Abstract
The incidence of stroke among younger adults in the United States is increasing. Few studies have investigated the prevalence of depressive symptoms after stroke among different age groups or the extent to which subjective stress at the time of stroke interacts with age to contribute to post-stroke depression. The present study examined whether there exists an age gradient in survivors’ level of depressive symptoms and explored the extent to which financial, family, and health-related stress may also impact on depression. Bivariate analyses (N = 322) indicated significant differences in depression and stress by age group, as well as differences in age and stress by 3-month depression status. Linear regression analyses indicated that survivors between the ages of 25–54 and 55–64 years old had, on average, significantly higher depressive symptom scores. Those with financial, family, and health-related stress at the time of stroke, irrespective of age, also had significantly higher scores.
Keywords: Stroke, Depression, Age, Stress
Introduction
The American Heart Association (AHA) estimates that approximately 6.6 million Americans over the age of 20 years old have had a stroke (Mozaffarian et al., 2015). Stroke can be a devastating disease and one in which psychiatric complications throughout recovery are far too common. Ayerbe et al., (2013) reported that the pooled prevalence of post-stroke depression across 43 studies ranged from 29 to 33 %, depending on the time post-stroke at which symptoms were observed (Ayerbe et al., 2013). This can be compared with a 12-month prevalence rate for major depression in the general United States (US) adult population of approximately 6.7 % (Kessler et al., 2005). In addition to being distressing in and of itself, depression after stroke has been shown to contribute to other adverse outcomes, including lack of engagement in rehabilitation activities, longer hospital stays, poor functional recovery, increased recurrence of stroke, and early mortality (Bartoli et al., 2013; Morris et al., 1993; Naess et al., 2010; Pan et al., 2011; Turner-Stokes & Hassan, 2002; West et al., 2010; Wulsin et al., 2012).
Population-based studies suggest that overall stroke incidence in the US has declined significantly in recent decades (Carandang et al., 2006; Kleindorfer et al., 2010). Combined with what the AHA characterizes as a “striking and more accelerated” (Lackland et al., 2014, p. 315) decrease in stroke mortality in recent years, this trend has led to growing optimism about the intractability of stroke as a top cause of death and disability in the US. However, some research has given rise to questions about whether all individuals, irrespective of age, are represented within these positive trends. For example, Kissela et al. (2012) found that the number of strokes among persons between the ages of 20 and 54 years living in a metropolitan area of 1.3 million actually increased significantly from 227 out of 1942 cases (11.7 %) in 1993 to 393 out of 1916 cases (20.5 %) in 2005 (p = 0.002). Such findings raise the possibility that although efforts to control risk factors for stroke have led to remarkable gains overall, certain vulnerable subpopulations such as younger adults may be in need of additional attention.
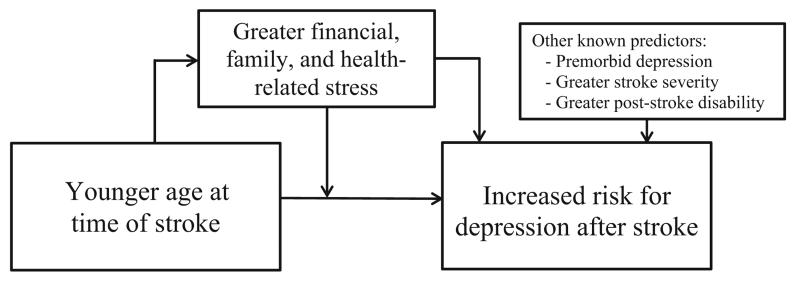
A growing body of literature has focused on the experiences and needs of younger stroke survivors. Although authors note that “a feature of the ‘young adult’ stroke research is the lack of consensus regarding the definition of the term ‘young’” (Lawrence, 2010, p. 241), studies suggest that younger persons, many of whom may be in their peak years for employment and parenting demands, may experience greater stress which may in turn, increase their risk for depression (Fig. 1). For example, in Low et al. (2003) analysis of the unmet needs of 135 survivors aged 18–65 years, 33 % of the sample reported that they needed either “help with finances” and/or “family support,” including assistance with childcare responsibilities (Low et al., 2003). In fact, the need for family support was significantly greater in the lower age range (40 % among 18–45 year olds vs. 20 % among 46–65 year olds, p = 0.02). These findings are supported by other studies with younger individuals and couples coping with stroke (Banks & Pearson, 2004; Roding et al., 2003; Lawrence, 2010; Lawrence & Kinn, 2012). Theoretical work by authors such as Bury (1982) and Rook et al. (1989) about the consequences of experiencing an “off-time” illness (i.e., one that is typically associated with older age) in midlife also raises the possibility that health-related stress may be greater for younger survivors. To date, however, there have been few empirical studies about this topic.
Fig. 1.
Theoretical model linking survivor age and subjective stressors to depression after stroke
Complementing our understanding about potential stressors among younger stroke survivors is a well-developed body of literature about the association between stress and depression in non-chronic illness populations (Kessler, 1997; Mazure, 1998; Ronnlund et al., 2013). Large studies have also documented age differences in rates of depression in the general population and have concluded that younger adults generally experience more depression than their older counterparts. For example, in an analysis of data from the National Comorbidity Survey Replication (NCS-R), Kessler et al. (2010) found a prevalence rate for major depression of between 19.4 and 22.7 % for persons aged 18–64 years, compared with a rate of 9.8 % in those 65 years or older. Interestingly, Kessler et al. (2010) study also found a significantly stronger association between physical disorders and depression in the younger age groups.
Although younger individuals, especially younger stroke survivors, appear to be at higher risk for depression, systematic reviews have not found a uniform relationship between age and incidence of post-stroke depression (Ayerbe et al., 2013; Kouwenhoven et al., 2011; Ouimet et al., 2001). At present, we understand little about the association between age, stress, and depression after onset of a chronic illness such as stroke (Hammen, 2005; Laures-Gore & Defife, 2013). As Ouimet et al. (2001) suggest, the influence of subjective stress on individuals’ developmental experiences with stroke may be one critical missing piece of the puzzle of explaining the exceedingly high prevalence of depression in the stroke population.
At present, the field of stroke recovery is not sufficiently advanced to return all patients back to full health. Although most survivors are offered interventions for improving motor function, less often do they receive assistance with other important matters of reintegration into their post-stroke life that can, if not addressed, become significant stressors. If younger persons and those who experience particular stressors do, in fact, experience higher levels of depression, this would be a significant problem from the perspective of these individuals, as well as their spouses, children, and other family members with whom they interact. This would also be a problem from the standpoint of the healthcare system as the onset of depression at a younger age contributes to increased illness burden, more years of lost or reduced productivity, and greater cumulative care-related costs (Berndt et al., 2000; Goetzel et al., 2003; Kessler et al., 2010; Zisook et al., 2007). In order to provide optimal rehabilitation services, we need to gain a clearer understanding about the dynamic intersection of age, subjective stress, and depression after stroke.
The present study represents a preliminary attempt to determine whether there exists an age gradient in stroke survivors’ level of depressive symptoms and to examine the extent to which financial, family, and health-related stress at the time of stroke impacts on depression. Our first hypothesis was that younger persons would experience significantly higher depressive symptoms after stroke, controlling for other known predictors such as history of depression, greater stroke severity, and greater degree of post stroke disability (Hackett & Anderson, 2005). Our second hypothesis was that baseline financial, family, and health-related stress would be additional independent predictors of depressive symptoms after stroke. Our third hypothesis was that stress would moderate the association between age and depressive symptoms, with younger survivors who report higher stress experiencing the highest level of symptoms.
Methods
Participants and procedure
In 2005, the population-based greater cincinnati/northern kentucky stroke study prospectively enrolled a cohort of 460 ischemic stroke patients from 15 participating hospitals in the study area. Interviews were conducted at base-line (M = 5.07 days from stroke onset) and at 3 months post stroke by study nurses. For 78 patients (24.2 %), at least a portion of the baseline interview was completed by proxy due to the patient being unresponsive, unable to provide reliable information, aphasic, or confused. The same nurse who conducted the baseline interview for a given participant also conducted the 3-month interview. At 3 months post stroke, among the 460 patients enrolled, 33 had died, 35 were unavailable for interview, and 70 provided reduced interviews that did not include the depression outcome measure. The sample for the present study therefore includes 322 survivors for whom 3-month follow-up data on depression were available. Overall, 267 patients (82.9 %) were living at home at the time of the 3-month interview. All study activities were approved by the Institutional Review Board at all participating institutions.
Measures
Outcome variable
Depressive symptomatology was measured at the 3-month follow-up with the 10-item Center for Epidemiological Studies Depression (CESD-10) scale (Andresen et al.,1994; Irwin et al., 1999). Patients were asked to respond about how often they had experienced each symptom of depression in the past week, from rarely or none of the time (0) to most or all of the time (3). Thus, total scores for the CESD-10 range from 0 to 30, with higher scores representing higher states of depression. Consistent with previous studies, including studies by the current research team, survivors were considered to be at risk for clinical depression if their CESD-10 score was greater than or equal to 10 (Andresen et al., 1994; Shrout & Yager, 1989; Whooley et al., 1997; Wulsin et al., 2012).
Predictor variables
Demographic variables at baseline, including sex, race, marital status, level of education, employment status, and age, were determined by self-report. History of depression was based upon a formal diagnosis of depression found in patient medical records. Stroke severity was determined by patient scores on the National Institutes of Health Stroke Scale (Brott et al., 1989) which were estimated retrospectively (rNIHSS; Williams et al., 2000) from patient medical records. Scores for the rNIHSS range from 0 to 42, with a higher score representing a more severe stroke. Degree of disability prior to and immediately post-stroke was measured with the Modified Rankin Scale (mRS; de Haan et al., 1995). With the exception of 6 (“dead”), the mRS ranges from 0 (“No symptoms at all”) to 5 (“Severe disability; bedridden, incontinent and requiring constant nursing care and attention”).
Subjective financial, family, and health-related stress were measured at baseline with three individual items: (1) “Do you regularly have trouble paying your monthly bills?”; (2) “In the week prior to your stroke, how much stress did you feel with regard to family?”; and (3) “In the week prior to your stroke, how much stress did you feel with regard to health?”. Question 1 required a “yes” or “no” response, and questions 2 and 3 were measured on a semantic-differential scale of 1 (no stress) to 10 (highest level of stress possible).
Analysis
Survivors were categorized into four age groups according to the groupings used by Kissela et al. (2012; i.e., 25–54, 55–64, 65–74, and ≥75 years old) in their study that reported an increase in stroke incidence among younger persons. These groups reflected our interest in stress and depression at different broad stages of life (e.g., survivors who are working vs. not working, with dependent children vs. not, “young and healthy” vs. having some experience with previous serious illness) and were also statistically pragmatic. Only six participants were between the ages of 25 (our youngest participant) and 34 years, and 16 participants were between the ages of 35 and 44 years. Combining those 22 participants with the 42 participants who were between the ages of 45 and 55 years into a single group allowed us to have sufficient statistical power to detect differences among age groups across a variety of variables.
Demographics, clinical characteristics, and subjective financial stress at baseline were compared among the four age groups using the Chi square test for categorical variables (sex, race, marital status, education, employment, history of depression, and trouble paying bills) and the Kruskal–Wallis test for continuous variables (rNIHSS, mRS, and family- and health-related stress). Unadjusted proportions of patients at risk for depression at 3-month follow-up were compared among the four age groups using the Chi square test. Similarly, demographics, clinical characteristics, and baseline financial stress were compared between survivors at risk for depression at 3 months versus not using the Chi square test for categorical variables and the Wilcoxon rank sum test for continuous variables.
Linear regression, with 3-month follow-up CESD-10 scores as the dependent variable, was used to identify potential predictors of depressive symptomatology, including sex (with male as the reference group), race (with African-American as the reference group), marital status (with “married or living with partner” as the reference group), education (with “at least high school graduation” as the reference group), history of depression (with no history as the reference group), stroke severity (continuous), degree of post-stroke disability (continuous), and categorical age (with ≥75 as the reference group). The effects of the three subjective stress variables at baseline were considered in separate models, as potential modifiers of the effect of age on outcome. For each model, interaction between the age categories and the subjective stress variable was evaluated.
Results
Characteristics of the study sample of 322 ischemic stroke survivors, stratified by age group, are presented in Table 1. Overall, 13 % of the study sample had experienced depression before stroke, with no significant differences among age groups. However, at 3-months post-stroke, 37 % overall were considered at risk for clinical depression, with significantly higher rates among those in the age groups under 65 years (p = 0.02). Overall, 22 % of the sample reported having trouble paying bills regularly at baseline, with a significantly larger proportion in the younger age groups (p < 0.01). Survivors in the 25–54 year age group reported significantly higher family stress at baseline compared with other age groups (p < 0.01). Significant differences by age were also found on the variables of sex, race, marital status, employment status, and pre- and post-stroke mRS.
Table 1.
Characteristics of the study sample by age group
| Overall (N = 322) | Age group |
p | ||||
|---|---|---|---|---|---|---|
| 25–54 (n = 64) | 55–64 (n = 80) | 65–74 (n = 75) | 75+ (n = 103) | |||
| Sex (female), n (%) | 153 (48 %) | 29 (45 %) | 33 (41 %) | 28 (37 %) | 63 (61 %) | <0.01 |
| Race, n (%) | <0.01 | |||||
| African-American | 80 (25 %) | 26 (41 %) | 22 (27 %) | 19 (25 %) | 13 (13 %) | |
| White/other | 242 (75 %) | 38 (59 %) | 58 (72 %) | 56 (75 %) | 90 (87 %) | |
| Marital status, n (%) | <0.01 | |||||
| Married or living with partner | 166 (52 %) | 31 (48 %) | 49 (61 %) | 46 (61 %) | 40 (39 %) | |
| Single, widowed, divorced, separated | 156 (48 %) | 33 (52 %) | 31 (39 %) | 29 (39 %) | 63 (61 %) | |
| Education, n (%) | 0.26 | |||||
| <High school graduation | 100 (31 %) | 17 (27 %) | 20 (25 %) | 25 (33 %) | 38 (37 %) | |
| ≥High school graduation | 221 (69 %) | 47 (73 %) | 60 (75 %) | 50 (67 %) | 64 (63 %) | |
| Employment status, n (%) | <0.01 | |||||
| Employed | 96 (30 %) | 41 (64 %) | 39 (49 %) | 12 (16 %) | 4 (4 %) | |
| Not employed, retired, disability/sick leave | 226 (70 %) | 23 (36 %) | 41 (51 %) | 63 (84 %) | 99 (96 %) | |
| History of depression (yes), n (%) | 43 (13 %) | 10 (16 %) | 9 (11 %) | 7 (9 %) | 17 (16 %) | 0.47 |
| rNIHSS (median, 25th, 75th ‰) | 4 (2, 7) | 3 (2, 6) | 4 (2.5, 7) | 4 (2, 8) | 4 (2, 7) | 0.37 |
| Pre-stroke mRS, n (%) | <0.01 | |||||
| 0–1 | 207 (64 %) | 51 (80 %) | 63 (79 %) | 48 (64 %) | 45 (44 %) | |
| ≥2 | 115 (36 %) | 13 (20 %) | 17 (21 %) | 27 (36 %) | 58 (56 %) | |
| Post-stroke mRS, n (%) | <0.01 | |||||
| 0–1 | 46 (14 %) | 18 (28 %) | 15 (19 %) | 7 (9 %) | 6 (6 %) | |
| ≥2 | 276 (86 %) | 46 (72 %) | 65 (81 %) | 68 (91 %) | 97 (94 %) | |
| At risk for depression at 3 months (yes), n (%) | 120 (37 %) | 30 (47 %) | 37 (46 %) | 20 (27 %) | 33 (32 %) | 0.02 |
| Trouble paying bills (yes), n (%) | 71 (22 %) | 25 (39 %) | 26 (32 %) | 10 (13 %) | 10 (10 %) | <0.01 |
| Family stress (median, 25th, 75th ‰) | 2 (1, 6) | 4.5 (2, 8) | 2 (1, 7) | 2 (1, 5) | 1 (1, 5) | <0.01 |
| Health stress (median, 25th, 75th ‰) | 3 (1, 5) | 3 (1, 6) | 3 (1, 6) | 2 (1, 5) | 2(1, 5) | 0.47 |
At risk for depression at 3 months defined as CESD score ≥ 10. P values for differences between age categories based on Chi square test for categorical variables and Kruskal–Wallis test for continuous variables. All variables measured at baseline, except for 3-month clinical depression. “Other” race includes one Asian, one Hispanic, and one American Indian/Alaskan native
rNIHSS retrospective National Institutes of Health Stroke Scale, mRS modified Rankin Scale
Bivariate associations between potential predictor variables and depression risk at 3 months are presented in Table 2. The median age of participants at risk for depression was significantly lower than those who were not (p = 0.02), and the age category proportions differed between depression status groups (p = 0.02). A significantly higher proportion of survivors who were at risk for depression indicated having trouble paying bills at the time of stroke, compared with those who were not at risk (p < 0.01). Similarly, the median family stress scores were significantly higher for those who were at risk for depression (p < 0.01), as were the median health stress scores (p < 0.01). Significant differences by depression status were also found on the variables of depression history and pre- and post-stroke mRS.
Table 2.
Characteristics of the study sample by 3-month depression risk status
| 3-Month depression risk |
|||
|---|---|---|---|
| Yes (n = 120) | No (n = 202) | p | |
| Age (median, 25th, 75th ‰) | 62 (54, 75.5) | 69 (58, 78) | 0.02 |
| Age categories, n (%) | 0.02 | ||
| 25–54 | 30 (25 %) | 34 (17 %) | |
| 55–64 | 37 (31 %) | 43 (21 %) | |
| 65–74 | 20 (17 %) | 55 (27 %) | |
| 75+ | 33 (27 %) | 70 (35 %) | |
| Sex (female), n (%) | 64 (53 %) | 89 (44 %) | 0.11 |
| Race, n (%) | 0.75 | ||
| African-American | 31 (26 %) | 49 (24 %) | |
| White/other | 89 (74 %) | 153 (76 %) | |
| Marital status, n (%) | 0.07 | ||
| Married or living with partner | 54 (45 %) | 112 (55 %) | |
| Single, widowed, divorced, separated | 66 (55 %) | 90 (45 %) | |
| Education, n (%) | 0.06 | ||
| <High school graduation | 45 (37 %) | 55 (27 %) | |
| ≥High school graduation | 75 (62 %) | 146 (73 %) | |
| Employment status, n (%) | 0.96 | ||
| Employed | 36 (30 %) | 60 (30 %) | |
| Not employed, retired, disability/sick leave | 84 (70 %) | 142 (70 %) | |
| Hx of depression (yes), n (%) | 25 (21 %) | 18 (9 %) | < 0.01 |
| rNIHSS (median, 25th, 75th ‰) | 4 (2, 8) | 4 (2, 7) | 0.29 |
| Pre-stroke mRS, n (%) | 0.03 | ||
| 0–1 | 68 (57 %) | 139 (69 %) | |
| ≥2 | 52 (43 %) | 63 (31 %) | |
| Post-stroke mRS, n (%) | 0.04 | ||
| 0–1 | 11 (9 %) | 35 (17 %) | |
| ≥2 | 109 (91 %) | 167 (83 %) | |
| Trouble paying bills (yes), n (%) | 39 (32 %) | 32 (16 %) | < 0.01 |
| Family stress (median, 25th, 75th ‰) | 5 (1, 8) | 1 (1, 5) | < 0.01 |
| Health stress (median, 25th, 75th ‰) | 4 (1, 7) | 2 (1, 5) | < 0.01 |
3-month depression risk defined as CESD score ≥ 10. P-values for differences in 3-month depression groups based on Chi square test for categorical variables and Wilcox on rank sum test for continuous variables
rNIHSS retrospective National Institutes of Health Stroke Scale, mRS modified Rankin Scale
Table 3 presents the results of the linear regression analyses. Results indicated that survivors in the 25–54 age group, on average, had higher depressive symptom scores at 3 months post stroke than those in the 75 + group (B = 3.84, 95 % CI [1.90, 5.79]; p < 0.01) after controlling for the other relevant variables, as did those in the 55–64 age group (B = 3.41, 95 % CI [1.62, 5.21]; p < 0.01). Adjusting for age, survivors who reported having “trouble paying bills” at baseline had higher depression scores at 3 months than those who did not (B = 1.80, 95 % CI [0.71, 1.94]; p = 0.03). Family and health-related stress at baseline were also associated with higher depression scores at 3 months (B = 0.40, 95 % CI [0.16, 0.56]; p < 0.01 and B = 0.44, 95 % CI [0.21, 0.67]; p < 0.01). No statistically significant interactions between age and subjective stress were found. Supplementary logistic regression models (i.e., with age treated as a categorical and a continuous predictor of dichotomous depression status at 3 months) were run with results from each analysis confirming the results of the linear regression.
Table 3.
Results of linear regression predicting CESD scores (N = 322)
| Est (95 % CI) | p | R2 | |
|---|---|---|---|
| Sex (female) | 0.50 (−0.88, 1.88) | 0.48 | |
| Race (white/other) | 0.29 (−1.27, 1.85) | 0.71 | |
| Marital status (single/widowed/divorced/separated) | 1.00 (−0.39, 2.39) | 0.16 | |
| Education (<high school) | 0.97 (−0.42, 2.37) | 0.17 | |
| History of depression (yes) | 4.13 (2.22, 6.04) | <0.01 | |
| rNIHSS | 0.14 (−0.01, 0.29) | 0.07 | |
| Post-stroke mRS | 1.30 (0.68, 1.93) | <0.01 | |
| Age | |||
| 25–54 | 3.84 (1.90, 5.79) | <0.01 | |
| 55–64 | 3.41 (1.62, 5.21) | <0.01 | |
| 65–74 | 0.06 (−1.75, 1.87) | 0.95 | |
| 75+ | Reference group | - | 0.20 |
| Trouble paying bills (yes) | 1.80 (0.71, 1.94) | 0.03 | 0.21 |
| Family stress | 0.40 (0.16, 0.56) | <0.01 | 0.23 |
| Health-related stress | 0.44 (0.21, 0.67) | <0.01 | 0.24 |
Stress variables were evaluated in separate models in which each stress variable was added to the base model of sex, race, marital status, education, history of depression, baseline NIHSS, mRS, and categorical age
rNIHSS retrospective National Institutes of Health Stroke Scale, mRS modified Rankin Scale
Discussion
The present study investigated three related hypotheses about the association among age, subjective stress, and depression in survivors of ischemic stroke. Regarding our first hypothesis that younger stroke survivors would experience greater depressive symptomatology, we found that those in the 25–54 age group and those in the 55–64 age group experienced significantly higher levels of depressive symptoms. These findings are in accordance with certain studies in stroke (e.g., Paradiso & Robinson, 1998; Robinson et al., 1983), although they appear to disconfirm others, including multivariable analyses in which age had no effect (e.g., Aström et al., 1993; Berg et al., 2003; Fure et al., 2006; Pohjasvaara et al., 1998).
One reason for the mixed findings in existing literature may be the coarse, often dichotomous treatment of age as an independent variable in models predicting depression (e.g., using a median split to define two groups; Aström et al., 1993). Another reason may be that some study samples are restricted, either intentionally or unintentionally, in terms of age (e.g.,<70 years old, Berg et al., 2003), thereby limiting the variability of age and its potential as a predictive factor. Unlike the present study, which sought to determine age-group-specific levels of symptoms, other studies have conceptualized the association between age and depression as a continuous relationship in which, as a survivor’s age increases or decreases by 1 year, his or her risk for depression or severity of depressive symptoms increases or decreases proportionally (e.g., Taylor-Piliae et al., 2013). This linear approach may lead to erroneous conclusions about the lack of association between age and depression in this population. In fact, the pattern of depression prevalence among the four age groups in our study raises the possibility of a curvilinear effect in which one’s risk for depression may be the greatest between the ages of 25 and 54, subside through the remainder of midlife and into early old age, and then increase again in later old age. Future studies should investigate such a curvilinear relationship, as has been found in depression studies with otherwise healthy populations as well as those experiencing unanticipated health-related events (Carlson, 2011; Mirowsky & Kim, 2004; Tuohy et al., 2005). Studies should also examine more closely the types of depressive symptoms (i.e., cognitive, affective, somatic) experienced by stroke survivors across the lifespan, as research suggests that the nature of symptoms may vary by age (Goldberg et al., 2003).
Regarding our second hypothesis that baseline financial, family, and health-related stress would be additional predictors of depressive symptoms after stroke, we found dramatically higher rates of each stressor among those who were at risk for clinical depression at 3 months (i.e., CESD score ≥10) versus those who were not. The linear model indicated that while each subjective stressor exerted significant independent influence on survivor depressive symptoms, financial stress had the most pronounced effect. This finding supports the limited amount of research about subjective stress and depression in the context of a chronic illness including a small study in multiple sclerosis (N = 22) in which subjective stress at “Time 1” (M = 4.7 years after diagnosis) was strongly correlated with depressive symptoms 6 months later (Aikens et al., 1997).
Our findings also support what we understand about the association between stressors such as economic poverty and depression in otherwise healthy populations (Wittayanukorn et al., 2014). Moreover, our study adds significantly to existing knowledge by prospectively assessing the impact of specific subjective stressors immediately after diagnosis. Additional research examining how, for example, the perception of financial stress might be different than objective poverty (e.g., ratio of household income to family size, which is often difficult to obtain with a high degree of accuracy, especially among persons with cognitive impairment) would be extremely valuable. It may be that, in terms of one’s risk for depression, the perception of financial stress is a simple but adequate indicator of socioeconomic struggle.
We also found associations between family- and health-related stress at baseline and depressive symptoms 3 months later. These findings are consistent with the small body of qualitative research that currently exists, as well as the more extensive body of sociological theory, about the struggles experienced by younger stroke survivors and persons who are experiencing an illness that they perceive to be “off-time” with their age, life stage, or their expected life course (Bury, 1982; Lawrence, 2010; McCarthy & Bauer, 2015; Rook, Catalano & Dooley, 1989). The critical contribution of this study is that it quantifies the impact of each specific stressor.
Regarding our third hypothesis that younger survivors who reported higher subjective stress would experience the highest level of depressive symptoms, we did not find a significant interaction, thereby suggesting that younger age may not amplify the negative effects of financial, family, and health-related stress. However, we did find very different rates of subjective stress between survivors at each end of the age spectrum (e.g., 39 % of survivors aged 25–54 with financial stress versus 10 % aged 75+), as well as dramatically different rates of each stressor between survivors at risk for depression at 3 months versus not. The lack of a significant interaction between age and subjective stress in the linear models may have been due to the poor sensitivity of our single-item indicators or our inability to control for other known correlates of stress and depressive symptoms. As some research suggests, age-related differences in rates of depression may also be more attributable to biological mechanisms than psychosocial mechanisms such as subjective stress (Fang & Cheng, 2009).
Taken in their entirety, findings from this study add to what we understand about levels of depressive symptoms among stroke survivors from different age groups and how subjective stress factors into this experience. In addition to being informative for future research on these topics, the present study could also inform interpretation of findings from clinical trials that promote prophylactic treatment with antidepressant medication for aiding stroke survivor physical and psychiatric recovery (Chollet et al., 2011; Niedermaier et al., 2004). With the potential for serious adverse side effects from many antidepressant medications, it is critical that prescribers be aware of which patient groups may actually require such treatments versus, for example, a watchful waiting approach.
Several limitations must be mentioned. First, the hypotheses for this study are based on the assumption that chronological age can be a reliable indicator of financial, family, and health-related stress after stroke. Although data from this and other studies support this assumption, it would be erroneous to conclude that all younger survivors experience the same age-related challenges and that these challenges inevitably lead to greater stress. Second, basing our outcome variable on self-reported depressive symptoms using the CES-D is less than optimal. Although the CES-D has performed well in studies with chronic illness populations, using a “gold standard” such as the clinician-rated Quick Inventory of Depressive Symptomatology (QIDS) for the determination of clinical depression is recommended (Rush et al., 2003). Similarly, basing our assessment of pre-stroke depression on retrospective chart review could reflect a conservative estimation of the extent of pre-stroke depression in this sample. Although we did require a formal diagnosis, the potential for underestimation raises the possibility that the dramatic change we found in pre versus post-stroke depression (i.e., 13 % pre vs. 37 % post) could be inflated and should therefore be interpreted with caution. Measuring financial, family, and health-related stress with single items is also potentially problematic for drawing firm conclusions about the association between survivor age, subjective stressors, and depression, as is our reliance on proxy reports of these measures for a portion of the sample. However, given the lack of literature available on this topic and the large magnitude of effects we found, the present study serves as a good starting point for further investigation of these issues. Additional studies are needed that are specifically designed to measure these concepts in greater depth and with more precision. Finally, it is possible that all confounding factors may not have been controlled for in our models. However, we did control for known predictors such as history of depression, stroke severity, and post-stroke disability.
This study calls attention to the fact that younger persons and those experiencing financial, family, and health-related stress, may experience higher levels of depressive symptoms after stroke. These findings are particularly meaningful given the evidence that stroke, as well as the aftermath of stoke, is becoming increasingly prevalent among younger adults.
Acknowledgments
This research was supported by funding from the National Institute on Neurological Disorders and Stroke [PI Kissela, Grant No R01NS030678-20].
Footnotes
Compliance with ethical standards
Conflict of interest Michael J. McCarthy, Heidi J. Sucharew, Kathleen Alwell, Charles J. Moomaw, Daniel Woo, Matthew L. Flaherty, Pooja Khatri, Simona Ferioli, Opeolu Adeoye, Dawn O Kleindorfer and Brett M Kissela declare that they have no conflict of interest.
Human and animal rights and Informed consent All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.
References
- Aikens JE, Fischer JS, Namey M, Rudick RA. A replicated prospective investigation of life stress, coping, and depressive symptoms in multiple sclerosis. Journal of Behavioral Medicine. 1997;20:433–445. doi: 10.1023/a:1025547431847. doi:10.1023/A:1025547431847. [DOI] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine. 1994;10:77–84. [PubMed] [Google Scholar]
- Aström M, Adolfsson R, Asplund K. Major depression in stroke patients. A 3-year longitudinal study. Stroke; a Journal of Cerebral Circulation. 1993;24:976–982. doi: 10.1161/01.str.24.7.976. doi:10.1161/01.STR.24.7.976. [DOI] [PubMed] [Google Scholar]
- Ayerbe L, Ayis S, Wolfe C, Rudd A. Natural history, predictors and outcomes of depression after stroke: Systematic review and meta-analysis. British Journal of Psychiatry. 2013;202:14–21. doi: 10.1192/bjp.bp.111.107664. [DOI] [PubMed] [Google Scholar]
- Banks P, Pearson C. Parallel lives: Younger stroke survivors and their partners coping with crisis. Sexual and Relationship Therapy. 2004;19:413–429. doi:10.1080/14681990412331298009. [Google Scholar]
- Bartoli F, Lillia N, Lax A, Crocamo C, Mantero V, Carrà G, Clerici M. Depression after stroke and risk of mortality: A systematic review and meta-analysis. Stroke Research and Treatment. 2013;2013:862978. doi: 10.1155/2013/862978. doi:10.1155/2013/862978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg A, Palomäki H, Lehtihalmes M, Lönnqvist J, Kaste M. Poststroke depression: An 18-month follow-up. Stroke. 2003;34:138–143. doi: 10.1161/01.str.0000048149.84268.07. doi:10.1161/01.STR.0000048149.84268.07. [DOI] [PubMed] [Google Scholar]
- Berndt ER, Koran LM, Finkelstein SN, Gelenberg AJ, Keller MB. Lost human capital from early-onset chronic depression. The American Journal of Psychiatry. 2000;157:940–947. doi: 10.1176/appi.ajp.157.6.940. [DOI] [PubMed] [Google Scholar]
- Brott T, Hertzberg V, Adams J, Olinger CP, Marler JR, Barsan WG, Eberle R. Measurements of acute cerebral infarction: A clinical examination scale. Stroke. 1989;20:864–870. doi: 10.1161/01.str.20.7.864. doi:10.1161/01.STR.20.7.864. [DOI] [PubMed] [Google Scholar]
- Bury M. Chronic illness as biographical disruption. Sociology of Health & Illness. 1982;4:167–182. doi: 10.1111/1467-9566.ep11339939. doi:10.1111/1467-9566.ep11339939. [DOI] [PubMed] [Google Scholar]
- Carandang R, Seshadri S, Beiser A, Kelly-Hayes M, et al. Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. Journal of the American Medical Association. 2006;296:2939–2946. doi: 10.1001/jama.296.24.2939. [DOI] [PubMed] [Google Scholar]
- Carlson DL. Explaining the curvilinear relationship between age at first birth and depression among women. Social Science and Medicine. 2011;72:494–503. doi: 10.1016/j.socscimed.2010.12.001. doi:10.1016/j.socscimed.2010.12.001. [DOI] [PubMed] [Google Scholar]
- Chollet F, Niclot P, Guillon B, Moulin T, Marque P, Pariente J, Jaillard A. Fluoxetine for motor recovery after acute ischaemic stroke (FLAME): A randomised placebo-controlled trial. Lancet Neurology. 2011;10:123–130. doi: 10.1016/S1474-4422(10)70314-8. doi:10.1016/S1474-4422(10)70314-8. [DOI] [PubMed] [Google Scholar]
- de Haan R, Limburg M, Bossuyt P, van der Meulen J, Aaronson N. The clinical meaning of rankin ‘handicap’ grades after stroke. Stroke. 1995;26:2027–2030. doi: 10.1161/01.str.26.11.2027. doi:10.1161/01.STR. 26.11.2027. [DOI] [PubMed] [Google Scholar]
- Fang J, Cheng Q. Etiological mechanisms of post-stroke depression: A review. Neurological Research. 2009;31:904–909. doi: 10.1179/174313209X385752. doi:10.1179/174313209X385752. [DOI] [PubMed] [Google Scholar]
- Fure B, Wyller TB, Engedal K, Thommessen B. Emotional symptoms in acute ischemic stroke. International Journal of Geriatric Psychiatry. 2006;21:382–387. doi: 10.1002/gps.1482. [DOI] [PubMed] [Google Scholar]
- Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S. The health and productivity cost burden of the “Top 10” physical and mental health conditions affecting six large U.S. employers in 1999. Journal of Occupational and Environmental Medicine. 2003;45:5–14. doi: 10.1097/00043764-200301000-00007. doi:10.1097/00043764-200301000-00007. [DOI] [PubMed] [Google Scholar]
- Goldberg JH, Breckenridge JN, Sheikh JI. Age differences in symptoms of depression and anxiety: Examining behavioral medicine outpatients. Journal of Behavioral Medicine. 2003;26:119–132. doi: 10.1023/a:1023030605390. doi:10.1023/A:1023030605390. [DOI] [PubMed] [Google Scholar]
- Hackett ML, Anderson CS. Predictors of depression after stroke: A systematic review of observational studies. Stroke. 2005;36:2296–2301. doi: 10.1161/01.STR.0000183622.75135.a4. doi:10.1161/01.STR.0000183622.75135.a4. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. doi:10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: Criterion validity of the 10-item center for epidemiological studies depression scale (CES-D) Archives of Internal Medicine. 1999;159:1701–1704. doi: 10.1001/archinte.159.15.1701. doi:10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The effects of stressful life events on depression. Annual Review of Psychology. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Birnbaum H, Bromet E, Hwang I, Sampson N, Shahly V. Age differences in major depression: results from the National Comorbidity Survey Replication (NCS-R) Psychological Medicine. 2010;40:225–237. doi: 10.1017/S0033291709990213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. doi:10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kissela BM, Khoury JC, Alwell K, Moomaw CJ, Woo D, Adeoye O, Kleindorfer DO. Age at stroke: Temporal trends in stroke incidence in a large, biracial population. Neurology. 2012;79:1781–1787. doi: 10.1212/WNL.0b013e318270401d. doi:10.1212/WNL.0b013e318270401d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleindorfer DO, Khoury J, Moomaw CJ, Alwell K, Woo D, Flaherty ML, Kissela BM. Stroke incidence is decreasing in whites but not in blacks: A population-based estimate of temporal trends in stroke incidence from the greater cincinnati/northern kentucky stroke study. Stroke; a Journal of Cerebral Circulation. 2010;41:1326–1331. doi: 10.1161/STROKEAHA.109.575043. doi:10.1161/STROKEAHA.109.575043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouwenhoven SE, Kirkevold M, Engedal K, Kim HS. Depression in acute stroke: Prevalence, dominant symptoms and associated factors. A systematic literature review. Disability and Rehabilitation. 2011;33:539–556. doi: 10.3109/09638288.2010.505997. [DOI] [PubMed] [Google Scholar]
- Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, Towfighi A. Factors influencing the decline in stroke mortality: A statement from the American heart association/american stroke association. Stroke. 2014;45:315–353. doi: 10.1161/01.str.0000437068.30550.cf. doi:10.1161/01.str.0000437068.30550.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laures-Gore JS, DeFife LC. Perceived stress and depression in left and right hemisphere post-stroke patients. Neuropsychological Rehabilitation. 2013;23:783–797. doi: 10.1080/09602011.2013.811087. doi:10.1080/09602011.2013.811087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence M. Young adults’ experience of stroke: A qualitative review of the literature. British Journal of Nursing (Mark Allen Publishing) 2010;19:241–248. doi: 10.12968/bjon.2010.19.4.46787. [DOI] [PubMed] [Google Scholar]
- Lawrence M, Kinn S. Determining the needs, priorities, and desired rehabilitation outcomes of young adults who have had a stroke. Rehabilitation Research and Practice. 2012 doi: 10.1155/2012/963978. doi:10.1155/2012/963978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low JTS, Kersten P, Ashburn A, George S, McLellan DL. A study to evaluate the met and unmet needs of members belonging to young stroke groups affiliated with the Stroke Association. Disability and Rehabilitation. 2003;25:1052–1056. doi: 10.1080/0963828031000069753. [DOI] [PubMed] [Google Scholar]
- Mazure CM. Life stressors as risk factors in depression. Clinical Psychology: Science and Practice. 1998;5:291–313. [Google Scholar]
- McCarthy MJ, Bauer EA. In sickness and in health: Couples coping with stroke across the lifespan. Health and Social Work. 2015;40(3) Retrieved from http://hsw.oxfordjournals.org/content/early/2015/06/07/hsw.hlv043.full. [Google Scholar]
- Mirowsky J, Kim J. Age trajectories of depression: Growth-curve vectors, synthetic cohorts, and cross-sectional profiles; Paper presented at the annual meeting of the American Sociological Association; San Francisco, CA. 08-14-2004.2004. [Google Scholar]
- Morris PL, Robinson RG, Andrzejewski P, Samuels J, Price TR. Association of depression with 10-year poststroke mortality. The American Journal of Psychiatry. 1993;150:124–129. doi: 10.1176/ajp.150.1.124. [DOI] [PubMed] [Google Scholar]
- Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Turner MB. Heart disease and stroke statistics—2015 Update: A report from the American Heart Association. Circulation. 2015 doi: 10.1161/CIR.0000000000000152. doi:10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- Naess H, Lunde L, Brogger J, Waje-Andreassen U. Depression predicts unfavourable functional outcome and higher mortality in stroke patients: The Bergen stroke study: Depression and stroke. Acta Neurologica Scandinavica. 2010;122:34–38. doi: 10.1111/j.1600-0404.2010.01373.x. doi:10.1111/j.1600-0404.2010.01373.x. [DOI] [PubMed] [Google Scholar]
- Niedermaier N, Bohrer E, Schulte K, Schlattmann P, Heuser I. Prevention and treatment of poststroke depression with mirtazapine in patients with acute stroke. The Journal of Clinical Psychiatry. 2004;65:1619–1623. doi: 10.4088/jcp.v65n1206. doi:10.4088/JCP.v65n1206. [DOI] [PubMed] [Google Scholar]
- Ouimet MA, Primeau F, Cole MG. Psychosocial risk factors in poststroke depression: A systematic review. Canadian Journal of Psychiatry. 2001;46:819–828. doi: 10.1177/070674370104600905. [DOI] [PubMed] [Google Scholar]
- Pan A, Okereke OI, Sun Q, Logroscino G, Manson JE, Willett WC, Rexrode KM. Depression and incident stroke in women. Stroke. 2011;42:2770–2775. doi: 10.1161/STROKEAHA.111.617043. doi:10.1161/STROKEAHA.111.617043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradiso S, Robinson R. Gender differences in poststroke depression. The Journal of Neuropsychiatry and Clinical Neurosciences. 1998;10:41–47. doi: 10.1176/jnp.10.1.41. [DOI] [PubMed] [Google Scholar]
- Pohjasvaara T, Leppävuori A, Siira I, Vataja R, Kaste M, Erkinjuntti T. Frequency and clinical determinants of poststroke depression. Stroke. 1998;29:2311–2317. doi: 10.1161/01.str.29.11.2311. doi:10.1161/01.STR.29.11.2311. [DOI] [PubMed] [Google Scholar]
- Robinson RG, Starr LB, Kubos KL, Price TR. A two-year longitudinal study of post-stroke mood disorders: Findings during the initial evaluation. Stroke. 1983;14:736–741. doi: 10.1161/01.str.14.5.736. doi:10.1161/01.STR.14.5.736. [DOI] [PubMed] [Google Scholar]
- Roding J, Lindstrom B, Malm J, Ohman A. Frustrated and invisible: Young stroke patients’ experiences of the rehabilitation process. Disability and Rehabilitation. 2003;25:867–874. doi: 10.1080/0963828031000122276. [DOI] [PubMed] [Google Scholar]
- Ronnlund M, Sundstrom A, Sorman DE, Nilsson L. Effects of perceived long-term stress on subjective and objective aspects of memory and cognitive functioning in a middle-aged population-based sample. Journal of Genetic Psychology. 2013;174:25–41. doi: 10.1080/00221325.2011.635725. [DOI] [PubMed] [Google Scholar]
- Rook KS, Catalano R, Dooley D. The timing of major life events: Effects of departing from the social clock. American Journal of Community Psychology. 1989;17:233–258. doi: 10.1007/BF00931009. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Keller MB. The 16-item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry. 2003;54:573–583. doi: 10.1016/s0006-3223(02)01866-8. doi:10.1016/S0006-3223(02)0 1866-8. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Yager TJ. Reliability and validity of screening scales: Effect of reducing scale length. Journal of Clinical Epidemiology. 1989;42:69–78. doi: 10.1016/0895-4356(89)90027-9. doi:10.1016/0895-4356(89)90027-9. [DOI] [PubMed] [Google Scholar]
- Taylor-Piliae RE, Hepworth JT, Coull BM. Predictors of depressive symptoms among community-dwelling stroke survivors. Journal of Cardiovascular Nursing. 2013;28:460–467. doi: 10.1097/JCN.0b013e318258ad57. [DOI] [PubMed] [Google Scholar]
- Tuohy A, Knussen C, Wrennall MJ. Effects of age on symptoms of anxiety and depression in a sample of retired police officers. Psychology and Aging. 2005;20:202–210. doi: 10.1037/0882-7974.20.2.202. doi:10.1037/0882-7974.20.2.202. [DOI] [PubMed] [Google Scholar]
- Turner-Stokes L, Hassan N. Depression after stroke: A review of the evidence base to inform the development of an integrated care pathway. Part 1: Diagnosis, frequency and impact. Clinical Rehabilitation. 2002;16:231–247. doi: 10.1191/0269215502cr487oa. doi:10.1191/0269215502cr487oa. [DOI] [PubMed] [Google Scholar]
- West R, Hill K, Hewison J, Knapp P, House A. Psychological disorders after stroke are an important influence on functional outcomes: A prospective cohort study. Stroke. 2010;41:1723–1727. doi: 10.1161/STROKEAHA.110.583351. doi:10.1161/STROKEAHA.110.583351. [DOI] [PubMed] [Google Scholar]
- Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression: Two questions are as good as many. Journal of General Internal Medicine. 1997;12:439–445. doi: 10.1046/j.1525-1497.1997.00076.x. doi:10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams LS, Yilmaz EY, Lopez-Yunez AM. Retrospective assessment of initial stroke severity with the NIH stroke scale. Stroke. 2000;31:858–862. doi: 10.1161/01.str.31.4.858. doi:10.1161/01.STR.31.4.858. [DOI] [PubMed] [Google Scholar]
- Wittayanukorn S, Qian J, Hansen RA. Prevalence of depressive symptoms and predictors of treatment among US adults from 2005 to 2010. General Hospital Psychiatry. 2014;36:330–336. doi: 10.1016/j.genhosppsych.2013.12.009. doi:10.1016/j.genhosppsych.2013.12.009. [DOI] [PubMed] [Google Scholar]
- Wulsin L, Alwell K, Moomaw CJ, Lindsell CJ, Kleindorfer DO, Woo D, Kissela BM. Comparison of two depression measures for predicting stroke outcomes. Journal of Psychosomatic Research. 2012;72:175–179. doi: 10.1016/j.jpsychores.2011.11.015. doi:10.1016/j.jpsychores.2011.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zisook S, Lesser I, Stewart JW, Wisniewski SR, et al. Effect of age at onset on the course of major depressive disorder. The American Journal of Psychiatry. 2007;164:1539–1546. doi: 10.1176/appi.ajp.2007.06101757. [DOI] [PubMed] [Google Scholar]