 3):116–125. doi: 10.2106/JBJS.F.00775. [DOI] [PubMed] [Google Scholar]
- 38.Dahl J, Snorrason F, Nordsletten L, Röhrl SM. More than 50% reduction of wear in polyethylene liners with alumina heads compared to cobalt-chrome heads in hip replacements: a 10-year follow-up with radiostereometry in 43 hips. Acta Orthop. 2013;84:360–364. doi: 10.3109/17453674.2013.810516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim YH. Comparison of polyethylene wear associated with cobalt-chromium and zirconia heads after total hip replacement. A prospective, randomized study. J Bone Joint Surg Am. 2005;87:1769–1776. doi: 10.2106/JBJS.D.02572. [DOI] [PubMed] [Google Scholar]
- 40.Kraay MJ, Thomas RD, Rimnac CM, Fitzgerald SJ, Goldberg VM. Zirconia versus Co-Cr femoral heads in total hip arthroplasty: early assessment of wear. Clin Orthop Relat Res. 2006;453:86–90. doi: 10.1097/01.blo.0000246544.95316.1f. [DOI] [PubMed] [Google Scholar]
- 41.Nakahara I, Nakamura N, Nishii T, Miki H, Sakai T, Sugano N. Minimum five-year followup wear measurement of longevity highly cross-linked polyethylene cup against cobaltchromium or zirconia heads. J Arthroplasty. 2010;25:1182–1187. doi: 10.1016/j.arth.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 42.Kawate K, Ohmura T, Kawahara I, Tamai K, Ueha T, Takemura K. Differences in highly cross-linked polyethylene wear between zirconia and cobalt-chromium femoral heads in Japanese patients: a prospective, randomized study. J Arthroplasty. 2009;24:1221–1224. doi: 10.1016/j.arth.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 43.Engh CA, MacDonald SJ, Sritulanondha S, Korczak A, Naudie D, Engh C. Metal ion levels after metal-on-metal total hip arthroplasty: a five-year, prospective randomized trial. J Bone Joint Surg Am. 2014;96:448–455. doi: 10.2106/JBJS.M.00164. [DOI] [PubMed] [Google Scholar]
- 44.Jacobs M, Gorab R, Mattingly D, Trick L, Southworth C. Three- to six-year results with the Ultima metal-on-metal hip articulation for primary total hip arthroplasty. J Arthroplasty. 2004;19:48–53. doi: 10.1016/j.arth.2004.06.021. [DOI] [PubMed] [Google Scholar]
- 45.Bascarevic Z, Vukasinovic Z, Slavkovic N, Dulic B, Trajkovic G, Bascarevic V, Timotijevic S. Alumina-on-alumina ceramic versus metal-onhighly cross-linked polyethylene bearings in total hip arthroplasty: a comparative study. Int Orthop. 2010;34:1129–1135. doi: 10.1007/s00264-009-0899-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Desmarchelier R, Viste A, Chouteau J, Lerat JL, Fessy MH. Metasul vs Cerasul bearings: a prospective, randomized study at 9 years. J Arthroplasty. 2013;28:296–302. doi: 10.1016/j.arth.2012.05.028. [DOI] [PubMed] [Google Scholar]
- 47.Pabinger C, Biedermann R, Stöckl B, Fischer M, Krismer M. Migration of metal-on-metal versus ceramic-on-polyethylene hip prostheses. Clin Orthop Relat Res. 2003;412:103–110. doi: 10.1097/01.blo.0000068766.86536.d3. [DOI] [PubMed] [Google Scholar]
- 48.Woods BS, Hawkins N, Scott DA. Network meta-analysis on the log-hazard scale, combining count and hazard ratio statistics accounting for multi-arm trials: a tutorial. BMC Med Res Methodol. 2010;10:54. doi: 10.1186/1471-2288-10-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and metaanalyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 50.Furlan AD, Pennick V, Bombardier C, van Tulder M Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976) 2009;34:1929–1941. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 51.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 52.Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment metaanalysis: an overview and tutorial. J Clin Epidemiol. 2011;64:163–171. doi: 10.1016/j.jclinepi.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 53.Zagra L, Maccario C, Mondini A, Bianchi L. Treatment of failures related to articulation material in THA. A comprehensive algorithm of surgical options and open questions. Hip Int. 2014;24(Suppl 10):S48–57. doi: 10.5301/hipint.5000170. [DOI] [PubMed] [Google Scholar]
- 54.Hu D, Tie K, Yang X, Tan Y, Alaidaros M, Chen L. Comparison of ceramic-on-ceramic to metal-on-polyethylene bearing surfaces in total hip arthroplasty: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2015;10:22. doi: 10.1186/s13018-015-0163-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Paxton E, Cafri G, Havelin L, Stea S, Pallisó F, Graves S, Hoeffel D, Sedrakyan A. Risk of revision following total hip arthroplasty: metal-onconventional polyethylene compared with metal-on-highly cross-linked polyethylene bearing surfaces: international results from six registries. J Bone Joint Surg Am. 2014;96(Suppl 1):19–24. doi: 10.2106/JBJS.N.00460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Si HB, Zeng Y, Cao F, Pei FX, Shen B. Is a ceramic-on-ceramic bearing really superior to ceramic-on-polyethylene for primary total hip arthroplasty? A systematic review and metaanalysis of randomised controlled trials. Hip Int. 2015;25:191–198. doi: 10.5301/hipint.5000223. [DOI] [PubMed] [Google Scholar]
- 57.Voleti PB, Baldwin KD, Lee GC. Metal-on-metal vs conventional total hip arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Arthroplasty. 2012;27:1844–1849. doi: 10.1016/j.arth.2012.05.023. [DOI] [PubMed] [Google Scholar]
- 58.Furnes O, Paxton E, Cafri G, Graves S, Bordini B, Comfort T, Rivas MC, Banerjee S, Sedrakyan A. Distributed analysis of hip implants using six national and regional registries: comparing metal-on-metal with metal-on-highly crosslinked polyethylene bearings in cementless total hip arthroplasty in young patients. J Bone Joint Surg Am. 2014;96(Suppl 1):25–33. doi: 10.2106/JBJS.N.00459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Song F, Harvey I, Lilford R. Adjusted indirect comparison may be less biased than direct comparison for evaluating new pharmaceutical interventions. J Clin Epidemiol. 2008;61:455–463. doi: 10.1016/j.jclinepi.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 60.Cohen D. How safe are metal-on-metal hip implants? BMJ. 2012;344:e1410. doi: 10.1136/bmj.e1410. [DOI] [PubMed] [Google Scholar]
- 61.Nich C, Hamadouche M. Cup loosening after cemented Metasul® total hip replacement: a retrieval analysis. Int Orthop. 2011;35:965–970. doi: 10.1007/s00264-010-1061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Graves SE, Rothwell A, Tucker K, Jacobs JJ, Sedrakyan A. A multinational assessment of metal-on-metal bearings in hip replacement. J Bone Joint Surg Am. 2011;93(Suppl 3):43–47. doi: 10.2106/JBJS.K.01220. [DOI] [PubMed] [Google Scholar]
- 63.Keurentjes JC, Kuipers RM, Wever DJ, Schreurs BW. High incidence of squeaking in THAs with alumina ceramic-on-ceramic bearings. Clin Orthop Relat Res. 2008;466:1438–1443. doi: 10.1007/s11999-008-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Viste A, Chouteau J, Desmarchelier R, Fessy MH. Fractures of a sandwich ceramic liner at ten year follow-up. Int Orthop. 2012;36:955–960. doi: 10.1007/s00264-011-1375-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cooper HJ, Urban RM, Wixson RL, Meneghini RM, Jacobs JJ. Adverse local tissue reaction arising from corrosion at the femoral neckbody junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg Am. 2013;95:865–872. doi: 10.2106/JBJS.L.01042. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


