Abstract
Background
Several studies have linked marijuana use with a variety of health outcomes among young adults. Information about marijuana’s long-term health effects is critically needed.
Methods
Data are from a ten-year study of 1,253 young adults originally recruited as first-year college students and assessed annually thereafter. Six trajectories of marijuana use during college (Non-Use, Low-Stable, Early-Decline, College-Peak, Late-Increase, Chronic) were previously derived using latent variable growth mixture modeling. Nine health outcomes assessed in Year 10 (modal age 27) were regressed on a group membership variable for the six group trajectories, holding constant demographics, baseline health status, and alcohol and tobacco trajectory group membership.
Results
Marijuana trajectory groups differed significantly on seven of the nine outcomes (functional impairment due to injury, illness, or emotional problems; psychological distress; subjective well-being; and mental and physical health service utilization; all ps<.001), but not on general health rating or body mass index. Non-Users fared better than the Late-Increase and Chronic groups on most physical and mental health outcomes. The declining groups (Early-Decline, College-Peak) fared better than the Chronic group on mental health outcomes. The Late-Increase group fared significantly worse than the stable groups (Non-Use, Low-Stable, Chronic) on both physical and mental health outcomes.
Conclusions
Even occasional or time-limited marijuana use might have adverse effects on physical and mental health, perhaps enduring after several years of moderation or abstinence. Reducing marijuana use frequency might mitigate such effects. Individuals who escalate their marijuana use in their early twenties might be at especially high risk for adverse outcomes.
Keywords: Cannabis, health care utilization, health outcomes, longitudinal studies, mental health, physical health
1. Introduction
Marijuana use is highly prevalent, with approximately one in ten U.S. adults and one-third of college students having used during the past year (Johnston et al., 2014; Substance Abuse and Mental Health Services Administration, 2014). Recent legislative trends toward decriminalization and legalization have been accompanied by declining perceptions of marijuana’s harmfulness (Johnston et al., 2014; Substance Abuse and Mental Health Services Administration, 2014). Given that emerging adulthood is a critical developmental stage with respect to identity exploration and establishing long-term adult roles, the consequences of marijuana use during this period could be substantial and enduring (Arnett, 2005). Young adulthood is also the peak developmental period for marijuana use and related problems (Substance Abuse and Mental Health Services Administration, 2014).
Public perceptions notwithstanding, abundant research evidence from both cross-sectional and longitudinal studies supports the association between marijuana use and a variety of psychosocial and health outcomes, especially when use begins early or is frequent, although not all studies have controlled for potential confounds such as alcohol and tobacco use (for reviews, see Hall, 2015; Joshi et al., 2014; Thomas et al., 2014). For example, marijuana use has been linked to psychosis (Di Forti et al., 2015; Di Forti et al., 2009; Fergusson et al., 2005; Hall, 2015; Henquet et al., 2005; Moore et al., 2007; van Os et al., 2002), bipolar disorder (Lagerberg et al., 2014), and major depression (Juon et al., 2011; Lynne-Landsman et al., 2010). The apparent dose-response relationship is particularly concerning given the increasing potency of marijuana during the past several decades (Mehmedic et al., 2010). Marijuana’s physical health effects include respiratory outcomes such as chronic bronchitis, airway inflammation, and decreased pulmonary function (Joshi et al., 2014; Tashkin, 2013), as well as increased risk for cardiovascular disease and acute cardiac events (Jouanjus et al., 2014; Mittleman et al., 2001; Mukamal et al., 2008; Thomas et al., 2014). Accordingly, some evidence indicates that health care utilization is higher for frequent marijuana users than non-users, namely for respiratory illness and injuries, even when excluding tobacco smokers (Polen et al., 1993).
Studies using group-based trajectory modeling can provide a more complete picture of the association between marijuana use patterns during adolescence and health outcomes in young adulthood. Despite methodological differences (e.g., frequency measures, age ranges, number of trajectory groups), certain commonalities emerge from the existing research utilizing this method. Most include a group that abstains from marijuana use, a group that consistently uses infrequently, and a group that consistently uses at high frequencies (Brook et al., 2013; Caldeira et al., 2012; Homel et al., 2014; Schulenberg et al., 2005). Many studies also identified groups with increasing or decreasing frequency of use over time (Brook et al., 2013; Caldeira et al., 2012; Ellickson et al., 2004; Schulenberg et al., 2005) or with different ages of onset (Flory et al., 2004).
In these studies, the trajectory groups that abstain from marijuana use throughout adolescence and young adulthood generally fare best in terms of education, employment, health, and social outcomes (Brook et al., 2013; Caldeira et al., 2012; Ellickson et al., 2004; Flory et al., 2004; Homel et al., 2014; Schulenberg et al., 2005). In contrast, the chronic trajectory groups generally exhibit poor outcomes related to employment and finances (Brook et al., 2013), education (Homel et al., 2014), alcohol and tobacco use (Schulenberg et al., 2005), and mental health (Brook et al., 2011; Caldeira et al., 2012). Even among an “early high” trajectory group (i.e., frequent use at age 13 that declined and stabilized by age 18), self-ratings of overall health at age 29 were significantly lower relative to the other trajectory groups (Ellickson et al., 2004). Nevertheless, few studies have examined young adult outcomes related to physical and mental health, and more comprehensive measures of these outcomes are needed. Additionally, previous studies have been limited in their ability to account for alcohol and tobacco use, which covary with marijuana use (Jackson et al., 2008).
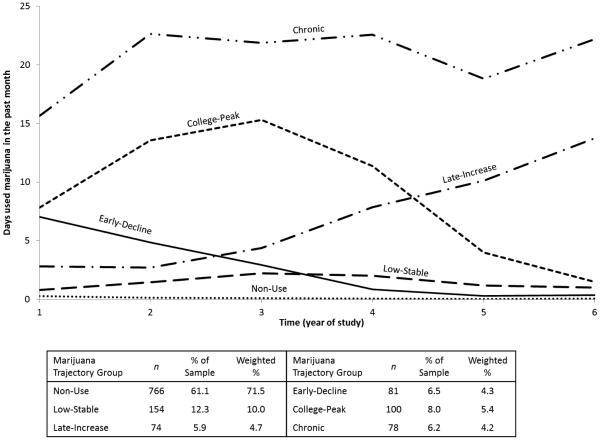
The present study builds on our team’s prior work examining health outcomes in young adulthood in relation to marijuana use trajectories during college (Caldeira et al., 2012). Among a sample of 1,253 college students studied over seven years, we identified six distinct trajectories of marijuana use frequency spanning the first six years of the study (see Figure 1), which—as noted above—were significantly associated with several health outcomes in the seventh year, even after adjusting for baseline health status, demographics, alcohol use, and tobacco use. The present study aims to extend this prior research to evaluate what, if any, relationship might exist between marijuana use trajectory group membership during college and self-reported health outcomes measured in Year 10 (i.e., nine years post-matriculation). An important goal of this work was to replicate our earlier models to understand whether the observed associations with certain health outcomes would persist as participants approached age 30. We hypothesized that marijuana trajectory group membership would be significantly associated with health outcomes in Year 10, even after accounting for alcohol and tobacco use, demographics, and baseline health status.
Figure 1.
Marijuana use trajectories (N=1,253).
This figure was originally printed in Caldeira, K.M., O'Grady, K.E., Vincent, K.B., Arria, A.M. (2012). Marijuana use trajectories during the post-college transition: Health outcomes in young adulthood. Drug and Alcohol Dependence. 125(3), 267-275. doi:10.1016/j.drugalcdep.2012.02.022.
2. Methods
2.1. Study design
Data were collected as part of the College Life Study, which followed a cohort of 1,253 individuals originally recruited in 2004 as incoming freshmen at one large public university (Arria et al., 2008; Vincent et al., 2012). After screening the entire incoming class of students ages 17 to 19 (82% response rate), a sample was selected for longitudinal follow-up, with oversampling of individuals who used an illicit drug at least once during high school. Baseline and annual follow-up assessments through Year 8 included a personal interview and self-administered questionnaires. Follow-up assessments were scheduled throughout the academic year (i.e., September through May) to coincide approximately with each individual’s baseline anniversary. A 30-minute web-based assessment was conducted in Year 10. Participants were paid for each assessment. Follow-up rates were excellent, with 74% of the original cohort completing the Year 10 assessment. The study was approved by the university’s IRB. Informed consent was obtained. Interviewers were trained extensively in procedures for maintaining confidentiality.
2.2. Participants
The analysis sample consisted of the 932 individuals (43% male, 73% white, 5% Hispanic) who completed the Year 10 assessment (modal age 27). Attrition was significantly higher for men than women (34% vs. 18%, p<.001) but did not differ significantly by race, parental education, or marijuana trajectory group membership. Mean neighborhood income of family of origin was slightly higher among non-responders (76.7K vs. 72.3K, p<.05).
2.3. Measures
2.3.1. Marijuana, alcohol, and tobacco trajectory groups
As described by Caldeira et al. (2012), latent variable growth mixture modeling was used to identify six distinct trajectories of marijuana use, based on the annual observations of past-month marijuana use frequency from Year 1 (2004-2005) through Year 6 (2009-2010) of the study (see Figure 1). Similar procedures were used to identify seven alcohol trajectory groups and five tobacco trajectory groups. For each substance, models were fit assuming a Poisson distribution using PROC TRAJ (Jones and Nagin, 2007) in SAS 9.2 (SAS Institute Inc., 2008). Three separate categorical variables were created to represent trajectory group membership for marijuana, alcohol, and tobacco use frequency, respectively (see Caldeira et al., 2012).
2.3.2. Baseline alcohol quantity
In Year 1 participants were asked the number of drinks they would have on a typical drinking day.
2.3.3. Year 10 marijuana, tobacco, and alcohol use
Frequencies were assessed for marijuana use and tobacco cigarette smoking during the past month (0-30 days) and alcohol consumption during the past year (0-365 days).
2.3.4. General health outcomes
At both baseline and Year 10, participants rated their current health as excellent, good, fair, or poor (Wells et al., 1988). Responses were later dichotomized as excellent or not excellent (i.e., good, fair, and poor). Self-reported weight and height were used to compute body mass index (BMI) following the standard formula for adults. BMI values were then dichotomized as overweight/obese or normal/underweight, using the standard cutoff value of 25.0 (Centers for Disease Control and Prevention, 2012).
2.3.5. Year 10 mental health
The 12-item General Health Questionnaire (GHQ) measures psychological distress, with higher scores representing a higher level of distress symptoms. It was scored using standard methods (Goldberg and Williams, 1988) for a possible range of 0-36.
2.3.6. Year 10 life satisfaction
The Satisfaction with Life Scale (SWLS; Diener et al., 1985), a general measure of global life satisfaction, has previously exhibited convergent validity with other measures of subjective well-being. Its five items are each scored on a seven-point Likert scale, with total scores ranging from 5-35. Internal consistency was acceptable for both the SWLS and GHQ (Cronbach’s α≥.89 in this sample).
2.3.7. Year 10 physical and mental health service utilization
Participants were asked how many times they visited a health professional during the past year for (1) problems with their physical health and (2) problems with their “emotions, nerves, or mental health.” We abbreviate these constructs as physical health visits and mental health visits.
2.3.8. Year 10 functional impairment
Participants were asked how many days during the past year they were limited in their usual activities due to (1) “an accident or injury,” (2) “an illness or physical condition,” and (3) “an emotional problem or trouble with your nerves.” We abbreviate these constructs as injury days, illness days, and emotion days.
2.3.9. Demographics
Sex, race, and ethnicity (Hispanic, non-Hispanic) were self-reported. Race was dichotomized as white vs. non-white due to the preponderance of white individuals (73%). As a proxy for socioeconomic status of the family of origin, neighborhood income of participants’ home during high school was approximated using publicly available data on the mean adjusted gross income for their ZIP code (MelissaDATA, 2003).
2.4. Statistical analyses
A series of ordinary least squares and Poisson regressions were conducted to examine the association between the six-group marijuana trajectory variable and each of the nine health outcomes. We assumed a Poisson distribution for the count variables (physical and mental health visits; impairment days due to illness, injury, or emotional problems), a normal distribution for the scale variables (SWLS, GHQ), and a binomial distribution for the dichotomous variables (general health rating, BMI). The four control variables (sex, race, ethnicity, parents’ neighborhood income) were included as additional predictors, as were the baseline alcohol quantity variable, a baseline health variable corresponding to the Year 10 health outcome, and the alcohol and tobacco trajectory group variables. For six of the outcomes tested (SWLS, mental health visits, physical health visits, illness days, injury days, and emotion days), no equivalent baseline measure was available, and therefore baseline GHQ score was used as a proxy for overall health. For models in which the overall Wald χ2 value for the marijuana trajectory group variable was statistically significant (p<.05), all possible pairwise comparisons between the groups were evaluated with Bonferonni correction for multiple comparisons. To facilitate interpretation of the results of such comparisons, estimated marginal means were tabulated for each outcome that was significantly associated with the marijuana trajectory group variable.
3. Results
3.1. Health outcomes at Year 10
Among the overall sample at Year 10, approximately one-third (34%) rated their health as “excellent” and 58% rated their health as “good.” Approximately half visited a health provider for physical health problems at least once during the past year (52%) or had at least one day when their usual activities were limited by illness (46%). Fewer visited a provider for mental health problems (16%) or had their usual activities limited by an emotional problem (13%). Limiting usual activities due to an accident and/or an injury was reported by 16%.
3.2. Marijuana use in Year 10
Marijuana use data from Year 10 suggest that relative levels of use did not change appreciably between the end of the trajectory interval in Year 6 and the Year 10 follow-up (see Table 1). Marijuana use remained highly prevalent in the Chronic (88%) and Late-Increase (87%) trajectory groups, and members of these groups used more frequently, on average, than users in the other groups. A high degree of variability in marijuana use was seen among the College Peak group, with only half (50%) continuing their marijuana use in Year 10. The large standard deviations in the Chronic, Late-Increase, and College-Peak groups reflect the presence of many individuals with daily or near-daily use patterns (i.e., 50.0%, 26.9%, and 9.0%, respectively, who used marijuana 200 or more times during the past year). Data on alcohol and tobacco use in Year 10 are provided in Table 1.
Table 1.
Sample characteristics, by marijuana trajectory group membership (N=932)a
| Total (N=932) |
Non-Use (n=568) |
Low-Stable (n=121) |
Early-Decline (n=65) |
College-Peak (n=78) |
Late-Increase (n=52) |
Chronic (n=48) |
|
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Demographic and Control Variables | |||||||
| % male | 48.5% | 41.9% | 48.1% | 58.0% | 62.0% | 68.9% | 67.9% |
| % White | 73.1% | 68.9% | 75.3% | 85.2% | 80.8% | 77.0% | 83.3% |
| % Hispanic | 4.7% | 4.8% | 6.5% | 4.9% | 3.1% | 4.1% | 2.6% |
| Mean (SD) parents’ neighborhood income during high school |
7.3 (3.4) | 7.1 (3.3) | 7.4 (3.3) | 7.5 (3.4) | 7.5 (3.7) | 7.5 (3.4) | 8.5 (4.1) |
| Mean (SD) typical alcohol quantity (Year 1) |
4.9 (2.7) | 4.3 (2.6) | 5.0 (2.5) | 6.3 (3.4) | 6.1 (2.6) | 5.1 (2.3) | 6.2 (2.6) |
| Year 10 Substance Use | |||||||
| % drank alcohol during past year | 95.6% | 93.7% | 99.2% | 98.5% | 98.7% | 96.2% | 100.0% |
| Mean (SD) days/year alcohol use, among past-year drinkers |
104.3 (81.8) | 91.2 (75.0) | 130.3 (83.0) | 93.9 (70.7) | 131.1 (86.9) | 128.5 (100.4) | 129.3 (101.0) |
| Mean (SD) drinks/day, among past-year drinkers |
2.7 (1.6) | 2.5 (1.6) | 2.8 (1.2) | 2.9 (1.4) | 3.1 (1.6) | 3.0 (1.6) | 3.1 (1.5) |
| % smoked tobacco during past year | 24.8% | 15.3% | 33.9% | 26.2% | 42.3% | 51.9% | 54.2% |
| Mean (SD) days/year tobacco use, among past-year tobacco smokers |
87.1 (124.0) | 81.3 (123.7) | 47.7 (83.5) | 60.6 (100.2) | 89.7 (112.5) | 138.4 (156.9) | 129.4 (147.0) |
| % used marijuana at least once during past year | 34.8% | 17.4% | 61.2% | 38.5% | 50.0% | 86.5% | 87.5% |
| % high-frequency marijuana use (≥200 days/year) |
5.5% | 0.5% | 1.7% | 1.5% | 9.0% | 26.9% | 50.0% |
| Mean (SD) days/year marijuana use, among past-year users |
68.0 (110.1) | 21.4 (52.0) | 27.9 (61.1) | 28.8 (62.2) | 70.9 (98.7) | 122.0 (124.1) | 211.4 (145.6) |
Marijuana trajectory group membership is based on the annual observations of past-month marijuana use frequency during Years 1 through 6.
3.3. Overall multiple regression predicting Year 10 health outcomes
As shown in Table 2, marijuana trajectory group membership was significantly associated with seven of the nine health outcome variables tested, after controlling for the effects of demographics (i.e., sex, race, ethnicity, neighborhood income), baseline alcohol quantity, health status (i.e., GHQ score, general health rating, BMI), and the alcohol and tobacco trajectory group variables. Specifically, statistically significant differences were observed among the marijuana trajectory groups on GHQ and SWLS scores, numbers of visits for physical and mental health problems, and number of impairment days due to illness, emotional problems, and injuries. Marijuana trajectory group membership was not significantly associated with health rating or BMI.
Table 2.
Results of multiple regression analyses predicting nine different Year 10 health outcomes (N=932)
| Mental Health Outcome Variables | Physical Health Outcome Variables | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Wald χ2 for each explanatory variable |
df | GHQ | SWLS | Mental health visits |
Emotion days |
Physical health visits |
Illness days |
Injury days |
Excellent Health Rating |
BMI ≥ 25.0 |
| Sex | 1 | 2.78 | 254.68*** | 100.76** | 39.43*** | 14.29*** | 150.58*** | 13.16*** | 0.71 | 18.57*** |
| Race | 1 | 170.13*** | 279.20*** | 8.19** | 70.94*** | 24.49*** | 112.92*** | 0.09 | 3.50 | <0.01 |
| Ethnicity | 1 | 0.31 | 0.76 | 7.11** | 41.00*** | 6.24* | 9.20** | 53.70*** | 0.02 | <0.01 |
| Neighborhood income during high school |
1 | 7.74** | 66.41*** | 98.85*** | 17.56*** | 0.05 | 30.05*** | 0.34 | 0.84 | 0.31 |
| Baseline health | 1 | 602.16*** | 305.18*** | 364.78*** | 139.22*** | 3.26 | 5.41* | 0.01 | 32.35*** | 171.75*** |
| Baseline alcohol quantity | 1 | 29.30*** | 34.07*** | 15.35*** | 0.91 | 2.40 | 2.40 | 40.19*** | 0.07 | 0.78 |
| Alcohol trajectory group | 6 | 33.75*** | 397.64*** | 218.14*** | 249.05*** | 95.71*** | 447.39*** | 407.97*** | 6.43 | 2.02 |
| Tobacco trajectory group | 4 | 121.03*** | 413.21*** | 19.70** | 80.87*** | 20.52*** | 117.38*** | 188.54*** | 15.93** | 1.37 |
| Marijuana trajectory group | 5 | 93.77*** | 668.49*** | 386.40*** | 277.08*** | 87.79*** | 512.60*** | 271.58*** | 6.77 | 6.31 |
p<.05;
p <.01;
p<.001
Note. The baseline health variable was equivalent to the corresponding outcome variable for Year 10 health rating, BMI, and GHQ. For all other outcomes, the baseline GHQ served as the control variable.
3.4. Rationale for presentation of multiple comparisons
Table 3 displays the results of all possible pairwise comparisons for the seven health outcomes that were significantly associated with marijuana trajectory group membership. We selected a series of comparisons to highlight due to their potential public health significance. First, we compare the Non-Use group with all other groups. Second, we compare the groups whose marijuana use declined (College-Peak, Early Decline) to the groups whose use remained high or stable (Chronic, Low-Stable). Third, we compare the Late-Increase group to the two “stable use” groups (Chronic, Low-Stable). For each set of comparisons, we report results first for the mental health outcomes, followed by physical health outcomes.
Table 3.
Estimated marginal means (standard errors) from the seven statistically significant multiple regression analyses predicting Year 10 health outcomes on the basis of marijuana trajectory group membership (N=932)
| Mental Health Outcome Variables |
Physical Health Outcome Variables |
||||||
|---|---|---|---|---|---|---|---|
| GHQ | SWLS | Mental health visits |
Emotion days |
Physical health visits |
Illness days |
Injury days |
|
|
|
|
||||||
| Non-Use | 10.78 (0.11)b | 24.94 (0.11) | 0.23 (0.04)b | 0.39 (0.05)a | 0.91 (0.09)a | 1.47 (0.11)a | 1.46 (0.13)a,b |
| Low-Stable | 10.30 (0.13)a | 24.47 (0.13)a | 0.39 (0.06)a | 0.44 (0.07)a,b | 0.88 (0.11)a | 1.56 (0.14)a,b | 2.71 (0.25)c |
| Early-Decline | 10.63 (0.15)a,b | 23.88 (0.15)b | 0.44 (0.08)a,c | 0.71 (0.11)b,c | 1.19 (0.16)a,b | 1.86 (0.18)a,b,c | 0.95 (0.11)d |
| College-Peak | 9.58 (0.14) | 26.71 (0.14) | 0.36 (0.07)a,b,c | 0.30 (0.07)a | 1.69 (0.20)b,c | 2.06 (0.20)b,c | 1.58 (0.16)a |
| Late-Increase | 10.59 (0.17)a,b | 22.34 (0.17) | 1.06 (0.18)d | 2.10 (0.29) | 1.75 (0.23)b,c | 5.89 (0.48) | 2.68 (0.27)c |
| Chronic | 10.90 (0.17)b | 24.02 (0.17)a,b | 1.15 (0.19)d | 0.93 (0.16)c | 2.05 (0.27)c | 2.39 (0.25)c | 1.12 (0.14)b,d |
Note. Results reported as estimated marginal means, adjusting for Year 1 GHQ score, sex, race, ethnicity, neighborhood income, alcohol trajectory group membership, tobacco trajectory group membership, and baseline alcohol quantity. Groups sharing a superscripted letter within a given column are not significantly different (p>.05).
3.5. Comparisons between non-users and other marijuana trajectory groups
Relative to the Non-Use group, the Chronic, Late-Increase, and Early-Decline groups each fared significantly worse on the SWLS, mental health visits, and emotion days, but did not differ significantly on GHQ. The Low-Stable group had significantly worse (i.e., lower) scores on the SWLS and more mental health visits than the Non-Use group, but slightly better (i.e., lower) GHQ scores. The College-Peak group had better SWLS and GHQ scores than the Non-Use group, but did not differ on emotion days or mental health visits.
Compared with the Non-Use group, the Chronic and College-Peak groups fared significantly worse on illness days and physical health visits but did not differ on injury days. Conversely, the Low-Stable group had significantly more injury days than the Non-Use group, but did not differ on illness days or physical health visits. The Early-Decline group reported significantly fewer injury days than the Non-Use group, but did not differ on illness days or physical health visits. The Late-Increase group fared significantly worse than the Non-Use group on all three measures.
3.6. Comparisons between decreasing and stable marijuana trajectory groups
Relative to the Chronic group, both the College-Peak and Early-Decline groups reported significantly fewer mental health visits. The Early-Decline group did not differ from the Chronic group on emotion days, SWLS, or GHQ. The College-Peak group fared significantly better than the Chronic group on each of the mental health outcomes we tested. Relative to the Low-Stable group, the College-Peak group scored significantly better on the SWLS and GHQ, but did not differ on emotion days or mental health visits. Conversely, the Early-Decline group scored significantly worse on the SWLS, compared with the Low-Stable group, but did not differ on emotion days, mental health visits, or GHQ.
The College-Peak group reported significantly more injury days than the Chronic group, but did not differ on illness days or physical health visits. By contrast, the Early-Decline group fared significantly better than the Chronic group on physical health visits, but did not differ on illness or injury days. Relative to the Low-Stable group, the College-Peak group had significantly fewer injury days but more physical health visits, and did not differ on illness days. The Early-Decline group also had significantly fewer injury days than the Low-Stable group, and did not differ on illness days or physical health visits.
3.7. Comparisons between late-increasers and stable marijuana trajectory groups
The Late-Increase group fared significantly worse than the Chronic group on emotion days and SWLS score, but did not differ on mental health visits. Compared with the Low-Stable group, the Late-Increase group fared worse on emotion days, SWLS score, and mental health visits. The Late-Increase group had similar GHQ scores to both the Chronic and Low-Stable groups.
The Late-Increase group reported significantly more illness and injury days than the Chronic group, but did not differ on physical health visits. Compared with the Low-Stable group, the Late-Increase group fared significantly worse on illness days and physical health visits, but did not differ on injury days.
3.8. Post-hoc analysis
The models on GHQ and SWLS were replicated with dichotomous variables derived based on previously established cutoffs of <15 for the SWLS, denoting high levels of dissatisfaction (Diener, 2006) and >2 for the GHQ, using the alternative 0 to 12 scoring method (Goldberg and Williams, 1988). As in the original models, the variables on alcohol and tobacco trajectory group membership, baseline alcohol quantity, baseline GHQ, and demographics were held constant. The marijuana trajectory group variable was not significantly associated with probability of high GHQ score (p=.364), which was estimated at 30% for the overall sample. Estimated probability of low SWLS score was 6% for the Non-Use group, 7% for College-Peak, 12% for both Low-Stable and Chronic, and 16% for Early-Decline (overall p=.014), although none of the pairwise comparisons were statistically significant.
4. Discussion
In this study of young adults assessed annually for ten years since college entry, the trajectory of students’ marijuana use patterns during and immediately following college was significantly associated with seven health outcomes measured in their late 20s, even after accounting for background risk factors and concomitant rates of change in alcohol and tobacco use. Whereas an earlier report on this sample documented marijuana-related differences in health outcomes in Year 7 (Caldeira et al., 2012), the present findings indicate that many of those differences persisted in Year 10. Results were largely consistent with prior findings in that the Non-Use group tended to exhibit the best health outcomes, while the Chronic and Late-Increase groups tended to fare the worst.
Overall, individuals who followed a trajectory of minimal or non-use of marijuana during the first six years of the study had significantly better health outcomes than most of the other marijuana trajectory groups. Importantly, these health outcome differences encompassed measures of functional impairment due to illness, injuries, and emotional problems, health service utilization for physical and mental health problems, and subjective well-being. Although more subtle than typical morbidity and mortality measures, these types of measures have particular utility in a high-functioning young adult population because they might be indicative of early stages of developing more serious health problems. We cannot say whether any of the observed differences might be considered clinically significant, yet the differences in service utilization alone highlight the potential for substantial long-term personal and economic impacts of marijuana use.
In this sample, individuals whose marijuana use declined over time appeared to have better mental health outcomes than their counterparts who maintained stable marijuana use trajectories. This was particularly true of the College-Peak group, which fared better than the Chronic group on all four of the mental health measures tested, and better than the Low-Stable group on the SWLS and GHQ. Results support and extend prior evidence by Schulenberg et al. (2005) who observed that individuals who decreased their use by their early 20s (the “Fling” group) fared better than others who increased their use during young adulthood on measures of education, employment, and financial independence. Research on the mental health status of individuals in recovery would be highly informative to confirm whether or not mental health problems are reduced following sustained periods of abstinence. Alternatively, although we accounted for the influence of many baseline characteristics, we cannot rule out the possibility that results could be attributable to unmeasured third factors associated with both psychological well-being and resilience to becoming dependent on marijuana.
While the focus of the present study was on the possible longer-term impact of earlier patterns of marijuana use during college, it is possible that substance use during the intervening years might contribute to the variation in health outcomes. Future research with college students should examine the continuity of patterns of use from college through adulthood in relation to health outcomes.
Results are consistent with prior studies (Ellickson et al., 2004; Flory et al., 2004) that emphasize that early age of marijuana use initiation is associated with a greater likelihood of negative outcomes, relative to individuals with later onset of use. In the present study, individuals who established a heavier use pattern earlier in life (i.e., Early-Decline group) fared worse than those with onset during college (i.e., College-Peak group), even though both groups later reduced their use. Although both of these groups exhibited better mental health outcomes compared with those who did not reduce their use (i.e., Chronic group), the advantages were less pronounced among those with an earlier onset.
The finding that the Late-Increase group exhibited particularly poor health outcomes relative to all other groups—including the Chronic group—supports and extends prior research on the relationship between late-onset marijuana use and mental health problems such as depression (Brook et al., 2011; Juon et al., 2011). Schulenberg et al. (2005) found that individuals with no or low use at age 18 who increased their marijuana use through young adulthood experienced a range of adjustment difficulties, while Flory et al. (2004) found that late-onset marijuana users who continued to increase their use were more dysfunctional and had worse psychosocial outcomes than non-users. These results suggest that a later age of onset might not protect marijuana users from adverse mental health outcomes, and might be a marker for declining psychological functioning. Confirming these findings is particularly important given that young adulthood is the peak period of risk for onset of many psychiatric disorders.
Additional research is also critically needed to understand how increasing marijuana use during this period might contribute to increased risk for physical health problems. Physical health outcomes in the Late-Increase group were as bad as or worse than in the Chronic and Low-Stable groups. Although this study provides no evidence of causality, it is plausible that sustained and increasing marijuana use patterns might contribute to deteriorating health status. It is also plausible that marijuana use might increase after—or even because of—the onset of a chronic physical or mental illness. Some evidence indicates that adolescents with physical disabilities and chronic health problems are at increased risk for marijuana use (Jones and Lollar, 2008).
The growing availability and acceptance of marijuana for medicinal purposes in the U.S. lends urgency to the need for a rigorous research agenda aimed at understanding the extent to which marijuana use during young adulthood might undermine health and well-being, even when it is being used for ostensibly therapeutic purposes. Moreover, the increasing acceptance of marijuana and low perceived risk might create a scenario in which individuals with a chronic mental health condition choose to use marijuana as a therapeutic option rather than seeking conventional medical care.
Findings must be interpreted in light of the study’s limitations. Generalizability to students at other colleges or in other geographic regions is unknown, but is likely to be reasonably good for students at other large public universities with comparable levels of marijuana use. Despite having established and maintained rapport and trust with the cohort throughout a decade of assessments, we cannot say how the results might have differed if health outcomes had been assessed via interview rather than online survey. Clinical health assessments were not conducted, and some of the observed differences in health outcomes were modest. Nevertheless, the fact that present findings are largely consistent with findings from a similar set of health outcomes assessed three years earlier suggests that the observed differences in health outcomes are meaningful. We found no evidence of attrition bias in relation to marijuana trajectory group membership, yet we cannot rule out the possibility that individuals with worse health outcomes might have been underrepresented at Year 10. It is possible that the present findings might underestimate the true magnitude of any relationships between marijuana use trajectories and health outcomes. Finally, because of our prospective focus, marijuana use that was concurrent with the observed health outcomes was not a focus of this research; studies describing the post-college marijuana use trajectories in this sample are forthcoming.
Future research using prospective designs with even larger samples should include other potential moderators and mediators of the association between marijuana use and health outcomes. For example, it is plausible that transient withdrawal symptoms, such as disrupted sleep and changes in mood, experienced by individuals with a chronic pattern of marijuana use might partially account for differences in self-reported acute health problems or exacerbate underlying health issues. Moreover, background variables that might influence risk for trajectory group membership could be included in such future studies to gain a more complete understanding of the processes by which marijuana influences health outcomes.
This study illustrates the utility of group-based trajectory modeling for understanding the relationships between marijuana use patterns and subsequent health outcomes. An important strength is our longitudinal design with high follow-up rates even after ten years, as well as our ability to account for trajectories of alcohol and tobacco use, which tend to covary with marijuana use (Gray et al., 2011; Jackson et al., 2008). The ability to examine a diverse set of both physical and mental health outcome measures, which are complementary to the assessment batteries of prior studies, strengthens our confidence in the contribution of the present findings to the broader literature on marijuana and health outcomes.
Findings highlight the possibility that the longer-term health effects of frequent marijuana use might be mitigated if students successfully cut back on their use. College is an opportune time to identify and intervene with individuals who have a prior history of marijuana use during adolescence to prevent further escalation of use, or to prevent others from initiating use. Increasing college students’ recognition of how their marijuana use affects their health and functioning—and convincing them that intervention is warranted—poses a major challenge even among individuals who meet criteria for marijuana dependence (Caldeira et al., 2009). Even if abstinence is not immediately achieved, the present findings support the possibility that health outcomes might be significantly improved by reductions in use over time. Results highlight the potential importance of developing and evaluating efficacious intervention strategies to prevent the escalation of marijuana use.
References
- Arnett JJ. The developmental context of substance use in emerging adulthood. J Drug Issues. 2005;35:235–253. doi:10.1177/002204260503500202. [Google Scholar]
- Arria AM, Caldeira KM, O'Grady KE, Vincent KB, Fitzelle DB, Johnson EP, Wish ED. Drug exposure opportunities and use patterns among college students: Results of a longitudinal prospective cohort study. Subst Abus. 2008;29:19–38. doi: 10.1080/08897070802418451. doi:10.1080/08897070802418451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook JS, Lee JY, Brown EN, Finch SJ, Brook DW. Developmental trajectories of marijuana use from adolescence to adulthood: Personality and social role outcomes. Psychol Rep. 2011;108:339–357. doi: 10.2466/10.18.PR0.108.2.339-357. doi:10.2466/10.18.PR0.108.2.339-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook JS, Lee JY, Finch SJ, Seltzer N, Brook DW. Adult work commitment, financial stability, and social environment as related to trajectories of marijuana use beginning in adolescence. Subst Abus. 2013;34:298–305. doi: 10.1080/08897077.2013.775092. doi:10.1080/08897077.2013.775092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldeira KM, Kasperski SJ, Sharma E, Vincent KB, O’Grady KE, Wish ED, Arria AM. College students rarely seek help despite serious substance use problems. J Subst Abuse Treat. 2009;37:368–378. doi: 10.1016/j.jsat.2009.04.005. doi:10.1016/j.jsat.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldeira KM, O'Grady KE, Vincent KB, Arria AM. Marijuana use trajectories during the post-college transition: Health outcomes in young adulthood. Drug Alcohol Depend. 2012;125:267–275. doi: 10.1016/j.drugalcdep.2012.02.022. doi:10.1016/j.drugalcdep.2012.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Defining adult overweight and obesity. 2012 http://www.cdc.gov/obesity/adult/defining.html. Accessed on June 25, 2015.
- Di Forti M, Morgan C, Dazzan P, Pariante C, Mondelli V, Marques TR, Handley R, Luzi S, Russo M, Paparelli A, Butt A, Stilo SA, Wiffen B, Powell J, Murray RM. High-potency cannabis and the risk of psychosis. Br J Psychiatry. 2009;195:488–491. doi: 10.1192/bjp.bp.109.064220. doi:10.1192/bjp.bp.109.064220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Forti M, Marconi A, Carra E, Fraietta S, Trotta A, Bonomo M, Bianconi F, Gardner-Sood P, O'Connor J, Russo M, Stilo SA, Marques TR, Mondelli V, Dazzan P, Pariante C, David AS, Gaughran F, Atakan Z, Iyegbe C, Powell J, Morgan C, Lynskey M, Murray RM. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: A case-control study. Lancet Psychiatry. 2015;2:233–238. doi: 10.1016/S2215-0366(14)00117-5. doi:10.1016/s2215-0366(14)00117-5. [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction with Life Scale. J Pers Assess. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. doi:10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Diener E. Understanding scores on the satisfaction with life scale. Ed Diener. 2006 http://internal.psychology.illinois.edu/~ediener/Documents/Understanding%20SWLS%20Scores.pdf. Accessed on September 22, 2015.
- Ellickson PL, Martino SC, Collins RL. Marijuana use from adolescence to young adulthood: Multiple developmental trajectories and their associated outcomes. Health Psychol. 2004;23:299–307. doi: 10.1037/0278-6133.23.3.299. doi:10.1037/0278-6133.23.3.299. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM. Tests of causal linkages between cannabis use and psychotic symptoms. Addiction. 2005;100:354–366. doi: 10.1111/j.1360-0443.2005.01001.x. doi:10.1111/j.1360-0443.2005.01001.x. [DOI] [PubMed] [Google Scholar]
- Flory K, Lynam D, Milich R, Leukefeld C, Clayton R. Early adolescent through young adult alcohol and marijuana use trajectories: Early predictors, young adult outcomes, and predictive utility. Dev Psychopathol. 2004;16:193–213. doi: 10.1017/s0954579404044475. doi:10.1017/S0954579404044475. [DOI] [PubMed] [Google Scholar]
- Goldberg D, Williams P. A user's guide to the General Health Questionnaire. NFER-NELSON, Windsor; Berkshire: 1988. [Google Scholar]
- Gray KM, Riggs PD, Min S-J, Mikulich-Gilbertson SK, Bandyopadhyay D, Winhusen T. Cigarette and cannabis use trajectories among adolescents in treatment for attention-deficit/hyperactivity disorder and substance use disorders. Drug Alcohol Depend. 2011;117:242–247. doi: 10.1016/j.drugalcdep.2011.02.005. doi:10.1016/j.drugalcdep.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110:19–35. doi: 10.1111/add.12703. doi:10.1111/add.12703. [DOI] [PubMed] [Google Scholar]
- Henquet C, Krabbendam L, Spauwen J, Kaplan C, Lieb R, Wittchen HU, van Os J. Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. Br Med J. 2005;330:11–14. doi: 10.1136/bmj.38267.664086.63. doi:10.1136/bmj.38267.664086.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homel J, Thompson K, Leadbeater B. Trajectories of marijuana use in youth ages 15-25: Implications for postsecondary education experiences. J Stud Alcohol Drugs. 2014;75:674–683. doi: 10.15288/jsad.2014.75.674. doi:10.15288/jsad.2014.75.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, Schulenberg JE. Conjoint developmental trajectories of young adult substance use. Alcohol Clin Exp Res. 2008;32:723–737. doi: 10.1111/j.1530-0277.2008.00643.x. doi:10.1111/j.1530-0277.2008.00643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future: National survey results on drug use, 1975-2013: Volume II: College students and adults ages 19-55. Institute for Social Research, The University of Michigan; Ann Arbor, MI: 2014. [Google Scholar]
- Jones BL, Nagin DS. Advances in group-based trajectory modeling and a SAS procedure for estimating them. Sociol Methods Res. 2007;35:542–571. doi:10.1177/0049124106292364. [Google Scholar]
- Jones SE, Lollar DJ. Relationship between physical disabilities or long-term health problems and health risk behaviors or conditions among US high school students. J Sch Health. 2008;78:252–257. doi: 10.1111/j.1746-1561.2008.00297.x. doi:10.1111/j.1746-1561.2008.00297.x. [DOI] [PubMed] [Google Scholar]
- Joshi M, Joshi A, Bartter T. Marijuana and lung diseases. Curr Opin Pulm Med. 2014;20:173–179. doi: 10.1097/MCP.0000000000000026. doi:10.1097/mcp.0000000000000026. [DOI] [PubMed] [Google Scholar]
- Jouanjus E, Lapeyre-Mestre M, Micallef J. Cannabis use: Signal of increasing risk of serious cardiovascular disorders. J Am Heart Assoc. 2014;3:e000638–e000638. doi: 10.1161/JAHA.113.000638. doi:10.1161/JAHA.113.000638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juon H-S, Fothergill K, Green KM, Doherty EE, Ensminger M. Antecedents and consequences of marijuana use trajectories over the life course in an African American population. Drug Alcohol Depend. 2011;118:216–223. doi: 10.1016/j.drugalcdep.2011.03.027. doi:10.1016/j.drugalcdep.2011.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagerberg TV, Kvitland LR, Aminoff SR, Aas M, Ringen PA, Andreassen OA, Melle I. Indications of a dose-response relationship between cannabis use and age at onset in bipolar disorder. Psychiatry Res. 2014;215:101–104. doi: 10.1016/j.psychres.2013.10.029. doi:10.1016/j.psychres.2013.10.029. [DOI] [PubMed] [Google Scholar]
- Lynne-Landsman SD, Bradshaw CP, Ialongo NS. Testing a developmental cascade model of adolescent substance use trajectories and young adult adjustment. Dev Psychopathol. 2010;22:933–948. doi: 10.1017/S0954579410000556. doi:10.1017/S0954579410000556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehmedic Z, Chandra S, Slade D, Denham H, Foster S, Patel AS, Ross SA, Khan IA, ElSohly MA. Potency trends of delta9-THC and other cannabinoids in confiscated cannabis preparations from 1993 to 2008. J Forensic Sci. 2010;55:1209–1217. doi: 10.1111/j.1556-4029.2010.01441.x. [DOI] [PubMed] [Google Scholar]
- MelissaDATA Income tax statistics lookup. 2003 http://www.melissadata.com/lookups/taxzip.asp. Accessed on May 28, 2008.
- Mittleman MA, Lewis RA, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation. 2001;103:2805–2809. doi: 10.1161/01.cir.103.23.2805. doi:10.1161/01.CIR.103.23.2805. [DOI] [PubMed] [Google Scholar]
- Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, Lewis G. Cannabis use and risk of psychotic or affective mental health outcomes: A systematic review. Lancet. 2007;370:319–328. doi: 10.1016/S0140-6736(07)61162-3. doi:10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- Mukamal KJ, Maclure M, Muller JE, Mittleman MA. An exploratory prospective study of marijuana use and mortality following acute myocardial infarction. Am Heart J. 2008;155:465–470. doi: 10.1016/j.ahj.2007.10.049. doi:10.1016/j.ahj.2007.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polen MR, Sidney S, Tekawa IS, Sadler M, Friedman GD. Health care use by frequent marijuana smokers who do not smoke tobacco. West J Med. 1993;158:596–601. [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. 2008 SAS 9.2. SAS Institute Inc., Cary, NC. [Google Scholar]
- Schulenberg J, Merline A, Johnston LD, O'Malley PM, Bachman JG, Laetz VB. Trajectories of marijuana use during the transition to adulthood: The big picture based on national panel data. J Drug Issues. 2005;35:255–279. doi: 10.1177/002204260503500203. doi:10.1177/002204260503500203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2013 National Survey on Drug Use and Health: Detailed tables. US Department of Health and Human Services, Office of Applied Studies; Rockville, MD: 2014. [Google Scholar]
- Tashkin DP. Effects of marijuana smoking on the lung. Ann Am Thorac Soc. 2013;10:239–247. doi: 10.1513/AnnalsATS.201212-127FR. doi:10.1513/AnnalsATS.201212-127FR. [DOI] [PubMed] [Google Scholar]
- Thomas G, Kloner RA, Rezkalla S. Adverse cardiovascular, cerebrovascular, and peripheral vascular effects of marijuana inhalation: What cardiologists need to know. Am J Cardiol. 2014;113:187–190. doi: 10.1016/j.amjcard.2013.09.042. doi:10.1016/j.amjcard.2013.09.042. [DOI] [PubMed] [Google Scholar]
- van Os J, Bak M, Hanssen M, Bijl RV, Graaf R.d., Verdoux H. Cannabis use and psychosis: A longitudinal population-based study. Am J Epidemiol. 2002;156:319–327. doi: 10.1093/aje/kwf043. doi:10.1093/aje/kwf043. [DOI] [PubMed] [Google Scholar]
- Vincent KB, Kasperski SJ, Caldeira KM, Garnier-Dykstra LM, Pinchevsky GM, O’Grady KE, Arria AM. Maintaining superior follow-up rates in a longitudinal study: Experiences from the College Life Study. Int J Mult Res Approach. 2012;6:56–72. doi: 10.5172/mra.2012.6.1.56. doi:10.5172/mra.2012.6.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells KB, Golding JM, Hough RL, Burnam MA, Karno M. Factors affecting the probability of use of general and medical health and social/community services for Mexican Americans and Non-Hispanic Whites. Med Care. 1988;26:441–452. doi: 10.1097/00005650-198805000-00001. doi:10.1097/00005650-198805000-00001. [DOI] [PubMed] [Google Scholar]