Abstract
Background
Compared with the general population in the United States (U.S.), Hispanics with hypertension are less likely to be aware of their condition, to take antihypertensive medication, and to adopt healthy lifestyles to control high blood pressure. We examined whether a multi-community intervention successfully increased the prevalence of actions to control hypertension among Hispanics.
Methods
Annual survey from 2009–2012 was conducted in six Hispanic communities in the Racial and Ethnic Approaches to Community Health (REACH) Across the U.S. project. The survey used address based sampling design that matched the geographies of intervention program.
Results
Age- and sex-standardized prevalences of taking hypertensive medication, changing eating habits, cutting down on salt, and reducing alcohol use significantly increased among Hispanics with self-reported hyper-tension in REACH communities. The 3-year relative percent increases were 5.8, 6.8, 7.9, and 35.2% for the four indicators, respectively. These favorable (healthier) trends occurred in both foreign-born and U.S.-born Hispanics.
Conclusion
This large community-based participatory intervention resulted in more Hispanic residents in the communities taking actions to control high blood pressure.
Keywords: Community intervention, Hispanic, Hypertension, Health disparity
Introduction
Hispanics, the nation's largest and fastest growing minority group, comprised 16% of the United States (U.S.) population in 2010 and are expected to comprise 30% by 2050 (Ortman and Guarneri, 2009). Hispanics bear a disproportionate burden of disease, injury, death, and disability when compared with non-Hispanic whites (Centers for Disease and Prevention, 2004). If Hispanics continue to experience poorer health status, the projected demographic change in the population will magnify the nation's economic, social, and health disparities (Centers for Disease and Prevention, 2004). The Healthy People 2020 goal of achieving health equity cannot succeed without eliminating Hispanic health disparities.
As in some other ethnic groups (e.g., non-Hispanic white, non-Hispanic black, or American Indian), cardiovascular disease is the leading cause of death in Hispanics (Centers for Disease and Prevention, 2004). Hypertension is a major risk factor for cardiovascular disease and is a significant predictor of premature death and disability. In 2010, the prevalence of hypertension was similar or somewhat lower in Hispanics than that in non-Hispanic whites (Go et al., 2014; Yoon et al., 2012), but as data from the National Health and Nutrition Examination Survey (NHANES) showed, Hispanics with hypertension were less likely to be aware of their condition than were non-Hispanic whites and non-Hispanic blacks (Yoon et al., 2012). Hispanics were also less likely to be instructed by their physicians or other health professionals to take antihypertensive medication or adopt lifestyle modifications to control their blood pressure, or to follow the medical advice once given (Wang and Wang, 2004). Among persons with hypertension, Hispanics were less likely to have their blood pressure adequately controlled than non-Hispanic whites and non-Hispanic blacks (Wang and Wang, 2004; Yoon et al., 2012).
Racial and Ethnic Approaches to Community Health Across the U.S. (REACH U.S.), funded by the Centers for Disease Control and Prevention (CDC), was launched in 2007 (Liburd, 2011). This project supported the development and implementation of innovative approaches to working with racial and ethnic minority populations to eliminate health disparities. The 40 funded communities targeted one or more racial and ethnic groups, including African American/black, Hispanic/Latino, Asian, Native Hawaiian/Other Pacific Islander, and American Indian/Alaska Native. The health priority areas included cardiovascular disease, diabetes mellitus, breast and cervical cancer, adult/older adult immunization, hepatitis B, asthma, and infant mortality. Six of the 40 communities chose cardiovascular disease as the only or one of the priority areas in their intervention of Hispanics residents. These six communities are the focus of this report. The purpose of this study was to examine whether REACH U.S. interventions resulted in favorable 4-year trends of actions to control high blood pressure among residents with self-reported hypertension in Hispanic communities.
Methods
REACH U.S. community interventions
REACH U.S. included 40 communities in the nation (Liburd, 2011). The six REACH U.S. Hispanic communities in this report were located in California, Illinois, Massachusetts, and New York (see Acknowledgement). Local strategies varied according to local needs; however, interventions in all communities had three major common approaches: building strong community-based coalitions; focusing on policy, systems, and environmental (PSE) changes; and cultural and linguistic tailoring of interventions.
Community-based coalitions
Community coalitions were established, which included community-based organizations, local or state health departments, universities, health care providers, and organizations or groups with primary missions unrelated to health, such as faith-based groups, YMCA, social service agencies, volunteer groups, and various advocacy groups. These coalitions were primarily driven by residents of the community at every stage of the program, including planning, implementation, and evaluation. The coalitions met regularly to discuss the context, causes, and solutions for health disparity and to take actions outlined in coalition-developed community action plans.
Policy, systems, and environmental changes
REACH U.S. focused on PSE change approaches that addressed “upstream” factors that impact health disparities. The coalitions assessed disparities in health care access and outcomes and advocated for equitable health care access, service delivery, and quality (Golub et al., 2011). Some communities worked with clinical partners to provide medical interpreting, translation, and cultural broker services to Latino clients; some created patient-centered medical home initiatives; and some utilized electronic health record systems to promote patient-provider communication and patient self-management (Calman et al., 2007). Educational approaches focused on provider knowledge and beliefs about cultural competence and health disparities. The project also made efforts to increase awareness and utilization of public health insurance programs and community health services for those without health insurance.
REACH U.S. also promoted community and environmental changes regarding food security and access to healthy foods (Castillo et al., 2013). The Neighborhood Food Watch program was such an example. The coalitions worked with local food businesses and vendors to increase healthy food options at neighborhood grocery stores and to develop new full service grocery stores in underserved areas. Some communities supported the production of locally grown food, such as community gardens, school gardens, and home gardens. To increase the available opportunities to engage in physical activity, REACH U.S. implemented a variety of worksite wellness policies (Maxwell et al., 2011) and revitalized the community environment to include more accessible recreational areas.
Culturally tailored intervention
REACH implemented an extensive range of strategies to tailor their interventions to the needs as well as the characteristics of the Hispanic population. Hispanic community leaders were invited to serve as coalition members and to act as catalysts for change in the community. Education initiatives to improve blood pressure control took account of cultural factors, such as inadequate cardiovascular disease knowledge, lack of familiarity with medical care systems, and poor access to quality health care.
In addition, health promotion materials (including newsletters and posters), talk shows on local radio stations, educational classes, and workshops were culturally and linguistically appropriate and tailored to the target population's health literacy level. The church community was an important source of social support and community leadership (Kaplan et al., 2009). Churches were the active sites for a series of health promotion, blood pressure screening, disease prevention, and education activities. The switching from offering traditional to healthier foods in churches and other gatherings facilitated the establishment of a healthier eating norm in Hispanic communities.
Many communities recruited and trained local, bilingual lay health workers (i.e., Promotoras) to provide culturally relevant and appropriate education, counseling, and social support (Cosgrove et al., 2014). These grass-roots health workers had well-established ties and a good reputation in the community. They responded to the needs of patients and families, particularly new immigrants, provided health education on cardiovascular disease, delivered direct or indirect assistance related to blood pressure control, and served as mediators between participants and the healthcare system.
Hispanic cultures are predominantly family-oriented. When a family member is experiencing a chronic disease, such as cancer, diabetes, or hypertension, typically the entire family acts to take care of this member. REACH projects involved all family members across multiple generations through various sectors such as worksites, churches, senior service facilities, and schools. The Massachusetts program was able to form cohesive units of care through active engagement with the major senior center and through provision of family-centered activities that focused on improving the health outcomes of participants.
REACH U.S. Risk Factor Survey
As part of the REACH U.S. project evaluation, the CDC conducted annual Risk Factor Surveys from 2009 through 2012 in 28 communities that targeted cardiovascular diseases, diabetes, breast and cervical cancer, adult immunization, or hepatitis B (Liao et al., 2011). This report includes data from six Hispanic communities where cardiovascular disease is the only or one of primary foci in their intervention.
An address-based sampling design was used in the survey to reduce the potential coverage bias of traditional landline random-digit-dialing (Liao et al., 2011). Geographic information systems technology was used to construct an address frame that matched the intervention geographies of the REACH program. The survey was conducted by telephone for sampled addresses that matched to telephone numbers. Self-administered questionnaires were mailed to households without a phone match and to those who did not respond by telephone. Participants had the choice of using English or Spanish for the telephone interview and for self-administration of questionnaire. On average 76% cooperated with the screening interview to determine the age and racial/ethnic eligibility of the household members over the survey years among all households successfully contacted by telephone. The completion rate of detailed household member interviews was 50% for eligible household members. For the mailed questionnaire, the return rate was on average 28%. Of respondents in this report, 51% were from telephone interviews, and 49% were from questionnaire mailings.
A uniform questionnaire was used in all communities and in all survey years. Respondents were asked “Have you ever been told by a doctor, nurse, or other professional that you have high blood pressure?” Adults who reported prehypertension or borderline high blood pressure were not considered as having hypertension. Those who reported having high blood pressure were further asked: “Are you currently taking medicine for your high blood pressure?” and other questions related to actions to control high blood pressure. These questions began with a general probe, “Are you now doing any of the following to help lower or control your high blood pressure?” followed by four questions about: (1) changing your eating habits? (2) cutting down on salt? (3) reducing alcohol use? and (4) exercising? Other information presented in this report included the highest grade or year of school completed, the annual household income from all sources, and birth place of the respondent (U.S.-born or foreign-born).
The study was approved by the Office of Management and Budget (OMB 0920-0805) and the Institutional Review Board of the Centers for Disease Control and Prevention (#5337).
Data analysis
Prevalences of actions to control high blood pressure among those reported having high blood pressure were calculated for each survey year and were ageand sex-standardized by the direct method to the distribution of adults with self-reported hypertension in the U.S. based on the 2009 Behavioral Risk Factor Surveillance System (BRFSS) (Mokdad et al., 2003). The prevalences were also stratified by place of birth (foreign-born vs. U.S.-born) for Hispanics in REACH communities. Logistic regression was performed on personal level data to examine the temporal trend through testing the year term in the prevalence from 2009 through 2012. Age (categorized into four groups), and sex were included in the model as covariates. The year × place of birth interaction term was tested in logistic regression to examine whether the secular trends are significantly different between foreign-born and U.S.-born Hispanics.
We calculated the 3-year absolute percentage point change and 3-year relative percent change for each action to control high blood pressure from 2009 through 2012. The age- and sex-standardized prevalence in the four survey years was the dependent variable and linear regression was performed with a year term as the independent variable in the model. The 3-year absolute percentage point change was calculated as 3 * β, where β is the regression coefficient of the year term derived from the linear regression. When the age- and sex-standardized prevalence was log transformed as the dependent variable in the regression model, the average annual percent change was calculated as 100 * (eβ – 1) and the 3-year percent change was 100 * (e3β – 1).
Analyses were performed using SUDAAN software (Version 11, Research Triangle Institute, NC) to account for the complex sampling designs.
Results
Characteristics of study populations in 2009 (baseline)
There were 968 Hispanic respondents who reported having high blood pressure in 2009, 1215 in 2010, 1570 in 2011, and 1445 in 2012 for the six REACH U.S. communities. Baseline characteristics of REACH populations are shown in Table 1. For comparison purpose, we also present data for the U.S. non-Hispanic whites and Hispanics with self-report hypertension in 2009 from BRFSS. REACH communities had a similar age distribution as the Hispanic population in BRFSS; both were, in general, younger than non-Hispanic whites in BRFSS. Educational attainment and annual household income were markedly lower among Hispanics in REACH communities than non-Hispanic whites and to a lesser extent lower than Hispanics in BRFSS. These data illustrate that the six REACH communities were disadvantaged Hispanic communities.
Table 1.
Characteristics of adults and age- and sex-standardized prevalence ofmeasures of actions to control high blood pressure in REACH USHispanic communities, 2009, US non-Hispanicwhite and US Hispanic from 2009 the Behavioral Risk Factor Surveillance System.
| REACH U.S. |
Behavioral risk factor surveillance system |
|||||
|---|---|---|---|---|---|---|
| Communities |
Non-Hispanic white |
Hispanic |
||||
| % | 95% CI | % | 95% CI | % | 95% CI | |
| Characteristics (unadjusted) | ||||||
| Age groups | ||||||
| 18–44 | 33.2 | 29.6–37.0 | 19.1 | 18.6–19.7 | 34.3 | 31.8–36.9 |
| 45–54 | 23.9 | 21.1–26.9 | 18.8 | 18.4–19.2 | 23.5 | 21.6–25.5 |
| 55–64 | 25.2 | 22.5–28.0 | 23.2 | 22.8–23.6 | 19.8 | 18.2–21.5 |
| ≥65 | 17.8 | 15.8–20.1 | 38.9 | 38.4–39.3 | 22.4 | 20.8–24.1 |
| % Male | 47.3 | 43.8–49.3 | 51.2 | 50.6–51.7 | 51.8 | 49.4–54.2 |
| Education level | ||||||
| Less than high school | 46.0 | 42.5–49.5 | 8.4 | 8.1–8.7 | 38.0 | 35.7–40.4 |
| High school | 26.1 | 23.0–29.4 | 33.2 | 32.7–33.7 | 28.1 | 25.8–30.5 |
| >High school | 27.9 | 24.8–31.4 | 58.4 | 58.0–58.9 | 33.9 | 31.7–36.1 |
| Annual family income | ||||||
| <25,000 | 63.6 | 59.9–67.2 | 26.1 | 25.6–26.6 | 51.8 | 49.2–54.4 |
| 25,000–<50,000 | 25.0 | 21.7–28.5 | 28.4 | 27.9–28.8 | 26.6 | 24.3–29.1 |
| ≥50,000 | 11.4 | 9.1–14.2 | 45.6 | 45.0–46.1 | 21.6 | 19.6–23.7 |
Table 2 shows the adjusted prevalences of the five actions to control high blood pressure from 2009 through 2012. Logistic regression analyses confirmed a significant increase (p < 0.05) for four of the five actions (except exercising). Among these four actions, the 3-year absolute increases ranged from 4.3 to 9.6 percentage points and the relative percent increases ranged from 5.8% to 35.2%.
Table 2.
Age- and sex-standardized prevalence (%) and 3-year trends in actions to control high blood pressure in REACH US Hispanic communities, 2009–2012.
| Actions to control high blood pressure |
Survey year |
P value for trend | 3-year changes |
||||
|---|---|---|---|---|---|---|---|
| 2009 | 2010 | 2011 | 2012 | Absolute | Percent | ||
| Taking medication | 73.4 | 72.9 | 77.8 | 76.5 | 0.049 | 4.3 | 5.8 |
| Changing eating habits | 76.8 | 79.3 | 80.3 | 82.3 | 0.029 | 5.3 | 6.8 |
| Cutting down on salt | 78.1 | 83.8 | 83.0 | 85.3 | 0.001 | 6.2 | 7.9 |
| Reducing alcohol use | 27.2 | 32.2 | 36.4 | 36.5 | <0.001 | 9.6 | 35.2 |
| Exercising | 65.4 | 65.9 | 66.1 | 68.6 | 0.357 | 2.9 | 4.5 |
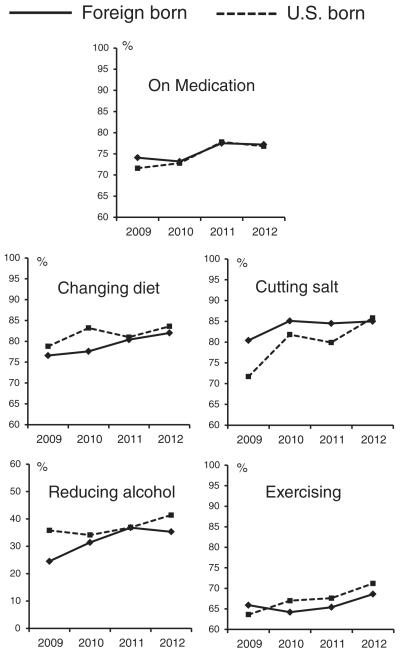
Stratification analyses demonstrated that the increasing trends in antihypertensive medication use, changing diet, reducing alcohol use, and exercising to control high blood pressure occurred similarly in both foreign-born and U.S.-born Hispanics (Fig. 1). The prevalence of cutting down on salt was lower among U.S.-born Hispanics than foreign-born Hispanics at baseline (2009), but increased sharply among the U.S.-born group afterward. All the interaction terms between year and place of birth were not statistically significant (ps > 0.05).
Fig. 1.
Trends of age- and sex-standardized prevalence of five actions to control high blood pressure among Hispanics with self-reported hypertension in REACH U.S. communities, 2009–2012, foreign- vs U.S.-born.
Discussion
Prior to REACH U.S., only a few small-scale (up to 920 patients) and short-term (up to 9 months) hypertension interventions at the local level targeting Hispanic patients had been reported in the literature (Balcazar et al., 2009; Lai, 2007; Rocha-Goldberg Mdel et al., 2010; Sanchez et al., 2014). The REACH U.S. project, a large scale community-based intervention, demonstrates a significant increase in actions to control hypertension – taking medication, changing eating habits, cutting down on salt, and reducing alcohol use – among six Hispanic communities from 2009 through 2012. The favorable trends in most of the actions to control hypertension in REACH communities were similar in both foreign-born and U.S.-born Hispanics, indicating that the project reached the most disadvantaged segments of the community, including those who were new immigrants and those with language barriers.
Among persons with hypertension, Hispanics are less likely to have their blood pressure under control than non-Hispanic whites and non-Hispanic blacks (Wang and Wang, 2004; Yoon et al., 2012). Economic, social, behavioral, cultural factors, and access to quality health care likely contributed to this health disparity. REACH coalitions recognized that many important factors fall outside the traditional realms of the physician's office and moved beyond interventions that focus on individual disease treatment to policy, system, and environmental change. These approaches created supportive community environments for healthy behaviors and made the healthy choices easier and became the public norms.
The REACH U.S. project used culturally relevant interventions for underrepresented Hispanic populations. These interventions have two dimensions: surface and deep structures (Resnicow et al., 1999). Surface structure refers to the tailoring of print and audiovisual materials to Hispanic populations as well as identifying channels and settings that are most appropriate for delivery of messages and programs to the target population. For example, REACH U.S. Hispanic community coalitions created strong bilingual and bi-cultural faith-based outreach initiatives for Hispanic/Latino churches. The capacity and resources of local faith-based institutions were used to change the knowledge and health behaviors of community members related to health promotion, disease (e.g., hypertension or diabetes) self-management, and navigation of the health care system. These initiatives also motivated clergy and church members to promote health equality and equal access to care.
The second dimension of culturally tailoring interventions—deep structure—goes further to incorporate cultural beliefs and social norms into the REACH U.S. project. Several cultural characteristics and behaviors in Hispanics are barriers to health care-seeking. For example, some Hispanics believe that sickness is God's will and control of it is beyond an individual's power (Hunter et al., 2007). However, Hispanic culture places a great deal of emphasis on both immediate and extended family. Hence, family-based interventions involving spouses and family members through Promotoras (community health workers) were a key strategy.
The Promotoras felt passionate about their work and often resided in the communities they served. They provided education, training, and support for healthy lifestyles and chronic disease prevention and management; raised community members' health literacy levels; and served as advocates for friends, family, and providers of social support for health improvement. They also assisted with navigation to needed services, including health, basic needs (food, shelter, medication), transportation, and bridged the gap between health care services and community members. In addition, the Promotoras contributed to culturally relevant care in health care systems by helping health care providers understand and address barriers associated with a community's historical and cultural context, including barriers to health care associated with differences in language and culture (Cosgrove et al., 2014).
There are several limitations of this report. First, the prevalence estimates were based on self-reported data and are subject to recall errors or social desirability effects. Nonetheless, we assume that any bias resulting from the methodological limitations did not change considerably across the 3-year period. Second, the REACH project was not a clinical trial and had no formal control groups. We did not find any similar data, at either the local or national level, from the same time period (2009 through 2012) for comparison. Finally, the REACH project did not use a uniform intervention protocol, but was sufficiently flexible to allow community choices based on available resources and local realities. It is difficult to assess the impact of any individual approach.
This study demonstrates the success of a large scale community participatory intervention targeting Hispanic communities outside a controlled research setting. Health disparities can be reduced and the health status of groups most affected by health inequities can be improved through community collaborations, system and environmental interventions, and culturally tailored approaches.
Acknowledgments
Racial and ethnic approaches to community health across the U.S. Risk Factor Survey participating Hispanic communities:
Chicago Department of Health, Chicago, Illinois
Greater Lawrence Family Health Center, Inc., Lawrence, Massachusetts
Institute for Urban Family Health, New York, New York
Southeast Chicago Development Commission, Chicago, Illinois
The Regents of the University of California, Los Angeles, California
University of Illinois at Chicago, Chicago, Illinois
Footnotes
Conflict of interest statement
The authors declare that there are no conflicts of interest.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Balcazar HG, Byrd TL, Ortiz M, Tondapu SR, Chavez M. A randomized community intervention to improve hypertension control among Mexican Americans: using the promotoras de salud community outreach model. J. Health Care Poor Underserved. 2009;20:1079–1094. doi: 10.1353/hpu.0.0209. [DOI] [PubMed] [Google Scholar]
- Calman NS, Golub M, Kitson K, Ruddock C. Electronic health records: the use of technology to eliminate racial disparities in health outcomes. In: Ong K, editor. Medical informatics: An executive primer. 2nd ed Health Information and Management Systems Society; Chicago, IL: 2007. [Google Scholar]
- Castillo SR, Block D, Lohff C, Krauss S. Innovation in the collection of food availability data: a case study of the Chicago Department of Public Health Sanitarian Survey. Prev. Med. 2013;57:70–71. doi: 10.1016/j.ypmed.2013.03.006. [DOI] [PubMed] [Google Scholar]
- Centers for Disease C. Prevention Health disparities experienced by Hispanics—United States. MMWR Morb. Mortal. Wkly Rep. 2004;53:935–937. [PubMed] [Google Scholar]
- Cosgrove S, Moore-Monroy M, Jenkins C, et al. Community health workers as an integral strategy in the REACH U.S. program to eliminate health inequities. Health Promot. Pract. 2014;15:795–802. doi: 10.1177/1524839914541442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golub M, Calman N, Ruddock C, et al. A community mobilizes to end medical apartheid. Prog. Community Health Partnersh. 2011;5:317–325. doi: 10.1353/cpr.2011.0041. [DOI] [PubMed] [Google Scholar]
- Kaplan SA, Ruddock C, Golub M, et al. Stirring up the mud: using a community-based participatory approach to address health disparities through a faith-based initiative. J. Health Care Poor Underserved. 2009;20:1111–1123. doi: 10.1353/hpu.0.0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai LL. Community pharmacy-based hypertension disease-management program in a Latino/Hispanic–American population. Consult. Pharm. 2007;22:411–416. doi: 10.4140/tcp.n.2007.411. [DOI] [PubMed] [Google Scholar]
- Liao Y, Bang D, Cosgrove S, et al. Surveillance of health status in minority communities — racial and ethnic approaches to community health across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. Morb. Mortal. Wkly. Rep. Surveill. Summ. 2011;60:1–44. (Washington, D.C. : 2002) [PubMed] [Google Scholar]
- Liburd LC. REACH U.S. in action: inspiring hope, rewarding courage. Fam. Community Health. 2011;34(Suppl. 1):S2–S6. doi: 10.1097/FCH.0b013e31820af643. [DOI] [PubMed] [Google Scholar]
- Maxwell AE, Yancey AK, AuYoung M, et al. A midpoint process evaluation of the Los Angeles Basin Racial and Ethnic Approaches to Community Health Across the US (REACH US) Disparities Center, 2007–2009. Prev. Chronic Dis. 2011;8:A115. [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, Stroup DF, Giles WH. Public health surveillance for behavioral risk factors in a changing environment. Recommendations from the Behavioral Risk Factor Surveillance Team. MMWR Recomm. Rep. 2003;52:1–12. [PubMed] [Google Scholar]
- Ortman JM, Guarneri CE. United States Population Projections: 2000 to 2050. U.S. Census Bureau; Washington, DC: 2009. [Google Scholar]
- Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn. Dis. 1999;9:10–21. [PubMed] [Google Scholar]
- Rocha-Goldberg Mdel P, Corsino L, Batch B, et al. Hypertension Improvement Project (HIP) Latino: results of a pilot study of lifestyle intervention for lowering blood pressure in Latino adults. Ethn. Health. 2010;15:269–282. doi: 10.1080/13557851003674997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez V, Cacari Stone L, Moffett ML, et al. Process evaluation of a promotora de salud intervention for improving hypertension outcomes for Latinos living in a rural U.S.–Mexico border region. Health Promot. Pract. 2014;15:356–364. doi: 10.1177/1524839913516343. [DOI] [PubMed] [Google Scholar]
- Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch. Intern. Med. 2004;164:2126–2134. doi: 10.1001/archinte.164.19.2126. [DOI] [PubMed] [Google Scholar]
- Yoon SS, Burt V, Louis T, Carroll MD. Hypertension among adults in the United States, 2009–2010. NCHS Data Brief. 2012:1–8. [PubMed] [Google Scholar]