Abstract
Background: Hypocalcemia is a common complication following thyroidectomy. To explore reasonable and simple methods for predicting postoperative hypocalcemia and identify the optimal strategies for selective calcium supplement are meaningful for surgeon. Methods: Based on the NCCN risk stratification system, patients were divided into 4 groups (A-D): low-risk group A, who only underwent limited thyroidectomy (LT) and high-risk groups B, C and D, who had received total thyroidectomy (TT) and selective central and/or lateral neck dissection (SND). After surgery, group C patients were orally given calcium gluconate and group D patients were intravenously given calcium 2 g/day for 7 days, while group B patients did not receive any calcium supplement. Serum calcium and parathyroid hormone (PTH) levels were collected before and after surgery. The incidence of asymptomatic and symptomatic hypocalcemia in each group was recorded. Results: A total of 132 patients with differentiated thyroid carcinoma (DTC) were included who received surgical treatment. No a significant change was observed in serum calcium and PTH levels in group A, while significant decreases in serum calcium and PTH levels were seen in group B (P < 0.05). Intravenous calcium supplement in group D resulted in a more rapid recovery in serum calcium levels (P < 0.05). The incidences of symptomatic hypocalcemia and asymptomatic hypocalcemia were significantly lower in group A and group D respectively compared to the other groups (All P values < 0.05). In group B, a highest asymptomatic and symptomatic hypocalcemia incidence was detected. Conclusion: Selective calcium supplementation for DTC based on NCCN risk stratification system could be recommended for the high-risk patients.
Keywords: Differentiated thyroid carcinoma, complication, hypocalcemia, calcium supplement
Introduction
Thyroid cancer, especially differentiated thyroid carcinoma (DTC), is the most common malignancy in head and neck region. The incidence has increased markedly over the past several decades worldwide regardless of age and sex. Hypocalcemia is one of the most frequent complications of thyroidectomy with a reported incidence ranging from 5 to 60% [1]. Previous researches have reported that hypocalcemia is generally temporary in the first week after surgery [2]. Common causes include devascularization, damage and erroneous excision of the parathyroid glands during the operation due to the close proximity or direct involvement of the malignant tumor [3]. Hypocalcemia can be asymptomatic or symptomatic perioral or distal acral paresthesia, severe cramps, tetany, and convulsion. Although serum calcium levels in most patients spontaneously are recovered within a few months, it inevitably leads to delayed hospital discharge and potential readmission. Hypocalcemia in a few cases persists after one year and is thus considered as permanent. In order to avoid hypocalcemia, current regimens include routine and selective calcium supplementation via oral or intravenous administration. Routine administration of supplemental calcium can lead to adverse effects such as constipation, nausea, and inhibition of PTH production by a negative feedback mechanism [6]. In addition, frequent biochemical monitoring after hospital discharge can be burdensome. Researchers propose a selective, rather than routine, calcium replacement therapy [7,8]. Controversies remain whether a lack of immediate intervention could precipitate the occurrence of hypocalcemia [4,5]. Various factors have been reported to influence the risk of hypocalcemia. Early postoperative calcium level < 8 mg/dL [8,9], intraoperative PTH level < 10 pg/mL [10] or preoperative 25-hydroxyvitamin D (25-OHD) level (< 14 ng/mL) [11] may increase the risk of hypocalcemia. Thus, some researchers recommended a selective calcium supplementation according to the mentioned above independent risk factors. Nevertheless, these risk factors are still largely debatable. Others claim that there is no a significant association between these factors and hypocalcemia and they have yet adopted selective calcium supplement as a standard practice. Moreover, the variations in assays, time of measurements and cut off values further make comparisons more difficult between studies.
To our knowledge, the incidence of hypocalcemia mainly depends on the extent of surgery, which is performed upon the risk stratification systems. In addition, the methods and doses of calcium supplementation need to be taken into account. This prospective study was conducted to compare the serum calcium and TSH levels between DTC patients who received different calcium supplement strategies according to the surgery extent and the NCCN risk stratification system.
Methods
Study patients
A total of 132 DTC patients, who were pathologically confirmed and prospectively enrolled, were eligibly included according to the inclusion and exclusion criteria between March 1, 2012, and March 1, 2015 from a single-institution, Sichuan Cancer Hospital. The inclusion criteria included: a) Patients had initial treatment without any surgical produces; b) Patients had stage from T1N0M0 to T3N1M0; c) Patients had postoperation pathological diagnosis, PTC or follicular thyroid carcinoma; d) Patients had normal thyroid function and basal metabolic rate; e) Patients had normal cardiac function, liver function and renal function; and f) At least one parathyroid was identified and preserved intraoperation. The exclusion criteria included: a) Patients had history of previous head and neck related surgery, irradiation or chemotherapy; b) Patients had disease stage from T4N1M0 to T4N1M1; c) Patients did receive preoperative calcium, 25-hydroxyvitamin D or parathyroid hormone supplementation; d) Patients had concomitant parathyroid disease; e) Patients had related other thyroid diseases, such as acute, subacute or chronic thyroiditis; hashimoto’s thyroiditis;etc; f) Patients had hyperthyroidism or hypothyroidism; and g) Patients had hyperparathyroidism or hypoparathyroidism. These patients received the initial surgical treatment and were divided into four groups (group A, n=33; group B, n=30; group C, n=34; and group D, n=35) in accordance with the clinicopathologic factors from risk stratification system of National Comprehensive Cancer Network (NCCN) guidelines [12]. The study protocol was approved by the institutional review board of Sichuan Cancer Hospital. Informed consent was obtained from all the patients.
Intervening measurement
Sequential therapies were performed based on NCCN risk stratification system from group A to D. Patients in the low-risk group A underwent LT such as lobectomy with isthmectomy. They did not receive postoperative calcium supplement. High-risk groups covered B, C and D. Patients in all these groups underwent TT and SND. However, the strategy of postoperative calcium supplement was different. Patients in group B received no calcium supplement. Patients in group C orally received 3 g daily calcium gluconate supplement from the first day after the surgery and lasted for 7 days. Patients in group D had been treated with 2 g per-day intravenous calcium gluconate for 7 days from the first day after the surgery (Figure 1).
Figure 1.
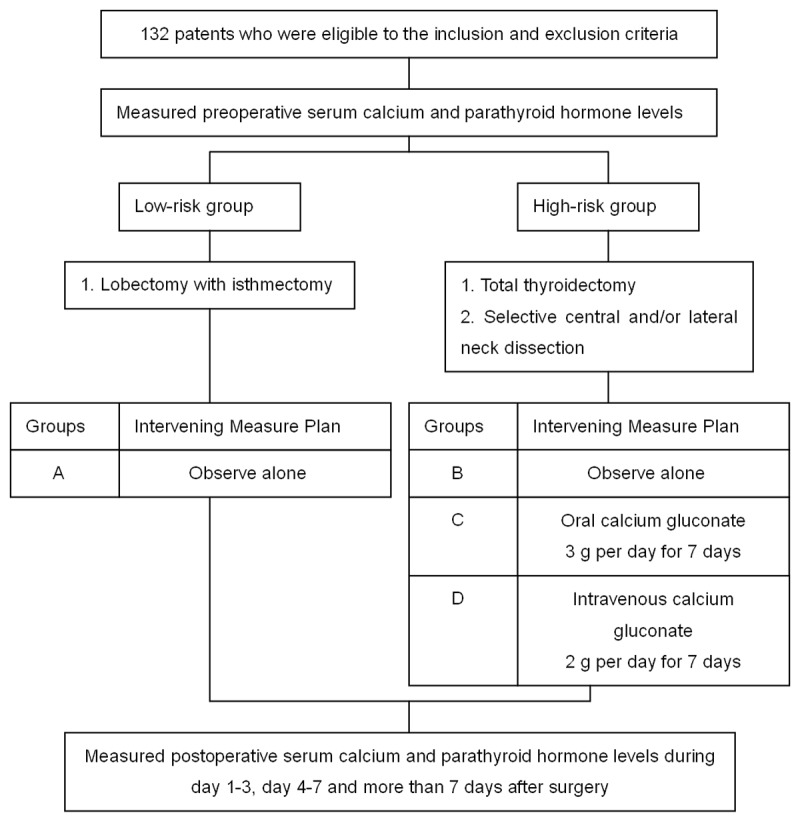
Breakdown of the cohort in this study.
Laboratory measurement
Routine serum calcium (reference normal range: 2.10-2.80 mmol/L) and parathyroid hormone (PTH reference range, 15-65 pg/mL) levels were measured in the hospital laboratory by standard methods with spectrophotometric techniques and paramagnetic particle chemiluminescent enzyme immunoassay. The serum calcium and parathyroid hormone (PTH) levels were collected on the day before surgery and three times after surgery (1-3 days, 4-7 days and over 7 days after surgery). Patients were considered to have postoperative asymptomatic hypocalcemia if at least once the postoperative serum calcium concentration was less than 2.10 mmol/L. Symptomatic hypocalcemia was defined as subjective or objective symptoms such as tingling, numbness or carpopedal spasm with laboratory hypocalcemia. Patients were all trained and educated for reporting the symptoms of hypocalcemia to the clinicians on time.
Statistical analysis
Statistical analysis was conducted using the Statistical Package for the Social Science (SPSS) software version 19.0, with statistical significance defined as P < 0.05. The Student’s t tests were used to compare the mean age between the groups. The chi-square test was applied in the analysis of categorical variables. For continuous variables, repeated measures analysis of variance was used to compare preoperative and postoperative biochemical levels. The results were reported as mean values ± standard deviation (Mean ± SD).
Results
Among 132 patients included in this study, 101 were females and 31 were males. The mean age was 43.3 ± 13.0 years old. A total of 126 (95.5%) patients were diagnosed as PTC and the other 6 patients (4.55%) as follicular thyroid carcinoma. As shown in Table 1, there were significant differences in gender, multifocality, capsular invasion, and affected lobes between the two groups (Group A vs. groups B-D) (All P values < 0.05), while the two groups were not significantly different in age, tumor sizes, and tumor location (All P values > 0.05). Asymptomatic hypocalcemia with transient decrease in serum calcium was recorded in 59 patients, while symptomatic hypocalcemia was observed in 29 patients. The rates of asymptomatic hypocalcemia and symptomatic hypocalcemia were statistically significant between the groups (all P values < 0.05) (Table 2). Serum calcium returned to normal level within a week in all patients. No patients had permanent hypocalcemia.
Table 1.
Patient basic and clinic features in both groups (Group A: low risk and groups B-D: high-risk)
| Variables | Groups | P | |
|---|---|---|---|
|
| |||
| A: low-risk (n, %) | B-D: high-risk (n, %) | ||
| Gender | < 0.05 | ||
| Male | 2 (6.1) | 29 (29.3) | |
| Female | 31 (93.9) | 70 (70.7) | |
| Age, M ± SD, y | 42.5 (9.4) | 43.6 (14.1) | 0.67 |
| Pathology | |||
| Papillary | 32 (97.0) | 94 (94.9) | |
| Follicular | 1 (3.0) | 5 (5.1) | |
| Tumor size, M ± SD, cm | 1.5 (0.8) | 2.0 (1.4) | 0.06 |
| Multifocality | < 0.05 | ||
| Yes | 2 (6.0) | 47 (48.0) | |
| No | 31 (94.0) | 52 (52.0) | |
| Capsular invasion | < 0.05 | ||
| Yes | 0 (0) | 43 (43.4) | |
| No | 33 (100) | 56 (56.6) | |
| Affected lobes | < 0.05 | ||
| Bilateral | 1 (3.0) | 35 (35.4) | |
| Unilateral | 32 (97.0) | 64 (64.6) | |
| Tumor location | 0.07 | ||
| Upper pole | 6 (18.2) | 39 (39.4) | |
| Middle | 15 (45.5) | 31 (31.3) | |
| Lower pole | 12 (36.3) | 29 (29.3) | |
Table 2.
Asymptomatic and symptomatic hypocalcemia incidences in different groups
| Group | Total | Hypocalcemia | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Asymptomatic | P | Symptomatic | P | ||||||||
|
|
|
||||||||||
| Positive | Negative | Positive | Negative | ||||||||
|
|
|
||||||||||
| N | (%) | N | (%) | N | (%) | N | (%) | ||||
| A | 33 | 15 | (45.5) | 18 | (54.5) | P < 0.05 | 2 | (6.1) | 31 | (93.9) | P < 0.05 |
| B | 30 | 22 | (73.3) | 8 | (26.7) | 12 | (40.0) | 18 | (60.0) | ||
| C | 34 | 15 | (44.1) | 19 | (55.9) | 10 | (29.4) | 24 | (70.6) | ||
| D | 35 | 7 | (20.0) | 28 | (80.0) | 5 | (14.3) | 30 | (85.7) | ||
*Categorical variables are presented as n (%). The differences were statistical significant between individual groups (All P < 0.05).
The level of preoperative serum calcium was 2.38±0.12 mmol/L in all patients. There was a significant decrease in serum calcium levels on day 1-3 (2.10±0.18 mmol/L); day 4-7 (2.14±0.20 mmol/L); and 7 days after surgery (2.21±0.19 mmol/L), respectively (all P values < 0.05). The mean values of serum calcium at any time during the first postoperative week for each group are showed in Table 3. Since the data did not meet the spherical symmetry (P < 0.100), Greenhouse Geisser (GG) was used for degrees of freedom (DOF) correction. The differences between the groups were statistically significant (P < 0.05). The mean values of preoperative PTH levels of all patients were 42.43±16.12 pg/mL. After surgery, the mean values of PTH levels were 24.22±15.56 pg/mL (day 1-3), 26.37±13.97 pg/mL (day 4-7), and 30.04±12.08 pg/mL (7 days after surgery), respectively. The preoperative and postoperative PTH levels were significantly different among the four groups (Table 4). Since the PTH levels did not meet the spherical symmetry (P < 0.100), the GG was used for DOF correction, and the differences between the groups were statistically different (P < 0.05).
Table 3.
Comparison of patients’ blood calcium levels among the 4 groups (Mean ± SD)
| Group | Total | Serum calcium concentration (mmol/L) | P | |||
|---|---|---|---|---|---|---|
|
|
||||||
| Before surgery | After surgery | |||||
|
|
||||||
| 1-3 days | 4-7 days | > 7 days | ||||
| A | 33 | 2.37±0.08 | 2.15±0.17 | 2.23±0.15 | 2.29±0.11 | P < 0.05 |
| B | 30 | 2.36±0.10 | 2.02±0.15 | 2.09±0.19 | 2.15±0.25 | |
| C | 34 | 2.38±0.13 | 2.03±0.16 | 2.11±0.20 | 2.16±0.18 | |
| D | 35 | 2.40±0.14 | 2.18±0.16 | 2.15±0.22 | 2.25±0.18 | |
*Continuous variables are presented as mean ± SD. The differences were statistical significant between individual groups (All P < 0.05).
Table 4.
Comparison of patients’ parathyroid hormone levels among the 4 groups (Mean ± SD)
| Group | No | Parathyroid hormone level (pg/mL) | P | |||
|---|---|---|---|---|---|---|
|
|
||||||
| Before surgery | After surgery | |||||
|
|
||||||
| 1-3 days | 4-7 days | > 7 days | ||||
| A | 33 | 45.84±20.40 | 35.53±17.43 | 33.93±14.03 | 36.94±13.37 | P < 0.05 |
| B | 30 | 39.24±14.54 | 23.13±18.95 | 25.03±15.41 | 28.14±13.11 | |
| C | 34 | 36.59±12.43 | 18.57±9.18 | 23.89±9.32 | 28.34±8.49 | |
| D | 35 | 47.61±14.05 | 19.97±9.14 | 22.80±14.28 | 26.84±10.69 | |
*Continuous variables are presented as mean (SD). The differences were statistical significant between individual groups (All P < 0.05).
Discussion
The hypocalcemia-related symptoms are common after surgery in patients with thyroid cancer and have been an issue of great concern for surgeons. Although more studies have been reported for selective calcium supplementation in prevention of postoperative hypocalcemia among patients with DTC, early identification of patients at risk for postoperative hypocalcemia is crucial for optimal treatment.
Clinicopathologic factors affecting the development of hypocalcemia includes age, gender, preoperative diagnosis, nodule size, etc [13,14], while some biochemical factors are considered the most important parameters of impending postoperative hypocalcemia. Daily monitoring of serum calcium has been used during the perioperative period. Due to the lack of predictability of serum calcium levels, some have implied PTH as a predictor for hypocalcemia. A single PTH level < 10 pg/mL on the first day after surgery could indicate the patients could be at risk [15]. It is been reported that delta PTH, which was defined as the values of PTH levels one-hour after surgery minus PTH levels before surgery, has a better sensitivity (87%), and a marginally better specificity (76%) one hour after surgery [16]. Surgical factors may contribute to the decrease in parathyroid function as well, such as the number of parathyroid gland autotrans plantation and preservation [18]. Serum calcium decrease could be further exacerbated by extensive surgical dissection of thyroid and central neck dissection, since they not only bring a higher risk for accidental excision of parathyroid glands but also endanger the arterial and venous vasculature of the parathyroid glands [19]. In spite of the abovementioned risk factors, to date, no powerful or accurate indicators for parathyroid function have been identified.
As many clinical practices about DTC are based on risk stratification system of guidelines, by categorizing patients into high-risk and low-risk groups. High-risk group is the patients who undergo TT and CND, while low-risk group is those with LT. Serum calcium concentration may also be affected by operation strategies. According to the risk stratification system, we divided 132 patients into four groups in this study. Of the 33 patients undergoing LT in group A, we found serum calcium concentrations at 1-3, 4-7, and > 7 days after surgery were not significantly different compared with normal preoperative levels. All patients in the four groups experienced decreases in serum calcium concentration and PTH levels. Serum calcium concentration reached a minimum during 1-3 days after surgery and returned to normal levels after 7 days. When compared with groups A, serum calcium concentrations in group B were significantly lower at each time point. The trend was the same for the PTH monitoring. Higher incidences of postoperative asymptomatic and symptomatic hypocalcemia were also observed in group B. The incidence of asymptomatic hypocalcemia in group B was significantly higher than that in group A. In group B, 12 (40%) patients had transient symptomatic hypocalcemia, while in group A, only 2 patients had transient symptomatic hypocalcemia (6.1%). The comparison between group A and B indicates that the increased risk of hypocalcemia may occur before treatment. Extensive thyroidectomy with SND may be associated with a greater decrease in postoperative serum calcium. This is in consistence with our results in a previous meta-analysis [20,21]. The decrease may be from the vulnerability of parathyroid glands caused by aggressive exploration in the capsule of thyroid and the central neck compartment, resulting in a high probability of unplanned parathyroidectomy or parathyroid gland devascularization. This finding will greatly help surgeons conveniently predict the possibility of postoperative asymptomatic or symptomatic hypocalcemia before surgery and administer patients for treatment timely after operation. The high-risk patients are more likely to have postoperative hypocalcemia and may need calcium supplementation, while the low-risk patients may just need observation.
Another finding from this current study is to identify a safe dose and a convenient route of drug administration for selective calcium supplementation in high risk patients. After comparing the results of the three high-risk groups, we found that the mean value of serum calcium levels of patients in group C, who had taken oral calcium supplement, restored only slightly quickly than that in group B. This is probably due to limited calcium absorption of the oral supplement or insufficient dosage provided in this study. However, compared to the group B, the group C had fewer asymptomatic (44.1% vs 73.3%) and symptomatic (29.4% vs 40.0%) hypocalcemia cases, respectively. This indicates that take of oral calcium supplement can possibly reduce the range of fluctuation of serum calcium concentration, despite the fact that the oral calcium has been known to cause nausea, decreased appetite, and constipation. The group D patients who had taken intravenous calcium supplement had a higher serum calcium levels than the other three groups on 1-3 days after surgery. The percentage of asymptomatic hypocalcemia patients in group D (20.0%) is also lower than that in the group A (45.5%). In addition, the number of patients with obvious symptomatic hypocalcemia is also lower than those in the group B and C. This indicates that treatment of high-risk patients with 2 g/day of intravenous calcium for 7 days after surgery may prevent hypocalcemia effectively.
We also found that the change of PTH is correlated with that of serum calcium change (data not shown). However, the magnitudes of PTH change were greater than serum calcium in all four groups. Interestingly, the PTH levels in high-risk groups B, C and D decreased more significantly than that in low-risk group A. The high-risk patients in groups C and D treated with calcium supplement had lower PTH levels compared to those in group B. It took longer for patients in group C and D to recover their PTH levels and this status was even prominent for patients who underwent intravenous supplement. This is probably because the calcium supplementation or hypercalcemic conditions caused by overshoot of calcium supplement may suppress normal parathyroid hormone secretion and may result in prolonged suppression of PTH by negative feedback inhibition. Thus more attention needs to be paid to the PTH levels during calcium supplement process after surgery. The clinical management should aim to keep serum calcium levels within the low-to-normal range in order to prevent unwanted PTH suppression. The PTH levels of all the patients in this study were within the normal range, which indicated that the dosage and frequency of the calcium supplementation applied in the study were safe and effective.
There are several limitations in this study. First, the incidence of symptomatic or asymptomatic hypocalcemia was based on the record of patients’ self-reported. As a result, under- and/or over-reporting of symptoms are possible and some symptoms might not be related to the serum calcium levels. Second, the severity of symptoms was not recorded. Therefore, it is difficult to correlate severity of symptoms with the need of calcium supplementation. Third, there were still some patients in low-risk group A met the criteria of asymptomatic and symptomatic hypocalcemia. Thus, the optimal management regimen remains unknown and requires further investigation.
In summary, the findings of this prospective study demonstrated that NCCN multifactorial-based risk stratification system plays an important role in the development of postoperative hypocalcemia due to different extent of operation. Selective calcium supplementation for DTC based on NCCN risk stratification system could be recommended for the high-risk patients. Ultimately, we recommend that selective, rather than routine, calcium supplementation may be better and more achievable.
Acknowledgements
The work was supported by grants from the Sichuan Provincial Bureau of Health (No. 080390, No. 100572); Sichuan Provincial Science and Technology Department (No. 2009 JY0093, No. 11ZC0323). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure of conflict of interest
None.
Abbreviations
- NCCN
national comprehensive cancer network
- DTC
differentiated thyroid carcinoma
- LT
limited thyroidectomy
- TT
total thyroidectomy
- PTH
parathyroid hormone
- SND
selective central and/or lateral neck dissection
References
- 1.Page C, Strunski V. Parathyroid risk in total thyroidectomy for bilateral, benign, multinodular goitre: report of 351 surgical cases. J Laryngol Otol. 2007;121:237–241. doi: 10.1017/S0022215106003501. [DOI] [PubMed] [Google Scholar]
- 2.Costanzo M, Marziani A, Condorelli F, Migliore M, Cannizzaro MA. Post-thyroidectomy hypocalcemic syndrome: predictive value of early PTH. Preliminary results. Ann Ital Chir. 2010;81:301–305. [PubMed] [Google Scholar]
- 3.Goodman WG, Frazao JM, Goodkin DA, Turner SA, Liu W, Coburn JW. A calcimimetic agent lowers plasma parathyroid hormone levels in patients with secondary hyperparathyroidism. Kidney Int. 2000;58:436–445. doi: 10.1046/j.1523-1755.2000.00183.x. [DOI] [PubMed] [Google Scholar]
- 4.Landry CS, Grubbs EG, Hernandez M, Hu MI, Hansen MO, Lee JE, Perrier ND. Predictable criteria for selective, rather than routine, calcium supplementation following thyroidectomy. Arch Surg. 2012;147:338–344. doi: 10.1001/archsurg.2011.1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang TS, Cayo AK, Wilson SD, Yen TW. The value of postoperative parathyroid hormone levels in predicting the need for long-term vitamin D supplementation after total thyroidectomy. Ann Surg Oncol. 2011;18:777–781. doi: 10.1245/s10434-010-1377-5. [DOI] [PubMed] [Google Scholar]
- 6.Boquist L, Fahraeus B. Parathyroid morphology in gerbils after thyroidectomyand calcium administration. Acta Pathol Microbiol Scand A. 1975;83:539–549. doi: 10.1111/j.1699-0463.1975.tb00166.x. [DOI] [PubMed] [Google Scholar]
- 7.Suzuki M, Tsunoda A, Kudo T, Okada Rand Toyoda M. Successful management of hypoparathyroidism following total thyroidectomy with vitamin D3 alone. Auris Nasus Larynx. 2014;41:53–55. doi: 10.1016/j.anl.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Landry CS, Grubbs EG, Hernandez M, Hu MI, Hansen MO, Lee JE, Perrier ND. Predictable Criteria for Selective, Rather Than Routine, Calcium Supplementation Following Thyroidectomy. Arch Surg. 2012;147:338–344. doi: 10.1001/archsurg.2011.1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bentrem DJ, Rademaker A, Angelos P. Evaluation of serum calcium levels in predicting hypoparathyroidism after total/neartotal thyroidectomy or parathyroidectomy. Am Surg. 2001;67:249–251. [PubMed] [Google Scholar]
- 10.Quiros RM, Pesce CE, Wilhelm SM, Djuricin G, Prinz RA. Intraoperative parathyroid hormone levels in thyroid surgery are predictive of postoperative hypoparathyroidism and need for vitamin D supplementation. Am J Surg. 2005;189:306–309. doi: 10.1016/j.amjsurg.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 11.Kirkby-Bott J, Markogiannakis H, Skandarajah A, Cowan M, Fleming B, Palazzo F. Preoperative vitamin D deficiency predicts postoperative hypocalcemia after total thyroidectomy. World J Surg. 2011;35:324–330. doi: 10.1007/s00268-010-0872-y. [DOI] [PubMed] [Google Scholar]
- 12.NCCN Clinical Practice Guidelines in Oncology. Thyroid carcinoma [S/OL] Version 1. 2011. http://www.nccn.org/professionals/physician_gls/pdf/thyroid.pdf.
- 13.Lang BH, Yih PC, Ng KK. A prospective evaluation of quick intraoperative parathyroid hormone assay at the time of skin closure in predicting clinically relevant hypocalcemia after thyroidectomy. World J Surg. 2012;36:1300–1306. doi: 10.1007/s00268-012-1561-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcemia. Br J Surg. 2014;101:307–320. doi: 10.1002/bjs.9384. [DOI] [PubMed] [Google Scholar]
- 15.Cayo AK, Yen TW, Misustin SM, Wall K, Wilson SD, Evans DB, Wang TS. Predicting the need for calcium and calcitriol supplementation after total thyroidectomy: results of a prospective, randomized study. Surgery. 2012;152:1059–1067. doi: 10.1016/j.surg.2012.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bove A, Di Renzo RM, Palone G, D’Addetta V, Percario R, Panaccio P, Bongarzoni G. Early biomarkers of hypocalcemia following total thyroidectomy. Int J Surg. 2014;12:S202–4. doi: 10.1016/j.ijsu.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 17.Muscogiuri G, Tirabassi G, Bizzaro G, Orio F, Paschou SA, Vryonidou A, Balercia G, Shoenfeld Y, Colao A. Vitamin D and thyroid disease: to D or not to D? Eur J Clin Nutr. 2015;69:291–296. doi: 10.1038/ejcn.2014.265. [DOI] [PubMed] [Google Scholar]
- 18.Ozogul B, Akcay MN, Akcay G, Bulut OH. Factors affecting hypocalcemia following total thyroidectomy: a prospective study. Eurasian J Med. 2014;46:15–21. doi: 10.5152/eajm.2014.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Merchavy S, Marom T, Forest VI, Hier M, Mlynarek A, McHugh T, Payne R. Comparison of the incidence of postoperative hypocalcemia following total thyroidectomy vs completion thyroidectomy. Otolaryngol Head Neck Surg. 2015;152:53–56. doi: 10.1177/0194599814556250. [DOI] [PubMed] [Google Scholar]
- 20.Sun RH, Li C, Fan JC, Wang W, Li CH, Xu YQ, Li XX. Comparison of recurrence and complication by different thyroidectomy in the treatment of differentiated thyroid carcinoma as initial treatment: a meta-analysis. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2013;48:834–839. [PubMed] [Google Scholar]
- 21.Sun R, Li C, Fan J, Liu J, Chen J, Zhang B. Metaanalysis of the clinical significance of thyroidectomy combined with central neck dissection in DTC at the first treatment. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2014;49:157–163. [PubMed] [Google Scholar]


