Abstract
Background
Among Hispanics in the U.S., lower acculturation level has been found to be protective against alcohol abuse and depression. However, this relationship may not hold within at-risk samples. The prevalence and co-occurrence of hazardous drinking and depressive symptoms and their relationship to acculturation were examined among Hispanics enrolled in a study to reduce heavy drinking. At enrollment, all participants reported past-month heavy drinking (one or more occasions of >4/5 drinks for females/males, and average weekly consumption >7/14 drinks per week). We explored whether gender moderated the effects of acculturation on hazardous drinking and depressive symptoms.
Methods
Participants (N = 100) completed measures at baseline.
Results
Eighty-nine percent of participants met criteria for hazardous alcohol use as assessed by the AUDIT and of those, 55% (n=49) also reported elevated depressive symptoms. Of those who reported elevated depressive symptoms, nearly all (94%) met AUDIT criteria for hazardous drinking. Acculturation was not related to hazardous drinking or depressive symptoms in the full sample. Highly acculturated women reported more hazardous drinking than less acculturated women. Acculturation was not associated with hazardous drinking in men, but less acculturated men reported higher levels of depression than highly acculturated men.
Discussion
Depression should be assessed in alcohol interventions for Hispanics. Alcohol interventions should be tailored for acculturation level and gender to improve relevance and efficacy. Clinical Trial Registration #NCT01996280.
Keywords: Acculturation, depressive symptoms, gender, hazardous drinking, Hispanic
INTRODUCTION
According to U.S. Census projections, Hispanics are estimated to comprise up to 30% of the country’s population by 2050 (U.S. Census data), and are disproportionately low-income and underserved in the mental health care system (Mendelson, Rehkopf, & Kubansky, 2008). Understanding the prevalence of mood and substance use disorders among Hispanics is important to meet mental health needs (Alegría et al., 2007a; Mendelson et al., 2008). National surveys have documented a high prevalence of co-morbid mood and alcohol use disorders among Hispanics in the U.S. (National Comorbidity Study Replication, Kessler, Chiu, Demler, & Walters, 2005; National Epidemiological Survey on Alcohol and Related Conditions, Grant et al., 2004). The National Latino and Asian American Survey (NLAAS), the first nationally representative study of English and Spanish-speaking Hispanics, found high rates of past year mood, anxiety, and substance use disorders. (Alegría et al., 2007a).
Acculturation refers to individual changes that occur as a result of sustained contact between two or more distinct cultures, such as changes in ways of speaking or thinking (Berry, Trimble, & Olmedo, 1986). A surprising pattern in the vast majority of Hispanic mental health literature is that less acculturated immigrants report lower levels of mental disorders relative to more highly acculturated Hispanics (i.e., those who speak English well or who are U.S. born (Alegría, Canino, Stinson, & Grant, 2006; Alegría et al, 2007a). The fact that many immigrants have better mental health despite being more poorly resourced than their U.S.-born counterparts, suggests that low acculturation level confers a protective effect against poor mental health, possibly through growing up in a country with less exposure to discrimination, or through cultural socialization in the country of origin (Alegría et al., 2007b; Alegría, Sribney, Woo, Torres, & Guarnaccia, 2007c; Canino, Vega, Sribney, Warner, & Alegría, 2008). One explanation for this paradoxical finding is the healthy migrant hypothesis, which suggests that the paradox results from the selection of healthy Hispanic immigrants into the United States (Abraido-Lanza, Chao, & Florez, 2005). Those Hispanics who are able to migrate to the U.S. may be selected from the overall population in the country of origin for better physical and mental health (Abraido-Lanza, Dohrenwend, Ng-Mak, & Turner, 1999).
The National Comorbidity Study Replication (NCS-R) reported that immigrants (51% of Hispanic sample) had a lower lifetime risk of having a psychiatric disorder than U.S. born individuals, and that risk for any psychiatric disorder among immigrants increased following their arrival in the U.S. (Breslau et al., 2007). Studies of foreign and U.S. born Mexicans have identified U.S. nativity as a main factor associated with increased use of alcohol and drugs (Borges et al., 2011; Grant et al., 2004). A study using NLAAS data found that several indicators of acculturation, including longer length of time in the U.S., English language preference, and weaker Hispanic ethnic identification were associated with drug use disorders (Blanco et al., 2013).
In two separate analyses, a review of the literature on drinking behavior and alcohol-related problems among Hispanic adults (Zemore, 2007), as well as an analysis of data of Hispanic adults in the U.S. 1995 National Alcohol Survey, results indicated a strong association between higher acculturation and increased odds of drinking among women and a weaker, less consistent relationship among men (Zemore, 2005; 2007). Some evidence suggested that more acculturated men are more likely to drink (and thus have more alcohol-related problems) than less acculturated men (Cherpitel, Borges, & Medina-Mora, 2000; Zemore, 2007). Other evidence suggested that being highly acculturated and male was associated with a lighter drinking pattern (Zemore, 2007). Overall, findings of the Zemore (2007) literature review converge with research documenting a more dramatic and consistent change in drinking behavior among Hispanic immigrant women following U.S. arrival (e.g., Caetano, 1987a; Caetano, Ramisetty-Mikler, & Rodriguez, 2009), possibly due to more liberal norms for alcohol among women in the U.S. compared to Latin America (Vaeth, Caetano, & Rodriguez, 2012), and changes in social contexts in the U.S. where alcohol is available (Caetano, 1987a). Two prevailing theories that have been used to understand the relationship between acculturation and substance use and mental health among general samples of Hispanic immigrants are sociocultural theory (Room, 1992) and social stress theory (Graves, 1967). The sociocultural theory posits that the process of acculturation involves adapting behavioral antecedents (e.g. social norms, attitudes, behaviors and beliefs) of the receiving country. If the new behavioral antecedents support substance use, acculturation would be associated with an increase in use of substances such as alcohol (Caetano, 1987b). The stress model maintains that poor mental health (e.g. hazardous alcohol use, depressive symptoms) develops when stressors such as perceived discrimination, language barriers and poverty, exceed the immigrants’ resources for successfully acculturating into the new society (Graves, 1967).
The relationship between acculturation and drinking behavior has been reported in the context of national surveys such as the NLAAS and the NCS-R, which aim to track prevalence in the general population. Therefore, the extent to which findings on acculturation and drinking behavior extend to more at-risk samples, remains less known. There have been a handful of studies on Hispanics seeking substance use treatment (Alvarez, Olson, Jason, Davis, & Ferrari, 2004; Rojas, Hallford, Brand, & Tivis, 2012), and of them, one (Arciniega, Arroyo, Miller, & Tonigan, 1996) examined acculturation. In 1989, the U.S. National Institutes of Health launched Project MATCH (Matching Patients with Alcohol Disorders to Treatments), to investigate whether different behavioral treatments (Cognitive-Behavioral Therapy, Twelve-Step Facilitation, or Motivational Enhancement Therapy) were suited to patients with different characteristics, including: severity of alcohol involvement, gender, motivation, and psychiatric severity (Project MATCH Research Group, 1997). A secondary analysis of Project MATCH did not find any associations between acculturation level and drinking behavior, including number of heavy drinking days (Arciniega et al., 1996). Of note, the study used an acculturation scale that measured adherence to Mexican cultural norms and the Hispanic sample was only 34% Mexican.
Understanding the prevalence, co-morbidity, and etiology of substance abuse and depression among a Hispanic at-risk sample is needed given the poorer response to substance abuse treatment (Alvarez et al., 2004; Brecht, von Mayrhauser, & Anglin, 2000), including higher premature termination rates (see Alvarez et al., 2004, for a review; White, Winn, & Young, 1998). Hispanics report greater co-occurrence of elevated depressive symptoms and hazardous drinking than non-Hispanics (Mendelson et al, 2008; Sleath & Williams, 2004). A study that recruited Columbian, Dominican, and Puerto Rican men from U.S. community settings revealed that heavy alcohol use more than doubled the risk of depression (Zayas, Rojas, & Malgady, 1998). Further, the co-occurrence of hazardous alcohol use and depressive symptoms worsens clinical outcomes (Cooney et al., 2001; Karno & Longabaugh, 2003; Hesse, 2009). For example, providers are cautioned to assess depressive symptoms among their patients as depressed states may increase risk for poor outcomes after alcohol treatment (Cooney et al., 2001; Karno & Longabaugh, 2003). Moreover, Hispanics with poor mental health who drink heavily suffer more serious consequences relative to non-Hispanic whites. Analysis of the NVDRS National Violent Death Reporting System revealed higher rates of alcohol dependence were found among Hispanics who completed suicide (17%), second only to American Indians and Alaskan Natives (21%), and alcohol was found in 40% of all Hispanic suicide completers (Karch, Barker, & Strine, 2006).
The overarching purpose of this study was to clarify the clinical characteristics of an at-risk sample of Hispanic heavy drinkers. Our first aim was to examine the prevalence of and correlation and co-occurrence between hazardous drinking and depressive symptoms. The second aim was to examine the relationship between acculturation level and hazardous drinking and depressive symptoms in an at-risk sample. The final aim was to explore whether gender moderated the effects of acculturation on hazardous drinking and depressive symptoms. Based on the above theories and past studies with general population samples, we hypothesized that the relationship between acculturation and hazardous drinking and depressive symptoms would be stronger among more acculturated individuals than among less acculturated individuals. Given that our sample is more at-risk than the general population, we similarly hypothesized that the effects of low acculturation on hazardous drinking and depressive symptoms would be attenuated. Moderating effects of gender were exploratory.
METHODS
Participants
The sample (N = 100) was recruited as part of an on-going randomized clinical trial testing a motivational interviewing intervention delivered to heavy drinking Hispanics. Individuals who wanted to learn more about the health effects of their drinking responded to newspaper advertisements posted in the local free newspaper (English and Spanish). The study was not advertised as treatment for alcohol use disorders. Potential participants were asked the general question, “Do you enjoy drinking?” and were then asked how many drinks they typically had on one occasion. If their drinking met the following criteria (> 5/4 drinks per occasion or > 14/7 drinks per week on average for men/women respectively over the past 30 days (NIAAA, 2010)), they were enrolled in the study. We chose a general question to assess drinking among potential participants because it was perceived to be more open and less potentially stigmatizing than an alcohol screening measure that asked about drinking consequences. Other study inclusion criteria included: between 18–65 years of age, and self-identified as Hispanic. Study exclusion criteria: psychotic symptoms, as evidenced by hallucinations or delusions, cognitive impairment, as evidenced by inability to understand informed consent, and 3rd generation or later Hispanics. Eligible participants completed in-person assessments, which included the Alcohol Use Disorders Identification Test (AUDIT), a more detailed measure of their drinking behavior and consequences, prior to receiving the intervention. The AUDIT was administered only to study enrolled participants to assess their level of hazardous drinking. Respondents were given the choice between being interviewed and assessed in English or in Spanish. Fifty percent (n = 50) of the respondents chose to be interviewed in Spanish. At the time of the study, all of the measures (AUDIT, CES-D, SASH) were available in Spanish. Reliability and validity data for the Spanish translations are provided in the Measures section, as well as reliability data specific to our study. The study was approved by the Institutional Review Board at a university in the Northeast.
Measures
Hazardous drinking
The Alcohol Use Disorders Identification Test (AUDIT;Saunders, Aasland, Babor, DelaFuente, & Grant, 1993) was used at baseline to measure level of hazardous drinking. The AUDIT is a widely used 10-item screening questionnaire that asks about the quantity and frequency of alcohol use, alcohol-related negative consequences, and a few indices of dependence (Saunders et al., 1993). The total score was used to describe participants’ alcohol use severity at baseline and was used in analyses as the continuous hazardous drinking score. Sample items include questions about quantity of alcohol consumed: “How many drinks containing alcohol do you have on a typical day when you are drinking? and consequences: “How often during the last year have you had a feeling of guilt after drinking”. AUDIT total scores > 8 for men and > 6 for women indicate hazardous drinking, (Saunders et al., 1993), with higher scores (> 15 for men; > 13 for women) suggestive of probable alcohol use disorder. The AUDIT was originally intended to be valid in different cultures (Saunders et al., 1993), and has been translated and used with Spanish–speaking populations (Babor, La Fuente, Saunders, & Grant, 1992). In fact, only questions that could be translated, “literally and idiomatically” into multiple languages, were included in the AUDIT (Saunders et al., 1993, p. 799). The AUDIT has been found to perform equally well (e.g., differentiating between alcoholics and non-drinkers) across countries, including Mexico (Saunders et al., 1993; Steinbauer et al., 1998; Volk et al., 1997). That said, because the original AUDIT validation study included Mexicans only, further investigation on the validity of the Spanish-translated AUDIT (Reinert & Allen, 2007) for different ethnic subgroups, such as Puerto Ricans, is warranted. For example, in a comprehensive review of international studies using the AUDIT (Spain, n = 5 studies; Meneses-Gaya, Zuadi, Loureira, & Crippa, 2009), none reported the validity of the Spanish-translated AUDITs. With respect to the internal consistency reliability of the AUDIT in different countries, estimates are high, ranging between 0.80–0.83 (Meneses-Gaya et al., 2009; Reinert & Allen, 2008). However, future research is needed to be able to conclusively suggest optimal cut-points for AUDIT for different populations (Reinert & Allen, 2007). For example, low acculturation may diminish the ability of AUDIT to detect hazardous alcohol use (Cherpitel, 1999; Cherpitel & Borges, 1999). Among our entire study sample, internal consistency reliability was high (α = 0.85). Reliability coefficients were similar for Spanish-speaking (α = 0.81, n= 47), and for English-speaking (α = 0.87, n = 52).
Acculturation
The Short Acculturation Scale for Hispanics (SASH; Marin, Sabogal, Marin, Otero-Sabogal, & Perez-Stable, 1987) 12-item scale assesses acculturation by means of three subscales: Language use (English or Spanish-speaking preference, 5 items; sample item: “In general, what language(s) do you usually speak at home?”), media preference (3 items, sample item: “In what language(s) are the T.V. programs you usually watch?”), and ethnic and social relations (4 items, sample item: “your close friends are…”). Responses to each statement use a 5-point Likert scale where 1 = only Spanish and 5 = Only English (1=All Latinos/Hispanics and 5= All Americans regarding the Ethnic/Social relations subscale). Higher scores indicate higher acculturation levels; a score of three has been established as the cutoff for differentiating low versus highly acculturated Hispanics (high acculturation > 3; low acculturation < 3; Marin et al., 1987; Ellison, Jandorf, & Duhamel, 2011; Vella, Ontiveros, Zubia, & Bader, 2011). The SASH has good to excellent criterion validity, with Cronbach’s alpha = .92 for the entire scale and alpha coefficients ranging between.78 and .90 for the subscales (Marin et al., 1987). A validation study sampled Hispanic (n=363) and non-Hispanic (n=228) Whites, and revealed differentiation of responses on the sash between first and second generation Hispanics, positive correlations with length of U.S. residency, negative correlations with age of U.S. arrival, and differentiated between the two ethnic subgroups (Marin et al., 1987). However, the sample was mainly Mexican-American, so generalizability of results were limited (Marin et al., 1987). Further, it was not specified what percentage of the sample responded to the SASH in Spanish. The SASH has been used with Spanish and English-speaking participants and the alpha reliabilities reported for both populations have been similar to those reported by Marin et al., 1987. For example, a study of cancer screening beliefs among Hispanics (91% Spanish-speaking) revealed alpha reliabilities of .89 for the entire SASH scale (Ellison et al., 2011). Among our entire study sample, internal consistency reliability was excellent (α = 0.93). Reliability coefficients were similar for Spanish-speaking (α = 0.86), and for English-speaking (α = 0.82) participants.
Depressive symptomology
Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977) assessed level of depressive symptoms over the prior week, including the day of administration. Items are scored on a four-point Likert scale (0 = rarely or none of the time, 3 = most or all of the time). Sample items include: “I was bothered by things that usually don’t bother me”, and “I felt like I could not shake off the blues even with help from my family or friends”. Possible scores range from 0 to 60, with higher scores indicative of more severe depressive symptoms. Past research, including research on Hispanics, has used a score of 16 or greater (Caetano, 1987a; Zayas et al., 1998) to indicate risk for clinical depression (Lewinsohn, Seeley, Roberts, & Allen, 1997; Posner, Stewart, Marin, & Perez-Stable, 2001; Tsai, Pole, Levenson, & Munoz, 2003). CES-D scores of 0–9 suggest no depression, 10–15 are suggestive of minimum or mild risk, 16–24 suggests moderate risk, and those above 24 are suggestive of severe risk for major depression (Radloff, 1977). In English, the CES-D has high internal consistency (α = 0.85) (Radloff, 1977), as does the Spanish translation (α = 0.88; Roberts, 1980). Studies investigating the validity of the CES-D have been mixed, with most studies supporting its cross-cultural validity. The CES-D has been validated in multiple languages, including Spanish (Ruiz-Grosso et al., 2012). Spanish-speaking women enrolled in a health education study (Peragallo, Gonzalez-Guarda, McCabe, & Cianelli, 2011) responded similarly to the CES-D items, even after controlling for their level of depression (McCabe, Vermeesch, Hall, Peragallo, & Mitrani, 2011). However, another international study of smokers (N=13,629) revealed a different factor structure for English compared to Spanish-speaking participants, the latter group endorsing an Anxious/Somatic factor that was not endorsed by English speakers (Leykin, Torres, Aguilera, & Munoz, 2011), suggesting that the validity of the CES-D across different languages and cultural groups needs further investigation. In this study, for the entire sample, internal consistency reliability was excellent (α = 0.91). Reliability coefficients were similar for Spanish-speaking (α = .090) as well English-speaking (α = 0.92) participants.
Analysis
In preliminary analyses, we used Pearson product-moment correlations and chi-square tests to examine the correlation between and co-occurrence of hazardous drinking and depression. General linear modeling (GLM) was used to examine the effect of acculturation on hazardous drinking and depressive symptoms. We specified an interaction term (gender x acculturation) to test whether gender moderated the relationships between acculturation and hazardous drinking and depressive symptoms. We then used simple effects tests to follow up significant interactions and identify patterns of differences by gender. Alpha was set at .05 for hypothesis testing. Variables were not centered prior to running analyses because these analyses focused on variables at a single time point.
RESULTS
Participant characteristics
Detailed participant demographic characteristics are reported in Table 1. The average AUDIT score in this sample was 17.6 (SD = 9.00). Eighty-nine percent (n=89) of all participants (N=100) were hazardous drinkers and nearly 60% (n=58) of all participants met AUDIT criteria for probable alcohol use disorder. In the 90 days prior to study participation, both men and women reported high weekly drinking levels, and men consumed significantly more alcohol than women (men, M = 46 drinks/wk., SD = 48.53; women, M = 28 drinks/wk., SD = 29.51), t (91.28) = 2.29, p = .024, Cohen’s d = .48. In the 90 day window, women averaged 31% heavy drinking days (SD=24.3), and men averaged 40% heavy drinking days (SD=32.98), t (80.23) = 1.58, p = .118, Cohen’s d = .35. The average CES-D score was 19.02 (SD = 12.73). Overall, slightly more than half of participants scored at or above the CES-D cut point (> 16) for probable major depressive disorder (females, 54.5%; males, 51%).
Table 1.
Participant demographic characteristics (N=100)
| Variable | Total N | Male (n=67) |
% | Female (n=33) |
% | t | p |
|---|---|---|---|---|---|---|---|
| Age (M±SD)a | 42 ±11.81 | 43 ±12.24 | 41 ±10.82 | 1.13 | .26 | ||
| Age of Migration (M±SD) | 22 ±13.21 | 22 ±13.20 | 21 ±13.57 | .12 | .90 | ||
| Place of Birth | 1.34 | .19 | |||||
| Mainland US | 28 | 16 | 23.9 | 12 | 36.4 | ||
| Puerto Rico | 28 | 19 | 28.4 | 9 | 27.3 | ||
| Dominican Republic | 13 | 9 | 13.4 | 4 | 12.1 | ||
| Otherb | 31 | 23 | 34.3 | 8 | 24.2 | ||
| Race | .58 | .57 | |||||
| White | 23 | 15 | 22.4 | 8 | 24.2 | ||
| Black | 9 | 8 | 11.9 | 1 | 03.0 | ||
| More than one | 58 | 38 | 56.7 | 20 | 60.6 | ||
| Other | 10 | 5 | 09.0 | 4 | 12.2 | ||
| Acculturation Level (Low) | 57 | 36 | 53.7 | 21 | 63.6 | .94 | .35 |
| Marital Status | 1.05 | .30 | |||||
| Single/Never married | 52 | 32 | 47.8 | 20 | 60.6 | ||
| Married | 20 | 15 | 22.4 | 5 | 15.2 | ||
| Divorced or Separated | 28 | 20 | 29.8 | 8 | 24.2 | ||
| Education | .720 | .47 | |||||
| Less than High School | 9 | 5 | 07.5 | 4 | 12.1 | ||
| High School/ Equivalent | 36 | 27 | 40.3 | 9 | 27.3 | ||
| Some College | 29 | 20 | 29.9 | 9 | 27.3 | ||
| College | 26 | 15 | 22.4 | 11 | 33.3 | ||
| Current Employment | .78 | .44 | |||||
| Unemployed | 68 | 47 | 70.1 | 21 | 63.6 | ||
| Part Time | 15 | 10 | 14.9 | 5 | 15.2 | ||
| Full Time | 17 | 10 | 14.9 | 7 | 21.2 | ||
| Income (>$15,000)d | 73 | 49 | 73.1 | 24 | 72.7 | −.74 | .46 |
Range 18–65 years
Including: Cuba, Central America (México, Honduras, El Salvador, Nicaragua, and Guatemala) and South America (Colombia, Perú, Venezuela, Brazil)
Defined as either being born in Puerto Rico (n=28) or having at least one parent born in Puerto Rico (n=17)
Annual, individual
Correlation, co-occurrence, and prevalence of depressive symptoms and hazardous drinking
AUDIT scores were highly correlated with CES-D scores (r = .59, p < .001), sharing 35% of variance. Eighty-nine percent (89%) of participants met criteria for hazardous alcohol use as assessed by the AUDIT. Chi square analyses of those who met AUDIT criteria for hazardous use indicated that 55% (n = 49) also reported elevated depressive symptomatology, x2 = 3.03, p = .08. Of those who reported elevated depressive symptoms (> 16), nearly all (94%, n = 49) met AUDIT criteria for hazardous drinking, x2 = 3.03, p = .08.
Relationship between acculturation, hazardous drinking and depressive symptoms
In the full sample, no significant association was found between acculturation (continuous SASH score) and either hazardous drinking (r = .03, p = .76) or depressive symptoms CES-D (r = .11, p = .28).
Gender as a moderator of the relationship between acculturation, hazardous drinking, and depressive symptoms
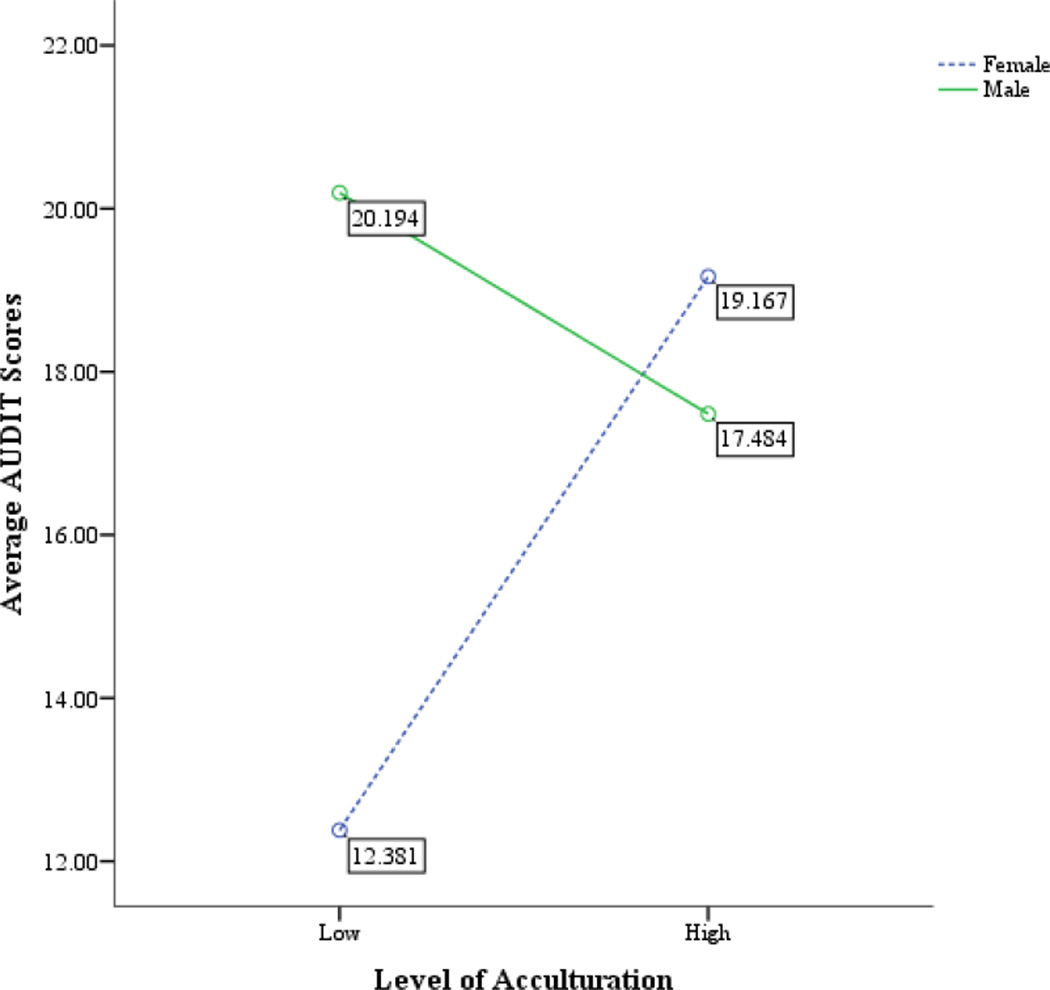
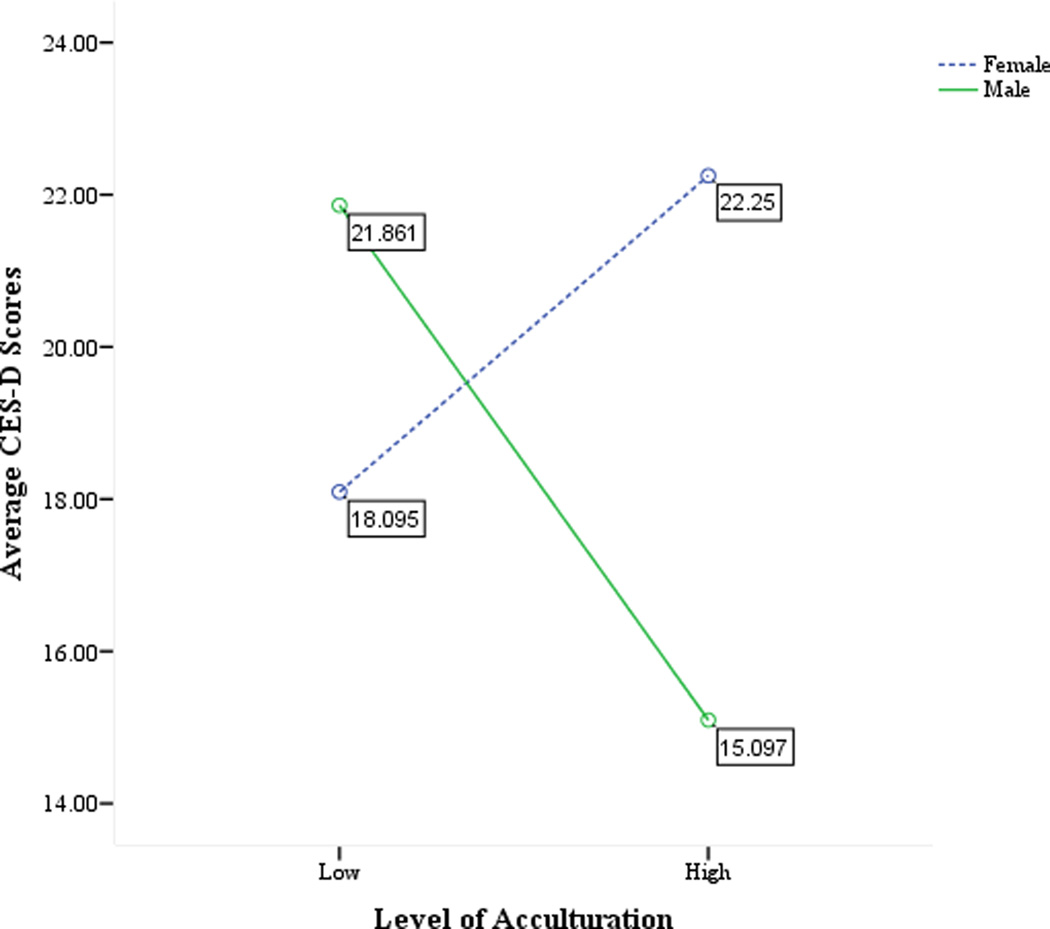
Using t-tests, we did not find any significant differences between men and women on level of acculturation, hazardous drinking (AUDIT), or level of depressive symptomatology (see Table 1). GLM modeling to investigate the moderating effects of gender revealed a significant interaction (F (1, 96) = 6.32, p < .05, η2 = .06) for hazardous drinking, as well as a significant acculturation by gender interaction (F (1, 96) = 3.96, p < .05, η2 = .04), for depressive symptoms. Simple effects tests for AUDIT demonstrated significant differences between low and high-acculturated women (F (1, 96) = 10.84, p < .01, η2 = .11). More acculturated women reported higher AUDIT scores than less acculturated women. (See Figure 1). Furthermore, simple effects tests for CES-D revealed statistically significant differences between low and high-acculturated men (F (1, 96) = 4.84, p < .05, η2 = .05); less acculturated men reported higher CES-D scores than more acculturated men. (See Figure 2).
Figure 1.
The relationship between average AUDIT scores and level of acculturation among men and women, p < .01
Figure 2.
The relationship between average CES-D scores and level of acculturation among men and women, p < .05
DISCUSSION
The present study helps to clarify the clinical picture of an at-risk group of Hispanic heavy drinkers. With regard to the first study aim, we found that more than half of both women and men reported elevated depressive symptoms, and a high co-occurrence of hazardous drinking and depressive symptoms. These findings are in line with estimates of depressive disorder found among Hispanic males (44%) and females (73%) in alcohol treatment (Hesselbrock, Hesselbrock, Segal, Schuckit, & Bucholz, 2003). Hazardous drinkers are typically targeted for brief alcohol interventions in medical and health care settings for several reasons. Hazardous drinking has been associated with negative social and physical consequences, including: alcohol impaired driving (Naimi et al., 2003), interpersonal violence and injury (NIAAA, 2000; Gmel, Givel, Yersin, & Daeppen, 2007), liver disease and cirrhosis mortality (Singh & Hoyert, 2000), and is related to other unhealthy behaviors, such as reckless behavior and low rates of physical activity (Laatikainen, Manninen, Poikolainen, & Vartiainen, 2003). In national surveys in Finland and in the U.S. (1984 National Alcohol Survey), those who drank higher than recommended amounts of drinking at one time had higher mortality rates than those who did not (Laatikainen, Manninen, Poikolainen, & Vartiainen et al., 2003; Rehm, Greenfield, & Rogers, 2001). Hazardous drinking also increases the likelihood of developing problems with drinking (Dawson, Pulay, & Grant, 2010). As a larger percent of the population (25%) experience hazardous drinking compared to those who have an alcohol abuse or dependence disorder (4%) (Grant et al., 2004; Dawson, Grant, Stinson, & Chou, 2004), targeting hazardous drinkers would have a high public health impact by assisting individuals before they need costly specialized treatment for substance use disorders. For example, Verrill and colleagues (2009) demonstrated that abstinence from alcohol, even after being diagnosed with late stage liver failure, can help increase long term survival (72% for alcohol-abstinent patients; 44% for patients continuing to drink). The need to intervene with hazardous drinkers is even more acute for Hispanics, who report higher rates of hazardous drinking (Chartier & Caetano, 2010). In short, our findings highlight the need to screen Hispanic patients for hazardous use and early intervention.
One recommendation is to provide an integrated, coordinated approach to screen and intervene with both hazardous alcohol use and poor mental health (Lydecker et al., 2010). Such an approach might be particularly effective in providing needed care to Hispanics, who are less likely to seek help for their poor mental health than non-Hispanics (Mendelson et al., 2008; Richardson cited in Breslau, Kendler, Su, Gaxiola-Aguilar, & Kessler, 2005, p. 325). Programs that address all patient needs instead of one single disorder can minimize patient burden by making it easier to access care in one place (Drake, Mueser, Clark, & Wallach, 1996; Mueser, Noordsky, Drake, Fox, & Barlow, 2003).
The high co-occurrence of hazardous drinking and elevated depressive symptoms that we found in this at-risk sample suggests that clinical depression should be assessed in the context of alcohol interventions for Hispanics. Under-treatment of depression in substance abusing individuals is common (Nunes & Levin, 2004; Young, Klap, Sherbourne, & Wells, 2001). Offering treatments that address both hazardous drinking and depression is important because untreated depression may increase the likelihood of poor outcomes following alcohol treatment (Cooney et al., 2001; Karno & Longabaugh, 2003).
With regard to the second study aim, we did not find any unmoderated relationships between acculturation level and hazardous drinking or depressive symptoms, consistent with Project MATCH, which studied Hispanics in treatment (Arciniega et al., 1996). Among men in the general population, the relationship between acculturation and alcohol/drug use is not as consistent as among women. Therefore, the non-significant effects of acculturation on hazardous drinking or depressive symptoms in our study overall may be driven primarily by the fact that our participants were predominately male. The lack of association between acculturation and mental health problems in this study is consistent with studies of Latino clinical samples and points to the need to broaden the study of acculturation, which is typically investigated as a unidimensional process, measured by a single construct, such as language preference. The current study did not consider the dual-axis model of acculturation, which views enculturation as a process that simultaneously occurs with acculturation (Gonzalez, Fabrett, & Knight, 2009). Doing so would help identify potential underlying mechanisms through which adaptation to the U.S. culture relates to mental health problems. Our findings, though limited by the lack of inclusion of enculturation as a measure in the original study (e.g., ethnic identity), demonstrate the importance of looking beyond acculturation alone to explain risk behaviors.
Our third study aim explored whether gender moderated the association between acculturation and hazardous drinking. The normally protective effects of low acculturation on heavy drinking were found for women only. That is, among women heavy drinkers but not among men, being less acculturated was associated with less drinking. One explanation may be related to the low base rates of alcohol use among women in Latin America (Canino et al., 1987; Medina-Mora et al., 2005). Traditional gender role norms in Latin America promote abstinence for women, but view drinking as permissible for men (Arciniega, Anderson, Tovar-Blank & Tracey, 2008; Arciniega et al., 1996; Caetano, Ramisetty-Mikler, & Rodriguez, 2009; Nielsen, 2000; Welte & Barnes, 1995). Hispanics in the United States reported more strict attitudes towards alcohol use for women than those reported for men; these attitudes were stricter also than those endorsed by non-Hispanics for non-Hispanic women (Caetano, 1984).
Cultural prohibitions against female drinking may also persist after immigration. National surveys indicate that rates of alcohol consumption among Hispanic females (Caetano & Medina-Mora, 1988) remain low even after years of U.S. residency. On average, study participants had lived in the U.S for over 20 years. The more highly acculturated of these women in the sample reported significantly higher levels of hazardous drinking, more in line with the drinking of non-Hispanic American women. Other research reports increased alcohol use among Hispanic women in the U.S. (Zemore, 2007), possibly due to increased access to places where alcohol is consumed and more liberalized norms (Caetano, 1987b). The use of the dual-axis model of adaptation to U.S. culture can advance the field by providing a more refined perspective on the link between acculturation and a range of psychological outcomes and problem behaviors, mainly by highlighting potential protective effects of culture and how risk for poor mental health increases as the protective effects attenuate over time. Although the role of gender is not specified by the sociocultural theory, the shift in gender norms around alcohol between many Latin American countries and the U.S. (Room, 1992), may aid in the interpretation of our findings among women. For example, even in the U.S., alcohol norms differ for men vs. women, but how much they differ in the U.S. is less pronounced than how much they differ in their country of origin. Similarly, according to the dual axis model, the shift in gender norms around alcohol between many Latin American countries and the U.S., are hypothesized to increase the risk of substance use, particularly for females (Gonzalez et al., 2009).
Among men in our study, acculturation level was not associated with hazardous drinking, consistent with national surveys of Hispanic men in the general population (Zemore, 2007). One possible explanation for the lack of change observed in male drinking with acculturation to the U.S. may be that drinking among Hispanic males is expected and allowed regardless of being in Latin America or in the U.S. In fact, drinking heavily and tolerance to the effects of alcohol has been considered a demonstration of masculinity in the Hispanic culture (Madsen, 1964; Fiorentino, Berger, & Ramirez, 2007; Panitz, McConchie, Sauber, & Fonseca, 1983; Arcinienga et al., 2008). Hispanic males who endorsed high machismo and low self-esteem and who were less educated reported significantly more drinking (Neff, Prihoda, & Hoppe, 1991). However, non-Hispanic males who endorsed this strong male orientation reported more drinking regardless of their educational or self-esteem levels, suggesting that this idea is not specific to Latino culture. Moreover, a factor analysis of the more recent machismo measure (Arciniega et al., 2008), revealed a multi-dimensional concept that included more traditional “masculine” behaviors such as preference for dominance and control, as well as “cabellerismo,” or an interpersonal orientation that included connection and the importance of family involvement. Future research should explore the meaning of machismo among Hispanic men of different socioeconomic backgrounds, and how that might influence drinking behaviors.
We then explored whether gender moderated the effects of acculturation on reported depressive symptoms. The normally protective effects of low acculturation to the U.S. culture on mental health reported in our Hispanic sample were not found for either men or women. In fact, women reported an average level of depressive symptoms that exceeded the clinical cut point for probable clinical depression, suggesting that heavy drinking Hispanic women express elevated depressive symptoms regardless of acculturation level. This pattern is consistent with studies reporting that (Hispanic and non-Hispanic) women who abuse substances in general report more serious levels of psychological and social problems than men (Alvarez et al., 2004; Rojas et al., 2012; Hesselbrock et al., 2003).
In this heavy drinking sample, less acculturated men reported significantly higher levels of depressive symptoms than more acculturated men. Depression has been identified as a risk factor for drinking among Hispanic men (Kail, Zayas, & Malgady, 2000; Vasquez, Gonzalez-Guarda, & DeSantis, 2011) and those who are less acculturated may be at even greater risk. Consistent with social stress theory (Graves, 1967), one explanation may be related to unique aspects of our study sample. On average, study participants resided in the U.S. for over 20 year and reported low income and educational levels, and high unemployment rates. Lack of upward mobility and integration into mainstream society may increase vulnerability to depression (Alcantara, Chen, & Alegría, 2014; Kail et al., 2000; Murphy & Mahalingam, 2006). The patterns observed in this study suggest that our participants may be marginalized, which may increase their risk for depression. It has also been hypothesized that traditional role changes, such as no longer being the sole provider, for men raised in a society that values traditional gender roles may cause stress that predisposes men towards drinking (Neff, 2001; Torres, 2010), and these same stressors may also increase depression. Mills and Caetano (2012) found that stress levels were highest among the least acculturated Hispanic men. Taken together, the social stress theory may offer some insight as to why less acculturated male participants reported higher levels of depressive symptoms. Because we did not measure the participant’s socioeconomic status at the time of U.S. arrival, nor their level of stress, it is beyond the scope of our present study to investigate these possibilities.
A last possible explanation for our findings may have to do with our study composition, which was nearly half Puerto Rican (45%). The protective effects of lower acculturation on mental health and substance use have been most consistently observed among Mexicans (Alegría et al, 2006; Alegría et al., 2008, Alegría et al., 2007b). In fact, higher rates of depression and substance use have been documented among Puerto Ricans, relative to other Hispanic groups in general population studies (Alegría et al., 2007a; Kail et al., 2000). As a U.S. territory for over a century, Puerto Ricans have a unique migratory history compared to other Hispanic groups. Despite having U.S. citizenship, evidence suggests that Puerto Rican migrants continue to be perceived as second-class citizens and experience discrimination (Alegría et al., 2008; Morales, 1986; Harper-Dorton & Lantz, 2007), even as the process of acculturation occurs (Caban-Owen, 2009). Additionally, female Puerto Ricans, many of whom are the heads of households, lose social ties upon arrival to the mainland U.S., thereby exacerbating stress (Canino et al., 1987). Understanding the co-morbidity of heavy drinking and depression can help tailor clinical treatment for Puerto Ricans. Despite having higher levels of education than other Hispanic national groups, Puerto Ricans with poor mental health are less likely to stay in substance abuse treatment (Guerrero, Cepeda, Duan, & Kim, 2012). Issues of substance use and depression need to be addressed especially in the context of understanding current social stressors due to acculturation when working with Puerto Ricans.
In our secondary analysis of clinical data from a randomized trial, examination of adaptation to U.S. culture and drinking behavior was not an a-priori aim. As we did not assess ethnic identity (the core aspect of enculturation; Gonzalez et al., 2009), we were unable to infer how acculturative and enculturative processes (underlying the “dual axis” model) might explain our findings (Gonzalez et al., 2009). Future studies should include measures of enculturation to better explain which strategies people use to adapt to the U.S. culture, and which adaptive strategies are associated with adaptive or mal-adaptive health outcomes (Gonzalez et al., 2009). Other limitations include our cross-sectional design, which does not permit understanding of the temporal ordering of hazardous drinking and depression. In our randomized trial, we needed to reduce response burden and thus gave shorter measures indicating risk for alcohol disorders and clinical depression, not full diagnostic interviewers. The small number of women in the study limits interpretability of the data. Finally, our study generated data that support the reliability of the translated measures used. Although our study did follow translation and back-translation procedures as outlined by Breslin (1986), we do not have quantitative validity data to report on the meaning of each item for participants. Future research should focus on investigating the validity of translated measures used with Spanish-speakers; this is a limitation in the field generally. Despite these limitations, in contrast to most extant research with general population samples, our study helps to clarify the clinical picture of an at-risk sample of Hispanics who drink at hazardous levels. In addition, to our knowledge this is among the first studies to examine whether the normally protective effects of acculturation hold in a clinical sub-sample of Hispanics. Moreover, the current study advances our understanding of if and how gender moderates the effects of acculturation on mood and substance use disorders in a clinical sample of Hispanics.
CONCLUSION
Our findings point to the importance of tailoring alcohol interventions for acculturation level and gender. Additionally, given the high co-morbidity between heavy drinking and depressive symptoms, integrating treatment for mental health problems into alcohol treatment for Hispanics is warranted. Early mental health and substance abuse intervention can reduce health disparities by more quickly connecting Hispanic heavy drinkers into care, thereby avoiding costly specialized treatment (Wang et al., 2005). Finally, adapting alcohol interventions to include acculturation-related stressors that Hispanic heavy drinkers experience (Zemore, Karriker-Jaffe, Keithly, & Mulia, 2011) could minimize the burdens and consequences of untreated mental disorders in this population.
Table 2.
Average scores for CES-D, AUDIT, and Acculturation (N=100)
| Variable | Total | Male | Female | P value |
|---|---|---|---|---|
| CESD | 19.02 (12.73) | 18.73 (12.48) | 19.60 (13.39) | .75 |
| AUDIT | 17.60 (9.00) | 18.94 (9.03) | 14.84 (8.40) | .032 |
| SASH | 2.70 (.93) | 2.76 (.99) | 2.57 (.79) | .35 |
References
- Abraido-Lanza AF, Chao MT, Florez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Social Science and Medicine. 2005;61:1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: A test of the “Salmon Bias” and healthy migrant hypotheses. American Journal of Public Health. 1999;89(10):1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcantara C, Chen CN, Alegría M. Do post-migration perceptions of social morbidity matter for Latino immigrant health? Social Science and Medicine. 2014;101:94–106. doi: 10.1016/j.socscimed.2013.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Shrout P, Woo M, Duan N, Vila D, … Meng XL. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino Groups. American Journal of Psychiatry. 2008;165(3):359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Stinson FS, Grant BF. Nativity and DSM-IV psychiatric disorders among Puerto Ricans, Cuban Americans, and non-Latino Whites in the United States: Results from the national Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67:56–65. doi: 10.4088/jcp.v67n0109. [DOI] [PubMed] [Google Scholar]
- Alegría M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. American Journal of Public Health. 2007a;97(1):68–75. doi: 10.2105/AJPH.2006.087205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Shrout PE, Woo M, Guarnaccia P, Sribney W, Villa D. Understanding differences in the past year psychiatric disorders for Latinos living in the U.S. Social Science and Medicine. 2007b;65:214–230. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Sribney W, Woo M, Torres M, Guarnaccia P. Looking beyond nativity: The relation of age of immigration, length of residence, and birth cohorts to the risk of onset of psychiatric disorders for Latinos. Research in Human Development. 2007c;4(1):19–47. doi: 10.1080/15427600701480980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez J, Olson BD, Jason LA, Davis MI, Ferrari JS. Heterogeneity among Latinas and Latinos entering substance abuse treatment: Findings from a national database. Journal of Substance Abuse Treatment. 2004;26:277–284. doi: 10.1016/j.jsat.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Arciniega GM, Anderson TC, Tovar-Blank ZG, Tracey TJG. Toward a fuller conception of machismo: Development of a Traditional Machismo and Caballerismo scale. Journal of Counseling Psychology. 2008;55:19–33. [Google Scholar]
- Arciniega LT, Arroyo JA, Miller WR, Tonigan JS. Alcohol, drug use and consequences among Hispanics seeking treatment for alcohol-related problems. Journal of Studies on Alcohol and Drugs. 1996;57:613–618. doi: 10.15288/jsa.1996.57.613. [DOI] [PubMed] [Google Scholar]
- Babor TE, La Fuente JR, Saunders J, Grant M. AUDIT–The alcohol use disorders identification test: guidelines for use in primary health care. Geneva: World Health Organization; 1992. [Google Scholar]
- Berry JW, Trimble JE, Olmedo EL. Assessment of acculturation. In: Lonner WJ, Berry JW, editors. Field Methods in cross-cultural research. Beverly Hills, CA: Sage Publishers; 1986. pp. 291–324. [Google Scholar]
- Blanco C, Morcillo C, Alegría M, Dedios MC, Fernández-Navarro P, Regincos R, Wang S. Acculturation and drug use disorders among Hispanics in the U.S. Journal of Psychiatric Research. 2013;47(2):226–232. doi: 10.1016/j.jpsychires.2012.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Breslau J, Orozco R, Tancredi DJ, Anderson H, Aguilar-Gaxiola S, Medina-Mora ME. A cross-national study on Mexico-U.S. migration, substance use and substance use disorders. Drug and Alcohol Dependence. 2011;117:16–23. doi: 10.1016/j.drugalcdep.2010.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brecht ML, von Mayrhauser C, Anglin MD. Predictors of relapse after treatment for methamphetamine use. Journal of Psychoactive Drugs. 2000;32(2):211–220. doi: 10.1080/02791072.2000.10400231. [DOI] [PubMed] [Google Scholar]
- Breslau J, Aguilar-Gaxiola S, Borges G, Kendler KS, Su M, Kessler R. Risk for psychiatric disorder among immigrants and their U.S.-born descendants: Evidence from the National Comorbidity Survey-Replication. Journal of Nervous and Mental Disease. 2007;195(3):189–195. doi: 10.1097/01.nmd.0000243779.35541.c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorder across ethnic groups in the United States. Psychological Medicine. 2005;35:317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslin RW. The wording and translation of research instruments. In: Lonner WJ, Berry JW, editors. Field methods in cross-cultural research. Newbury Park: Sage; 1986. pp. 137–165. [Google Scholar]
- Caban-Owen CV. A study of the acculturation experiences of Puerto Rican migrant women: Manifestations and meaning making process. Doctoral Dissertations. Paper AAI3361000. 2009 http://digitalcommons.uconn.edu/dissertations/AAI3361000.
- Caetano R. Ethnicity and drinking in Northern California: a comparison among Whites, Blacks, and Hispanics. Alcohol and Alcoholism. 1984;19:31–43. [PubMed] [Google Scholar]
- Caetano R. Alcohol use and depression among U.S. Hispanics. British Journal of Addiction. 1987a;82:1245–1251. doi: 10.1111/j.1360-0443.1987.tb00422.x. [DOI] [PubMed] [Google Scholar]
- Caetano R. Acculturation, drinking and social settings among U.S. Hispanics. Drug and Alcohol Dependence. 1987b;19:215–226. doi: 10.1016/0376-8716(87)90041-x. [DOI] [PubMed] [Google Scholar]
- Caetano R, Medina-Mora ME. Acculturation and drinking among people of Mexican descent in Mexico and in the United States. Journal of Studies on Alcohol. 1988;49(5):462–471. doi: 10.15288/jsa.1988.49.462. [DOI] [PubMed] [Google Scholar]
- Caetano R, Ramisetty-Mikler S, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): The association between birthplace, acculturation, and alcohol abuse and dependence across Hispanic national groups. Drug and Alcohol Dependence. 2009;99:215–221. doi: 10.1016/j.drugalcdep.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canino G, Rubio-Stipec M, Shrout PBravo M, Stolberg R, Bird HR. Sex differences and depression in Puerto Rico. Psychology of Women Quarterly. 1987;11:443–459. [Google Scholar]
- Canino GJ, Vega WA, Sribney WM, Warner LA, Alegría M. Social Relationships, social assimilation, and substance use disorder among adult Latinos in the U.S. Journal of Drug Issues. 2008;38(1):69–102. doi: 10.1177/002204260803800104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chartier K, Caetano R. Ethnicity and health disparities in alcohol research. Alcohol Health and Research World. 2010;33(1–2):152–160. [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ. Gender, injury status, and acculturation differences in performance of screening instruments for alcohol problems among U.S. Hispanic emergency department patients. Drug and Alcohol Dependence. 1999;53:147–157. doi: 10.1016/s0376-8716(98)00122-7. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Borges G. Performance of screening instruments for alcohol problems in the ER: A comparison of Mexican-Americans and Mexicans in Mexico. American Journal of Drug and Alcohol Abuse. 2000;26:683–702. doi: 10.1081/ada-100101902. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Borges G, Medina-Mora ME. Screening for alcohol problems: A comparison of instrument performance between the ER and the general population among Mexican Americans in the U.S. and Mexicans in Mexico. Addiction: Research and Theory. 2000;99(1):59–72. [Google Scholar]
- Cooney N, Anton R, Carbonari J, Carroll K, Randall C, Roberts J. Matching clients to alcoholism treatment based on psychopathology. In: Longabaugh R, Wirtz PW, editors. Project MATCH Hypotheses: Results and Causal Chain Analyses. NIAAA Project MATCH Monograph Series. Vol. 8. Washington: Government Printing Office; 2001. pp. 82–97. NIH Publication No. 01–4238. [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Toward the attainment of low-risk drinking goals: A 10-year progress report. Alcoholism: Clinical and Experimental Research. 2004;28:1371–1378. doi: 10.1097/01.alc.0000139811.24455.3e. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Pulay AJ, Grant BF. A comparison of two single-item screeners for hazardous drinking and alcohol use disorder. Alcoholism: Clinical and Experimental Research. 2010;34(2):364–374. doi: 10.1111/j.1530-0277.2009.01098.x. [DOI] [PubMed] [Google Scholar]
- Drake RE, Mueser KT, Clark RE, Wallach ME. The course, treatment, and outcome of substance disorder in persons with severe mental illness. American Journal of Orthopsychiatry. 1996;66(1):42. doi: 10.1037/h0080153. [DOI] [PubMed] [Google Scholar]
- Ellison J, Jandorf L, Duhamel K. Assessment of the short acculturation scale for Hispanics (SASH) among low-income, immigrant Hispanics. Journal of Cancer Education. 2011;26:478–483. doi: 10.1007/s13187-011-0233-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorentino DD, Berger DE, Ramirez JR. Drinking and driving among high-risk young Mexican-American men. Accident Analysis and Prevention. 2007;39:16–21. doi: 10.1016/j.aap.2006.05.013. [DOI] [PubMed] [Google Scholar]
- Gmel G, Givel JC, Yersin B, Daeppen JB. Injury and repeated injury-what is the link with acute consumption, binge drinking and chronic heavy alcohol use? Swiss medical weekly. 2007;137(45–46):642–648. doi: 10.4414/smw.2007.11697. [DOI] [PubMed] [Google Scholar]
- Gonzalez NA, Fabrett FC, Knight GP. Acculturation, enculturation, and the psychosocial adaptation of Latino youth. In: Villarruel FA, Carlo G, Grau JM, Azmitia M, Cabrera NJ, Chanin TJ, editors. Handbook of U.S. Latino Psychology: Developmental and Community-Based Perspectives. Los Angeles: Sage Publishers; 2009. pp. 115–134. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Cou SP, Dufour MC, Compton W, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Graves TD. Acculturation, access, and alcohol in a tri-ethnic community. American Anthropologist. 1967;69:306–321. [Google Scholar]
- Guerrero EG, Cepeda A, Duan L, Kim T. Disparities in completion of substance abuse treatment among Latino subgroups in Los Angeles County, CA. Addictive Behaviors. 2012;37:1162–1166. doi: 10.1016/j.addbeh.2012.05.006. [DOI] [PubMed] [Google Scholar]
- Harper-Dorton K, Lantz J. Cross-cultural practice: social work with diverse populations. 2nd ed. Chicago: Lyceum Books; 2007. [Google Scholar]
- Hesse M. Integrated psychological treatment for substance U.S. and co-morbid anxiety or depression vs. treatment for substance U.S.e alone. A systematic review of the published literature. BMC psychiatry. 2009;9(1):6. doi: 10.1186/1471-244X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesselbrock MN, Hesselbrock VM, Segal B, Schuckit MA, Bucholz K. Ethnicity and psychiatric comorbidity among alcohol-dependent persons who receive inpatient treatment African Americans, Alaska Natives, Caucasians, and Hispanics. Alcoholism: Clinical and Experimental Research. 2003;27:1368–1373. doi: 10.1097/01.ALC.0000080164.21934.F9. [DOI] [PubMed] [Google Scholar]
- Kail B, Zayas LH, Malgady RG. Depression, acculturation, and motivations for alcohol use among young Colombian, Dominican, and Puerto Rican men. Hispanic Journal of Behavioral Sciences. 2000;22:64–77. [Google Scholar]
- Karch DL, Barker L, Strine TW. Race/ethnicity, substance abuse, and mental illness among suicide victims in 13 U.S. states: 2004 data from the National Violent Death Reporting System. Injury Prevention. 2006;12(Suppl 2):i22–ii27. doi: 10.1136/ip.2006.013557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karno MP, Longabaugh R. Patient depressive symptoms and therapist focus on emotional material: A new look at Project MATCH. Journal of Studies on Alcohol. 2003;64:607–615. doi: 10.15288/jsa.2003.64.607. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walter EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Archives of General Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laatikainen T, Manninen L, Poikolainen K, Vartiainen E. Increased mortality related to heavy alcohol intake pattern. Journal of Epidemiology and Community Health. 2003;57:379–384. doi: 10.1136/jech.57.5.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiological Studies-Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging. 1997;12:277–287. doi: 10.1037//0882-7974.12.2.277. http://dx.doi.org/10.1037/0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- Leykin Y, Torres LD, Aguilera A, Munoz RF. Factor structure of the CES-D in a sample of Spanish and English-speaking smokers on the Internet. Psychiatry Research. 2011;185:269–274. doi: 10.1016/j.psychres.2010.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lydecker KP, Tate SR, Cummins KM, McQuaid J, Granholm E, Brown SA. Clinical outcomes of an integrated treatment for depression and substance use disorders. Psychology of Addictive Behaviors. 2010;24(3):453. doi: 10.1037/a0019943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madson W. The alcoholic agringado. American Anthropologist. 1964;66:355–361. [Google Scholar]
- Marin G, Sabogal F, Marin FV, Otero-Sabogal R, Perez-Stable E. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Studies. 1987;9:183–205. [Google Scholar]
- McCabe BE, Vermeesch AL, Hall RF, Peragallo NP, Mitrani VB. Acculturation and the Center for Epidemiological Studies Depression Scale for Hispanic women. Nursing Research. 2011;60(4):270–275. doi: 10.1097/NNR.0b013e318221b8dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina-Mora ME, Borges G, Lara C, Benjet C, Blanco J, Fleiz C, … Zambrano J. Prevalence, service use, and demographic correlates of 12 month DSM-IV psychiatric disorders in Mexico: Results from the Mexican National Comorbidity Survey. Psychological Medicine. 2005;35(12):1773–1783. doi: 10.1017/S0033291705005672. [DOI] [PubMed] [Google Scholar]
- Mendelson T, Rehkopf DH, Kubzansky LD. Depression among Latinos in the United States: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2008;76(3):355–366. doi: 10.1037/0022-006X.76.3.355. [DOI] [PubMed] [Google Scholar]
- Meneses-Gaya C, Zuardi AW, Loureiro SR, Crippa JA. Alcohol Use Disorders Identification Test (AUDIT): An updated systematic review of psychometric properties. Psychology & Neuroscience. 2009;2:83–97. [Google Scholar]
- Mills BA, Caetano R. Decomposing associations between acculturation and drinking in Mexican Americans. Alcoholism: Clinical and Experimental Research. 2012;36(7):1205–1211. doi: 10.1111/j.1530-0277.2011.01712.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales J. Puerto Rican poverty and migration: We just had to try elsewhere. Westport, CT: Praeger; 1986. [Google Scholar]
- Mueser KT, Noordsky DL, Drake RE, Fox L, Barlow DH. Integrated treatment for dual disorders: A guide to effective practice. New York, NY: Guilford Press; 2003. [Google Scholar]
- Murphy EJ, Mahalingam R. Perceived congruence between expectations and outcomes: Implications for mental health among Caribbean Immigrants. American Journal of Orthopsychiatry. 2006;76(1):120–127. doi: 10.1037/0002-9432.76.1.120. [DOI] [PubMed] [Google Scholar]
- Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS. Binge drinking among U.S. adults. Journal of the American Medical Association. 2003;289(1):70–75. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) Rethinking Drinking: Alcohol and Your Health. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2010. Accessed at http://pubs.niaaa.nih.gov/publications/RethinkingDrinking/Rethinking_Drinking.pdf. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) Tenth Special Report to the U.S. Congress on Alcohol and Health. Bethesda, MD: National Institutes of Health; 2000. Accessed at http://pubs.niaaa.nih.gov/publications/10report/intro.pdf. [Google Scholar]
- Neff JA, Prihoda TJ, Hoppe SK. “Machismo”, self-esteem, education and high maximum drinking among Anglo, Black and Mexican-American male drinkers. Journal of Studies on Alcohol. 1991;52(5):458–463. doi: 10.15288/jsa.1991.52.458. [DOI] [PubMed] [Google Scholar]
- Neff JA. A Confirmatory factor analysis of a measure of “machismo” among Anglo, African-American, and Mexican-American male drinkers. Hispanic Journal of Behavioral Sciences. 2001;23(92):171–188. [Google Scholar]
- Nielsen AL. Examining drinking patterns and problems among Hispanic groups: Results from a national survey. Journal of Studies on Alcohol. 2000;61:301–310. doi: 10.15288/jsa.2000.61.301. [DOI] [PubMed] [Google Scholar]
- Nunes EV, Levin FR. Treatment of depression in patients with alcohol or other drug dependence: A meta-analysis. Journal of the American Medical Association. 2004;291(15):1887–1896. doi: 10.1001/jama.291.15.1887. [DOI] [PubMed] [Google Scholar]
- Panitz DR, McConchie RD, Sauber SR, Fonseca JA. The role of machismo and the Hispanic family in the etiology and treatment of alcoholism in Hispanic American males. American Journal of Family Therapy. 1983;11:31–44. [Google Scholar]
- Peragallo N, Gonzalez-Guarda RM, McCabe BE, Cianelli R. The efficacy of an HIV risk reduction intervention for Hispanic women. AIDS and Behavior. 2012;16(5):1316–1326. doi: 10.1007/s10461-011-0052-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner SF, Stewart AL, Marin G, Perez-Stable EJ. Factor variability of the Center for Epidemiological Studies Depression Scale (CES-D) among urban Latinos. Ethnicity and Health. 2001;6:137–144. doi: 10.1080/13557850120068469. [DOI] [PubMed] [Google Scholar]
- Project MATCHResearch Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58(1):7–9. [PubMed] [Google Scholar]
- Radloff LS. The CES-Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rehm J, Greenfield TK, Rogers JD. Average volume of alcohol consumption, patterns of drinking, and all-cause mortality: Results from the U.S. National Alcohol Survey. American Journal of Epidemiology. 2001;153(1):64–70. doi: 10.1093/aje/153.1.64. [DOI] [PubMed] [Google Scholar]
- Reinert DF, Allen JP. The alcohol use disorders identification test: an update of research findings. Alcoholism: Clinical and Experimental Research. 2007;31(2):185–199. doi: 10.1111/j.1530-0277.2006.00295.x. [DOI] [PubMed] [Google Scholar]
- Roberts RE. Reliability of the CES-D scale in different ethnic contexts. Psychiatry research. 1980;2(2):125–134. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- Rojas JI, Hallford G, Brand MW, Tivis LJ. Latino/as in substance abuse treatment: Substance use patterns, family history of addiction and depression. Journal of Ethnicity in Substance Abuse. 2012;11(1):75–85. doi: 10.1080/15332640.2012.652530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Room R. Paradigms of social research on alcohol and drug use and dependence. In: Cohén-Yáñez JL, Amezcua-Gastélum J, Villarreal L, Salazar Zavala, editors. Drug Dependence: From the Molecular to the Social Level. Amsterdam: Elsevier Science Publishers; 1992. pp. 213–220. [Google Scholar]
- Rumpf H, Hapke U, Meyer C, John U. Screening for alcohol use disorders and at-risk drinking in the general population: psychometric performance of three questionnaires. Alcohol and Alcoholism. 2002;37:261–268. doi: 10.1093/alcalc/37.3.261. [DOI] [PubMed] [Google Scholar]
- Ruiz-Grosso P, de Mola CL, Vega-Dienstmaier JM, Arevalo JM, Chavez K, Vilela A, Huapaya J. Validation of the Spanish center for epidemiological studies depression and Zung self-rating depression scales: a comparative validation study. 2012 doi: 10.1371/journal.pone.0045413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland O, Babor TF, De La Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Singh GK, Hoyert DL. Social epidemiology of chronic liver disease and cirrhosis mortality in United States, 1935–1997: Trends and differentials by ethnicity, socioeconomic status, and alcohol consumption. Human Biology. 2000;72(5):801–820. [PubMed] [Google Scholar]
- Sleath BL, Williams JW. Hispanic ethnicity, language, and depression: Physician-patient communication and patient use of alternative treatments. International Journal of Psychiatry in Medicine. 2004;34(3):235–246. doi: 10.2190/VQU1-QYWT-XW6Y-4M14. [DOI] [PubMed] [Google Scholar]
- Steinbauer JR, Cantor SB, Holzer CE, III, Volk RJ. Ethnic and sex bias in primary care screening tests for alcohol use disorders. Annals of Internal Medicine. 1998;129:353–362. doi: 10.7326/0003-4819-129-5-199809010-00002. [DOI] [PubMed] [Google Scholar]
- Torres L. Predicting levels of Latino depression: acculturation, acculturative stress, and coping. Cultural Diversity and Ethnic Minority Psychology. 2010;16(2):256–263. doi: 10.1037/a0017357. [DOI] [PubMed] [Google Scholar]
- Tsai JL, Pole M, Levenson RW, Munoz RF. The effects of depression of the emotional responses of Spanish-speaking Latinas. Cultural Diversity and Ethnic Minority Psychology. 2003;9:49–63. doi: 10.1037/1099-9809.9.1.49. http://dx.doi.org/10.1037/1099-9809.9.1.49. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. U.S. Census Bureau News. Profile America: Hispanic Heritage Month 2012; 2012. Retrieved from http://www.census.gov/ne/releases/pdf/cb12ff-19_hispanic.pdf. [Google Scholar]
- United States Census Bureau. Census Bureau Projects Tripling of Hispanic and Asian populations in 50 years: Non-Hispanic Whites may drop to half of total population. Washington, D.C: U.S. Census Bureau; 2004. [Google Scholar]
- Vaeth PAC, Caetano R, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): The association between acculturation, birthplace and alcohol consumption across Hispanic national groups. Addictive Behaviors. 2012;37:1029–1037. doi: 10.1016/j.addbeh.2012.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasquez EP, Gonzalez-Guerda RM, De Sanits JP. Acculturation, depression, self-esteem, and substance abuse among Hispanic Men. Issues in Mental Health Nursing. 2011;32(2):90–97. doi: 10.3109/01612840.2010.528169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vella CA, Ontiveros D, Zubia RY, Bader JO. Acculturation and metabolic syndrome risk factors in young Mexican and Mexican-American women. Journal of Immigrant and Minority Health. 2011;13:119–126. doi: 10.1007/s10903-009-9299-7. [DOI] [PubMed] [Google Scholar]
- Verrill C, Markham H, Templeton A, Carr NJ, Sheron N. Alcohol-related cirrhosis—early abstinence is a key factor in prognosis, even in the most severe cases. Addiction. 2009;104(5):768–774. doi: 10.1111/j.1360-0443.2009.02521.x. [DOI] [PubMed] [Google Scholar]
- Volk RN, Steinbauer JR, Cantor SB, Holzer CE., III The Alcohol Disorders Identification Test (AUDIT) as a screen for at-risk drinking in primary care patients of different racial/ethnic backgrounds. Addiction. 1997;92:197–206. [PubMed] [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- Welte JW, Barnes GM. Alcohol and other drug use among Hispanics in New York State. Alcoholism: Clinical and Experimental Research. 1995;19:1061–1066. doi: 10.1111/j.1530-0277.1995.tb00989.x. [DOI] [PubMed] [Google Scholar]
- White JM, Winn KL, Young W. Predictors of attrition from an outpatient chemical dependency program. Substance Abuse. 1998;19:49–59. doi: 10.1080/08897079809511374. [DOI] [PubMed] [Google Scholar]
- Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry. 2001;58:55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- Zayas LH, Rojas M, Malgady RG. Alcohol and drug use, and depression among Hispanic men in early adulthood. American Journal of Community Psychology. 1998;26(3):425–438. doi: 10.1023/a:1022111221380. [DOI] [PubMed] [Google Scholar]
- Zemore SE. Re-examining whether and why acculturation relates to drinking outcomes in a rigorous, National survey of Latinos. Alcoholism: Clinical and Experimental Research. 2005;29(12):2144–2153. doi: 10.1097/01.alc.0000191775.01148.c0. [DOI] [PubMed] [Google Scholar]
- Zemore SE. Acculturation and alcohol among Latino adults in the United States: A comprehensive review. Alcoholism: Clinical and Experimental Research. 2007;31(12):1968–1990. doi: 10.1111/j.1530-0277.2007.00532.x. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Karriker-Jaffe KJ, Keithly S, Mulia N. Racial prejudice and unfair treatment: interactive effects with poverty and foreign nativity on problem drinking. Journal of Studies on Alcohol and Drugs. 2011;72:361–370. doi: 10.15288/jsad.2011.72.361. [DOI] [PMC free article] [PubMed] [Google Scholar]