Abstract
The symptomatic characteristics and psychosocial factors of belching were analyzed through questionnaire, and the pathophysiology of belch was studied with the combined methods of high-resolution manometry and impedance (HRM-IMP). 21 consecutively-enrolled patients with repeated belching, were conducted a questionnaire survey, and the data were analyzed with Pearson correlation analysis and exact propability method. 10 patients were performed HRM-IMP. 20 patients met the diagnostic criteria of belch, among who 17 cases had overlapped symptoms, and the functional dyspepsia was the most common, followed by gastroesophageal reflux disease; 16 patients experienced mental stimulation or negative events; 12 cases existed anxiety and (or) depression; 8 cases had neurotic personality. The number of the overlapped symptoms was associated with the anxiety status, while the belch severity had nothing to do with the anxiety/depression status. Among the 10 patients who accepted HRM-IMP, 9 existed the esophageal motility dysfunction, and 9 had supra-gastric belching. Belch had a variety of clinical manifestations, related to the mood changes and the environmental stress, and normally was combined with the abnormalities of psychology and personality traits. The belch patients normally experienced the esophageal motility disorders, among which the typical pattern was supra-gastric belching.
Keywords: Belch, clinical features, high-resolution manometry, impedance, supra-gastric belching
Introduction
Belching disorders is a functional gastroduodenal disease characterized by the excessive belch and disturbance [1]. Accumulation of air in the stomach increases gastric volume, which activates receptors in the gastric wall. A reflex is initiated, leading to relaxation of the lower esophageal sphincter, upward movement of the air through the esophagus, and finally passage through the upper esophageal sphincter, during which an audible belch can sometimes be heard. So, belching is physiological venting of excessive gastric air. Excessive and bothersome belching is a common symptom, which is often seen in patients with functional dyspepsia and gastroesophageal reflux disease. Often other symptoms are predominant, and these should be treated first. Sometimes patients present with excessive belching as an isolated symptom. These patients belch in very high frequencies, up to 20 times per minute, and often during consultation. Although belching are regarded as normal behaviors, they can occur at high frequency, or become persistent, becoming bothersome, even interfering with social functioning and affecting quality of life, and requiring medical care. Clinical data of belch is very lack, therefore the meticulous and deep research would be very necessary [2-5]. Through the questionnaire survey towards the belch patients enrolled in the clinic service of the Department of Gastroenterology, Peking Union Medical College Hospital, from Sep. 2010 to Feb. 2011, this study aimed to understand the demographic characteristics, symptom spectrum, the factors that would induce and affect the symptoms and the patient’s psychosocial factors and current mental status. Recently, high-resolution manometry (HRM) capable of pressure monitoring from the pharynx to the stomach together with pressure topography plotting was used for clinical diagnosis of functional esophageal disorders and clinical researches. In this study, HRM combined with impedance (HRM-IMP) was performed for the preliminary pathophysiological study of belching disorders.
Subjects and methods
Subjects
The belch patients consecutively enrolled in the clinic service of the Department of Gastroenterology, Peking Union Medical College Hospital, from Sep. 2010 to Feb. 2011, who met the diagnostic criteria of Rome III belching disorders: the onset of the symptoms was 6 months before the diagnosis, and the symptoms in the near 3 months met the following criteria: 1) uncomfortable repeated belch appeared several times a week; 2) could objectively observe or detect the evidence of belch symptoms caused by gas swallowing and (or) no excessive gas swallowing; 3) Exclusion of other diseases with belching; 4) no organic disease significantly causing repeated belch. This study was conducted with approval from the Ethics Committee of Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College. Written informed consent was obtained from all participants.
Clinical research method
A survey questionnaire was adopted, including general demographic characteristics, belching-related digestive symptom spectrum (nausea, acid reflux, regurgitation, postprandial fullness, early satiety, abdominal burning sensation, upper abdominal pain, vomiting, abdominal pain, bloating, constipation, diarrhea, reduced food intake, appetite loss, weight loss, etc.), duration of disease, inducing factors, previous medical conditions, psychosocial situation, and psychological status. Psychological assessment scale: the Zung Self-Rating Scale of depression or anxiety (SAS/SDS) [6,7] and the Eysenck Personality questionnaire (EPQ) [8] were adopted for the assessment of the mental psychological state of belch patients. Patients completed questionnaires based on the actual situation, and the doctor would make the necessary explanations. The score of SAS/SDS ≤50 was considered as normal, 51~59 as mild depression or anxiety, 60~69 as moderate depression or anxiety, ≥70 as severe depression or anxiety. EPQ includes 4 parts, namely P (psychoticism), E (extraversion), N (neuroticism) and L (lie). The standard scores (i.e., T score) <38.5 points indicates low score, 38.5~61.5 is the intermediate values, >61.5 is high scores. The high P score illustrates that the subject has pathological personality; high E score indicates extroversion, while low E score means introversion; high N score means emotional lability, while low N score means emotional stability; high L score indicates disguised or false answer, which also is the unstable performance.
HRM-IMP test
22-channel water perfusion HRM-IMP system (Solar GI acquisition system) was provided by Medical Measurement Systems Company (Netherlands). The side hole of P1 channel lied in the bottom of the catheter, recording the proximal stomach pressure. 5 cm above the P1 channel was the P2 channel. From the P2 channel, each channel was distributed 1 cm with the other until the P7 channel. And started from the P7 channel, each channel was distributed 2 cm with the other until the P22 channel. The total length of the 22 channels distributed was 40 cm, and could display the pressure situation of the upper esophageal sphincter (UES), esophageal body, lower esophageal sphincter (LES) and intragastric. P2 to P7 channels were used to accurately reflect the dynamic changes of LES pressure. A transitional zone of the upper esophagus displayed as weak pressure area in HRM, and the section between the transitional zone and UES was the proximal section of the esophagus, while the smooth muscles were below the transitional zone [9]. 8 IMP loops formed 7 IMP path regions, with 2 cm interval between each IMP loop. E1~E8 were evenly distributed between P8 and P16, among which the E1 was 1 cm above the P8, and could simultaneously detect the direction of gas moving and the possible pathogenesis [10]. The patients were fasted for at least 8 h before receiving the inspection. During the test, they were in sitting position, the catheter was inserted through the nose after the calibration, and adjusted the appropriate depth of the catheter for the fixation. After 10-min adaptation, the patients were required to stop swallowing for 30 s, recording the basic pressure level of each esophageal segment. After that, the patients were asked to swallow 5 ml warm salt water every other 30 s, with a total of 10 times, and do belch action 5 times.
Statistical analysis
SPSS17.0 statistical analysis software was used for the statistical analysis. The data were of normal distribution. The measurement data were expressed as x̅ ± s, the relationships between variables was expressed with Pearson correlation analysis. The count data were expressed with frequency (%), and the test method was the exact propability method, with P<0.05 as the statistically significant difference.
Results
Demographic characteristics
A total of 21 patients with recurrent belch were studied, and 20 of them met the diagnostic criteria of belch, including 5 males and 15 females, with the mean age (49 ± 10) years old, among them 12 cases lived in Beijing, and 8 cases lived outside Beijing. 13 cases and 7 cases performed mild to moderate intensity of labor work, respectively, and no one performed severe labor intensity; as for the working status, 6 were employed and 14 were unemployed, no students, sick and off-employed; 4 patients were of primary education level or below, 11 were of secondary school level, and 5 were of university level; in the point of economic conditions, 7 felt comfortable, 12 felt normal, while 1 felt nervous; as for the life satisfaction, 3 felt very satisfied, 16 felt basically satisfied, and 1 felt not satisfied.
Symptom characteristics
1) Duration: 0.5~40.0 years, the mean duration was 9.9 years, with the median duration as 5 years. 2) Episode features of belch: 18 patients (90.0%) occurred per day. The belch of the most patients (16 cases, 80.0%) was related with meals, 10 cases (50.0%) were obvious postprandially, more lasting within 1 h, and could be controlled; 4 cases (20.0%) occurred belch longer than 3 h, and hard to control. 3) Inducing method of belch: 15 cases (75.0%) needed no self-induced, while 5 cases (25.0%) needed to be stimulated, including 2 cases of hand-compression on chest, 1 case of hand-compression on the upper-abdomen, 1 case of beating or hardly pressing the sternum or pinching leg, and 1 case of pinching the neck or expanding chest or running and jumping. These 5 patients felt “gas block” and “chest suppression” in the lower sternum, and inflating discomfort on the upper-abdomen and rib sections before belch, while mitigated after belch. 4) Belch characteristic: 2 cases could be smelled the food taste, 1 case contained the sour smell, and the remaining 17 cases (85.0%) were tasteless. 5) Severity: 3 cases were mild (15.0%), and did not affect the work and life, 10 cases were moderate (50.0%), already affected the working life; 7 cases were severe (35.0%), which had seriously affected the work and life.
Overlapped disease
Among the 20 cases, 17 patients (85.0%) had the overlapped symptoms, including 11 patients (55.0%) of overlapped gastroesophageal reflux disease (GERD), 13 cases (65.0%) of overlapped functional dyspepsia (FD), 6 cases (30.0%) of overlapped chronic constipation (CC), 9 cases (45.0%) of mixed overlapped symptoms (4 cases of GERD and FD, 2 cases of FD and CC, and 3 cases of GERD, FD and CC); 3 cases (15.0%) had no overlapped symptoms.
Inductive, aggravating and (or) mitigating factors of belch
The open-loop questionnaire was designed to recall the patients with the possible inductive, aggravating and (or) mitigating factors of belch. 1) inductive and (or) aggravating factors: 9, 13, 3, 8 and 12 cases were related with food, violent emotion changes such as anger or excitement, overwork, study or work pressure and stress, respectively; there were 8 and 10 cases, respectively, who occurred aggravating belch symptoms with GERD symptoms (acid reflux, heartburn and others) and FD symptoms (postprandial fullness, epigastric burning sensation and others); 1 and 2 cases exhibited other inductive factors (smoking cessation) and without obvious inductive and (or) aggravating factors, respectively. 2) Mitigating factors: 9, 5, 7, 4, 3, 3 and 2 cases were of diet, emotional self-regulation, relax or rest, mitigated GERD or FD symptoms, sports participation, attention diversion and sleep, respectively.
Treatment conditions
1) Visiting counts and medical expenses: 14 cases visited ≥3 hospitals and the counts of 11 cases’ hospital-visiting were no less than 5 times, and the visiting times of 3 cases were too frequent to remember clearly. The average spent on diagnosis and treatment was more than 17,000 yuan, with the most was more than 100,000 yuan. 2) Overall efficacy of self-rating: 14 patients consciously felt “almost no effective”; most patients expressed that an effective could be obtained in the initial treatment, while the symptoms were easily repeated, the treatment effect was then gradually weakened, leading to repeated treatment in multi-hospitals, and no long-term regular medication.
Survey of psychosocial factors
1) Environmental stress conditions: 16 cases (80.0%) had experienced mental stimulation or negative events, of which 13 cases were related with family tensions (quarrels and conflicts), work pressure, overwork, and 3 patients experienced the decease of family member who suffered from gastrointestinal cancers. Another 1 case experienced criminal sentencing of his intimate kin, and 1 case experienced repeated belch after he quit the smoking. There was no case suffered from the history of abuse. 2) Psychological survey: 18 patients completed the SAS/SDS self-rating scale, among who 12 cases had anxiety or depression or both (6 cases of anxiety states; 12 cases of depression; 6 cases of the 2 states). 3) Personality traits: 17 cases completely finished the EPQ, and 8 had obvious neurotic personality traits, including 2 males and 6 females.
Relationship analysis of symptoms and psychosocial factors
The Pearson Correlation analysis was performed towards the number of overlapped symptoms and psychological, personality scale scores, the results showed that anxiety status was positively correlated with the number of overlapped symptoms (r=0.47, t=2.14, P<0.05). Exact propability analysis showed that anxiety and depression status had no significant correlation with the severity degree of belch (P=0.096).
HRM-IMP test results
10 patients were performed HRM-IMP test, including 4 males, aged 28~50 years, with the mean age as (47.5 ± 9.0) years; 6 females, aged 29~65 years, with the mean age as (49.3 ± 13.0) years. The clinical symptoms of the 10 patients were all frequent belch, and the main associated symptoms (symptom rate ≥50%) were abdominal fullness, abdominal discomfort and chest oppression; the secondary associated symptoms (symptom rate <50%) were upper-abdominal pain, chest pain, acid reflux, heartburn and constipation, some patients occurred weight loss.
Among the 10 patients, 9 cases were of supra-gastric belching, and only 1 case was of stomach belch. The non-specific excessive belch did not exist the phenomena of frequent air swallowing, primary or secondary esophageal peristalsis (Figure 1).
Figure 1.
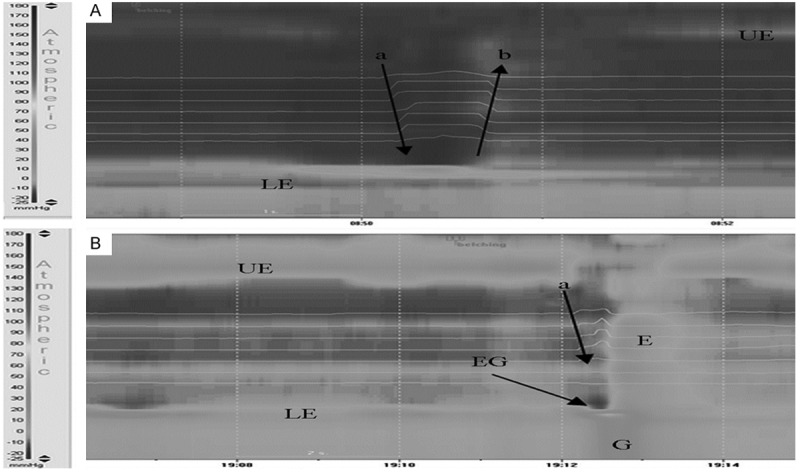
Supragastric belching of non-specific belch patients exhibited in the combined HRM-IMP. A: Air moved rapidly into the esophagus (arrow a) and expelled from oral direction (arrow b) less than 1 second later, without primary or secondary esophageal peristalsis, while associated with the contraction of abdominal muscles and diaphragm; B: Air moved rapidly into the esophagus (arrow a). The abdominal contraction led to the esophageal and gastric internal pressure increased. The diaphragmatic contraction made the EGJ move distally, which decreased the pressure within the esophagus. Notes: UES, upper esophageal sphincter; LES, lower esophageal sphincter; EGJ, gastroesophageal junction; E, esophagus; G, stomach; Arrows indicated the directions of gas movement.
Among the 10 patients, 9 and 8 cases exhibited normal contraction pressure in the distal and proximal esophageal regions. According to the classification criteria of Chicago Ineffective Esophageal Motility [11], 9 patients had obvious esophageal motility disorders, including 2 cases of mild peristaltic dysfunction, 7 cases of severe peristaltic dysfunction, appearing as the performance of non-conductive contraction, interruptive contraction, shedded contraction (Figure 2). Among the 9 patients, 5 cases mainly were non-peristaltic contractions, and 4 cases were non-peristaltic contractions. LES pressure of 3 patients was lower than the normal value [the normal value was 9~27 mmHg [12]. (1 mmHg=0.133 kPa)]. 4 s integrated relaxation pressure (4 s IRP) of LES of 1 patient was >15 mmHg (the normal value was <15 mmHg), prompting LES was relaxed insufficiently. There were 2 kinds of mechanisms of gas entering into the esophagus among the 9 supra-gastric belch. 7 patients were because of inhalation, the chest negative pressure increased when inhaled, UES then relaxed, and air was sucked into the esophagus (Figure 3A). 2 patients were because of force-in, the contraction of the pharyngeal muscles forced the gas into the esophagus (Figure 3B). All the patients discharged the gas from mouth through the contraction of abdominal muscles and diaphragm, which increased the gastric pressure and esophageal pressure.
Figure 2.
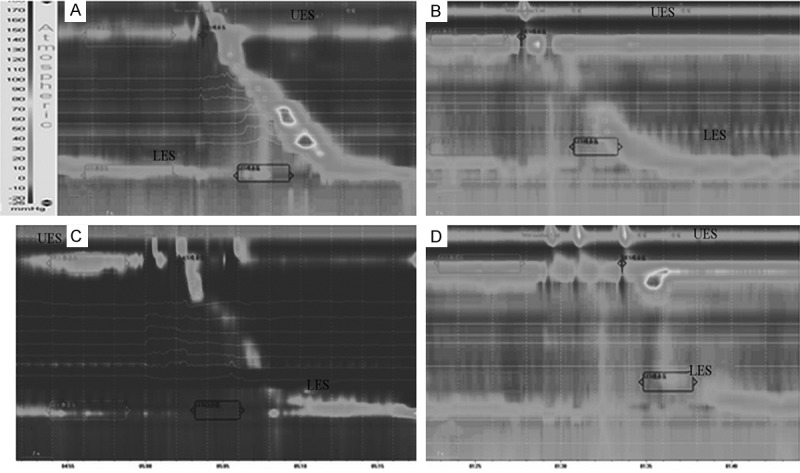
Combined HRM-IMP showed esophageal body motility. A: Normal peristaltic contraction; B: Non- conductive contraction; C: Interruptive contraction; D: Construction loss. Notes: UES, upper esophageal sphincter; LES, lower esophageal sphincter.
Figure 3.
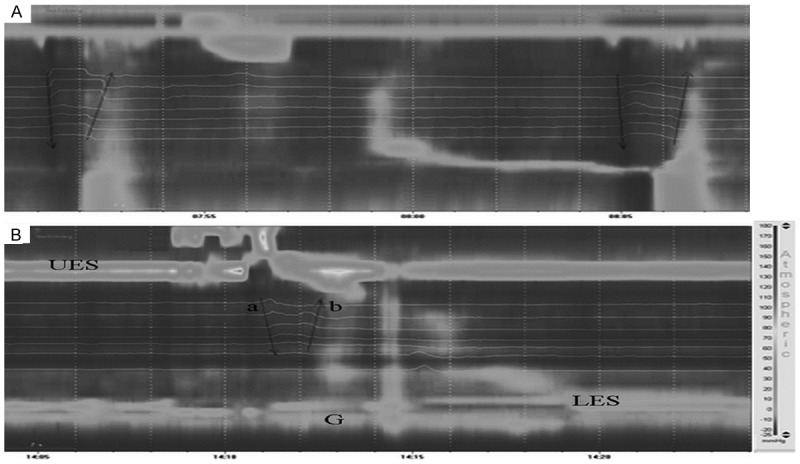
2 kinds of mechanisms of gas entering into the esophagus in supragastric belching. A: inhalation: the intrathoracic negative pressure increased when inhaled, the air entered the esophagus through pharynx (arrow a); then the gas was discharged immediately from the outlet with the increased intra-abdominal pressure (arrow b); B: Force-in: the pharyngeal muscle contracted, UES relaxed, so the gas was forced into the esophagus (arrow a), then exhausted (arrow b). Note: UES, upper esophageal sphincter; LES, lower esophageal sphincter; E, esophagus; G, stomach; Arrows indicated the directions of gas movement.
Discussion
Frequent belch is more related with meal, leading to longer duration, expensive cost, while with poor treatment efficiency, significantly affecting the qualities of work and life, which needs to be paid high attention. The results of this study were similar with Bredenoord and Smout [13]. Belch is a behavioral abnormality. Recent research about the attention on belch frequency found [14] that when the patient was not aware of being monitored, the belch frequency was significantly lower than that when informed of the monitoring; when the attention was distracted, the belch frequency decreased, supporting that belch was a behavioral abnormality. The results of this study also showed that when some patients were concentrating on doing one thing (such as completing the questionnaire), the frequency of belch could significantly reduce, some patients even needed to induce belch, and this phenomenon also supported that belch was a behavioral abnormality, suggesting that cognitive behavioral therapy might be effective towards some belch patients.
Belch patients exhibit significant overlapped symptoms, and belch is a response to the gastrointestinal indisposition. In addition to heartburn and regurgitation outside, GERD patients often have belch. Studies have shown that the gas discharging might cause acid reflux. At the same time, the study also found that the gas reflux would follow the liquid reflux [15]. Another study found that proton pump inhibitor therapy could reduce the gas swallowing of some GERD patients, indicating that the discomfort of heartburn would stimulate the swallowing and eating of GERD patients [16]. Toward the patients with reflux symptoms, belch originated from the increasing of gas swallowing; at the same time, gas reflux could also cause reflux symptoms. Because the gas reflux will also expand the esophageal body, and this expansion would lead to the heartburn and chest pain [17]. It was also found indeed that in some GERD patients, the heartburn would only appear when the gas reflux occurred [18].
Studies reported that the incidence of belch in FD patients was up to 80%, and gas swallowing was higher than the healthy people [18]. Although the cause of frequent gas swallowing in these patients is not known, it seems similar to the belch mechanism in GERD patients, namely excessive gas swallowing is a reaction to gastrointestinal discomfort. In this study, more than half of patients presented overlapped belch symptoms, and 65.0% belch patients overlapped FD, 55.0% belch patients overlapped GERD; 50.0% patients with such FD symptoms as postprandial fullness and epigastric burning sensation and 40.0% patients with such GERD symptoms as acid reflux and heartburn might induce or aggravate belch, and 20.0% patients would alleviate when their GERD symptoms or FD symptoms alleviated.
Psychological and social factors in patients play an important role. The association of the imitation of the parents’ disease symptoms in childhood, important mental stimulation, negative or stressful life events, history of abuse with functional gastrointestinal disorders has been generally accepted by the medical profession. This study found that most self-conscious incidence of the patients had inductive factors, over half patients had experienced mental stimulation/negative events, among which dramatic mood change was the most common cause of belch (65.0%), life stress, overwork accounted for 55.0%, eating accounted for 45.0%. These factors would also increase the belch symptoms, and emotional self-regulation, small amount while multi-meals and rest would help to alleviate the symptoms.
Past studies have shown that the status of anxiety and depression in functional gastrointestinal disease is higher than the normal population, and would impact the disease outcome [17]. In this study, about 2/3 patients exhibited anxiety and (or) depression disorders, and the number of overlapped symptoms were associated with anxiety, while anxiety and depression status had no significant effect on the severity of belch. Psychological characteristic, namely personality survey, showed that the N scores of nearly half of the patients were above the normal range, suggesting that these patients were of emotional instability, and there would be a strong response to the emotional stimulus.
Environmental stress and associated emotional changes would directly affect the gastrointestinal function and symptoms perception of functional gastrointestinal patients [19]; abnormal mental status might be associated with visceral hypersensitivity and often accompanied by the autonomic dysfunction, and thus would mediate the changes of gastrointestinal motility and sensation; the history of abuse and negative events might further aggravate the psychological stress and mental disorders. This survey also found that mood changes were the most frequent inductive factors changing the incidence of belch, negative events, anxiety-depression status and neurotic personality traits were more common in patients. These all tipped the psychosocial factors might play an important role in the occurrence and development of belch. In the treatment process, attention should be paid to the patient’s mental status, and treatment should be performed to patients’ psychological abnormality in time.
HRM-IMP combined detection is a good research tool towards the pathophysiological mechanism of belch [20-24]. Test results showed the abnormalities of esophageal body motility presented in belch. Although most patients had normal esophageal contraction pressure, almost all patients had esophageal peristalsis dysfunction, non-peristaltic contraction was the obvious esophageal motility abnormality. The LES of belch patients had normal functions. Clinical researches considered that belch might be a behavioral abnormality, and HRM-IMP test results showed the presence of esophageal body motility disorders in belch patients, suggesting that there might be the interaction between the abnormal belch motility and abnormal behavior, namely there might be brain-gut interactions, and involved in the pathogenesis. Clinical studies suggested that psychosocial factors might play an important role in the occurrence and development of belch, and the dynamic HRM-IMP test might be able to evaluate the possible roles of psychosocial factors in the pathogenesis of belch. The mechanism of esophageal body motility dysfunction is not clear, whether it is the high-risk factor of belch is not clear, which needed further study and observation. HRM-IMP detection showed the frequent air swallowing did not exist in non-specific excessive belch, and also no primary or secondary esophageal peristaltic waves, the typical pattern of belch was supra-gastric belching, namely the gas quickly entered the esophagus and quickly reversed back before it has reached the stomach.
Aerophagia and excessive belch are two different diseases. The study also showed that there were 2 kinds of mechanisms that gas entering into the esophagus in belching, 1 was inhalation (the chest negative pressure increased when inhaled, UES then relaxed, and air was sucked into the esophagus), and the other was force-in (the contraction of the pharyngeal muscles forced the gas into the esophagus). This might be able to explain the symptoms difference in supra-gastric belching and stomach belching.
Although the sample size of this study was small, the preliminary conclusion could be obtained that belch was more common in middle-aged women, with a variety of clinical manifestations, including overlapped symptoms, which often was associated with eating. The occurrence of belch is mainly associated with the emotional changes and the environmental stress, and normally combined with abnormal psychological and personality traits, belch might be an abnormal behavior response towards gastrointestinal discomforts. Psychosocial factors might have an important role in the pathogenesis of belch, and the specific roles, ties with the symptoms and prognosis, prediction towards the therapy response of psychosocial factors in the pathogenesis of belch would be our future research objectives. HRM-IMP was performed for the preliminary study of the pathophysiology in belch, the dynamic HRM-IMP detection, portable IMP detection might be more conducive towards the study of the possible roles of pathophysiology and psychosocial factors in the pathogenesis of belch, which would also be the directions of our future research.
Acknowledgements
This study was supported by National “11th 5-Year” Key Technology R&D Program (2007BAI04B01), Shanghai Municipal Health Bureau Project (20114309).
Disclosure of conflict of interest
None.
References
- 1.Tack J, Talley NJ, Camilleri M, Holtmann G, Hu P, Malagelada JR, Stanghellini V. Functional gastroduodenal disorders. Gastroenterology. 2006;130:1466–1479. doi: 10.1053/j.gastro.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 2.Bredenoord AJ, Weusten BL, Timmer R, Akkermans LM, Smout AJ. Relationships between air swallowing, intragastric air, belching and gastro-oesophageal reflux. Neurogastroenterol Motil. 2005;17:341–347. doi: 10.1111/j.1365-2982.2004.00626.x. [DOI] [PubMed] [Google Scholar]
- 3.Bredenoord AJ. Management of Belching, Hiccups, and Aerophagia. Clin Gastroenterol Hepatol. 2013;11:6–12. doi: 10.1016/j.cgh.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Scheid R, Teich N, Schroeter ML. Aerophagia and belching after herpes simplex encephalitis. Cogn Behav Neurol. 2008;21:52–54. doi: 10.1097/WNN.0b013e318165a9b9. [DOI] [PubMed] [Google Scholar]
- 5.Hemmink GJ, Ten Cate L, Bredenoord AJ, Timmer R, Weusten BL, Smout AJ. Speech therapy in patients with excessive supragastric belching-a pilot study. Neurogastroenterol Motil. 2010;22:24–28. doi: 10.1111/j.1365-2982.2009.01371.x. [DOI] [PubMed] [Google Scholar]
- 6.Zung WW. A rating instrument for anxiety disorder. Psychosomatics. 1971;12:371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 7.Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12:63–70. doi: 10.1001/archpsyc.1965.01720310065008. [DOI] [PubMed] [Google Scholar]
- 8.Eysenck HJ, Eysenck SG. The Manual of the Eysenck Personality Questionnaire. London: Hodder and Stoughton; 1975. [Google Scholar]
- 9.Fox MR, Bredenoord AJ. Oesophageal highresolution manomtry: moving from research into clinical practice. Gut. 2008;57:405–423. doi: 10.1136/gut.2007.127993. [DOI] [PubMed] [Google Scholar]
- 10.Ravi K, Francis DL. New technologies to evaluate esophageal function. Expert Rev Med Devices. 2007;4:829–837. doi: 10.1586/17434440.4.6.829. [DOI] [PubMed] [Google Scholar]
- 11.Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJ, Stanghellini V International High Resolution Manometry Working Group. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24:57–65. doi: 10.1111/j.1365-2982.2011.01834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang ZF, Sun XH, Song ZQ, Zhao Y, Ke MY, Zhu YL, Wang XQ, Luo JY, Xie XP, Hou XH, Zou DW. Normative values of the esophageal manometry and its influential factors in the healthy subjects: a multiple center study in China. Chinese Journal of Digestion. 2012;32:14–18. [Google Scholar]
- 13.Bredenoord AJ, Smout AJ. Impaired healthrelated quality of life in patients with excessive supragastric belching. Eur J Gastroenterol Hepatol. 2010;22:1420–1423. doi: 10.1097/MEG.0b013e328340887c. [DOI] [PubMed] [Google Scholar]
- 14.Bredenoord AJ, Weusten BL, Timmer R, Smout AJ. Psychological factors affect the frequency of belching in patients with aerophagia. Am J Gastroenterol. 2006;101:2777–2781. doi: 10.1111/j.1572-0241.2006.00917.x. [DOI] [PubMed] [Google Scholar]
- 15.Sifrim D, Silny J, Holloway RH, Janssens JJ. Patterns of gas and liquid reflux during transient lower oesophageal sphincter relaxation: a study using intraluminal electrical impedance. Gut. 1999;44:47–54. doi: 10.1136/gut.44.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hemmink GJ, Weusten BL, Bredenoord AJ, Timmer R, Smout AJ. Increased swallowing frequency in GORD is likely to be caused by perception of reflux episodes. Neurogastroenterol Motil. 2009;21:143–148. doi: 10.1111/j.1365-2982.2008.01197.x. [DOI] [PubMed] [Google Scholar]
- 17.Kahrilas PJ, Dodds WJ, Hogan WJ. Dysfunction of the belch reflex. A cause of incapacitating chest pain. Gastroenterology. 1987;93:818–822. doi: 10.1016/0016-5085(87)90445-8. [DOI] [PubMed] [Google Scholar]
- 18.Conchillo JM, Selimah M, Bredenoord AJ, Samsom M, Smout AJ. Air swallowing, belching, acid and non-acid reflux in patients with functional dyspepsia. Aliment Pharmacol Ther. 2007;25:965–971. doi: 10.1111/j.1365-2036.2007.03279.x. [DOI] [PubMed] [Google Scholar]
- 19.Levy RL, Olden KW, Naliboff BD, Bradley LA, Francisconi C, Drossman DA, Creed F. Psychosocial aspects of the functional gastrointestinaldisorders. Gastroenterology. 2006;130:1447–1458. doi: 10.1053/j.gastro.2005.11.057. [DOI] [PubMed] [Google Scholar]
- 20.Bredenoord AJ, Tutuian R, Smout AJ, Castell DO. Technology review: Esophageal impedance monitoring. Am J Gastroenterol. 2007;102:187–194. doi: 10.1111/j.1572-0241.2006.00966.x. [DOI] [PubMed] [Google Scholar]
- 21.Bredenoord AJ, Weusten BL, Sifrim D, Timmer R, Smout AJ. Aerophagia, gastric, and supragastric belching: a study using intraluminal electrical impedance monitoring. Gut. 2004;53:1561–1565. doi: 10.1136/gut.2004.042945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karamanolis G, Triantafyllou K, Tsiamoulos Z, Polymeros D, Kalli T, Misailidis N, Liakakos T, Ladas SD. Effect of sleep on excessive belching: a 24-hour impedance-pH study. J Clin Gastroenterol. 2010;44:332–334. doi: 10.1097/MCG.0b013e3181bd885e. [DOI] [PubMed] [Google Scholar]
- 23.Rommel N, Tack J, Arts J, Caenepeel P, Bisschops R, Sifrim D. Rumination or belchingregurgitation? Differential diagnosis using oesophageal impedance-manometry. Neurogastroenterol Motil. 2010;22:e97–104. doi: 10.1111/j.1365-2982.2009.01431.x. [DOI] [PubMed] [Google Scholar]
- 24.Kessing BF, Bredenoord AJ, Smout AJ. Gastric belching and supragastric belching are two distinct pathophysiological entities: a study using combined high-resolution manometry and impedance monitoring. Gastroenterology. 2012;142:282. [Google Scholar]


