Abstract
Background
The improvement in discrimination gained by adding nontraditional cardiovascular risk markers cited in the 2013 American College of Cardiology/American Heart Association cholesterol guidelines to the atherosclerotic cardiovascular disease (ASCVD) risk estimator (pooled cohort equation [PCE]) is untested.
Objectives
We assessed the predictive accuracy and improvement in reclassification gained by the addition of coronary artery calcium (CAC) score, ankle-brachial index (ABI), high-sensitivity C-reactive protein (hsCRP), and family history (FH) of ASCVD to the PCE in participants of the MESA (Multi Ethnic Study of Atherosclerosis).
Methods
The PCE was calibrated (cPCE) and used for this analysis. Cox proportional hazard model, Harrell's C-statistics, and net reclassification improvement analyses were used. ASCVD was defined as myocardial infarction, coronary heart disease death, or fatal or nonfatal stroke.
Results
Of 6,814 MESA participants not on statins at baseline, 5,185 had complete data and were included in this analysis. Mean age was 61years; 53.1% were women, 9.8% diabetic, and 13.6% current smokers. After 10 years of follow-up, 320 (6.2%) ASCVD events occurred. CAC, ABI, and FH were independent predictors of ASCVD events in the multivariable Cox models. CAC modestly improved the Harrell's C-statistic (0.74 vs. 0.76; p = 0.04) while ABI, hsCRP, and FH showed no improvement in Harrell's C-statistic when added to the cPCE.
Conclusions
CAC, ABI, and FH are independent predictors of ASCVD events. CAC modestly improved the discriminative ability of the cPCE best compared with other nontraditional risk markers.
Keywords: ankle brachial index, coronary artery calcium, high-sensitivity C-reactive protein, Pooled Cohort Equation
In the recently published guidelines on assessment of cardiovascular risk and treatment of blood cholesterol to reduce atherosclerotic risk in adults (1,2), the American College of Cardiology (ACC) and American Heart Association (AHA) introduced a new risk prediction tool utilizing Pooled Cohort Equations (PCEs) for primary atherosclerotic cardiovascular disease (ASCVD) (1). The ACC/AHA cholesterol guidelines also recommends the use of additional markers to improve ASCVD risk assessment and medical decision making, especially in individuals in whom a decision to initiate statin is unclear (2). The additional markers mentioned included low-density lipoprotein (LDL) cholesterol, other genetic hyperlipidemias, family history (FH) of premature ASCVD, high-sensitivity C-reactive protein (hsCRP), coronary artery calcium (CAC) score, lifetime ASCVD risk, and ankle-brachial index (ABI).
The ACC/AHA cholesterol guidelines did not cite data or provide evidence concerning what the yield would be when using these additional risk markers as additional tests for primary ASCVD risk assessment. To address this gap, in this report we describe the improvement in discrimination afforded by the addition of CAC, hsCRP, ABI, and FH of premature ASCVD, over and beyond the PCE for 10-year ASCVD events in asymptomatic adult participants in MESA (Multi-Ethnic Study of Atherosclerosis).
Methods
The MESA study design has been previously published (3). Briefly, MESA is a prospective population-based cohort study investigating the prevalence, correlates, and progression of subclinical CVD in persons without known CVD at baseline. The full cohort includes 6,814 women and men age 45 to 84 years recruited from 6 U.S. communities (Baltimore, Maryland; Chicago, Illinois; Forsyth County, North Carolina; Los Angeles County, California; northern Manhattan, New York; and St. Paul, Minnesota). MESA included 38% white, 28% African American, 22% Hispanic, and 12% Chinese adults. Demographics, medical history, and anthropometric and laboratory data for the present study were taken from the first examination (July 2000 to August 2002). The MESA study was approved by the institutional review boards of each study site and written informed consent was obtained from all participants.
For the current analysis, we excluded participants who had missing data related to traditional or additional risk factors or to follow-up, or those who were using statins at baseline. We also restricted our analyses to participants 40 to 75 years of age because they were identified in the guidelines as having the strongest data pointing to benefit from statin therapy for primary prevention.
Conventional Risk Factors
As part of the baseline examination, clinical teams collected information on traditional and additional putative cardiovascular risk factors. Current smoking was defined as having smoked a cigarette in the last 30 days. Medication use was based on medication inventory. Diabetes mellitus (DM) was defined as self-reported history of diabetes, use of diabetes medication, or fasting glucose ≥126 mg/dl. Resting blood pressure was measured 3 times in the seated position, with the average of the second and third readings recorded. Hypertension was defined as a systolic blood pressure (SBP) ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or use of antihypertensive medication. Body mass index (BMI) was calculated as weight (kg) divided by height (m2). Total and high-density lipoprotein (HDL) cholesterol were measured from blood samples obtained after a 12-h fast; LDL cholesterol was estimated by the Friedewald equation (4).
Additional Guideline-Recommended Risk Markers
Determining the presence of genetic hyperlipidemias, as recommended in the guidelines (2), was not assessed in the current analysis because it was not collected in MESA. Also, we did not assess lifetime ASCVD risk because it can only be calculated in adults ages 20 to 59 years and many MESA participants are older than 59. In addition, to create the lifetime risk calculator, only cohorts with more than 15 years of follow-up were included, which is beyond the duration of follow-up in MESA.
Family History of ASCVD
In MESA, we did not specifically define FH of ASCVD as premature (i.e., before the age of 55 years for men and 65 years for women). Instead, such a history was obtained by asking participants whether any member in their immediate family (first-degree relatives: parents, siblings, or children) had experienced fatal or nonfatal myocardial infarction (MI) or stroke. Age of onset of the event was not specified, and so it is not known whether the events were premature.
High-Sensitivity C-Reactive Protein
We measured hsCRP using the BN™ II nephelometer (N High Sensitivity CRP; Dade Behring Inc., Deerfield, Illinois) at the Laboratory for Clinical Biochemistry Research (University of Vermont, Burlington, Vermont). Analytical intra-assay coefficient of variations ranged from 2.3% to 4.4%, and interassay coefficient of variation ranged from 2.1% to 5.7% with a detection level of 0.18 mg/l.
Coronary Artery Calcium Score
Details of the MESA computed tomography (CT) scanning and interpretation methods have been reported by Carr et al. (5). Scanning centers assessed CAC by chest CT with either a cardiac-gated electron-beam CT scanner (Chicago, Los Angeles, and New York field centers) or a multidetector CT system (Baltimore, Forsyth County, and St. Paul field centers). Certified technologists scanned all participants twice over phantoms of known physical calcium concentration. A radiologist or cardiologist read all CT scans at a central reading center (Los Angeles Biomedical Research Institute at Harbor–UCLA, Torrance, California). We used the mean Agatston score for the 2 scans in all analyses (6). Intraobserver and interobserver agreements were excellent (κ = 0.93 and κ = 0.90, respectively).
Ankle-Brachial Index
Details of the MESA ABI measurement protocol have been published by Criqui et al. (7). Briefly, SBP measurements in the bilateral brachial, dorsalis pedis, and posterior tibial arteries were obtained in the supine position using a hand-held Doppler instrument with a 5 mHz probe. To avoid potential bias from subclavian stenosis, the higher of the brachial artery pressures was used as the denominator. For each lower extremity, the ABI numerator used was the highest pressure (dorsalis pedis or posterior tibial) from that leg. Reproducibility of the ABI was evaluated using measurements of 43 participants by 2 technicians. The inter- and intrareader correlation coefficients were 0.845 and 0.937 respectively with an intra- and inter-reader coefficient of variation of 5.14% and 3.27% respectively. Participants with an ABI ≥1.4 were excluded.
Event Ascertainment
A detailed description of the event ascertainment procedures and the adjudication process in MESA has been published (8). In summary, every 9 to 12 months since the baseline examination, MESA participants or, when necessary, their proxies are contacted to inquire about hospital admissions, CVD diagnosis, and death that may have occurred. Hospital and other documentation of possible cardiovascular events and deaths are subsequently obtained. These documentations are sent to at least 2 MESA morbidity and mortality committee members for adjudication using a standard protocol. This committee included cardiologists, physician epidemiologists, and neurologists. All possible events with disagreements after adjudication by at least 2 MESA morbidity and mortality members were discussed and voted on by the committee during their monthly meetings. For the purposes of this study, we defined incident ASCVD as adjudicated MI, coronary heart disease (CHD) death, and fatal and nonfatal stroke as described by the MESA protocol.
Statistical Analysis
Baseline characteristics are presented as mean ± SD for continuous variables and percentages for categorical variables. Analyses were performed to address 2 specific questions:
-
Are the additional risk markers independent predictors of ASCVD events?
Additional markers were treated as continuous variables (with the exception of FH). Normalizing log transformation was used for hsCRP and CAC+1. Cox proportional hazard analysis was used to assess the association between each of the markers (CAC, ABI, hsCRP, and FH) and incident ASCVD in univariable and multivariable models adjusting for age, sex, race/ethnicity, total and HDL cholesterol, DM, cigarette use, BMI, SBP, and anti-hypertensive medication use. These potential confounders were chosen based on their association with incident ASCVD in prior studies and also in our univariate analysis.
-
Do the additional risk markers improve discrimination over and beyond the calibrated PooledCohort Equations (cPCE)?
The PCE is known to overestimate risk in MESA (9). Thus, to avoid overstating the contribution of the additional risk factors in improving the PCE risk estimates, the PCE was recalibrated to the MESA data. Calibration was accomplished by including the PCE in a Cox model predicting ASCVD events (10), thus creating a calibrated PCE (cPCE) that used the baseline survival estimate from the MESA data, reducing the risk overestimation presented in the original PCE/score. These cPCEs were used in all subsequent analyses. Ten-year cPCE was calculated for each participant including individuals with type 2 DM. The cPCE included race-specific risk estimates for blacks and whites only. Risk estimates for Hispanic and Chinese participants were calculated using the cPCE for whites, as suggested in the new guidelines. We assessed discrimination using Harrell's C-statistic for the cPCE with and without each additional risk marker (11,12). Cross-tabulation of the cPCE with and without each additional risk marker was performed to calculate the net reclassification improvement (NRI). Bootstrapping was used to calculate 95% confidence intervals (CI) (13). The NRI for events and nonevents were calculated separately as previously recommended. The NRI analysis was done using the 7.5% ASCVD risk cut-off per the ACC/AHA guidelines (2 categories). Three categories of ASCVD risk (0 to 5, 5 to 7.5, and >7.5%) were also used as a sensitivity analysis. The improvement in Harrell's C-statistics and NRI of the additional risk markers were directly compared. In a subsequent analysis, the Framingham risk score (14) was recalibrated as described for the PCE and the improvement in reclassification afforded by the addition of these additional risk markers (CAC, ABI, hsCRP, and FH) assessed using Harrell C-statistics and NRI analysis with incident CHD as the outcome of interest. The statistical analysis was performed using STATA 12.0 (StataCorp LP, College Station, Texas).
Results
Of the 6,814 MESA participants, 1,629 (23.9%) were either on statins, had an ABI ≥ 1.4, or had incomplete data and were therefore eliminated from this analysis. In terms of baseline characteristics of the remaining 5,185 participants (Table 1), the mean age of the participants included in this analysis was 61.2 years, 53.1% were female, and 38% were white, 12.1% Chinese, 27% blacks, and 22.9% Hispanics. After a mean follow-up of 10 years, 320 (6.2%) ASCVD events occurred; 139 (43.4%) were MIs, 132 (41.3%) were fatal or nonfatal strokes, and 49 (15.3%) were CHD death.
Table 1. Baseline Characteristics.
| Variable | <7.5% cPCE (n = 4,185) | ≥7.5% cPCE (n = 1,000) | Total Cohort (N = 5,185) |
|---|---|---|---|
|
| |||
| Age, yrs | 58.2 ± 8.6 | 73.6 ± 6.6 | 61.2 ± 10.3 |
|
| |||
| Female | 2,380 (56.9) | 371 (37.1) | 2,751 (53.1) |
|
| |||
| Race/Ethnicity | |||
| White | 1,606 (38.4) | 363 (36.3) | 1,969 (38) |
| Chinese | 518 (12.4) | 107 (10.7) | 625 (12.1) |
| Black | 1,117 (26.7) | 285 (28.5) | 1,402 (27.0) |
| Hispanic | 944 (22.6) | 245 (24.5) | 1,189 (22.9) |
|
| |||
| Diabetes mellitus | 236 (5.6) | 270 (27.0) | 506 (9.8) |
|
| |||
| Cholesterol, mg/dl | |||
| Total | 196.2 ± 35.1 | 197.2 ± 37.9 | 196.4 ±35.7 |
| LDL* | 119.3 ± 31.2 | 121.2 ± 32.0 | 119.7 ±31.4 |
| HDL | 51.6 ± 15.0 | 48.4 ± 14.4 | 51.0 ± 15.0 |
| Triglycerides | 126.6 ± 75.5 | 142.7 ± 125.8 | 129.7 ± 87.7 |
|
| |||
| BMI, kg/m2 | 28.2 ± 5.6 | 28.0 ± 4.9 | 28.2 ±5.4 |
|
| |||
| Blood pressure, mm Hg | |||
| Systolic | 121.0 ± 18.5 | 145.0 ± 21.9 | 125.6 ± 21.4 |
| Diastolic | 71.3 ± 10.1 | 75.1 ± 11.0 | 72.1 ± 10.4 |
|
| |||
| Cigarette smoking | |||
| Never | 2,177 (52.0) | 447 (44.7) | 2,624 (50.6) |
| Former | 1,457 (34.8) | 397 (44.7) | 1,854 (35.8) |
| Current | 551 (13.2) | 156 (15.6) | 707 (13.6) |
|
| |||
| Antihypertensive medication use | 1,092 (26.1) | 591 (59.1) | 1,683 (32.5) |
|
| |||
| CAC, Agatston | 0 (0-24.2) | 94.5 (4.7-374.5) | 0 (0-63.6) |
|
| |||
| hsCRP, mg/l | 1.9 (0.8-4.3) | 2.1 (1.0-4.1) | 1.9 (0.8-4.3) |
|
| |||
| ABI, | 1.1 (1.1-1.2) | 1.1 (1.0-1.2) | 1.1 (1.1-1.2) |
Values are mean ± SD, n (%), or median (interquartile range).
LDL sample size = 5,123 (due to missing values)
ABI = ankle-brachial index; ASCVD = atherosclerotic cardiovascular disease; BMI = body mass index; CAC = coronary artery calcium score; cPCE = calibrated Pooled Cohort Equation; HDL = high-density lipoprotein; hsCRP = high-sensitivity C-reactive protein; LDL = low-density lipoprotein.
As to the added value of the additional risk markers, CAC, ABI, and FH were each independent predictors of incident ASCVD events in multivariable Cox models (Table 2). Online Table 1 shows the hazard ratios and 95% CIs of the additional risk markers and the covariates in the multivariable Cox model.
Table 2. ASCVD Event Hazard Associated with Additional Risk Markers*.
| Novel Risk Marker | Univariable | Multivariable† | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| HR | 95% CI | p Value | HR | 95% CI | p Value | |
| CAC (ln+1, per 1.98 SD) | 2.06 | 1.86-2.29 | <0.001 | 1.58 | 1.40-1.79 | <0.001 |
| hsCRP (ln, per 1.17 SD) | 1.23 | 1.10-1.37 | <0.001 | 1.12 | 0.99-1.27 | 0.077 |
| Family history of ASCVD | 1.57 | 1.26-1.95 | <0.001 | 1.37 | 1.09-1.71 | 0.007 |
| ABI (per 0.11 SD) | 0.69 | 0.63-0.75 | <0.001 | 0.87 | 0.79-0.94 | 0.001 |
Total population N = 5,185; number of events = 320.
Multivariable Cox model adjusted for age, sex, race/ethnicity, diabetes mellitus, total cholesterol, HDL cholesterol, BMI, systolic blood pressure, cigarette smoking status, and antihypertensive medication use CI = confidence interval; HR = hazard ratio; other abbreviations as in Table 1.
As to whether the markers improve discrimination beyond the cPCEs, the Central Illustration shows the comparative improvement in area under the curve (AUC)/C-statistic afforded by the addition of each of the additional risk markers to the cPCE for predicting incident ASCVD; CAC was the only additional risk marker to significantly improve discrimination.
Central Illustration. Utility of risk markers for ASCVD Assessment: Receiver Operator Characteristic Curves.
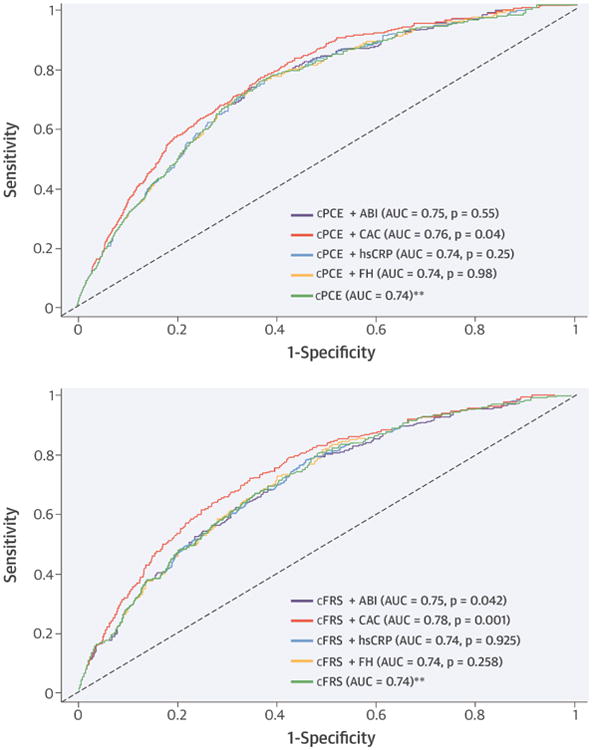
To assess predictive accuracy and reclassification improvement of various risk markers for incident atherosclerotic cardiovascular disease (ASCVD), receiver operator characteristics curves showing the area under the curve (AUC) were calculated for (A) calibrated Pooled Cohort Equation (cPCE) and (B) calibrated Framingham Risk Score (cFRS) for study participants. Of the factors assessed, coronary artery calcium (CAC) modestly improved the discriminative ability of the cPCE. **Reference. ABI = ankle-brachial index; FH = family history; hsCRP = high-sensitivity C-reactive protein.
Table 3 shows the NRI for events and nonevents when CAC, hsCRP, FH, and ABI were added individually to the cPCE. The addition of CAC to the model resulted in a larger improvement in the classification of risk than the other risk markers, but was limited to an improvement in classification for events (event NRI: 0.178; 95% CI: 0.080 to 0.256]; nonevent NRI: -0.059; 95%CI: (-0.075 to -0.030). ABI provided a very modest but the highest nonevent NRI (event NRI: 0.013; 95% CI: -0.034 to 0.051); nonevent NRI 0.004; 95% CI: -0.004 to 0.011). Using 3 ASCVD risk categories (0% to 5%, 5% to 7.5%, and >7.5%) instead of the 2 categories (sensitivity analysis) produced similar results (Online Table 2) for all the additional risk markers considered.
Table 3. Net Reclassification Improvement: Risk Markers Added to cPCE.
| cPCE Alone | ||||
|---|---|---|---|---|
| cPCE + Marker | <7.5% | ≥7.5 % | Row Total | NRI (95% CI) |
| cPCE + CAC | ||||
| Event (n = 320) | ||||
| <7.5% | 107 | 19 | 126 (39.4) | 0.178 (0.080-0.256) |
| ≥7.5% | 76 | 118 | 194 (60.6) | |
| Column total | 183 (57.2) | 137 (42.8) | ||
| Nonevent (n =4,865) | ||||
| <7.5% | 3,506 | 202 | 3,708 (76.2) | -0.059 (-0.075,-0.030) |
| ≥7.5% | 496 | 661 | 1,157 (23.8) | |
| Column total | 4,002 (82.3) | 863 (17.7) | ||
| Total NRI for CAC | 0.119 (0.080-0.256) | |||
| cPCE + hsCRP | ||||
| Event (n = 320) | ||||
| <7.5% | 165 | 9 | 174 (54.4) | 0.028 (-0.013-0.077) |
| ≥7.5% | 18 | 128 | 146 (45.6) | |
| Column total | 183 (57.2) | 137 (42.8) | ||
| Nonevent (n =4,865) | ||||
| <7.5% | 3,882 | 98 | 3,980 (81.8) | -0.005 (-0.015-0.003) |
| ≥7.5% | 120 | 765 | 885(18.2) | |
| Column total | 4,002 (82.3) | 863(17.7) | ||
| Total NRI for hsCRP | 0.024 (-0.015-0.067) | |||
| cPCE + FH | ||||
| Event (n = 320) | ||||
| <7.5% | 153 | 12 | 175 (54.6) | 0.056 (0.007-0.118) |
| ≥7.5% | 30 | 125 | 155 (48.4) | |
| Column total | 183(57.2) | 137(42.8) | ||
| Nonevent (n =4,865) | ||||
| <7.5% | 3,832 | 140 | 3,972 (81.6) | -0.006 (-0.019-0.003) |
| ≥7.5% | 170 | 723 | 893 (18.4) | |
| Column total | 4,002 (82.3) | 863 (17.7) | ||
| Total NRI for FH | 0.051 (0.000-0.109) | |||
| cPCE + ABI | ||||
| Event (n = 320) | ||||
| <7.5% | 166 | 13 | 179 (55.9) | 0.013 (-0.034-0.051) |
| ≥7.5% | 17 | 124 | 141 (44.1) | |
| Column total | 183 (57.2) | 137 (42.8) | ||
| Nonevent (n =4,865) | ||||
| <7.5% | 3,910 | 113 | 4,023 (82.7) | 0.004 (-0.004-0.011) |
| ≥7.5% | 92 | 750 | 842 (17.3) | |
| Column total | 4,002 (82.3) | 863 (17.7) | ||
| Total NRI for ABI | 0.017 (-0.031-0.058) | |||
A total of 194 (3.7%) CHD events occurred. When considering the comparative improvement in AUC/C-statistic afforded by adding each of the risk markers to the calibrated Framingham Risk Score (cFRS) for predicting incident CHD, CAC was the only one to significantly improve discrimination (Central Illustration). Table 4 shows the NRI for events and nonevents when CAC, hsCRP, FH, and ABI were added individually to the cFRS. The addition of CAC resulted in a larger improvement in the classification of risk than the other additional risk markers, but was limited to an improvement in classification of events.
Table 4. Net Reclassification Improvement: Risk Markers Added to cFRS*.
| cFRS Alone | |||||
|---|---|---|---|---|---|
| cFRS + Marker | <10% | 10%-20% | >20 % | Row Total | NRI (95% CI) |
| cFRS + CAC | |||||
| Event (n = 194) | |||||
| <10% | 132 | 5 | 0 | 137 (70.6) | 0.119 (0.045-0.239) |
| 10%-20% | 26 | 18 | 2 | 46 (23.7) | |
| >20% | 0 | 4 | 7 | 11 (5.7) | |
| Column total | 158 (81.4) | 27 (13.9) | 9 (4.6) | ||
| Nonevent (n = 4,991) | |||||
| <10% | 4,540 | 63 | 8 | 4,611 (92.4) | -0.034 (-0.053,-0.017) |
| 10%-20% | 230 | 101 | 11 | 342 (6.9) | |
| >20% | 3 | 20 | 15 | 38 (0.8) | |
| Column total | 4,773 (95.6) | 184 (3.7) | 34 (0.7) | ||
| Total NRI for CAC | 0.084(0.024,0.196) | ||||
| cFRS + hsCRP | |||||
| Event (n = 194) | |||||
| <10% | 158 | 1 | 0 | 159 (82.0) | 0.005 (-0.027-0.027) |
| 10%-20% | 1 | 24 | 1 | 26 (13.4) | |
| >20% | 0 | 2 | 7 | 9 (4.6) | |
| Column total | 159 (82.0) | 27 (13.9) | 8 (4.1) | ||
| Nonevent (n = 4,991) | |||||
| <10% | 4,749 | 16 | 0 | 4765 (95.5) | -0.002 (-0.007-0.001) |
| 10%-20% | 28 | 158 | 6 | 192 (3.8) | |
| >20% | 0 | 3 | 31 | 34 (0.7) | |
| Column total | 4,777 (95.7) | 177 (3.5) | 37 (0.7) | ||
| Total NRI for hsCRP | 0.003 (-0.028-0.026) | ||||
| cFRS + FH | |||||
| Event (n = 194) | |||||
| <10% | 150 | 6 | 0 | 156 (80.4) | 0.010 (-0.032-0.074) |
| 10%-20% | 8 | 19 | 3 | 30 (15.5) | |
| >20% | 0 | 3 | 5 | 8 (4.1) | |
| Column total | 158 (81.4) | 28 (14.4) | 8 (4.1) | ||
| Nonevent (n = 4,991) | |||||
| <10% | 4,681 | 65 | 0 | 4,746 (95.1) | -0.007 (-0.013-0.002) |
| 10%-20% | 95 | 98 | 13 | 206 (4.1) | |
| >20% | 0 | 17 | 22 | 39 (0.8) | |
| Column total | 4,776 (95.7) | 180 (3.6) | 35 (0.7) | ||
| Total NRI for FH | 0.003 (-0.034-0.069) | ||||
| cFRS + ABI | |||||
| Event (n = 194) | |||||
| <10% | 152 | 4 | 0 | 156 (80.4) | 0.041 (-0.010-0.108) |
| 10%-20% | 6 | 17 | 1 | 24 (12.4) | |
| >20% | 1 | 6 | 7 | 14 (7.2) | |
| Column total | 159 (82.0) | 27 (13.9) | 8 (4.1) | ||
| Nonevent (n = 4,991) | |||||
| <10% | 4,724 | 50 | 0 | 4,774 (95.7) | -0.003 (-0.008-0.004) |
| 10%-20% | 51 | 106 | 12 | 169 (3.4) | |
| >20% | 6 | 18 | 24 | 48 (1.0) | |
| Column total | 4,781 (95.8) | 174 (3.5) | 36 (0.7) | ||
| Total NRI for ABI | 0.039 (-0.011-0.109) | ||||
Discussion
The goal of this study was to assess the improvement in discrimination that would be gained by adding the recommended nontraditional risk markers to the calibrated 2013 Pooled Cohort Equation. The current study shows that among 4 ACC/AHA recommended nontraditional risk markers studied, CAC provides the highest (albeit, modest) improvement in discrimination over and beyond the cPCE (Central Illustration). The superiority of CAC appears to be consistent across all possible ASCVD strata. To our knowledge, this is the first study to assess whether nontraditional risk markers improve risk prediction afforded by the cPCE.
Previous studies showed that CAC, ABI, hsCRP, and FH improve discrimination and classification of risk over the Framingham risk score (FRS), but to varying degrees (15-18). Our group (19) and a report by the Rotterdam study (15) showed that among these 4 risk markers, CAC provided the greatest improvement in discrimination across the whole CHD risk spectrum and also in those classified as intermediate risk by the FRS. In the 2013 ACC/AHA guidelines (1), the primary outcome was expanded to ASCVD, which includes fatal and nonfatal stroke, in addition to fatal and nonfatal MI. The PCE also includes variables for the presence or absence of DM and race (white or African American) (1). The present study shows that among the 4 recommended nontraditional risk markers, CAC is superior for improving ASCVD risk prediction and may be useful in individuals in whom quantitative ASCVD risk-based treatment decision making may be uncertain.
The magnitude of improvement in discrimination afforded by the 4 nontraditional risk markers beyond the cPCE appears to be modest compared with what was reported in MESA using Framingham risk factors as the baseline model (16) but similar when the FRS was used (Table 4). For example, in the study by Polonsky et al. (16) in which the Framingham risk factors were used as the baseline model, CAC had an event NRI of 0.23 and a nonevent NRI of 0.02 for incident CHD events. In the present study, when the cFRS was used in the same cohort for incident CHD events, CAC had an event NRI of 0.119 and a nonevent NRI of -0.034. However CAC, as well as some of the other risk markers, showed significant improvement in classification when the analysis was limited to those classified as intermediate risk by the Framingham risk score (19).
It should be noted that during National Cholesterol Education Program/Adult Treatment Panel III era, these additional risk markers were only recommended for improvement in risk assessment in intermediate FRS individuals (20). Presently these additional risk markers are recommended for improvement in ASCVD risk assessment in those who are not in 1 of the 4 statin-benefit groups and for whom the decision to initiate statin is uncertain (2). It is plausible that despite the modest improvement in discrimination observed in the present study, these additional risk markers may still have significant roles for ASCVD risk assessment in a subgroup of the population. Studies on the improvement in discrimination afforded by these additional risk markers in subgroups of asymptomatic individuals (primary prevention) is needed, especially those who are not recommended statin therapy by the new ACC/AHA cholesterol guidelines (1).
Despite the finding of superior (albeit modest) discrimination when CAC was added to the PCE, its ultimate use in the clinical setting for risk assessment, especially after the introduction of the ASCVD risk estimator, demands consideration of additional variables such as cost effectiveness, radiation exposure, and patient preference.
Study Limitations
The present study has limitations. Even though we excluded participants who were taking statins during the baseline MESA exam from this analysis, some of the participants included in this analysis were prescribed statins during follow-up. This may have affected our event rates and therefore our results. However, sensitivity analysis in which statin use during 10-year follow-up was accounted for in our models did not significantly change either our point estimates or our conclusions. The MESA cohort is also not representative of the U.S. population. In addition, the calibrated versions of the PCE and FRS are not presently available to clinicians, so while these tools are the most appropriate for statistical analysis, some caution may be needed when directly applying these results to clinical practice with the present PCE and FRS.
Conclusions
In this study of well-characterized individuals, including those who are nonwhite as well as white race, followed for 10 years, CAC, ABI, and FH were each independently associated with incident ASCVD beyond traditional risk factors. The nontraditional risk factors resulted in varying degrees of improvement in discrimination and reclassification of risk, including no improvement. Verification of our findings in other race and ethnic groups and other cohorts are needed.
Supplementary Material
Online Table 1: Hazard of an ASCVD event associated with additional risk markers. The MultiEthnic Study of Atherosclerosis, 2000-2012
Online Table 2: Net Reclassification improvement gained by the addition of coronary artery calcium (CAC) score, high sensitivity C - reactive protein (hsCRP), family history (FH) and ankle brachial index (ABI) to the calibrated Pooled Cohort Equation (cPCE) for incident atherosclerotic cardiovascular (ASCVD) event, using <5%, 5-7.5%, and >7.5% categories.
Perspective.
Competency in Medical Knowledge
The nontraditional risk markers cited by the 2013 ACC/AHA cholesterol guidelines for ASCVD risk refinement and considered in this study provided modest degrees of improvement in discrimination over and beyond the cPCE, including no improvement.
Translational Outlook
Confirmation of our findings in other cohorts should consider the utility and the cost effectiveness of using these risk markers for improving ASCVD risk assessment. The promise seen with CAC needs further study.
Acknowledgments
This research was supported by contracts N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168 and N01-HC-95169 from the National Heart, Lung, and Blood Institute and by grants UL1-TR-000040 and UL1-RR-025005 from NCRR. Diversity Supplement to R01HL098445 (PI: J. Jeffrey Carr). The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Abbreviations and Acronyms
- ABI
ankle-brachial index
- ASCVD
atherosclerotic cardiovascular disease
- CAC
coronary artery calcium
- FH
family history
- hsCRP
high-sensitivity C-reactive protein
- PCE
Pooled Cohort Equation
Footnotes
Financial Disclosure and Relationship with Industry: None for all coauthors
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Goff DC, Jr, Lloyd-Jones DM, Bennett G, et al. J Am Coll Cardiol. 2014. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines; pp. 2935–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Bild DE, Bluemke DA, Burke GL, et al. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:87181. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 4.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 5.Carr JJ, Nelson JC, Wong ND, et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 6.Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 7.Criqui MH, McClelland RL, McDermott MM, et al. The ankle-brachial index and incident cardiovascular events in the MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2010;56:1506–12. doi: 10.1016/j.jacc.2010.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–45. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 9.DeFilippis AP, Young R, Carrubba CJ, et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med. 2015;162:266–75. doi: 10.7326/M14-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Janssen KJ, Moons KG, Kalkman CJ, et al. Updating methods improved the performance of a clinical prediction model in new patients. J Clin Epidemiol. 2008;61:76–86. doi: 10.1016/j.jclinepi.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 11.Harrell FE, Califf RM, Pryor DB, et al. Evaluating the yield of medical tests. JAMA. 1982;247:2543–6. [PubMed] [Google Scholar]
- 12.Pencina MJ, D'Agostino RB, Vasan RS. Statistical methods for assessment of added usefulness of new biomarkers. Clin Chem Lab Med. 2010;48:1703–11. doi: 10.1515/CCLM.2010.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kerr KF, Wang Z, Janes H, et al. Net reclassification indices for evaluating risk prediction instruments: a critical review. Epidemiology. 2014;25:114–21. doi: 10.1097/EDE.0000000000000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.D'Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P CHD Risk Prediction Group. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286:180–7. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 15.Kavousi M, Elias-Smale S, Rutten JH, et al. Evaluation of newer risk markers for coronary heart disease risk classification: a cohort study. Ann Intern Med. 2012;156:438–44. doi: 10.7326/0003-4819-156-6-201203200-00006. [DOI] [PubMed] [Google Scholar]
- 16.Polonsky TS, McClelland RL, Jorgensen NW, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303:1610–6. doi: 10.1001/jama.2010.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ridker PM, Paynter NP, Rafai N, et al. C-reactive protein and parental history improveglobal cardiovascular risk prediction: the Reynolds Risk Score for men. Circulation. 2008;118:2243–51. doi: 10.1161/CIRCULATIONAHA.108.814251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sivapalaratnam S, Boekholdt SM, Trip MD, et al. Family history of premature coronary heart disease and risk prediction in the EPIC-Norfolk prospective population study. Heart. 2010;96:1985–9. doi: 10.1136/hrt.2010.210740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yeboah J, McClelland RL, Polonsky TS, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate risk individuals. JAMA. 2012;308:788–95. doi: 10.1001/jama.2012.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2010;56:e50–e103. doi: 10.1016/j.jacc.2010.09.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Table 1: Hazard of an ASCVD event associated with additional risk markers. The MultiEthnic Study of Atherosclerosis, 2000-2012
Online Table 2: Net Reclassification improvement gained by the addition of coronary artery calcium (CAC) score, high sensitivity C - reactive protein (hsCRP), family history (FH) and ankle brachial index (ABI) to the calibrated Pooled Cohort Equation (cPCE) for incident atherosclerotic cardiovascular (ASCVD) event, using <5%, 5-7.5%, and >7.5% categories.


