Abstract
Background
Prevalence and characteristics of the continuum of diagnoses within fetal alcohol spectrum disorders (FASD) were researched in previously unstudied rural, agricultural, lower socioeconomic populations in South Africa (ZA).
Methods
Using an active case ascertainment approach among first grade learners, 1354 (72.6%) were consented into the study via: height, weight, and/or head circumference ≤25th centile and/or random selection as normal control candidates. Final diagnoses were made following: examination by pediatric dysmorphologists/geneticists, cognitive/behavioral testing, and maternal risk factor interviews.
Results
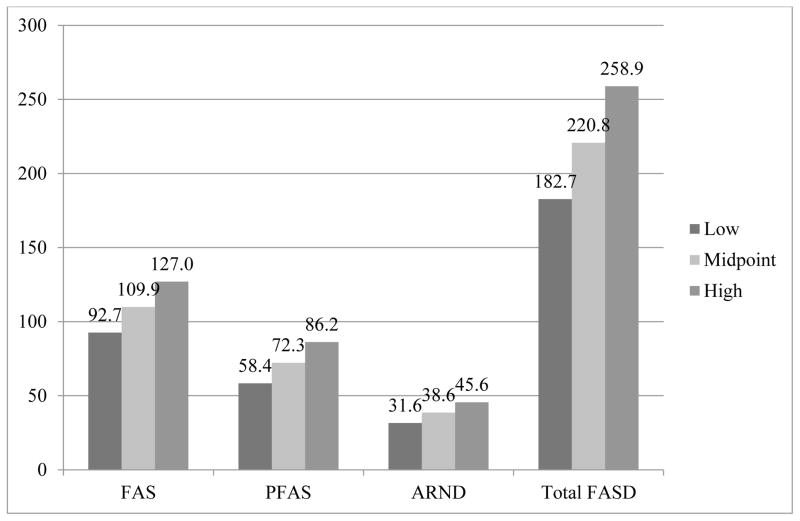
FASD children were significantly growth deficient and dysmorphic: physical measurements, cardinal facial features of FAS, and total dysmorphology scores clearly differentiated diagnostic categories from severe to mild to normal in a consistent, linear fashion. Neurodevelopmental delays were also significantly worse for each of the FASD diagnostic categories, although not as consistently linear across groups. Alcohol use is well documented as the proximal maternal risk factor for each diagnostic group. Significant distal maternal risk factors in this population are: low body weight, body mass, education, and income; and high gravidity, parity, and age at birth of the index child. In this low SES, highly rural region, FAS occurs in 93 – 128 per 1,000 children, PFAS in 58 – 86, and, ARND in 32 – 46 per 1,000. Total FASD affect 182 to 259 per 1,000 children or 18% to 26%.
Conclusions
Very high rates of FASD exist in these rural areas and isolated towns where entrenched practices of regular binge drinking co-exist with challenging conditions for childbearing and child development.
Keywords: fetal alcohol spectrum disorders (FASD), prenatal alcohol use, alcohol abuse, maternal risk for FASD, prevalence, children with FASD, South Africa
1. INTRODUCTION
1.1 Diagnosing a continuum
The diagnosis of fetal alcohol spectrum disorders (FASD) has been evolving since the first criteria for fetal alcohol syndrome (FAS) were defined by Jones and Smith (1973). Children with the most dysmorphic features and cognitive and behavioral impairments were identified as FAS. Soon thereafter, less consistent, less severe patterns of dysmorphia and impairment were recognized in animal and human studies and referred to as fetal alcohol effects (FAE; Aase, 1994; Aase et al., 1995; Clarren et al, 1978). In 1996, four specific diagnoses were developed by a committee of the Institute of Medicine (IOM): FAS, partial FAS (PFAS), alcohol-related birth defects (ARBD), and alcohol-related neurodevelopmental disorder (ARND) (Stratton et al., 1996). These four diagnoses form a continuum from the most dysmorphic to least dysmorphic and came to be known as FASD (Streisgguth and O’Malley, 2000; Warren et al., 2004). FASD are rarely diagnosed or diagnosed properly (Chasnoff et al., 2015) which colors understanding of the full spectrum of FASD. Because of this, FASD epidemiology information gathered through registries are inaccurate (Fox et al., 2015). Focused epidemiologic studies of FASD are difficult and expensive to pursue (Stratton et al., 1996). Few studies have documented the prevalence and characteristics of the full continuum of FASD, especially in the United States and Europe where FASD were believed for many years to be rare occurrences, affecting an estimated maximum of 1% of the general population (May and Gossage, 2001; Sampson et al., 1997). But recent studies indicate that FASD prevalence is much higher, 2 to 5%. At least this has found to be true in the USA, Italy, Poland, and Croatia (May et al., 2009, 2011a, 2014a, 2015; Okulicz-Kozaryn, Borkowska, Brzozka, 2015; Petković and Barišić, 2010, 2013), and especially true in South Africa.
1.2 Epidemiology studies of FASD in South Africa
Unfortunately, some communities in South Africa (ZA) have the highest general-population rates of FASD anywhere in the world. But from an epidemiologic perspective, ZA has proven to be an excellent venue for understanding the diagnosis, prevalence, characteristics, and etiology of the FASD continuum. The prevalence and characteristics of FASD have been described by the authors of this paper in four studies of a single municipality and surrounding rural areas in the western portion of the Western Cape Province (WCP) close to the Cape Town metropolitan area (May et al., 2000, 2007, 2013a; Viljoen et al., 2005). Other researchers have completed community studies in other provinces of ZA (Olivier et al, 2013; Urban et al., 2008, 2015; Viljoen et al., 2003). In the previous case control studies in the WCP, physical and neurobehavioral traits were researched extensively, the diagnostic categories have been explored with thousands of children, and research has progressed from an exclusive focus on FAS to delineating and understanding all forms of FASD. In a recent WCP study publication, FAS affected 59 – 91 per 1,000 children, PFAS 45 – 70 per 1,000, no cases of ARBD were found, and ARND affected 31 – 47 per 1,000. The total FASD rates were 135 – 208 per 1,000 or 13.5 to 20.7% (May et al., 2013a). Quite noteworthy, the prevalence of FASD was highest in rural areas surrounding the town in all previous studies in the WCP. Multiple other findings indicated that norms and practices of regular binge drinking, low socioeconomic status (SES), insufficient nutrition, high fertility, and challenging conditions for prenatal and postnatal development combine to elevate the prevalence and severity of FASD (May et al., 2005, 2008, 2013b, 2014b; Viljoen et al., 2002).
1.3 The current study
As in previous studies of the WCP, this study utilizes active case ascertainment methodology employed by a multidisciplinary field research team and pediatric geneticists/dysmorphologists. However, the four small towns and their surrounding rural areas studied here had never been studied for FASD epidemiology before. And they are more rural, remote, and lower SES than the community of previous WCP studies.
2. METHODS
2.1 Sampling and recruitment
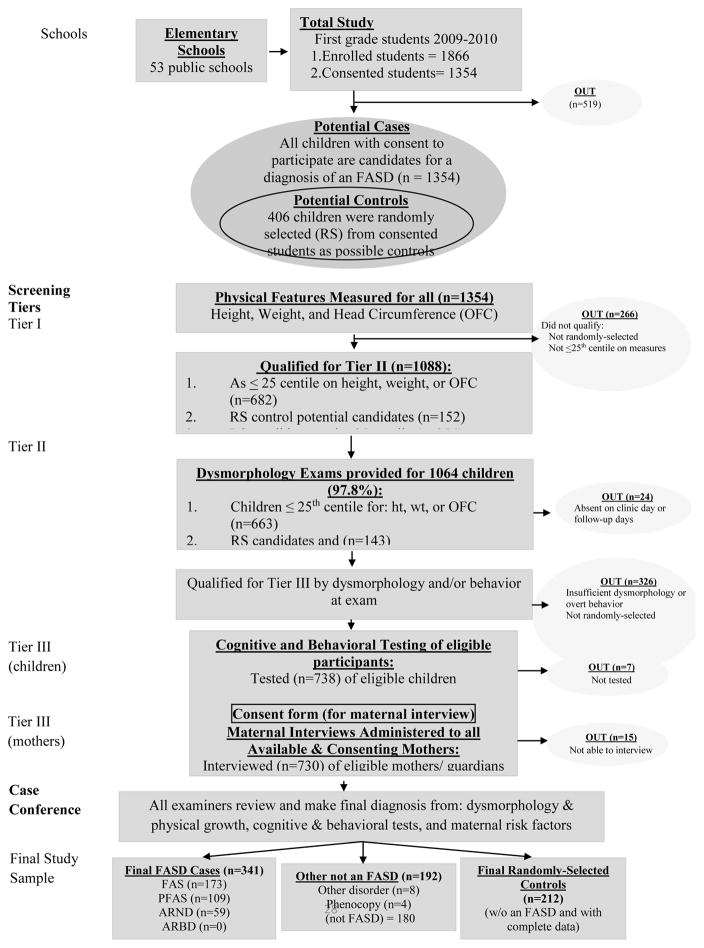
Active, written consent for children to participate in the study was sought from parents and guardians of all first grade pupils (n=1866) enrolled in all 53 primary schools of the four town region and child assent forms were obtained from all children seven years and older. Consent was received for 1,354 (72.6%). As in Figure 1, a three-tier process of screening, data collection, and diagnosis was instituted for all consented children. In Tier I all children were measured for height, weight, and head circumference. If a child was ≤25th centile on height, weight, and/or occipitalfrontal (head) circumference (OFC), he/she was advanced to Tier II which was an in-person pediatric dysmorphology exam to evaluate potential cases. In addition, 559 child enrollment numbers were picked randomly as potential controls (normal/not FASD comparison children) from all children on the school roles, and 406 had consent to participate. Each of the qualifying children (small and/or randomly-selected) was advanced to Tier II where they received the same dysmorphology exam from a dysmorphologist assisted by a scribe to record exam data. Of the children advanced to Tier III, the racial composition was generally a mirror of that of the four town region: 92.9% Coloured (mixed race), 5.6% Black, and 1.5% White.
Figure 1.
Diagnostic Guidelines for Specific Fetal Alcohol Spectrum Disorders (FASD), According to the Institute of Medicine, as Clarified by Hoyme et al., 2005
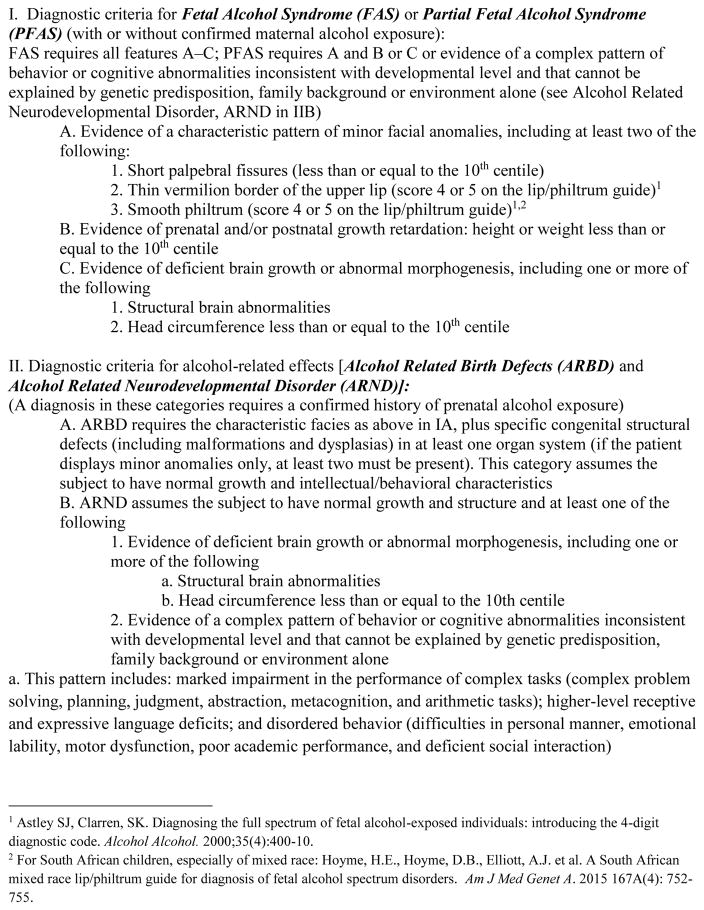
2.2 IOM diagnostic categories
The IOM diagnostic criteria of the four FASD diagnoses are presented in Figure 2 and described in more detail elsewhere (Hoyme et al., 2005, 2015). Significant growth retardation and significant dysmorphia are present in children with FAS, less growth restriction is present in children with PFAS, but at least two of the three cardinal facial features and a constellation of other minor anomalies are present in both FAS and PFAS. The clinical dysmorphic traits of FAS and PFAS have been clearly linked with prenatal alcohol exposure in thousands of cases and in multiple correlation studies (May et al., 2011b, 2013b), and these diagnoses can be made by qualified pediatricians without direct documentation of alcohol exposure, particularly after ruling out other anomalies with similar phenotypes. In previous studies in WCP communities, very seldom is it necessary to diagnose a child with FAS or PFAS without direct or strong collateral evidence of prenatal alcohol use (May et al., 2008, 2013b). Children with ARND do not have a characteristic pattern of facial characteristics, and therefore direct evidence of prenatal alcohol exposure and evidence of substantial cognitive impairment are required.
Figure 2.
Sampling Methodology for Prevalence of FASD in a Four Rural South African Communities
2.3 Assessment of cognitive and behavioral traits
In Tier III, all randomly-selected control candidates and all children with significant features common to a diagnosis within FASD were advanced to cognitive testing, and their teachers completed Achenbach Teacher Report Forms (TRF; Achenbach and Rescorla, 2001) to evaluate inattention and total behavioral issues. The tests were: Test of Reception of Grammar (TROG; Bishop, 1989) to measure verbal abilities; Raven Coloured Progressive Matrices (Raven, 1981) for non-verbal abilities; and the Digit Span subtest of the Wechsler Intelligence Scales for Children, Third Edition (WISC-III; Wechsler, 1997) to measure working memory. The tests were administered in the individual schools by blinded, contract psychometrists. Most tests were administered in Afrikaans, the dominant language of the region, although 0.4% were administered in English, and 5.4% were administered in isiXhosa for the Black African children. Centile scores from the standard charts of the Raven and the TROG respectively. Any scores falling at the 7th percentile or below were 1.5 standard deviations below the mean. The score reported for the Digit Span is a scaled score with a mean of 10 and standard deviation of 3. The two scores of the Achenbach (total problems and inattention) were scored as follows: total problem T score ≥64 fell in the clinical range and an inattention T score of ≥22 was in the clinical range.
2.4 Maternal risk factor assessment: proximal and distal variables
Also in Tier III, every child’s mother that could be located and consented was interviewed in person (96% in Afrikaans) regarding maternal risk for FASD in the index pregnancy using time-line follow back methods (Sobel et al., 1988, 2001) adapted to a specific format and questions used in all our ZA studies (May et al., 2005, 2008; Viljoen et al., 2002). Proximal variables assessed were: alcohol use by quantity, frequency, and timing during gestation of the fetus. Distal variables that influence the severity of damage in a child were also addressed: maternal height, weight, and body mass index (BMI), childbearing history; demographic and socioeconomic (SES) variables; and all questions were asked in a context of medical history and overall dietary intake (King, 1994). In previous ZA community studies, direct and presumably accurate maternal reports of prenatal alcohol use are obtained almost without exception. In this study direct reports of drinking during the index pregnancy were provided from all mothers of study children. Overall, 92% of the mothers of children with FAS, 82% of the mothers of children with PFAS, 91% of the mothers of children with ARND, and 28% of normal controls reported drinking during the index pregnancy. In a multidisciplinary case conference, data and findings from each domain (growth, dysmorphology, cognitive/behavioral performance, and maternal risk factors) were reviewed and assessed for significance by the research team members who participated in the exams, testing, and maternal interviews. After the review of the evidence and discussion, the final diagnosis was made for the child by the dysmorphologists.
2.5 Statistical analysis
Case control analysis compares results across the FASD diagnostic groups and controls. Data were processed with Excel (Microsoft, 2010) and analyzed with SPSS (IBM, 2011). Statistical significance for nominal and ordinal level data was determined using chi-square (with α = .05), and one-way analysis of variance (ANOVA) using conventional (α = .05) and Bonferroni-adjusted values as indicated on each table (Tabachnick and Fidel, 2013). With statistically significant ANOVAs, post-hoc analyses were performed using Dunnett’s C correction pairwise comparisons (α = .05). Table 4 utilizes partial correlation analysis to measure associations between maternal drinking during pregnancy and cognitive/behavioral and total dysmorphology outcomes after adjusting for household income and mother’s education.
Table 4.
Partial Correlation Coefficients (Adjusted for Square Root of Household Income and Square Root of Mother’s Education) for Developmental1 and Physical Dysmorphology Variables with Selected Maternal Drinking Measures During Pregnancy from Four Rural South African Communities
| Child Trait | Reported Drinking During Pregnancy | Drinks Per Drinking Day (log) | Drinks Per Week (log) | 3 or more Drinks Per Occasion During Pregnancy | 5 or more Drinks Per Occasion During Pregnancy | |
|---|---|---|---|---|---|---|
| Partial r | −.164 | −.162 | −.161 | −.134 | −.077 | |
| Verbal abilitya (log) | p | .001 | .001 | .001 | .006 | .116 |
| N | 427 | 428 | 426 | 415 | 415 | |
| Partial r | −.148 | −.156 | −.156 | −.179 | −.104 | |
| Non-verbal abilityb (log) | p | .002 | .001 | .001 | <.001 | .033 |
| N | 426 | 427 | 425 | 414 | 424 | |
| Partial r | −.172 | −.182 | −.158 | −.151 | −.088 | |
| WISC-IV digit span (log) | p | <.001 | <.001 | <.001 | .002 | .073 |
| N | 426 | 427 | 425 | 414 | 414 | |
| Partial r | .134 | .068 | .105 | .109 | .062 | |
| Behaviorc (sqrt) | p | .006 | .163 | .060 | .026 | .210 |
| N | 425 | 426 | 424 | 414 | 414 | |
| Partial r | .156 | .144 | .128 | .144 | .077 | |
| Inattention problems (sqrt) | p | .001 | .003 | .008 | .003 | .116 |
| N | 425 | 426 | 424 | 414 | 414 | |
| Partial r | .385 | .429 | .427 | .376 | .336 | |
| Dysmorphology score | p | <.001 | <.001 | <.001 | <.001 | <.001 |
| N | 436 | 437 | 425 | 424 | 424 | |
All scores standardized for age of child at time of testing
Tests of the Reception of Grammar (TROG).
Raven Coloured Progressive Matrices
Personal Behavior Checklist (PBCL-36).
3. RESULTS
3.1 Child physical growth and development and characteristic dysmorphology
In Table 1, mean values of study children for each salient demographic and growth variables and the three cardinal facial features for FASD are significantly different across the FASD continuum and the normal control group. Children with FASD were significantly smaller than controls on height, weight, BMI, OFC, and cardinal features of FAS: palpebral fissure length (PFL), smooth philtrum, and narrow vermillion. Age was also different among groups in the school sample; the FASD children were older because many were performing poorly and were not advanced to 2nd grade. Only the proportion male and female did not differ across groups. Significant pairwise differences between individual groups in Table 1 indicate that PFL most distinguished each group from one another, as each group was significantly different from one another with only one exception: children with PFAS and ARND. The pairwise differences for weight, BMI, and OFC were significantly different for 6 of the 9 possible comparisons, age for 5, and height for 4.
Table 1.
Children’s Demographic, Growth, Cardinal FASD Variables, and Total Dysmorphology Score from Four Rural South African Communities with Post Hoc Analysis Summary
| Variable | All Children1 | Children with FAS | Children with Partial FAS | Children with ARND | R-S Controls | Statistical Test | P |
|---|---|---|---|---|---|---|---|
| (n=1354) | (n = 173) | (n = 109) | (n =59) | (n =212) | |||
| Sex (%) | |||||||
| Males | 49.3 | 45.7 | 55.0 | 49.2 | 47.2 | χ2 = 2.484 | .478 |
| Females | 50.7 | 54.3 | 45.0 | 50.8 | 52.8 | ||
| Age (months) – Mean (SD) | 81.5 (9.1) | 86.7 (9.6) | 83.3 (8.5) | 85.3 (8.7) | 80.1 (7.7) | F = 15.712 | <.001a,c,e |
| Height (cm) – Mean (SD) | 115.4 (6.5) | 111.2 (4.9) | 114.9 (6.7) | 113.6 (6.3) | 116.5 (6.3) | F = 24.078 | <.001a,c,f |
| Weight (kg) – Mean (SD) | 20.0 (4.3) | 16.8 (2.1) | 19.70 (4.8) | 18.3 (2.8) | 20.9 (4.5) | F = 37.584 | <.001a–c,f |
| Child’s BMI – Mean (SD) | 14.9 (3.9) | 13.6 (1.2) | 14.6 (1.6) | 14.1 (1.3) | 15.3 (2.2) | F = 30.485 | <.001a–c,e,f |
| BMI Percentile – Mean (SD) | 32.7 (28.9) | 12.2 (16.9) | 25.9 (23.0) | 18.0 (20.2) | 39.9 (2.1) | F = 43.360 | <.001a,c,e,f |
| OFC (cm) - Mean (SD) | 50.5 (3.6) | 48.4 (1.4) | 50.4 (5.0) | 49.1 (1.3) | 51.1 (1.6) | F = 37.953 | <.001a–c,f |
| Palpebral Fissure Length (cm) Mean (SD) | -- | 2.25 (.14) | 2.36 (.13) | 2.37 (.12) | 2.4 (.11) | F = 48.30 | <.001a–c,e,f |
| Smooth Philtrum2 (%) | -- | 78.6 | 85.3 | 6.8 | 31.1 | χ2 = 182.155 | <.001 |
| Narrow Vermillion3 (%) | -- | 92.5 | 89.0 | 13.6 | 30.7 | χ2 = 241.833 | <.001 |
| Total Dysmorphology Score – Mean (SD) | -- | 18.63 (3.7) | 13.26 (3.8) | 11.24 (3.2) | 7.8 (4.1) | F =251.844 | <.001a–f |
The “All Children” group is not included in any of the Table 1 statistical test analyses.
Scores of 4 or 5 on Astley Lip Philtrum Guide;
Scores of 4 or 5 on Astley Lip Philtrum Guide
Bonferroni-adjusted p = .007
Significant (p<.05) post-hoc Dunnett C comparisons between:
FAS & PFAS;
FAS & ARND;
FAS & Controls;
PFAS & ARND;
PFAS & Controls
ARND & Controls
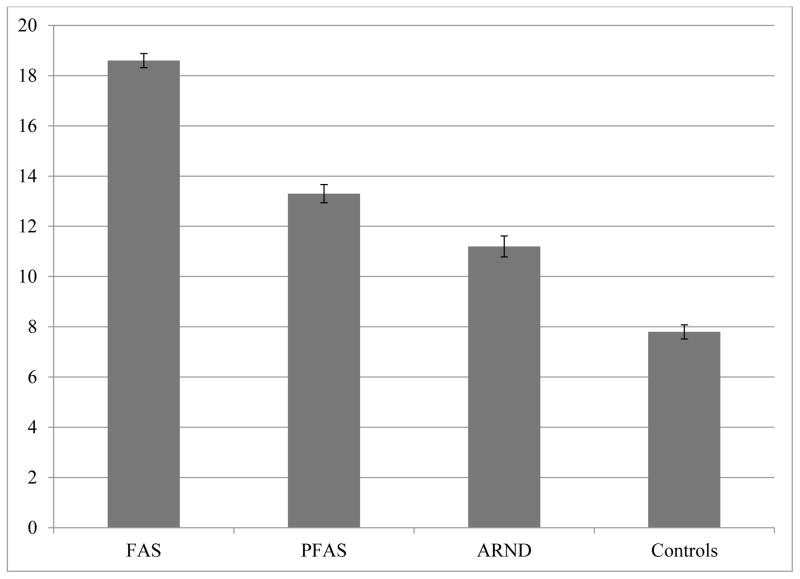
In the bottom row of Table 1, total dysmorphology score means summarize the total of FASD-relevant minor anomalies (including cardinal facial features) found in children of each group (see Hoyme et al., 2005 for an explanation of the score). Scores are significantly different across groups, with the highest values in the FAS group (18.6), PFAS (13.3) next, ARND (11.2), and the lowest in controls (7.8). Mean scores form a perfectly linear continuum across the spectrum and control group (see Figure 3). In the post-hoc analyses, each diagnostic group is significantly differentiated from the other by total dysmorphology score.
Figure 3.
Total Dysmorphology Score of FASD Diagnostic Groups and Normal Controls in Four Rural South African Communities
3.2 Cognitive and behavioral traits
The cognitive testing and behavior checklist results (Table 2) indicate a low mean achievement level for all children in these communities, and a significant statistical difference between groups with Bonferroni-adjusted values (α = .01). Mean values for the control group are best for each of the five measures. The three FASD groups perform significantly more poorly on each measure: verbal ability, non-verbal ability, Digit Span subtest for working memory, and higher scores on the Achenbach are indicative of more problems with behavior and inattention. Children with ARND perform most poorly, followed by those with FAS and then PFAS. Post-hoc analysis indicates that all tests/checklists distinguished each FASD diagnostic group from controls, but none of the FASD diagnostic groups from the other.
Table 2.
Mean Scores on Developmental and Behavioral Indicators1 of Children with FAS, PFAS, and ARND Compared to Controls from Four Rural South African Communities with Post Hoc Analyses
| FAS (n=168) | PFAS (n=109) | Children with ARND (n=59) | R-S Controls (n=203) | Test Score | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | (SD) | Mean | (SD) | Mean | (SD) | Mean | (SD) | p-value | ||
| Verbal IQ^ (percentile scores) | 11.4 | (15.1) | 13.8 | (13.6) | 10.7 | (13.7) | 26.6 | (19.9) | F=32.503 | <.001a,b,c |
| Non-verbal IQ scores+ (percentile) | 12.1 | (12.6) | 14.4 | (13.4) | 11.6 | (12.4) | 22.8 | (17.9) | F=13.497 | <.001a,b,c |
| WISC-IV Digit-Span Scaled Score† | 3.2 | (2.4) | 3.7 | (2.5) | 2.9 | (2.2) | 5.5 | (2.8) | F=32.610 | <.001a,b,c |
| Achenbach Teacher Report Form (TRF) Total Problem Score | 39.1 | (28.9) | 37.3 | (31.3) | 42.5 | (23.1) | 25.6 | (24.2) | F=10.862 | <.001a,b,c |
| Achenbach TRF Inattention Score | 18.4 | (12.4) | 15.9 | (13.3) | 20.1 | (10.1) | 10.5 | (10.3) | F=18.664 | <.001a,b,c |
All scores standardized for age of child at time of testing.
Test of Reception of Grammar (TROG). A measure of verbal intelligence.
Raven Coloured Progressive Matrices. A measure of nonverbal intelligence.
WISC-IV Digit Span Scaled Score – mean of 10 and standard deviation of 3.
Bonferroni-adjusted value = 0.01
Significant (p<.05) post-hoc Dunnett C comparisons between:
FAS & Controls;
PFAS & Controls;
ARND & Controls
3.3 The proximal maternal risk variable – alcohol use during the index pregnancy
Table 3 presents measures of alcohol consumption by mothers during the index pregnancies and at interview. Among the mothers of normal controls, 28% of them drank during the index pregnancy; 72% abstained. Levels of drinking reported by the mothers of controls who drank were generally as low or lower than the mothers of children with ARND and substantially lower than mothers of children with FAS or PFAS. Mothers of children with FAS drank the most on every prenatal measure of alcohol use, more than any other group. Among the mothers of children with FAS, 92% reported drinking during the index pregnancy; they drank averages of: 16.2 drinks per week, 6.5 drinks per drinking day. Eighty-four percent reported bingeing three or more drinks per occasion and 66% five or more per occasion. Drinking frequency and quantities were less among mothers of children with PFAS and ARND.
Table 3.
Maternal Demographic, Childbearing, Socioeconomic, Drinking, Tobacco, and Other Drug Use from Four Rural South African Communities: Mothers of Children with FASD and Normal Controls
| Maternal Variables | Mothers of Children with FAS (n=168) | Mothers of Children with Partial FAS (n=106) | Mothers of Children with ARND (n=59) | RS Control Children (n=212) | Statistical Test | df | P |
|---|---|---|---|---|---|---|---|
| Alcohol Consumption Variables* | |||||||
| Drinking during pregnancy | 92.4 (133/145) | 81.6 (80/98) | 90.9 (50/55) | 28.5 (59/207) | χ2 = 193.022 | 3 | <.001 |
| Avg # drinks per week (during pregnancy) | 16.2 (20.0) | 11.4 (19.5) | 8.5 (9.8) | 2.7 (8.9) | F=23.359 | 3 | <.001 |
| Drinks per drinking day during pregnancy – Mean (SD) | 6.5 (7.9) | 4.1 (5.1) | 3.5 (3.5) | .90 (2.8) | F = 32.693 | 3 | <.001 |
| Consumed 3 drinks or more per occasion during pregnancy (%) | 84.0 (122/144) | 71.4 (70/98) | 78.6 (44/56) | 23.5 (46/196) | χ2 = 262.594 | 3 | <.001 |
| Consumed 5 drinks or more per occasion during pregnancy (%) | 66.0 (96/144) | 58.2 (57/98) | 46.4 (26/56) | 14.3 (28/196) | χ2 = 106.927 | 3 | <.001 |
| Current drinker (%) | 54.8 (85/155) | 44.4 (44/99) | 53.7 (29/54) | 26.7 (55/206) | χ2 = 36.425 | 3 | <.001 |
| Drinking before index pregnancy (%) | 90.4 (133/146) | 80.4 (82/102) | 94.4 (51/54) | 37.9 (78/206) | χ2 = 143.052 | 3 | <.001 |
| Drank during 1st trimester (%) | 91.0 (131/144) | 81.6 (80/98) | 90.9 (50/55) | 28.0 (58/149) | χ2 = 190.587 | 3 | <.001 |
| Drank during 2nd trimester (%) | 80.0(116/ 145) | 61.2 (60/98) | 67.3 (37/55) | 15.0 (31/207) | χ2 = 164.000 | 3 | <.001 |
| Drank during 3rd trimester (%) | 68.3 (99/145) | 49.0 (48/98) | 59.3 (32/54) | 12.1 (25/207) | χ2 = 125.717 | 3 | <.001 |
| Tobacco Use | |||||||
| Used tobacco during index pregnancy (%) | 81.9 (127/155) | 81.7 (85/104) | 79.3 (46/58) | 39.6 (80/202) | χ2 = 94.979 | 3 | <.001 |
| Current smoker, smoked within week (%) | 85.6 (107/125) | 84.9 (73/86) | 85.1 (40/47) | 75.7 (78/103) | χ2 = 4.673 | 3 | .197 |
| Quantity of cigarettes smoked per week among smokers (each cigarette = 1 gram) | 32.5 (31.2) | 32.3 (26.8) | 27.0 (14.8) | 27.70 (17.3) | F=.897 | 3 | .443 |
| Other drug use during pregnancy (% Yes) | 1.9 | 0.0 | 0.0 | 1.0 | χ2 = | 3 | .373 |
| Demographics** | |||||||
| Age at pregnancy (yrs) – Mean (SD) | 28.7 (6.5) | 26.2 (6.5) | 27.9 (7.4) | 26.9 (6.8) | F = 3.729 | 3 | .011 |
Partial correlation analysis was completed to measure associations between maternal drinking and cognitive/behavioral measures and total dysmorphology scores after adjusting for household income and mother’s education (Table 4). Transformations were undertaken for most measures due to positive skewness. Logarithmic transforms were applied to number of drinks per drinking day, average number of drinks per week, verbal and non-verbal IQ, and digit span performance. Square root transformations were applied to behavior and inattention problems, income, and education. Although highly unbalanced, transformations could not be applied to “yes/no” items: reported drinking during pregnancy and the two measures of binge drinking. A statistical criterion of p < .008 was set to control for Type I familywise error rate.
All three measures of drinking during pregnancy (drank during pregnancy, drinks per drinking day, and drinks per week) correlate significantly with the three cognitive scores: Verbal and non-verbal IQ and Digit Span performance are significantly lower when drinking occurs during pregnancy (all p < .008). Several of the relationships between drinking during pregnancy and behavior measures are positive and statistically significant at the p < .008 level: Behavior problems and inattention with drinking during pregnancy and inattention with number of drinks per drinking day. However, none of these partial correlations are particularly strong once adjusted for socioeconomic measures, with r ranging from −.148 to −.182. Thus each drinking variable accounts for only about 3% of the variance in the child’s scores. The remaining behavioral measures also show indications of positive relationships but fail to meet the strict statistical criterion.
The binge drinking measure of 3+ drinks per occasion correlates significantly with all cognitive and behavioral measures in the expected direction except for behavior problems, which although in the expected direction fails to meet the strict statistical criterion. The binge drinking measure of 5+ drinks per occasion is not significantly related to any of the cognitive or behavioral measures, possibly as a result of attenuation due to the very small number of women who report doing so. Again, the signs of the (very small) correlations are all in the expected direction.
Maternal drinking measures correlate most highly with total dysmorphology score after adjusting for income and education: drinking during pregnancy (r =.385), drinks per drinking day (r =.429), drinks per week (r =.427), 3 or more drinks per occasion (r =.376) and 5 or more drinks per occasion (r =.336). More prenatal drinking is strongly associated with more minor anomalies/dysmorphology, even after adjusting for socioeconomic status.
3.4 Tobacco use
A significantly higher percentage of FASD mothers reported smoking during the index pregnancy and at the time of the interview (Table 3). The quantity of cigarette consumption by smokers did not differ across groups. A high percentage of women smoke, but average quantity is relatively low. Use of drugs other than alcohol was virtually non-existent and not significantly different among groups.
3.5 Distal maternal risk traits – physical, childbearing, and demographic
Distal risk variables in the third section of Table 3 are those which have been found to increase risk for FASD in mothers using alcohol prenatally. Lower maternal weight, low BMI, low educational achievement, and low income are all significantly more common in the FASD groups than controls. Furthermore, high gravidity and parity, and older age at the birth of the index child are significantly more common among mothers of children with FASD. Also, more children with FASD were from rural areas.
3.6 Prevalence estimates by three methods, their calculation, and the final estimates
The final diagnoses of the individual children in the entire consented sample are presented in Table 5, section 1, far left side. No cases of ARBD were found. There were 173 children diagnosed with FAS, 109 with PFAS, and 59 with ARND.
Table 5.
Prevalence Rates (per 1,000) of Individual Diagnoses within Fetal Alcohol Spectrum Disorders and Total FASD by Three Methods of Estimation from Rural ZA Communities
| Oversample of children ≤ 25th centile on height, weight, or OFC |
Random Sample Rate and Estimated Cases in the Non- Consented Children (n=406) |
Combined rate from consented sample (n=1354) and estimated cases in non- consented sample (n=512) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Diagnosis | (a) n |
Enrolled rate1 (n=1866) |
Consented rate2 (n=1354) |
n | Proportion of FASD cases in random sample |
(b) Estimated cases in non- consented sample (n=512) |
Rate of FASD from random sample only3 |
95% Confidence Interval |
(a + b) Total estimated cases (n=1866) |
Estimated rate for all enrolled students4 |
95% Conference Intervals |
| FAS | 173 | 92.7 | 127.7 | 51 | .1256 | 64 | 125.6 | 96.4 to 153.6 | 237 | 127.0 | 111.9 to 142.1 |
| PFAS | 109 | 58.4 | 80.5 | 41 | .1009 | 52 | 100.9 | 75.4 to 127.7 | 161 | 86.2 | 73.5 to 99.0 |
| ARND | 59 | 31.6 | 43.5 | 21 | .0517 | 26 | 51.7 | 31.8 to 69.8 | 85 | 45.6 | 36.1 to 55.0 |
| Total FASD | 341 | 182.7 | 251.8 | 113 | .2783 | 142 | 278.3 | 238.5 to 316.1 | 483 | 258.9 | 238.9 to 278.7 |
Denominator is all children attending first grade in local schools. Rate per 1,000 based on the entire enrollment in 1st grade classrooms (n=1866).
Denominator is the total number of children with consent to participate in this study. Rate per 1,000 based on the sample consented and screened (n=1354).
Calculated as the FASD cases diagnosed from the randomly-selected control candidates (numerator) over the total number of randomly-selected children x 1,000.
Rate per 1,000 children calculated from FASD cases diagnosed in the consented sample (a) added to the estimated cases in the non-consented sample utilizing the proportional diagnostic distribution of FASD cases among randomly-selected children (b), and divided by all 1st grade children enrolled in the schools (n=1866).
The first prevalence estimation is summarized in the left section of Table 5. With this technique, two different denominators were used: the number of children enrolled in 1st grade classes at all community schools (n=1866) for the low estimate, and the total number with consent to participate in this study (n=1354) for the upper estimate. The assumption is that oversampling small children provided the greatest probability of including most children with FAS or PFAS. The rate of FAS with this technique is 92.7 – 127.7 per 1,000, and the rate of total FASD is 182.7 – 251.8 per 1,000.
Alternatively, a second rate was calculated from the 113 cases of FASD found within the 406 children who entered the study via random selection as candidates for the normal comparison/control group (middle section of Table 5). The rates of FAS and total FASD from this technique are: 125.6 FAS cases per 1,000 (95% CI = 96.4 to 153.6) and total FASD rate is 278.3 per 1,000 (95% CI = 238.5 to 316.1) with this technique.
The third rate (Table 5, right section) was calculated by estimating the total number of cases which would likely have been found in the unconsented children and adding these estimated cases to the cases among the consented children. Using the proportions of FASD diagnoses in the random sample (technique 2) to estimate the number of cases among the 512 unconsented children and adding them to the cases diagnosed in the consented population. Technique 3 estimates the rate of FAS to be 127 per 1,000 and total FASD rate as 258.9 per 1,000 or 25.9%. Ninety-five percent confidence intervals make the range of FASD with this technique 238.9 to 278.7 per 1,000.
4. DISCUSSION
4.1 Summary findings in these rural communities
The physical, cognitive, and behavioral traits of the children with FASD and the controls in highly rural, low SES communities of the WCP are similar to those found in other population-based studies of FASD in the WCP, yet the traits are more prevalent and severe and the prevalence of FASD higher. Child physical variables of growth and development and many minor anomalies in this sample were clearly categorized in a linear fashion by the diagnostic categories of the revised IOM criteria. No cases of ARBD were found within this population which has been common in our experience with population-based and clinical studies, as cases of ARBD are extremely rare. That is, when prenatal alcohol use is substantial enough to cause any detectable physical anomalies, alcohol exposure to the fetus has been of sufficient quantity and duration to also cause other physical anomalies, cognitive delays, and/or behavioral problems that qualify the child for the other diagnoses within the spectrum: FAS, PFAS, or ARND. Some child traits were, however, more severe in these four communities (e.g., depressed cognitive performance, physical growth, and higher dysmorphology scores) than we have found elsewhere in the WCP using identical sampling and diagnostic methods. FASD prevalence is indeed higher than in other studies in this province. And as in our other studies in ZA, this research has once again clearly and empirically linked child traits of concern, especially dysmorphology, to detailed maternal reports of prenatal alcohol use, even which SES confounders are controlled.
Additionally, many distal variables of maternal risk were similar in this study to previous studies in the WCP. The findings regarding maternal risk indicated that less than optimal maternal health (e.g., low BMI) and SES (e.g., maternal education), and other challenging prenatal, postpartum, and environmental conditions for child growth and development yielded a higher prevalence of the most severe forms of FASD in these four communities. In similar studies in the United States we find more cases of ARND (the least dysmorphic form of FASD) per children with FAS and PFAS, most likely due to less prevalent and regular binge drinking and more favorable health and SES conditions for the mothers and children (May et al., 2014a, 2015). For example, virtually all mothers in the study communities of the WCP have been found to be undernourished (May et al., 2014b).
4.2 Prevalence estimates
The prevalence estimates from the three techniques do not vary widely. The highest rates were produced from the random sample alone (technique 2) where total FASD is 258.9 per 1,000 or 25.9% and 95% confidence intervals indicate a range of 238.5 to 316.1 per 1,000 children. But our research team with both clinical and epidemiologic experience feels that this is likely an overestimate that does not adequately capitalize on the fact that the most dysmorphic children are smaller and most accurately diagnosed.
The final low and high estimates that we present (Figure 4) are conservative and produced from a combination of all three techniques. The low estimate originates from technique 1, and utilizes as the numerator all of the cases diagnosed among all consented children. The denominator of this estimate is the total number of children enrolled in all first grade classes in the region. This assumes that the oversampling of small children (≤ 25th centile on height, weight, and/or head circumference) has maximized case finding of the most probable candidates for FAS and PFAS diagnoses. Therefore, using the entire student population as a denominator yields the low prevalence rate of 182.7 FASD per 1,000 or 18.3%.
Figure 4.
Prevalence of FASD Diagnostic Groups and Controls in Four Rural South African Communities
The high estimate of 258.9 per 1,000 is from technique 3 which uses extrapolation to estimate the cases likely to be found in the unconsented population. Taking the proportion of cases of FASD discovered in the randomly-selected sample (technique 2) and projecting it to the 519 children who were not consented into the study yields 113 additional cases. Adding this number to those diagnosed in the consented population provides the numerator. The overall high estimate of FASD prevalence is 258.9 per 1,000 or 25.9%.
Therefore, the final FASD prevalence rate that we feel is most accurate is 182.7 to 258.9 per 1,000 children or 18.3% to 25.9%.
4.3 Linking all parts of the study to prenatal alcohol use
Keeping in mind that all individual parts of the study (dysmorphology exams, testing, and maternal interviews) were performed blinded by professionals in their individual disciplines, the linking of the different domains for the final diagnosis is important. Furthermore, it is vital to link the traits and diagnoses of the children to the maternal use of alcohol in the prenatal period. This was accomplished very effectively by direct maternal report in over 90% of the FASD cases and in the remaining cases by collateral reports from relatives, neighbors, and other propinqutous and knowledgeable individuals during the time of the index pregnancy. The correlation analysis further links drinking to child traits. The more drinking during pregnancy, especially binge drinking or quantity of drinks per occasion, the more minor anomalies are detected in the children and the poorer their performance on the cognitive and behavioral measures. The latter association of drinking and neurobehavioral performance, however, is not as strong. We have demonstrated elsewhere with multivariate structural models and data from other samples (May et al., 2011b, 2013c) dysmorphology correlates most highly with drinking. The distal maternal risk variables studied once again appear to cause additional individual variation in child outcomes in this sample (over and above that caused by alcohol use alone), and as evidenced in the FASD maternal groups, if on the wrong end of the distal maternal risk variables, they often increase the severity of child outcomes.
4.4 Strengths and limitations
The strengths of this study are substantial. 1) A very high participation rate among children (72.6%) and their mothers (over 95%) 2) The study utilized a randomly-selected, fully screened, normal comparison/control group from the same community which ensured relevant and accurate comparisons of groups on all outcome variables. 3) Complete dysmorphology exams were coupled with cognitive testing and behavioral checklists for all children in the final sample. 4) Detailed, direct reports of prenatal alcohol use by quantity, frequency and timing of consumption were linked to actual child outcomes. 5) Multiple distal maternal risk factors were determined from direct, in-person interviews and were linked to specific child outcomes. 6) Three standard demographic/epidemiologic techniques were used to estimate prevalence. These included the use of both oversampling of the small, higher risk children and also random sampling techniques to determine overall risk in the non-consented population. Convergence of the prevalence estimates was substantial which lends credence to the final estimates.
Limitations of this study are as follows. 1) Since the population of these communities is rather unique in racial, ethnic, and cultural traits, extrapolating the exact values and findings directly to non-South African populations might be difficult and perilous for some of the variables (e.g. precise amounts of alcohol that pose severe risk to the fetus in another population). 2) Maternal interviews were administered to the mothers 7 years post-partum and recall may have been negatively affected for some maternal risk variables. 3) Without accurate alcohol biomarker samples administered to the interviewed mothers, it is impossible to know exactly how precise and accurate the reporting is. 4) Basing much of the initial study sample on child growth and development and dysmorphology, the prevalence of ARND is likely under-evaluated and under-estimated in the final results. However, an exception to a low ARND rate may be found using random-selection rates only (technique #2). 5) Finally, administering a more extensive battery of cognitive tests and behavioral instruments would have been desirable to more fully describe the behavioral phenotype of the children, but time and monetary resources made this impractical to impossible.
4.5 Conclusions
The rate of FASD in these four towns and surrounding rural areas is the highest ever documented in a general population study. A historical and common pattern of recreational drinking on the weekends, coupled with poverty and low SES conditions, combine for a breathtakingly high rate of FASD. The traits of children with FAS, PFAS, and ARND are clearly different from one another and from normal controls on most every child physical, developmental, and behavioral trait, and on multiple maternal risk variables in this population. The rate of FAS of 93 to 128 per 1,000 is extremely high as are the rates of PFAS and ARND. Total FASD of 18 to 26% is quite sadly the highest prevalence ever found or reported for a general population in the world.
Research Highlights.
High rates of fetal alcohol spectrum disorders (FASD) found in rural communities.
Fetal alcohol syndrome prevalence is 93 – 127 per 1,000 children.
FASD prevalence is 18.2% – 25.9%.
Alcohol is clearly linked to poor physical and behavioral outcomes in children.
Maternal risk factors are low BMI and SES; and high gravidity, parity, and age.
Acknowledgments
Role of the funding source
Funding was provided by the National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism (NIAAA) (UO1 AA15134).
We thank all of the parents who gave their permission for their children to participate in the study, the Department of Education and teachers who approved the study and supported us and the children, parents who consented their children into the study, children who participated in the study at each of the schools, and all of the mothers who provided information for the maternal risk portion this study. We are especially indebted to the fantastic field work staff for this study. Alitha Pithey was the lead project officer in the field office of the four communities. Project officers were: Isobel, Botha, Avil Surney and Irene Van Scheltinga and Leandi Matthep skill in locating and transporting subjects was invaluable.
Protocols and consent forms used were approved by the University of New Mexico (Medical School HRRC 96-209 and 00-422, and Main Campus IRB 9625), the Ethics Committee of Stellenbosch University, Faculty of Health Sciences, and the University of Cape Town.
Footnotes
Conflict of interests
None of the authors have any conflicts of interest to declare.
Contributors
Philip May was the principle investigator of the NIH grant that funded this research and he, in collaboration with Julie Hasken and Barbara Tabachnick on final data analysis and table preparation, was the major writer and final editor of all drafts. Anna-Susan Marais was the program manager who supervised all data and protocols in the main office at the Faculty of Medicine and Health Sciences of Stellenbosch University. Marlene de Vries, one of the program officers in the field office of the study communities, oversaw all final data compilation in the field program offices, including contributing greatly to final data quality and manuscript preparations. Wendy Kalberg supervised data entry, files, and data sets in the United States. Colleen Adnams and Wendy Kalberg designed and oversaw the cognitive testing and behavioral checklist data collection in the field and the analysis of results for diagnosis and manuscript preparation. Eugene Hoyme, Luther Robinson, Melanie Manning, Derek Hoyme, and Kenneth Jones generated all dysmorphology data for the team in the field and made final diagnoses of the children in multidisciplinary case conferences. Soraya Seedat and Charles Parry are the South African co-investigators who participated in the design and facilitated all study activities in South Africa both in the field and at Stellenbosch University. Each author contributed to, read, edited, and approved various drafts of the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aase JM. Clinical recognition of FAS: difficulties of detection and diagnosis. Alcohol Health Res. 1994;18:5–9. [PMC free article] [PubMed] [Google Scholar]
- Aase JM, Jones KL, Clarren SK. Do we need the term “FAE”? Pediatrics. 1995;95:428–430. [PubMed] [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms and profiles. University of Vermont, Research Center for Children, Youth & Families; Burlington, VT: 2001. [Google Scholar]
- Bishop DVM. Test of Reception of Grammar (TROG) 2. University of Manchester; Manchester: 1989. [Google Scholar]
- Chasnoff IJ, Wells AM, King L. Misdiagnosis and missed diagnoses in fosters and adopted children with prenatal alcohol exposure. Pediatrics. 2015;135:264–270. doi: 10.1542/peds.2014-2171. [DOI] [PubMed] [Google Scholar]
- Clarren SK, Smith DW. The fetal alcohol syndrome. N Engl J Med. 1978;11:1063–1067. doi: 10.1056/NEJM197805112981906. [DOI] [PubMed] [Google Scholar]
- Fox DJ, Pettygrove S, Cunniff C, O’Leary LA, Gilboa SM, Bertrand J, Druschel CM, Breen A, Robinson L, Ortiz L, Frias JL, Ruttenber M, Klumb D, Meaney J. Fetal alcohol syndrome among children aged 7–9 years – Arizona, Colorado, and New York, 2010. MMWR. 2015;64:54–57. [PMC free article] [PubMed] [Google Scholar]
- Hoyme HE, Hoyme DB, Elliott AJ, Blankenship J, Kalberg WO, Buckley D, Abdul-Rahman O, Adam MP, Robinson LK, Manning MA, Bezuidenhout H, Jones KL, May PA. A South African mixed race lip/philtrum guide for diagnosis of fetal alcohol spectrum disorders. Am J Med Genet A. 2015;167A:752–755. doi: 10.1002/ajmg.a.37023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyme HE, May PA, Kalberg WO, Kodituwakku P, Gossage JP, Trujillo PM, Buckley DG, Miller J, Khaole N, Viljoen DL, Jones KL, Robinson LK. A practical clinical approach to diagnosis of fetal alcohol spectrum disorders: clarification of the 1996 Institute of Medicine criteria. Pediatrics. 2005;115:39–47. doi: 10.1542/peds.2004-0259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM. SPSS Statistics for Windows, 2011. Version 20.0. IBM Corp; Armonk, NY: [Google Scholar]
- Jones KJ, Smith DW. Recognition of the fetal alcohol syndrome in early infancy. Lancet. 1973;302:999–1001. doi: 10.1016/s0140-6736(73)91092-1. [DOI] [PubMed] [Google Scholar]
- King AC. Enhancing the self-report of alcohol consumption in the community: two questionnaire formats. Am J Public Health. 1994;84:294–296. doi: 10.2105/ajph.84.2.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Keaster C, Bozeman R, Goodover J, Blankenship J, Kalberg WO, Buckley D, Brooks M, Hasken J, Gossage JP, Robinson LK, Manning M, Hoyme HE. Prevalence and characteristics of fetal alcohol syndrome and partial fetal alcohol syndrome in a Rocky Mountain Region City. Drug Alcohol Depend. 2015;155:229–127. doi: 10.1016/j.drugalcdep.2015.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Baete A, Russo J, Elliott AJ, Blankenship J, Kalberg WO, Buckley D, Brooks M, Hasken J, Abdul-Rahman O, Adam MP, Robinson LK, Manning M, Hoyme HE. Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics. 2014a;134:855–866. doi: 10.1542/peds.2013-3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Hamrick KJ, Corbin KD, Hasken J, Marais AS, Brooke LE, Blankenship J, Hoyme HE, Gossage JP. Dietary intake, nutrition, and fetal alcohol spectrum disorders in the Western Cape Province of South Africa. Reprod Toxicol. 2014b;46:31–39. doi: 10.1016/j.reprotox.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Blankenship J, Marais AS, Gossage JP, Kalberg WO, Barnard R, De Vries M, Robinson LK, Adnams CM, Buckley D, Manning M, Jones KL, Parry CDH, Hoyme HE, Seedat S. Approaching the prevalence of the full spectrum of fetal alcohol spectrum disorders in a South African population-based study. Alcohol Clin Exp Res. 2013a;37:818–830. doi: 10.1111/acer.12033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Blankenship J, Marais AS, Gossage JP, Kalberg WO, Joubert B, Cloete M, Barnard R, de Vries M, Hasken J, Robinson LK, Adnams CM, Buckley D, Manning M, Parry CD, Hoyme HE, Tabachnick BG, Seedat S. Maternal alcohol consumption producing fetal alcohol spectrum disorders (FASD): quantity, frequency, and timing of drinking. Drug Alcohol Depend. 2013b;133:502–512. doi: 10.1016/j.drugalcdep.2013.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Tabachnick B, Gossage JP, Kalberg WO, Marais AS, Robinson LK, Manning M, Blankenship J, Buckley D, Hoyme HE, Adnams C. Maternal factors predicting cognitive and behavioral characteristics of children with fetal alcohol spectrums disorders. J Dev Behav Pediatr. 2013c;34:314–325. doi: 10.1097/DBP.0b013e3182905587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Fiorentino D, Coriale G, Kalberg WO, Hoyme HE, Aragon AS, Buckley D, Stellavato C, Gossage JP, Robinson LK, Jones KL, Manning M, Ceccanti M. Prevalence of children with severe fetal alcohol spectrum disorders in communities near Rome, Italy: new estimated rates are higher than previous estimates. Int J Env Res Public Health. 2011a;8:2331–2351. doi: 10.3390/ijerph8062331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Tabachnick BG, Gossage JP, Kalberg WO, Marais AS, Robinson LK, Manning M, Buckley D, Hoyme HE. Maternal risk factors predicting child physical characteristics and dysmorphology in Fetal Alcohol Syndrome and Partial Fetal Alcohol Syndrome. Drug Alcohol Depend. 2011;119:18–27. doi: 10.1016/j.drugalcdep.2011.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Gossage JP, Kalberg WO, Robinson LK, Buckley D, Manning M, Hoyme HE. Prevalence and epidemiologic characteristics of FASD from various research methods with an emphasis on recent in-school studies. Dev Disabil Res Rev. 2009;15:176–192. doi: 10.1002/ddrr.68. [DOI] [PubMed] [Google Scholar]
- May PA, Gossage JP, Marais AS, Hendricks LS, Snell CL, Tabachnick BG, Stellavato C, Buckley DG, Brooke LE, Viljoen DL. Maternal risk factors for fetal alcohol syndrome and partial fetal alcohol syndrome in South Africa: a third study. Alcohol Clin Exp Res. 2008;32:738–753. doi: 10.1111/j.1530-0277.2008.00634.x. [DOI] [PubMed] [Google Scholar]
- May PA, Gossage JP, Marais AS, Adnams C, Hoyme HE, Jones KL, Robinson LK, Khaole NC, Snell C, Kalberg WO, Hendricks L, Brooke L, Stellavato C, Viljoen DL. The epidemiology of fetal alcohol syndrome and partial FAS in a South African community. Drug Alcohol Depend. 2007;88:259–271. doi: 10.1016/j.drugalcdep.2006.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Brooke LE, Gossage JP, Snell C, Hendricks L, Croxford J, Marais AS, Viljoen DL. Maternal risk factors for Fetal Alcohol Syndrome in the Western Cape Province of South Africa: a population-based study. Am J Public Health. 2005;95:1190–1199. doi: 10.2105/AJPH.2003.037093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA, Brooke LE, Gossage JP, Croxford J, Adnams C, Jones KL, Robinson LK, Viljoen D. The epidemiology of Fetal Alcohol Syndrome in a South African community in the Western Cape Province. Am J Public Health. 2000;90:1905–1912. doi: 10.2105/ajph.90.12.1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Microsoft Excel. Microsoft; Redmond, WA: 2010. [Google Scholar]
- Okulicz-Kozaryn K, Borkowska M, Brzozka K. FASD prevalence among schoolchildren in Poland. J App Res Intellect Disabil. 2015 doi: 10.1111/jar.12219. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Oliver L, Urban M, Chersich M, Temmerman M, Vijoen D. Burden of fetal alcohol syndrome in a rural West Coast area of South Africa. S Afr Med J. 2013;103:402–405. doi: 10.7196/samj.6249. [DOI] [PubMed] [Google Scholar]
- Petković G, Barišić I. FAS prevalence in a sample of urban schoolchildren in Croatia. Reprod Toxicol. 2010;29:237–272. doi: 10.1016/j.reprotox.2009.11.006. [DOI] [PubMed] [Google Scholar]
- Petković G, Barišić I. Prevalence of fetal alcohol syndrome and maternal characteristics in a sample of schoolchildren from a rural province of Croatia. Int J Environ Res Public Health. 2013;10:1547–1561. doi: 10.3390/ijerph10041547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raven J. Research Supplement No.1: The 1979 British Standardisation Of The Standard Progressive Matrices And Mill Hill Vocabulary Scales, Together With Comparative Data From Earlier Studies In The UK, US, Canada, Germany And Ireland. Harcourt Assessment; San Antonio, TX: 1981. Manual for Raven’s Progressive Matrices and Vocabulary Scales. [Google Scholar]
- Sampson PD, Streissguth AP, Bookstein FL, Little RE, Clarren SK, Dehaene P, Hanson JW, Graham JM. Incidence of fetal alcohol syndrome and prevalence of alcohol-related neurodevelopmental disorder. Teratology. 1997;56:317–326. doi: 10.1002/(SICI)1096-9926(199711)56:5<317::AID-TERA5>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- Stratton KR, Howe CJ, Battaglia FC. Fetal Alcohol Syndrome Diagnosis, Epidemiology, Prevention, And Treatment. Institute Of Medicine. National Academy Press; Washington, D.C: 1996. [Google Scholar]
- Streissguth AP, O’Malley K. Neuropsychiatric implications and long-term consequences of fetal alcohol spectrum disorders. Sem Clin Neuropsychol. 2000;47:177–190. doi: 10.1053/scnp.2000.6729. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Agrawal S, Annis H, Ayala-Velazquez H, Echeverria L, Leo GI, Rybakowski JK, Sandahl C, Saunders B, Thomas S, Zioikowski M. Cross-cultural evaluation of two drinking assessment instruments: alcohol timeline followback and inventory of drinking situations. Subst Use Misuse. 2001;36:313–331. doi: 10.1081/ja-100102628. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: assessing normal drinker’s reports of recent drinking and a comparative evaluation across several populations. Br J Addict. 1998;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 6. Pearson; Boston, MA: 2013. [Google Scholar]
- Urban M, Chersich F, Fourie LA, Chetty C, Olivier L, Viljoen D. Fetal alcohol syndrome among grade 1 schoolchildren in Northern Cape Province: prevalence and risk factors. S Afr Med J. 2008;98:877–880. [PubMed] [Google Scholar]
- Urban MF, Olivier L, Viljoen D, Lombard C, Louw JG, Drotsky LM, Temmerman M, Chersich MF. Prevalence of fetal alcohol syndrome in a South African city with a predominantly Black African population. Alcohol Clin Exp Res. 2015;39:1016–1026. doi: 10.1111/acer.12726. [DOI] [PubMed] [Google Scholar]
- Viljoen DL, Gossage JP, Adnams C, Jones KL, Robinson LK, HE, Snell C, Khaole N, Asante KK, Findlay R, Quinton B, Brooke LE, May PA. Fetal Alcohol Syndrome epidemiology in a South African community: a second study of a very high prevalence area. J Stud Alcohol. 2005;66:593–604. doi: 10.15288/jsa.2005.66.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viljoen D, Hymbaugh K. Fetal Alcohol syndrome---South Africa, 2001. MMWR. 2003;52:660–662. [PubMed] [Google Scholar]
- Viljoen D, Croxford J, Gossage JP, Kodituwakku PW, May PA. Characteristics of mothers of children with fetal alcohol syndrome in the Western Cape Province of South Africa: a case control study. J Stud Alcohol. 2002;63:6–17. [PubMed] [Google Scholar]
- Warren K, Floyd L, Calhoun F, et al. Consensus Statement on FASD. National Organization on Fetal Alcohol Syndrome; Washington, DC: 2004. [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children. 3. Psychological Corporation; San Antonio, TX: 2003. [Google Scholar]